Abstract
There is considerable variation in rehabilitation outcomes within the population of spinal cord–injured individuals across racial and socioeconomic groups. This suggests that the long-term health following spinal cord injury (SCI) is determined, at least in part, by group differences in exposure to advantages and disadvantages among persons living in the community. This article conceptualizes the nature of vulnerability and how increased vulnerability leads to disparities in SCI outcomes. Demographic, socioeconomic, and geographic determinants of adverse outcomes among vulnerable groups are discussed. Finally, a research model that outlines potential processes that elicit vulnerability following SCI and clinical implications is reviewed.
Keywords: health care disparities, health status disparities, spinal cord injury, vulnerable populations
Although advances in rehabilitation medicine have improved the mortality and morbidity rates for the population of spinal cord–injured individuals as a whole, evidence shows that significant disparities occur in rehabilitation outcomes according to differences in individual background and sociodemographic characteristics.1-3 These “uneven” health outcomes can impose a supplemental burden on the rehabilitation and reintegration of underserved groups into the community. Vulnerable populations are groups who have historically experienced marginalization in American society—the poor, racial and ethnic minorities, women, and older adults—and, therefore, experience a disproportionate amount of exposure to the disadvantages that increase the risk for poorer health and diminished well-being.4 In other words, the concept of vulnerability suggests that individuals' experiences, and not their intrinsic qualities, create disparities in health outcomes.5-7
Spinal cord injury (SCI) creates a state of vulnerability, in that this sudden and debilitating injury most often results in chronic disability and an increased risk for secondary health complications that reframe an individual's entire life.5 Living with an SCI exposes an individual to increased risk of “poor physical, psychological and/or social health”6(p487) that may be associated with increased morbidity and premature mortality.8 Furthermore, there is evidence that some groups are at a disproportionate risk for poor outcomes than others following injury. The goal of this paper is to provide a descriptive review of disparate outcomes for vulnerable groups living with SCI. The review is not exhaustive but highlights current findings that best illustrate the individual and social circumstances that contribute to health disparities among vulnerable groups following SCI. Specifically, the review will focus on the 2 salient circumstances that increase the risk of vulnerability for individuals with SCI: sociodemographic (ie, socioeconomic status and race/ethnicity) and resource factors (ie, assistive technology and geography). Finally, the paper will propose a conceptual framework that has research and clinical implications to address disparities observed in vulnerable groups living with SCI.
Socioeconomic Vulnerabilities
Socioeconomic status is the most commonly cited vulnerability characteristic that is associated with variations in mortality and morbidity both in the general population and among disabled groups.9,10 Among the social and demographic disparities noted in the distribution of health and illness, socioeconomic status (SES) – typically assessed by differences in income, educational attainment, and occupational status – is consistently associated with differences in rehabilitation outcomes following SCI. Low income and educational attainment, as well as lack of health insurance, have been shown to increase the risk of mortality among persons with SCI.11-15 Low SES also increases the risk for secondary health complications following SCI. Persons from socioeconomically disadvantaged backgrounds are more likely to report chronic pain16 and emotional distress.17 The relationship between SES and substance abuse is less clear, with reports of higher rates of alcohol and drug abuse among persons of low SES backgrounds18 versus an increased risk for heavy drinking post injury among persons with high educational attainment and income.19 Elsewhere in the literature, high SES is reported to confer advantages post injury. Persons with high levels of educational attainment are more likely to use customized wheelchairs20 and drive modified vehicles,21 which in turn improves their psychological and social outcomes following injury. Access to assistive technology (AT) reinforces and maintains SES attainment, as persons who report AT use also report employment success.22
The association between SES disadvantage and health raises concern that persons with SCI are vulnerable to poorer health because of increased exposure to the financial hardship and material deprivation that frequently accompanies chronic physical disability.23 SCI is an expensive condition; the estimated cost for health care and living expenses for a person with high level tetraplegia is $170,000 annually.24 Persons with chronic disability due to traumatic injuries are more likely to experience reduced income from un- or underemployment and disruptions in insurance coverage due to job loss, while incurring the high costs of ongoing medical care and accommodations necessary to adapt to community living.25 A recent study reported that the incidence of bankruptcy was 3.5% at 5 years post injury among braininjured and spinal cord–injured patients.26 This situation is compounded by the fact that only a fraction of persons with SCI are gainfully employed post injury. Estimates vary, but only about 35% of persons with SCI report working part-time or full-time for pay.24 Education, income, and occupational status preinjury predict employment status after injury, such that persons with low levels of education and low status occupations are less likely to be gainfully employed post injury.27-31 Highly educated individuals (ie, those with a college degree) are also more likely to report a higher rate of earnings.32 Meade et al observed that lower employment rates among persons from minority groups before injury also translated to a larger gap in employment rates post injury between African Americans and Whites.28
Racial and Ethnic Group Vulnerabilities
The US Census defines race and ethnicity according to self-identification of the racial background based on several groups (eg, Caucasian or White, Black or African American, Asian, Native American) and whether or not an individual is of Hispanic or Latino origin (ethnicity).33 This definition is frequently used by researchers to compare differences in morbidity and mortality across racial and ethnic groups. A thorough discussion of the concepts of race and ethnicity, which have been complicated by social, historical, and political origins, is beyond the scope of this article. However, the persistent associations of self-reported race and/or ethnicity with various health indicators continue to make the use of these concepts prevalent in health-related research. There is substantial evidence, for example, that self-reported racial group differences exist in types of treatment received, quality of care, and availability of care, even after controlling for other factors such as income, education, or insurance status.34 Further, as many public health researchers advocate, identifying groups based on some standardized groupings is necessary and beneficial if specialized and targeted interventions are to be designed for groups that are either at high risk for a particular health condition or subject to a health-related disparity.34,35
Racial and/or ethnic minorities living with an SCI are at increased risk of secondary complications,36,37 psychological distress,38,39 and poorer wheelchair quality.20 Several studies have suggested that the occurrence40,41 and severity42 of secondary complications such as pain and pressure ulcers are elevated among persons from minority backgrounds. Cardenas et al reported that among individuals who reported pain post injury, the level of pain severity was higher among minorities in comparison to Whites.43 Fuhrer et al reported that a higher percentage of African Americans with SCI reported severe pressure ulcers (ie, stage III and IV) in comparison to Whites.42 These results are consistent with current research.40 Minority groups are more likely to report problems with access to care to address secondary complications in comparison to Whites.40
Persons from racial and ethnic minority backgrounds are also vulnerable to poorer outcomes in psychological functioning and quality of life following a traumatic SCI. Previous studies have found elevated rates of depressive symptomatology among persons from minority group backgrounds relative to Whites.17,44 Few investigations have attempted to disentangle the covariation between SES and race/ethnicity, although many studies have observed group differences by race among SES factors in persons with SCI. For instance, Krause et al reported that Whites generally reported better subjective well-being (SWB) outcomes, particularly concerning their finances and employment opportunities, relative to the other racial/ethnic groups (ie, African Americans, Hispanics, and Native Americans).39,45 Native Americans reported the poorest SWB on all but one of the subscale (ie, participation), in comparison to the other racial/ethnic groups. Similar findings were reported in a 6-year follow-up study; however, the relative amount of disparities in SWB did not change over time.39
Assistive Technology Vulnerabilities
Recently, disparities in wheelchair prescription have been the focus of attention by rehabilitation researchers as an explanatory factor in race and SES disparities following SCI. Procedures for wheelchair prescription vary greatly depending on the type of insurance coverage and Veteran status. For example, Veterans Administration (VA) guidelines require that chair prescriptions adhere to a standard contracted cost list that includes both customizable and non-customizable manual and power wheelchairs and scooters.46 Although non-contracted chairs may be prescribed to a veteran if necessary, the additional documentation that is required is prohibitive. In contrast, persons with SCI who obtain wheelchairs from a non-VA facility must receive their coverage either through private insurance or through Medicare. In both cases, customizable chairs may be obtained, however both private insurance and Medicare require documentation with substantial justification.47 These differences in prescription practices may lead to racial as well as veteran status disparities that are being explored in our ongoing research.48
For example, research has shown that veterans with SCI from minority group backgrounds were less likely than non-Hispanic Whites to receive customizable wheelchairs and scooters.49 Although this study did not control for SES, participants included persons for whom chairs were fully funded by the Veterans Health Administration. Among non-veterans with SCI, research had shown that minorities, those with less than a high school education, those with public insurance, and people with low incomes were more likely to have standard manual and standard programmable power wheelchairs rather than customizable ones and were less likely to have back-up wheelchairs.50 These disparities are important because the customizability of wheelchairs is an indicator of wheelchair quality. Improved and alternative design and customizable wheelchairs can provide reasonable preventive measures against deleterious conditions like upper limb injuries while improving quality of life (QOL).51-54 Other studies found customizable manual wheelchairs to be more durable,51 cost-effective,55 and comfortable.56
Geographic Vulnerability
Vulnerability for poorer health outcomes is also infuenced by differences in the places where people live. Motivated by a large body of work demonstrating that geographic location is an important social determinant of health,57 several recent rehabilitation studies have suggested that the uneven distribution of resources and infrastructure across geographic areas contributes to differences among vulnerable groups in health and well-being for persons with SCI. For instance, an analysis of a subsample of the Spinal Cord Injury Model Systems (SCIMS) database found that the likelihood of reporting poor health following SCI was higher in socioeconomically disadvantaged areas based on an index derived from US Census measures of household income, wealth, home values, educational attainment, and employment in high status occupations.58 The same investigation also found that the likelihood of reporting dissatisfaction with life was positively associated with SES advantage as well as with living in an urban area. Conversely, other research has reported a negative relationship between area-level SES disadvantage (as measured by the percentage of Census tract residents living below the poverty level) and satisfaction with life following SCI.59 Although the pattern of results reported across these studies varies and is partially attributable to methodological differences in the study samples, level of analysis, and measurement of area-level SES, collectively this work suggests that long-term rehabilitation outcomes reported by persons living in the community varies, at least in part, by the places in which people live.
Rural versus urban differences in rehabilitation outcomes have also been the subject of empirical attention in medical rehabilitation. Adkins and colleagues concluded that living in high crime urban areas was associated with restricted mobility among persons with SCI, which is detrimental to long-term health and functioning.60 Liang and colleagues found that among persons with SCI living in urban areas, self-reported physical activity was lower among individuals living in neighborhoods with higher crime rates.61 However, others have asserted that living in urban versus rural areas is more beneficial to persons with SCI, as rural communities have fewer options for employment, recreation, transportation, and either unavailable or inaccessible health care.62 A recent analysis of the role of area-level economic conditions and urbanicity on employment also suggests that living in a suburban (compared to urban) area increases the odds of working for pay following SCI,63 suggesting that geographic location may also contribute to social participation for persons with chronic SCI. Although it is acknowledged that the quality of a person's environment is necessary to increase independence and functioning,64 research addressing the relationship between community characteristics and outcomes for persons with SCI is only in its nascent stages. In particular, investigations assessing the role of ecological factors such as infrastructure (ie, the distribution of health care facilities, rehabilitation services, transportation, and accessible neighborhoods) and social conditions on long-term outcomes are needed to advance our understanding of geographic vulnerability among persons with SCI.
Implications for Research
This review indicates that not all people adjust well after SCI rehabilitation, and much of this is determined by differences in background, access to technology, and the environment, as well as medical factors. However, explanatory studies of health disparities in SCI outcomes are rare and are needed in order to advance our ability to address health disparities in vulnerable groups. We propose a comprehensive model to assist rehabilitation researchers in advancing our understanding of why health disparities occur so that they may be addressed in clinical practice and public policy.
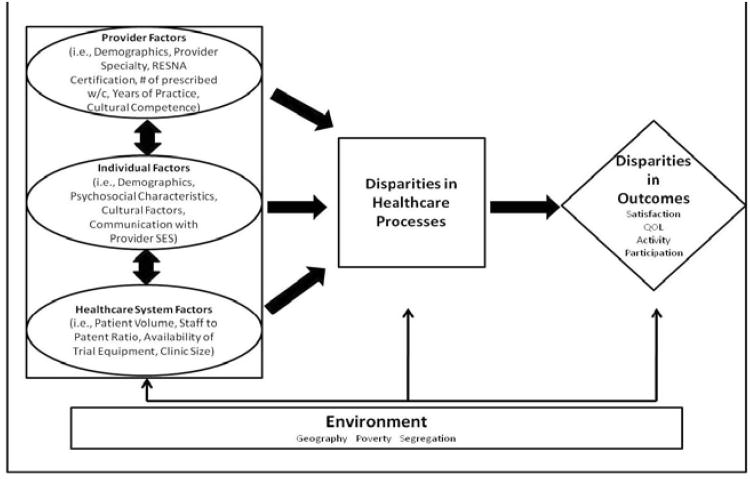
This conceptual model (Figure 1)47 of the associations among exogenous variables (ie, individual, provider, and health care system-level factors), processes of care, and health outcomes is based on a model developed by the Center for Health Equity Research and Promotion (CHERP).4 The model defines how individual, provider, and system factors, as well as the context of a rehabilitation encounter, may contribute to disparities in health care and health outcomes. It posits that individual factors (eg, culture, SES), provider factors (eg, attitudes, practice patterns, training), and health care system/policy factors (eg, organization, availability of expertise, and distribution of resources) interact to affect both health care delivery (processes of care) and health outcomes. The individual, provider, and system factors, processes of care, and health outcomes interact and are influenced by geographic differences in resources and infrastructure as well as other environmental factors (depicted at the bottom of the diagram).
Figure 1.
Conceptual model.
An application of this model considers that persons with SCI represent an at-risk group for health complications due to the chronic nature and complexities of SCI. However, this risk is not deterministic but rather varies based on differences in individual background factors, access, and experiences within the health care system. For example, an uninsured African American male living with an SCI who has a stage II pressure ulcer may be more vulnerable to disparities in health care and health outcomes because he may face more barriers to obtaining treatment. These barriers may include individual factors such as low SES as well as cultural factors such as experiences of discrimination and perceived racism in health care.65 Further, racial minorities and individuals with low SES may be more likely to live in a neighborhood with access to community medical clinics with providers who have limited expertise in SCI (provider factors) rather than outpatient rehabilitation services. Community medical clinics tend to have high patient volume and limited rehabilitation equipment (health care system factors). Providers' care for racial and ethnic minority groups living with an SCI may also be biased by their stereotypes and assumptions (eg, lack of cultural competency).66 Cultural competence requires a health provider to understand the complexities of “social and cultural infuences on patients' beliefs and behaviors and how these factors interact at multiple levels of the healthcare system.”67(p297) Thus, observed disparities in rehabilitation outcomes (eg, secondary health complications, QOL, AT use, and social participation) may occur because individual, provider, and system factors combine to contribute to inadequate health care service delivery.
The application of this model also suggests that methodological changes are necessary for understanding the complex processes that create disparities in rehabilitation outcomes. For example, measures of vulnerability factors, such as self-reported access to care and quality of care, are important aspects of the health care process that are understudied in SCI research. Much of the disparities research in SCI is cross-sectional and therefore limits our ability to draw conclusions on the direction of the associations between vulnerability factors and outcomes, as well as the role of intervening factors. Longitudinal studies will increase our understanding of how the relationship between these factors and outcomes change over time. Finally, research is also needed to examine the infuence of provider factors, such as cultural competence in caring for vulnerable groups, on disparities in health care processes and rehabilitation outcomes.66
Clinical Implications
Clinicians have a responsibility to reduce the risk of individual, provider, and environmental vulnerabilities that may impact a patient's functioning. Additionally, clinicians can offer assistance to clients to mitigate the consequences that result from their vulnerabilities. For example, the location of service delivery (eg, supplier's facility, general practitioner's office, or specialized rehabilitation or assistive technology center) is hypothesized to have a significant infuence on the role of providers on individual outcomes. Similarly, the expertise of the clinician who is treating the person with SCI and making the prescribing recommendation is critical. Clinicians infuence every component of the health care service process through their knowledge and understanding regarding the client's functional, structural, health, and safety needs as well as treatment options. The individual's knowledge about his/her SCI needs and issues is also critical to better health care. Prior experience with wheelchairs as well as self-awareness of functional needs, information-seeking, and the degree to which the individual's perceptions of need are shaped by their interpersonal network, cultural beliefs and experiences, and psychosocial resources are also important implications for clinical care. Finally, cost and insurance factors (eg, insurance requirements, complexity of the payment process, and other funding sources) affect every component of their clinical care even more so than with other disorders.47
Conclusion
Persons with chronic SCI are a vulnerable population due to the increased risk of health complications following injury. This risk is elevated among persons with SCI from racially and socioeconomically disadvantaged backgrounds. Although rehabilitation research has made considerable progress in the past decade in describing at-risk groups, more work in health disparities among rehabilitation populations is needed. In particular, this review suggests that research investigating the processes and the mechanisms that elicit vulnerability to poor health would be instrumental in advancing our understanding of health disparities. In particular, work that describes the complex interaction between individual, provider, and health care system factors that contribute to disparities in health outcomes is needed to improve health care delivery among vulnerable groups living with SCI.
Acknowledgments
This manuscript was supported by the Kessler Foundation Research Center (Fyffe & Botticello). Additional support was provided by grants funded by the National Institute on Disability and Rehabilitation Research: Northern New Jersey Spinal Cord Injury System (NNJSCIS) (H133N060022, Dyson-Hudson & Kirshblum, PIs); and a career development grant (K99HD065957, Botticello, PI). This material is also based upon work supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development Rehabilitation Research and Development Service (B7148I; Myaskovsky, PI).
The contents do not represent the views of the Department of Veterans Affairs or the United States Government.
References
- 1.Jackson A, Dijkers M, Devivo M, Poczatek R. A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil. 2004;85(11):1740–1748. doi: 10.1016/j.apmr.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 2.Krause J, Broderick L, Saladin L, Broyles J. Racial disparities in health outcomes after spinal cord injury: mediating effects of education and income. J Spinal Cord Med. 2006;29(1):17–25. doi: 10.1080/10790268.2006.11753852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krause J, Saladin L, Adkins R. Disparities in subjective well-being, participation, and health after spinal cord injury: a 6-year longitudinal study. NeuroRehabilitation. 2009;24(1):47–56. doi: 10.3233/NRE-2009-0453. [DOI] [PubMed] [Google Scholar]
- 4.Kilbourne A, Switzer GE, Hyman KB, Crowley-Matoka M, Fine M. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96(12):2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Angel S. Vulnerable, but strong: the spinal cord-injured patient during rehabilitation. Int J Qual Stud Health Well-being. 2010;5(3) doi: 10.3402/qhw.v5i3.5145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aday LA. Health status of vulnerable populations. Ann Rev Public Health. 1994;15:487–509. doi: 10.1146/annurev.pu.15.050194.002415. [DOI] [PubMed] [Google Scholar]
- 7.Shi L, Stevens GD. Vulnerable Populations in the United States. San Francisco: Jossey-Bass; 2010. [Google Scholar]
- 8.Flaskerud JH, Winslow BJ. Conceptualizing vulnerable populations health-related research. Nurs Res. 1998;47(2):69–78. doi: 10.1097/00006199-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 10.Wilkinson R, Marmot M. The Social Determinants of Health: The Solid Facts. Vol. 2. Copenhagen: World Health Organization; 2003. [Google Scholar]
- 11.Zarzaur BL, Stair BR, Magnotti LJ, Croce MA, Fabian TC. Insurance type is a determinant of 2-year mortality after non-neurologic trauma. J Surg Res. 2010;160(2):196–201. doi: 10.1016/j.jss.2009.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strauss D, DeVivo M, Shavelle R, Brooks J, Paculdo D. Economic factors and longevity in spinal cord injury: a reappraisal. Arch Phys Med Rehabil. 2008;89(3):572–574. doi: 10.1016/j.apmr.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 13.Krause JS, Devivo MJ, Jackson AB. Health status, community integration, and economic risk factors for mortality after spinal cord injury. Arch Phys Med Rehabil. 2004;85(11):1764–1773. doi: 10.1016/j.apmr.2004.06.062. [DOI] [PubMed] [Google Scholar]
- 14.Krause JS, Saunders LL, De Vivo MJ. Income and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2011;92(3):339–345. doi: 10.1016/j.apmr.2010.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krause JS, Carter RE. Risk of mortality after spinal cord injury: relationship with social support, education, and income. Spinal Cord. 2009;47(8):592–596. doi: 10.1038/sc.2009.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goossens D, Dousse M, Ventura M, Fattal C. Chronic neuropathic pain in spinal cord injury patients: what is the impact of social and environmental factors on care management? Ann Phys Rehabil Med. 2009;52(2):173–179. doi: 10.1016/j.rehab.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Krause JS, Kemp B, Coker J. Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil. 2000;81(8):1099–1109. doi: 10.1053/apmr.2000.7167. [DOI] [PubMed] [Google Scholar]
- 18.Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: risk factors and correlates. Arch Phys Med Rehabil. 2004;85(11):1837–1847. doi: 10.1016/j.apmr.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 19.Saunders LL, Krause JS. Psychological factors affecting alcohol use after spinal cord injury. Spinal Cord. 2011;49(5):637–642. doi: 10.1038/sc.2010.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hunt PC, Boninger ML, Cooper RA, Zafonte RD, Fitzgerald SG, Schmeler MR. Demographic and socioeconomic factors associated with disparity in wheelchair customizability among people with traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85(11):1859–1864. doi: 10.1016/j.apmr.2004.07.347. [DOI] [PubMed] [Google Scholar]
- 21.Norweg A, Jette AM, Houlihan B, Ni P, Boninger ML. Patterns, predictors, and associated benefts of driving a modified vehicle after spinal cord injury: findings from the National Spinal Cord Injury Model Systems. Arch Phys Med Rehabil. 2011;92(3):477–483. doi: 10.1016/j.apmr.2010.07.234. [DOI] [PubMed] [Google Scholar]
- 22.Hedrick B, Pape TL, Heinemann AW, Ruddell JL, Reis J. Employment issues and assistive technology use for persons with spinal cord injury. J Rehabil Res Dev. 2006;43(2):185–198. doi: 10.1682/jrrd.2005.03.0062. [DOI] [PubMed] [Google Scholar]
- 23.Turner JB, Turner RJ. Physical disability, unemployment, and mental health. Rehabil Psychol. 2004;49(3):241–249. [Google Scholar]
- 24.National Spinal Cord Injury Statistical Center. [Accessed April 22, 2011];Spinal Cord Injury Facts and Figures at a Glance. 2011 Feb; https://www.nscisc.uab.edu/public_content/pdf/Facts%202011%20Feb%20Final.pdf. [PubMed]
- 25.Woolhandler S, Himmelstein DU. Double catastrophe: injury-related bankruptcies. Med Care. 2007;45(8):699–701. doi: 10.1097/MLR.0b013e3180f62b9f. [DOI] [PubMed] [Google Scholar]
- 26.Hollingworth W, Relyea-Chew A, Comstock BA, Overstreet JK, Jarvik JG. The risk of bankruptcy before and after brain or spinal cord injury: a glimpse of the iceberg's tip. Med Care. 2007;45(8):702–711. doi: 10.1097/MLR.0b013e318041f765. [DOI] [PubMed] [Google Scholar]
- 27.Arango-Lasprilla JC, Ketchum JM, Stevens LF, et al. Ethnicity/racial differences in employment outcomes following spinal cord injury. NeuroRehabilitation. 2009;24(1):37–46. doi: 10.3233/NRE-2009-0452. [DOI] [PubMed] [Google Scholar]
- 28.Meade MA, Lewis A, Jackson MN, Hess DW. Race, employment, and spinal cord injury. Arch Phys Med Rehabil. 2004;85(11):1782–1792. doi: 10.1016/j.apmr.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Krause JS, Kewman D, Devivo MJ, et al. Employment after spinal cord injury: an analysis of cases from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil. 1999;80(11):1492–1500. doi: 10.1016/s0003-9993(99)90263-0. [DOI] [PubMed] [Google Scholar]
- 30.Krause JS, Sternberg M, Maides J, Lottes S. Employment after spinal cord injury: differences related to geographic region, gender, and race. Arch Phys Med Rehabil. 1998;79(6):615–624. doi: 10.1016/s0003-9993(98)90033-8. [DOI] [PubMed] [Google Scholar]
- 31.Krause JS, Terza JV, Dismuke C. Earnings among people with spinal cord injury. Arch Phys Med Rehabil. 2008;89(8):1474–1481. doi: 10.1016/j.apmr.2007.12.040. [DOI] [PubMed] [Google Scholar]
- 32.Krause JS, Terza JV. Injury and demographic factors predictive of disparities in earnings after spinal cord injury. Arch Phys Med Rehabil. 2006;87(10):1318–1326. doi: 10.1016/j.apmr.2006.07.254. [DOI] [PubMed] [Google Scholar]
- 33.United States Census B. [Accessed May 20, 2011];US Census glossary. http://factfinder.census.gov/home/en/epss/glossary_r.html.
- 34.Mays VM, Ponce NA, Washington DL, Cochran SD. Classification of race and ethnicity: Implications for public health. Ann Rev Publ Health. 2003;24:83–110. doi: 10.1146/annurev.publhealth.24.100901.140927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin SS, Kelsey JL. Use of race and ethnicity in epidemiologic research: concepts, methodological issues, and suggestions for research. Epidemiol Rev. 2000;22(2):187–202. doi: 10.1093/oxfordjournals.epirev.a018032. [DOI] [PubMed] [Google Scholar]
- 36.Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil. 2004;85(11):1740–1748. doi: 10.1016/j.apmr.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 37.Nobunaga AI, Go BK, Karunas RB. Recent demographic and injury trends in people served by the Model Spinal Cord Injury Care Systems. Arch Phys Med Rehabil. 1999;80(11):1372–1382. doi: 10.1016/s0003-9993(99)90247-2. [DOI] [PubMed] [Google Scholar]
- 38.Arango-Lasprilla JC, Ketchum JM, Francis K, Premuda P, Stejskal T, Kreutzer J. Infuence of race/ethnicity on divorce/separation 1, 2, and 5 years post spinal cord injury. Arch Phys Med Rehabil. 2009;90(8):1371–1378. doi: 10.1016/j.apmr.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 39.Krause JS, Saladin LK, Adkins RH. Disparities in subjective well-being, participation, and health after spinal cord injury: a 6-year longitudinal study. NeuroRehabilitation. 2009;24(1):47–56. doi: 10.3233/NRE-2009-0453. [DOI] [PubMed] [Google Scholar]
- 40.Saladin LK, Krause JS. Pressure ulcer prevalence and barriers to treatment after spinal cord injury: comparisons of four groups based on race-ethnicity. NeuroRehabilitation. 2009;24(1):57–66. doi: 10.3233/NRE-2009-0454. [DOI] [PubMed] [Google Scholar]
- 41.Chen Y, Devivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil. 2005;86(6):1208–1213. doi: 10.1016/j.apmr.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 42.Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil. 1993;74(11):1172–1177. [PubMed] [Google Scholar]
- 43.Cardenas DD, Bryce TN, Shem K, Richards JS, Elhefni H. Gender and minority differences in the pain experience of people with spinal cord injury. Arch Phys Med Rehabil. 2004;85(11):1774–1781. doi: 10.1016/j.apmr.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 44.Kemp BJ, Krause JS, Adkins R. Depression among African Americans, Latinos, and Caucasians with spinal cord injury: an exploratory study. Rehabil Psychol. 1999;44(3):235–247. [Google Scholar]
- 45.Krause JS, Broderick L. Outcomes after spinal cord injury: comparisons as a function of gender and race and ethnicity. Arch Phys Med Rehabil. 2004;85(3):355–362. doi: 10.1016/s0003-9993(03)00615-4. [DOI] [PubMed] [Google Scholar]
- 46.Hubbard SL, Fitzgerald SG, Vogel B, Reker D, Cooper RA, Boninger ML. Distribution and cost of wheelchairs and scooters provided by Veterans Health Administration. J Rehabil Res Dev. 2007;44(4):581–592. doi: 10.1682/jrrd.2006.10.0136. [DOI] [PubMed] [Google Scholar]
- 47.Eggers SL, Myaskovsky L, Burkitt KH, et al. A preliminary model of wheelchair service delivery. Arch Phys Med Rehabil. 2009;90:1030–1038. doi: 10.1016/j.apmr.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 48.Myaskovsky L, Boninger ML, Fine MJ, et al. Understanding Quality and Equity in Wheelchairs for Veterans. VA Pittsburgh Healthcare System: Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development Rehabilitation Research and Development Service; 2010-2013. [Google Scholar]
- 49.Hubbard SL, Fitzgerald SG, Reker DM, Boninger ML, Cooper RA, Kazis LE. Demographic characteristics of veterans who received wheelchairs and scooters from Veterans Health Administration. J Rehabil Res Dev. 2006;43(7):831–844. doi: 10.1682/jrrd.2005.11.0174. [DOI] [PubMed] [Google Scholar]
- 50.Hunt PC, Boninger ML, Cooper RA, Zafonte RD, Fitzgerald SG, Schmeler MR. Demographic and socioeconomic factors associated with disparity in wheelchair customizability among people with traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85:1859–1864. doi: 10.1016/j.apmr.2004.07.347. [DOI] [PubMed] [Google Scholar]
- 51.Boninger M, Cooper R, Baldwin M, Shimada S, Koontz A. Wheelchair pushrim kinetics: body weight and median nerve function. Arch Phys Med Rehabil. 1999;80(8):910–915. doi: 10.1016/s0003-9993(99)90082-5. [DOI] [PubMed] [Google Scholar]
- 52.Boninger ML, Baldwin MA, Cooper RA, Koontz AM, Chan L. Manual wheelchair pushrim biomechanics and axle position. Arch Phys Med Rehabil. 2000;81(5):608–613. doi: 10.1016/s0003-9993(00)90043-1. [DOI] [PubMed] [Google Scholar]
- 53.Cooper RA. Advances in wheelchair and related technologies. Med Eng Physics. 2001;23(4):iii–iv. [Google Scholar]
- 54.Fitzgerald SG, Cooper RA, Boninger ML, Rentschler AJ. Comparison of fatigue life for 3 types of manual wheelchairs. Arch Phys Med Rehabil. 2001;82(10):1484–1488. doi: 10.1053/apmr.2001.26139. [DOI] [PubMed] [Google Scholar]
- 55.Cooper RA, Robertson RN. Life-cycle analysis of depot versus rehabilitation manual wheelchairs. J Rehabil Res Dev. 1996;33(1):45–55. [PubMed] [Google Scholar]
- 56.DiGiovine MM, Cooper RA, Boninger ML, Lawrence BM, VanSickle DP, Rentschler AJ. User assessment of manual wheelchair ride comfort and ergonomics. Arch Phys Med Rehabil. 2000;81:490–494. doi: 10.1053/mr.2000.3845. [DOI] [PubMed] [Google Scholar]
- 57.Kawachi I, Berkman L. Neighborhoods and Health. New York: Oxford University Press; 2003. [Google Scholar]
- 58.Botticello AL, Chen Y, Cao Y, Tulsky DS. Do communities matter after rehabilitation? The effect of socioeconomic and urban stratifcation on well-being after spinal cord injury. Arch Phys Med Rehabil. 2011;92(3):464–471. doi: 10.1016/j.apmr.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roach MJ. Community social structure as an indicator of social integration and its effect on quality of life for persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2002;7(3):101–111. [Google Scholar]
- 60.Adkins RH, Hume B, Nabor M, Waters RL. Spinal cord injury indentified with violence: Community reintegration in urban areas. Top Spinal Cord Inj Rehabil. 1998;4:18–27. [Google Scholar]
- 61.Liang H, Tomey K, Chen D, Savar NL, Rimmer JH, Braunschweig CL. Objective measures of neighborhood environment and self-reported physical activity in spinal cord injured men. Arch Phys Med Rehabil. 2008;89(8):1468–1473. doi: 10.1016/j.apmr.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 62.Hagglund KJ, Clay DL, Acuff M. Community reintegration for persons with spinal cord injury living in rural America. Top Spinal Cord Inj Rehabil. 2009;4:28–40. [Google Scholar]
- 63.Botticello AL, McCabe J, Maldonado A. The infuence of area-level economic conditions on employment for adults with physical disability; Presented at: Annual Meeting of the American Public Health Association; 2009; Philadelphia, Pennsylvania. [Google Scholar]
- 64.Gray DB, Hendershot GE. The ICIDH-2: developments for a new era of outcomes research. Arch Phys Med Rehabil. 2000;81(12 Suppl 2):S10–14. doi: 10.1053/apmr.2000.20616. [DOI] [PubMed] [Google Scholar]
- 65.Myaskovsky L, Burkitt KH, Lichy AM, et al. The association of race, cultural factors, and health-related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil. 2011;92:441–448. doi: 10.1016/j.apmr.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 66.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40((1) (supplement)):I140–I151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 67.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports. 2003;118(July-August):293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]