Abstract
AIM: To assess the differences in clinical benefits and disadvantages of single-incision laparoscopic appendectomy (SILA) and conventional laparoscopic appendectomy (CLA).
METHODS: The Cochrane Library, MEDLINE, Embase, Science Citation Index Expanded, and Chinese Biomedical Literature Database were electronically searched up through January 2013 to identify randomized controlled trails (RCTs) comparing SILA with CLA. Data was extracted from eligible studies to evaluate the pooled outcome effects for the total of 1068 patients. The meta-analysis was performed using Review Manager 5.2.0. For dichotomous data and continuous data, the risk ratio (RR) and the mean difference (MD) were calculated, respectively, with 95%CI for both. For continuous outcomes with different measurement scales in different RCTs, the standardized mean difference (SMD) was calculated with 95%CI. Sensitivity and subgroup analyses were performed when necessary.
RESULTS: Six RCTs were identified that compared SILA (n = 535) with CLA (n = 533). Five RCTs had a high risk of bias and one RCT had a low risk of bias. SILA was associated with longer operative time (MD = 5.68, 95%CI: 3.91-7.46, P < 0.00001), higher conversion rate (RR = 5.14, 95%CI: 1.25-21.10, P = 0.03) and better cosmetic satisfaction score (MD = 0.52, 95%CI: 0.30-0.73, P < 0.00001) compared with CLA. No significant differences were found for total complications (RR = 1.15, 95%CI: 0.76-1.75, P = 0.51), drain insertion (RR = 0.72, 95%CI: 0.41-1.25, P = 0.24), or length of hospital stay (SMD = 0.04, 95%CI: -0.08-0.16, P = 0.57). Because there was not enough data among the analyzed RCTs, postoperative pain was not calculated.
CONCLUSION: The benefit of SILA is cosmetic satisfaction, while the disadvantages of SILA are longer operative time and higher conversion rate.
Keywords: Single incision, Laparoscopic, Appendectomy, Meta-analysis, Systematic review
Core tip: The clinical benefit of single-incision laparoscopic appendectomy (SILA), compared to the conventional three-port laparoscopic appendectomy, has been a controversial issue in recent years. We performed the first systematic review and meta-analysis of randomized controlled trails (RCTs) that have assessed the clinical benefits and disadvantages between SILA and conventional laparoscopic appendectomy (CLA). Six RCTs conducted between 2011 and 2013 were identified and pooled to determine outcomes using meta-analytic methods. From this analysis, we conclude that SILA is as safe as CLA. Although patients receiving SILA had longer operative times and a higher conversion rate, one benefit of SILA is cosmetic satisfaction.
INTRODUCTION
Appendectomy is one of the most commonly performed surgical procedures of the abdomen in the world. This surgical procedure has been performed for over 100 years, after first being described by McBurney[1]. With rapidly developing, minimally invasive surgery, the laparoscopic appendectomy has become a selectable method for appendectomy. Previous studies have reported that laparoscopic appendectomy has many advantages in comparison to open appendectomy, such as shorter hospital stays, reduced risks of complications, and better cosmetic satisfaction[2,3]. Therefore, the laparoscopic appendectomy, like laparoscopic cholecystectomy, is considered to be a favorable procedure for appendectomy in the future.
In addition, the use of single-incision laparoscopic techniques, which have been described with promising results in multiple studies[4-11], has increased over the past few years. Under such circumstances, surgical appendectomy may be undergoing a transition from the conventional three-port laparoscopic surgery toward the less-invasive, single-incision laparoscopic surgery. With the number of incisions reduced to just one umbilical incision, the potential advantages of single-incision surgery include better cosmetic outcome, less postoperative pain, and faster postoperative recovery. At the same time, this new technique may present potential disadvantages, such as increased operative time, higher conversion rates, and more complications.
Although a number of studies in the last few years have compared the single-incision laparoscopic appendectomy (SILA) with conventional laparoscopic appendectomy (CLA), most only demonstrated the feasibility and safety of SILA. Well-described benefits and disadvantages are still lacking in the literature. To our knowledge, there are no published meta-analyses describing randomized controlled trails (RCTs) comparing SILA with CLA. Therefore, we conducted a systematic review and meta-analysis of RCTs to assess the clinical benefits and disadvantages associated with SILA and CLA.
MATERIALS AND METHODS
Searching strategy
We searched the following databases up through January 2013 to identify RCTs: The Cochrane Library, MEDLINE, EMBASE, Science Citation Index Expanded, and the Chinese Biomedical Literature Database. The search strategies are shown in Table 1. Language was not used as a criterion for selection of studies, and both English and non-English studies were included. Moreover, the citations within the reference lists of the articles were searched manually to identify additional eligible studies. After all searches were completed, the search results were merged using the software package Endnote X6 to remove duplicate records. The title and abstract of every identified record was scanned by two independent authors (Wu SJ and Cheng Y) for the inclusion criteria. If compliance was not clear from the abstract, full-texts were retrieved for further assessment.
Table 1.
Search strategies
| Databases | Period of search | Search strategies |
| The Cochrane Library | Through January 30, 2013 | (1) MeSH descriptor Appendectomy, Laparoscopic explode all trees |
| (2) (laparoscop* or coelioscop* or celioscop* or peritoneoscop*) and appendectom* | ||
| (3) 1 or 2 | ||
| (4) “single incision” or “single port” or “single site” or “one port” or “one incision” or “one site” | ||
| (5) 3 and 4 | ||
| MEDLINE (Pubmed) | Through January 30, 2013 | (1) Appendectomy, laparoscopic [MeSH] |
| (2) (laparoscop* or coelioscop* or celioscop* or peritoneoscop*) and appendectom* | ||
| (3) 1 or 2 | ||
| (4) “single incision” or “single port” or “single site” or “one port” or “one incision” or “one site” | ||
| (5) (randomised controlled trial [pt] or controlled clinical trial [pt] or randomised [tiab] or placebo [tiab] or drug therapy [sh] or randomly [tiab] or trial [tiab] or groups [tiab]) not (animals [mh] not humans [mh]) | ||
| (6) 3 and 4 and 5 | ||
| EMBASE (OvidSP) | Through January 30, 2013 | (1) (appendectomy.af.) or ( exp appendectomy/) |
| (2) ((laparoscop* or coelioscop* or celioscop* or peritoneoscop*).af.) or ( exp Laparoscopy/) | ||
| (3) (single incision or single port or single site or one port or one incision or one site).af. | ||
| (4) (random* or factorial* or crossover* or placebo*).af. | ||
| (5) expcrossoverprocedure/or exp double-blind procedure/or exp randomized controlled trial/or single-blind procedure/ | ||
| (6) 4 or 5 | ||
| (7) 1 and 2 and 3 and 6 | ||
| Science Citation Index Expanded | Through January 30, 2013 | (1) TS = (appendectom*) |
| (2) TS = (laparoscop* or coelioscop* or celioscop* or peritoneoscop*) | ||
| (3) TS = (“single incision” or “single port” or “single site” or “one port” or “one incision” or “one site”) | ||
| (4) TS = (random* or blind* or placebo* or meta-analysis) | ||
| (5) 1 and 2 and 3 and 4 | ||
| CBM | Through January 30, 2013 | Search strategy in was performed in Chinese. Includes search terms similar to the terms used in MEDLINE |
MEDLINE: Medical Literature Analysis and Retrieval System Online; EMBASE: Excerpta Medica Database; CBM: Chinese Biomedical Literature Database; MeSH: Medical Subject Heading.
Inclusion and exclusion criteria
The aim of this meta-analysis was to specifically compare the benefits and disadvantages of SILA and CLA methods. Therefore, only those studies which provided comparison between those two methods mentioned above were included. Reliability was the most important point considered in this meta-analysis, so only RCTs were included. Prospective non-randomized, retrospective, and improperly performed RCTs were excluded from the analysis.
The definition of SILA was surgery through a single intra-umbilical incision. The included studies used various multiport devices or multiple conventional ports through a single skin incision but with multiple fascial incisions. CLA was defined as surgery with the standard three-port technique via a supra-umbilical or infra-umbilical port, a left lower quadrant port, and a right lower quadrant or supra-pubic region port.
Data extraction and validity assessment
Two independent authors (Lu J and Zhang J) extracted and confirmed the data and entered them into an electronic data collection form. Any disagreement in the two reviewers’ data collection and quality assessment was discussed until a consensus was reached. For the validity assessment, another two authors (Cai YL and Lin YX) independently assessed the methodological quality of the included trials using the quality checklist recommended by the Cochrane Handbook. The assessment contained six dimensions: (1) random sequence generation; (2) allocation concealment; (3) blinding; (4) addressing of incomplete outcome data; (5) selective reporting; and (6) other bias. Following the evaluation of the above domains, an included trial was judged as having low risk of bias if it was evaluated as “low” in all of the above domains. If the risk of bias was judged as “unclear” or “high”, then the trial was listed under the group of trials with “high risk of bias.” Otherwise, all disagreements were resolved by discussion and referral to a third author (Xiong XZ) for resolution.
Outcomes
Data for the following outcomes were extracted: total operative time, total complications (wound infection, abscess, ileus, stump leakage, etc.), drain insertion, conversion rate, length of hospital stay, postoperative pain as assessed using the visual analogue scale (VAS), and cosmetic satisfaction.
Statistical analysis
We performed all the statistical analyses of the extracted data with Review Manager 5.2.0. For dichotomous data and continuous data, we calculated the risk ratio (RR) and the mean difference (MD) with 95%CIs for both. For continuous outcomes with different measurement scales in different RCTs, we calculated the standardized mean difference (SMD) with 95%CI. Heterogeneity was described with the χ2 test. A P value less than 0.10 was considered to be significant heterogeneity and the I² statistic was used to measure the quantity of heterogeneity. If significant heterogeneity existed, a random-effect model was used. In the absence of significant heterogeneity, a fixed-effect model was adopted.
In the case of missing data, we contacted the original investigators to request further information. If there was no reply, we performed the analysis on an “intention-to-treat” principle, if applicable. Otherwise, we adopted the available-case analysis, also known as the per-protocol analysis. A few published clinical trials reported a median and a range instead of a mean and SD. To adjust this difference, we assumed that the median was equal to the mean, and we estimated the SD as a quarter of the reported range. Funnel plots were used to determine reporting biases. We conducted the meta-analysis and systematic review according to the Cochrane Handbook for Systematic Reviews of Interventions and Preferred Reporting Item for Systematic Reviews and Meta-Analysis.
RESULTS
Search results
We identified a total of 111 records through electronic searches of The Cochrane Library (n = 12), MEDLINE (n = 21), EMBASE (n = 32), Science Citation Index Expanded (n = 44), Chinese Biomedical Literature Database (n = 0), and a manual search of the references in the included RCTs (n = 2). We excluded 39 duplicates and 72 clearly irrelevant records by reading titles and abstracts. Fourteen full-text articles were retrieved for further assessment. We excluded seven articles for the reasons listed in Figure 1.
Figure 1.
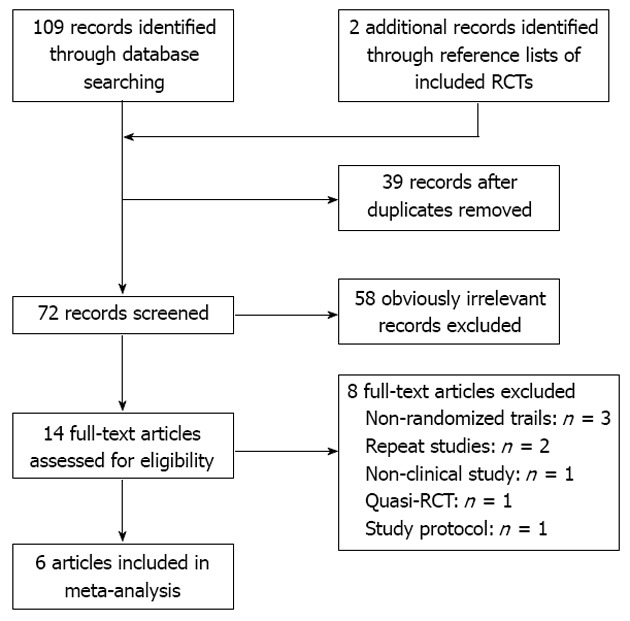
Flow diagram demonstrating the study selection process. RCT: Randomized controlled trial.
Description of included trials and risk of bias
Six RCTs published between 2011 and 2013 were identified that fulfilled the inclusion criteria[12-17]. A total of 1068 patients were included. There were 535 patients who received SILA and 533 who received CLA. Two included trials were of pediatric patients[14,15], and the remaining four trials were of adult patients[12,13,16,17]. Details on the included studies are shown in Table 2. The risk of bias is summarized in Table 3. Five RCTs had a high risk of bias[13-17], and one RCT had a low risk of bias[12].
Table 2.
Study characteristics
| Study | Area | Study design | Participants (SILA/CLA) | Mean age, yr (SILA/CLA) | Male:female ratio (SILA/CLA) |
| Teoh et al[12] | Hong Kong | Multi-center | 195 (98/97) | 39.2/40.7 | 58:40/59:38 |
| Lee et al[13] | South Korea | Single-center | 229 (116/113) | 28.4/28.5 | 64:52/68:45 |
| Perez et al[14] | United States | Single-center | 50 (25/25) | 8.7/8.9 | 10:15/15:10 |
| St Peter et al[15] | United States | Single-center | 360 (180/180) | 11.1/11.1 | 99:81/92:88 |
| Sozutek et al[16] | Turkey | Single-center | 50 (25/25) | 30.6/30.0 | 12:13/7:18 |
| Frutos et al[17] | Spain | Single-center | 184 (91/93) | 28.0/31.0 | 42:49/47:46 |
SILA: Single-incision laparoscopic appendectomy; CLA: Conventional laparoscopic appendectomy.
Table 3.
Risk of bias assessment
| Study | Sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting |
| Teoh et al[12] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Lee et al[13] | Low risk | Uncertain | High risk | High risk | Uncertain | Low risk |
| Perez et al[14] | Low risk | Low risk | Low risk | Low risk | Uncertain | High risk |
| St Peter et al[15] | Low risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Sozutek et al[16] | Low risk | Uncertain | High risk | High risk | Uncertain | High risk |
| Frutos et al[17] | Low risk | Uncertain | High risk | High risk | Low risk | High risk |
Effect of interventions
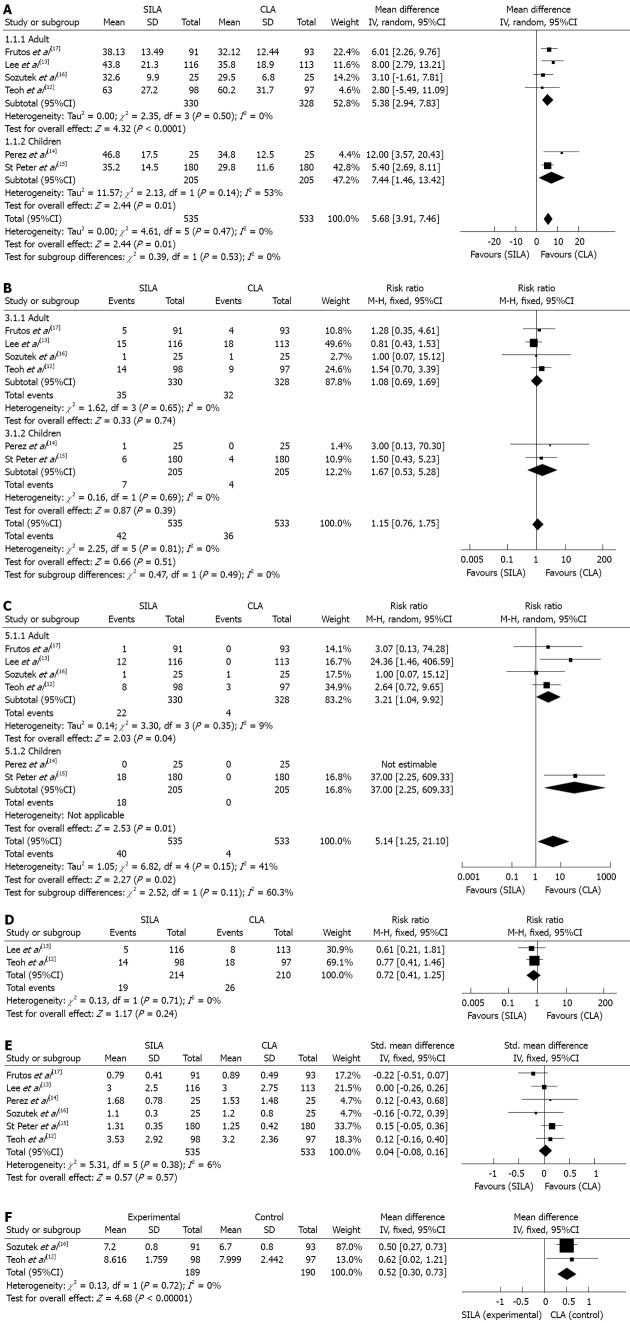
Total operative time: All six RCTs reported the operative time to complete appendectomy[12-17]. The operative time was significantly longer in the SILA group than in the CLA group (Figure 2A; MD = 5.68, 95%CI: 3.91-7.46, P < 0.00001). There was no evidence of statistical heterogeneity (χ² = 4.61, P = 0.47, I² = 0%).
Figure 2.
Forest plots of the meta-analysis. A: Comparisons of single-incision laparoscopic appendectomy (SILA) vs conventional laparoscopic appendectomy (CLA) in total operative time; B: Total complications; C: Conversion rate; D: Drain insertion; E: Length of hospital stay; F: Cosmetic satisfaction.
Total complications: All six RCTs reported the total complications after appendectomy[12-17]. There was no significant difference in the overall incidence of postoperative complications between the two groups (Figure 2B; RR = 1.15, 95%CI: 0.76-1.75, P = 0.51). There was no evidence of statistical heterogeneity (χ² = 2.25, P = 0.81, I² = 0%).
Conversion rate: All six RCTs reported the conversion rates during appendectomy[12-17]. This included placement of additional laparoscopic ports for SILA and conversion to open appendectomy from both SILA and CLA .The conversion rate was 7.48% (40 of 535 patients) and 0.75% (4 of 533 patients) in the SILA and CLA groups, respectively. The rate was significantly higher in patients who received SILA than CLA (Figure 2C; RR = 5.14, 95%CI: 1.25-21.10, P = 0.02). Significant heterogeneity was present in the trials (χ² = 6.82, P = 0.15, I² = 41%).
Drain insertion: Only two RCTs reported drain insertion during appendectomy[12,13]. There was no significant difference in the incidence of drain insertion between the two groups (Figure 2D; RR = 0.72, 95%CI: 0.41-1.25, P = 0.24). There was no evidence of statistical heterogeneity (χ² = 0.13, P = 0.71, I² = 0%).
Length of hospital stay: The length of hospital stay was evaluated in all studies[12-17], but only three studies reported this data in the form of mean and SD[12,16,17]. By contacting the authors personally by email, we were able to retrieve the mean and SD data for the other two studies[14,15]. Another study provided the mean and range[13]. According to our predefined plan, we equated the SD with a quarter of the reported range. There was no significant difference between the two groups (Figure 2E; SMD = 0.04, 95%CI: -0.08-0.16, P = 0.57). There was no evidence of statistical heterogeneity (χ² = 5.31, P = 0.38, I² = 6%).
Postoperative pain: Four of the included trials reported postoperative pain scores using the VAS (10-point or 100-mm) after appendectomy[12,13,16,17]. Teoh et al[12] indicated that there were no significant differences in the overall pain scores and the pain scores at rest (P = 0.109 and 0.154, respectively), while significantly worse pain was experienced in the SILA group after coughing 10 times and on standing (P = 0.001 and 0.038, respectively). Lee et al[13] stated that postoperative pain scores were not statistically different between the two groups at 12 h, 24 h, 36 h and 14 d postoperatively (P = 0.651, 0.555, 0.570 and 0.631, respectively). Likewise, Sozutek et al[16] stated that no difference was detected in terms of postoperative pain (P = 0.991). However, in Frutos’ trial, less pain was found in SILA group (SILA/CLA: 2.76 ± 1.64/3.78 ± 1.76, P < 0.001). Only one study provided the mean and SD, so those values were not calculated in this analysis.
Cosmetic satisfaction: Three studies reported cosmetic satisfaction scores[12,13,16]. The cosmetic score was also measured by a 5-point VAS with a higher score indicating better satisfaction. The meta-analysis of two studies[12,16], which provided the mean and SD, reported that the cosmetic scores were significantly higher in the SILA group than in the CLA group (Figure 2F; MD = 0.52, 95%CI: 0.30-0.73, P < 0.00001). There was no evidence of statistical heterogeneity (χ² = 0.13, P = 0.72, I² = 0%). However, the remaining trial reported no significant difference between the two groups with VAS scores of 4.0 and 3.3 for SILA and CLA, respectively (P = 0.128)[13].
Subgroup analysis: Because the age of the patients may have influenced the eventual outcome, we performed a subgroup analysis for operative time, total complications, and conversion rate. In the subgroup analysis of age, the outcomes were also equivalent.
DISCUSSION
The single-incision method of laparoscopic appendectomy, compared to the conventional three-port method, has been a controversial issue in recent years. Numerous studies have been performed to evaluate the differences; however, most of them were non-RCT studies. Fortunately, six new RCTs published between 2011 and 2013[12-17] evaluated the benefits and disadvantages of SILA and CLA in a quantitative manner and provided the basis of this study. This meta-analysis and systematic review of those six RCTs indicated that although SILA was associated with a longer operative time and a higher conversion rate, patients had better cosmetic satisfaction compared with CLA. No significant differences were found in total complications, drain insertion, length of hospital stay, and postoperative pain between the two procedures.
Regarding operative time, a meta-analysis of non-RCTs concluded that there was no difference between the two groups[18]. Those results were inconsistent with the results of this analysis, which determined that the SILA operative time was longer by 5.68 min. This discrepancy may have been due to the lack of surgical experience using the new technique. Performing SILA requires experience in laparoscopic surgery, and a certain number of cases must be performed to overcome the learning curve. A retrospective study by Lee et al[19] reported that the operation time tended to shorten when the surgeon gained more experience and accumulated cases. This finding is in agreement with a separate report by Perez et al[14], which reported that in the first 25 patients enrolled, the difference in operative time was significantly greater (49.31 min vs 33.50 min, P = 0.049) and that this difference decreased in a subsequent group of 25 patients (44.08 min vs 36.00 min, P = 0.123). Although one disadvantage of SILA is a longer operative time, we believe that with increased experience and developed instrumentation SILA will reach equivalent effectiveness to conventional three-port methods.
Conversion rate is another major concern for surgeons. The high conversion rate is an important disadvantage and has considerably limited the widespread use of SILA. In our meta-analysis, we found that the heterogeneity was very high among the analyzed studies. Therefore, in order to assess the reliability and stability of this outcome, we conducted a sensitivity analysis; only two of the evaluated RCTs precisely described the conversion- fulfilled, predefined outcome[13,15]. After this analysis, a significantly higher rate was observed in the SILA group (RR = 30.64, 95%CI: 4.22-222.68, P = 0.0007) and no heterogeneity was found (χ² = 0.04, P = 0.84, I² = 0%). Thus, we confirmed that a higher conversion rate was consistent with SILA treatment. Technical difficulty could account for this. Complicated appendicitis exists in 30% of all appendicitis cases[20] and when the operation is difficult, such as with serious adhesion or significant inflammation, the single-incision approach can be somewhat cumbersome.
In such scenarios, extra incision sites or use of surgical instruments may become necessary. In a study by St Peter et al[15], surgeons rated the degree of technical difficulty for every case, excluding perforated appendicitis, on a subjective scale from 1 to 5 with 1 indicating an easy case and 5 indicating a difficult case. Higher surgical difficultly ratings were noted for SILA relative to the standard three-port laparoscopic appendectomy (2.3 ± 1.4 vs 1.7 ± 1.0, P < 0.001). Thus, not only in complicated appendicitis, but also in uncomplicated appendicitis, the decision to add an additional site or use additional instrumentation is dependent on a lower comfort level with single-site procedures. However, Crohn’s disease can be performed with a single-site procedure in the presence of significant inflammation[21]. This indicates that if only to promote surgeon comfort level, pure SILA could become easier to complete. Further technical research and developments are needed to reduce the difficulty of SILA and to allow surgeons to comfortably perform this procedure. This may be the only way to reduce the conversion rate when implementing SILA.
Postoperative pain is another controversial topic to be discussed when a single-incision technique is applied. As a result of a reduced trocar use, less surgical pain was postulated in SILA[22]. A small case series and a retrospective analysis reported that reduced pain was found with SILA[23,24]. Conversely, the combined size of the fascial incision at the umbilicus required to accommodate the single-incision port may give rise to more potential pain compared with multiple, smaller fascial incisions in CLA. A 40-patient pilot trial in adults found significantly greater pain scores in the initial 24 h after SILA[25]. Moreover, from an anatomical point of view, the true pelvic peritoneum has less sensitivity to acute pain than the parietal peritoneum in the umbilicus[26]. Thus, the two ports in the lower abdomen in CLA may cause less pain than repositioning them to the umbilicus. Thus, by analyzing previous studies, whether there is less postoperative pain with SILA is uncertain.
In this analysis, three of the included RCTs indicated that the pain scores were comparable between the two groups[12,13,16]. Although, Teoh et al[12] concluded that more pain was identified in activity, the overall scores demonstrated no significant difference. This is in agreement with a previous non-RCT meta-analysis[18]. Moreover, the same comparison in cholecystectomy also showed no significant difference in pain scores at 6 and 24 h between single-incision and multiple-incision procedures[27]. Conversely, another RCT showed less pain was found with SILA, although this difference was very small[17]. Thus, we believe that the pain is not much different between SILA and CLA. However, the overall length of incision may be an important factor in this debate. As many discrepancies exist in the analyzed studies, data from future RCTs are anticipated to resolve these potential differences.
This meta-analysis highlighted cosmetic satisfaction as the significant benefit of SILA over CLA. This so-called “scarless” procedure meets the demand of expecting to conceal the surgical history of patients, especially in young females. Although SILA definitely reduces the number of incisions and often results in better cosmetic satisfaction among patients, there was not enough clinical data to support this claim previously. We recognize that some studies showed better scores without significant differences[13,28], possibly due to existing high cosmetic scores with CLA and leaving only slightly more room for improvement with SILA.
Some limitations exist in assessing cosmetic satisfaction. First, a standard tool to assess the appearance of the wound is still lacking. Second, patients rate the score by their own subjective feeling without a more quantitative reference. We speculate that after surgery, patients may be more focused on whether the disease had been cured rather than on a cosmetic score. Third, wound healing is a long-term process, and the cosmetic benefit should be assessed during both short-term and long-term follow-up examinations. Therefore, prospective RCTs with long-term follow-up are needed to confirm the cosmetic benefits of SILA. Establishing a validated scar assessment tool is also necessary for adequate quantitative analysis.
Six RCTs were included in this review. Most included patients with perforated appendicitis, while only one study excluded patients with perforated appendicitis. Thus, our results were relevant to all types of acute appendicitis. However, the quality of these newly analyzed RCTs was low as only one RCT had a low risk of bias[12].
Meta-analysis is an increasingly popular method of data analysis to examine discrepancies in the literature. Nevertheless, there were some limitations in our research. First, the number of included RCTs was small, and, among those, two RCTs were also of small sample size. Funnel plots were not performed to assess the publication bias due to the small number of included RCTs. Second, the surgical techniques among the studies were varied; thus, there may be variances in operative time, conversion rate, and complications. Third, a cost analysis was not conducted in this research as cost is always higher with the development of a new technique and the instruments varied significantly with each study.
In conclusion, despite the limitations mentioned above, this review currently provides the best available evidence for comparison of single-incision laparoscopic appendectomy vs conventional laparoscopic appendectomy. From a curative perspective, SILA is comparable to CLA in terms of total complications, drain insertion, length of hospital stay, and postoperative pain. The disadvantages of SILA are a longer operative time and a higher conversion rate. One benefit of SILA is patient cosmetic satisfaction. Thus, the option of this new treatment alternative should be carefully discussed with patients. More RCTs are needed to clarify the benefits and disadvantages of SILA compared to CLA.
COMMENTS
Background
Appendectomy is one of the most commonly performed surgical procedures of the abdomen in the world. In recent years, minimally invasive surgery has rapidly developed and conventional laparoscopic appendectomy (CLA) has been widely used. In addition, single-incision laparoscopic appendectomy (SILA), as a new technique, has been introduced as an alternative to conventional three-port laparoscopic appendectomy.
Research frontiers
Both SILA and CLA are used for patients undergoing appendectomy. Many studies, including randomized controlled trials (RCTs), have compared SILA with CLA in the last few years. However, most have only demonstrated the feasibility and safety of SILA. The clinical benefits and disadvantages between SILA and CLA are still controversial.
Innovations and breakthroughs
The authors identified all RCTs comparing SILA with CLA. A meta-analysis and systematic review was conducted according to the Cochrane Handbook. From this study, the disadvantages of SILA were determined to be longer operative times and higher conversion rates, while the benefit of SILA was cosmetic satisfaction among patients. This has not been clearly identified in previous studies.
Applications
From a curative perspective, SILA is proven to be a safe and effective treatment that is comparable to CLA. Based on the benefits and disadvantages of SILA, surgeons should carefully assess each patient’s situation and discuss surgical options that meet their needs.
Peer review
This article is a good meta-analysis about single-incision laparoscopic appendectomy vs conventional laparoscopic appendectomy. The conclusions are unbiased and give good clues to the readers.
Footnotes
P- Reviewer Mentes O S- Editor Wen LL L- Editor A E- Editor Li JY
References
- 1.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 2.Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2010;(10):CD001546. doi: 10.1002/14651858.CD001546.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Bennett J, Boddy A, Rhodes M. Choice of approach for appendicectomy: a meta-analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech. 2007;17:245–255. doi: 10.1097/SLE.0b013e318058a117. [DOI] [PubMed] [Google Scholar]
- 4.Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS) J Gastrointest Surg. 2009;13:159–162. doi: 10.1007/s11605-008-0737-y. [DOI] [PubMed] [Google Scholar]
- 5.Chouillard E, Dache A, Torcivia A, Helmy N, Ruseykin I, Gumbs A. Single-incision laparoscopic appendectomy for acute appendicitis: a preliminary experience. Surg Endosc. 2010;24:1861–1865. doi: 10.1007/s00464-009-0860-1. [DOI] [PubMed] [Google Scholar]
- 6.Dapri G, Casali L, Dumont H, Van der Goot L, Herrandou L, Pastijn E, Sosnowski M, Himpens J, Cadière GB. Single-access transumbilical laparoscopic appendectomy and cholecystectomy using new curved reusable instruments: a pilot feasibility study. Surg Endosc. 2011;25:1325–1332. doi: 10.1007/s00464-010-1304-7. [DOI] [PubMed] [Google Scholar]
- 7.Saber AA, Elgamal MH, El-Ghazaly TH, Dewoolkar AV, Akl A. Simple technique for single incision transumbilical laparoscopic appendectomy. Int J Surg. 2010;8:128–130. doi: 10.1016/j.ijsu.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Ponsky TA, Diluciano J, Chwals W, Parry R, Boulanger S. Early experience with single-port laparoscopic surgery in children. J Laparoendosc Adv Surg Tech A. 2009;19:551–553. doi: 10.1089/lap.2009.0092. [DOI] [PubMed] [Google Scholar]
- 9.Garey CL, Laituri CA, Ostlie DJ, St Peter SD. Single-incision laparoscopic surgery and the necessity for prospective evidence. J Laparoendosc Adv Surg Tech A. 2010;20:503–506. doi: 10.1089/lap.2009.0394. [DOI] [PubMed] [Google Scholar]
- 10.Dutta S. Early experience with single incision laparoscopic surgery: eliminating the scar from abdominal operations. J Pediatr Surg. 2009;44:1741–1745. doi: 10.1016/j.jpedsurg.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 11.de la Torre RA, Satgunam S, Morales MP, Dwyer CL, Scott JS. Transumbilical single-port laparoscopic adjustable gastric band placement with liver suture retractor. Obes Surg. 2009;19:1707–1710. doi: 10.1007/s11695-009-9896-5. [DOI] [PubMed] [Google Scholar]
- 12.Teoh AY, Chiu PW, Wong TC, Poon MC, Wong SK, Leong HT, Lai PB, Ng EK. A double-blinded randomized controlled trial of laparoendoscopic single-site access versus conventional 3-port appendectomy. Ann Surg. 2012;256:909–914. doi: 10.1097/SLA.0b013e3182765fcf. [DOI] [PubMed] [Google Scholar]
- 13.Lee WS, Choi ST, Lee JN, Kim KK, Park YH, Lee WK, Baek JH, Lee TH. Single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy: a prospective randomized controlled study. Ann Surg. 2013;257:214–218. doi: 10.1097/SLA.0b013e318273bde4. [DOI] [PubMed] [Google Scholar]
- 14.Perez EA, Piper H, Burkhalter LS, Fischer AC. Single-incision laparoscopic surgery in children: a randomized control trial of acute appendicitis. Surg Endosc. 2013;27:1367–1371. doi: 10.1007/s00464-012-2617-5. [DOI] [PubMed] [Google Scholar]
- 15.St Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, Murphy JP, Andrews WS, Sharp RJ, Snyder CL, et al. Single incision versus standard 3-port laparoscopic appendectomy: a prospective randomized trial. Ann Surg. 2011;254:586–590. doi: 10.1097/SLA.0b013e31823003b5. [DOI] [PubMed] [Google Scholar]
- 16.Sozutek A, Colak T, Dirlik M, Ocal K, Turkmenoglu O, Dag A. A prospective randomized comparison of single-port laparoscopic procedure with open and standard 3-port laparoscopic procedures in the treatment of acute appendicitis. Surg Laparosc Endosc Percutan Tech. 2013;23:74–78. doi: 10.1097/SLE.0b013e3182754543. [DOI] [PubMed] [Google Scholar]
- 17.Frutos MD, Abrisqueta J, Lujan J, Abellan I, Parrilla P. Randomized prospective study to compare laparoscopic appendectomy versus umbilical single-incision appendectomy. Ann Surg. 2013;257:413–418. doi: 10.1097/SLA.0b013e318278d225. [DOI] [PubMed] [Google Scholar]
- 18.Gill RS, Shi X, Al-Adra DP, Birch DW, Karmali S. Single-incision appendectomy is comparable to conventional laparoscopic appendectomy: a systematic review and pooled analysis. Surg Laparosc Endosc Percutan Tech. 2012;22:319–327. doi: 10.1097/SLE.0b013e31824f2cf8. [DOI] [PubMed] [Google Scholar]
- 19.Lee JS, Choi YI, Lim SH, Hong TH. Transumbilical single port laparoscopic appendectomy using basic equipment: a comparison with the three ports method. J Korean Surg Soc. 2012;83:212–217. doi: 10.4174/jkss.2012.83.4.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pittman-Waller VA, Myers JG, Stewart RM, Dent DL, Page CP, Gray GA, Pruitt BA, Root HD. Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies. Am Surg. 2000;66:548–554. [PubMed] [Google Scholar]
- 21.Laituri CA, Fraser JD, Garey CL, Aguayo P, Sharp SW, Ostlie DJ, Holcomb GW, St Peter SD. Laparoscopic ileocecectomy in pediatric patients with Crohn’s disease. J Laparoendosc Adv Surg Tech A. 2011;21:193–195. doi: 10.1089/lap.2010.0169. [DOI] [PubMed] [Google Scholar]
- 22.Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc. 2010;24:1842–1848. doi: 10.1007/s00464-010-0887-3. [DOI] [PubMed] [Google Scholar]
- 23.Kim HJ, Lee JI, Lee YS, Lee IK, Park JH, Lee SK, Kang WK, Cho HM, You YK, Oh ST. Single-port transumbilical laparoscopic appendectomy: 43 consecutive cases. Surg Endosc. 2010;24:2765–2769. doi: 10.1007/s00464-010-1043-9. [DOI] [PubMed] [Google Scholar]
- 24.Lee SY, Lee HM, Hsieh CS, Chuang JH. Transumbilical laparoscopic appendectomy for acute appendicitis: a reliable one-port procedure. Surg Endosc. 2011;25:1115–1120. doi: 10.1007/s00464-010-1326-1. [DOI] [PubMed] [Google Scholar]
- 25.Park JH, Hyun KH, Park CH, Choi SY, Choi WH, Kim DJ, Lee S, Kim JS. Laparoscopic vs Transumbilical Single-Port Laparoscopic Appendectomy; Results of Prospective Randomized Trial. J Korean Surg Soc. 2010;78:213–218. [Google Scholar]
- 26.Silen W. Abdominal pain. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, et al., editors. Harrison’s Principles of Internal Medicine. 17th ed. New York City: McGraw-Hill; 2005. pp. 91–94. [Google Scholar]
- 27.Garg P, Thakur JD, Garg M, Menon GR. Single-incision laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg. 2012;16:1618–1628. doi: 10.1007/s11605-012-1906-6. [DOI] [PubMed] [Google Scholar]
- 28.Kang KC, Lee SY, Kang DB, Kim SH, Oh JT, Choi DH, Park WC, Lee JK. Application of single incision laparoscopic surgery for appendectomies in patients with complicated appendicitis. J Korean Soc Coloproctol. 2010;26:388–394. doi: 10.3393/jksc.2010.26.6.388. [DOI] [PMC free article] [PubMed] [Google Scholar]