Abstract
Context:
Coagulopathy frequently occurs following traumatic brain injury (TBI) and usually occurs 6-72 hour post-trauma. The incidence and the probable risk factors for development of coagulopathy and poor outcome following TBI are largely unknown and vary considerably.
Aims:
To assess the incidence and probable risk factors for development of coagulopathy and to identify the risk factors for poor outcome in terms of median survival time following TBI.
Materials and Methods:
In this prospective study over two years, patients of isolated moderate and severe traumatic brain injury (GCS≤12) admitted to trauma center had coagulation profile (PT, APTT, thrombin time, fibrinogen and D-dimer), arterial lactate and ABG analysis done on day of admission and on day three. Coagulopathy was defined as prothrombin time (PT) or/and activated partial thromboplastin time (APTT) more than 1.5 times the normal control. Incidence of in-hospital mortality was assessed in all cases.
Statistical Analysis:
A stepwise logistic regression analysis was performed to identify risk factors for coagulopathy and mortality in these patients.
Results:
A total of 208 patients were enrolled in the study. The mean age was 32 ± 12 years and mean GCS was 7.1 ± 2.8. Coagulopathy was present in 46% (n = 96) of patients. Risk factors for development of coagulopathy were found out to be severity of head injury (OR: 2.81), elevated D-dimer (OR: 3.43), low hemoglobin (OR: 3.13), and effaced cisterns in the CT scan (OR: 2.72). Presence of coagulopathy (OR: 2.97) and severity of head injury (OR: 5.70) strongly predicted poor outcome, and were associated with a decreased median survival time.
Conclusions:
There is a high incidence of coagulopathy following TBI. The presence of coagulopathy as well as of severity of TBI are strong predictors of in-hospital mortality in these patients.
Keywords: Coagulopathy, head trauma, outcome, prognosis, severity of head injury, traumatic brain injury
INTRODUCTION
Coagulation abnormalities frequently occur following TBI and the incidence of the disturbance in the coagulation parameters varies considerably.[1,2] Goodnight et al. first recognized that tissue thromboplastin, of which brain is a rich source, is released into the circulation resulting in uncontrolled activation of clotting factors leading to depletion of coagulation proteins, which may eventually result in disseminated intravascular coagulation characterized by systemic coagulopathy, intravascular coagulation and hemorrhage after the clotting factors are consumed.[3] Stein et al. found a strong association between severity of coagulopathy and density of intravascular coagulation.[4] This insult to hemostatic system is further aggravated by the infusion of large number of colloids, crystalloids and massive blood transfusion resulting in dilutional coagulopathy. Further, acidosis and hypothermia, which commonly follow traumatic injury, also add on to the hemostatic insult forming a vicious triad of coagulopathy, acidosis and hypothermia. Coagulopathy has a significant impact on morbidity and mortality of patients with TBI.[5] Mortality in patients with severe head injury with coagulopathy is found to be four times higher than in patients with head injury without any coagulopathy.[6] However, from the above literature, it is still unclear whether it is the development of coagulopathy or the severity of head injury, which predicts the poor survival for patients with traumatic brain injury (TBI).
In this study, we aim to assess the incidence of coagulopathy in patients with isolated TBI, the association of coagulopathy with prognostic outcome in addition to the correlation with CT scan findings and acidosis, if any, and to identify the probable risk factors for development of coagulopathy and the reasons for poor outcome following head trauma by estimating the median survival time in these cases.
MATERIALS AND METHODS
Two hundred and eight patients diagnosed with isolated head injury, admitted in department of Neurosurgery at a tertiary care trauma center from June 2008 to May 2010, were enrolled in this prospective cohort study. Isolated TBI was defined as patient presenting with moderate to severe traumatic brain injury (GCS ≤ 12) without injury to chest or abdomen or limbs. Exclusion criteria were a known history of any hemorrhagic disorder, patient on anticoagulant medications, patient with poly-trauma or associated long bone fractures, clinical evidence of brain death at the time of admission, any other severe co-morbidity, such as liver disease, diabetes mellitus, known history of hypertension, which is likely to influence outcome.
All patients underwent detailed clinical evaluation followed by categorization into moderate and severe head injury group on the basis of Glasgow Coma Scale (GCS). Subsequent relevant laboratory investigations were carried out such as Prothrombin Time (PT)/INR, activated Partial Thromboplastin Time (APTT), Thrombin Time (TT), Plasma fibrinogen level, D-dimer level, Platelet count, ABG analysis, Arterial Lactate level and Hemoglobin concentration on the day of admission and subsequently on day three. Coagulopathy in this study was defined as Prothrombin time (PT) > 18.0 s or/and Activated Partial Thromboplastin Time (APTT) > 48 s (> 1.5 times of the laboratory control). Laboratory control was calculated using fifty healthy individuals (equal numbers of males and females of different age groups). Control PT was 13.7 s and APTT was 32 s.
Acidosis was defined as arterial blood pH < 7.3 and arterial blood HCO3 < 20 mEq/L. DIC score according to ISHT criteria[7] were calculated on the basis of these coagulation parameters. The patients were kept under a constant follow-up for the period of his/her hospital stay to assess the outcome, whether, discharged after recovery or died. The study was approved by the ethics committee of All India Institute of Medical Sciences (AIIMS).
Data entry was done using Microsoft Excel 2007. Analysis was done using Stata 9.1 (College Station, Texas, US). All the descriptive analysis was done for each variable under study. The data were presented as mean with SD for continuous variables such as PT, APTT, TT, Fibrinogen, Hb, Platelet count, Arterial lactate level etc. For categorical variables such as Sex, D-dimer levels Acidosis, DIC score etc., data were presented as frequency and percentages. Categorical variables were compared between the groups using Chi-Square/Fischer's exact test, whichever applicable. The continuous variables were analyzed between groups using Student's t-test/Wilcoxon rank-sum test, whichever applicable. Logistic regression were used to calculate the Odds Ratio (OR), and multivariate logistic regression were applied to those variables which were found significant in bivariate logistic regression (P < 0.05). For survival analysis, Log rank test and Kaplan-Meir survival analysis were used to find out the significant difference, if any, in median survival time in the context of different parameters. Results were considered significant at P < 0.05.
RESULTS
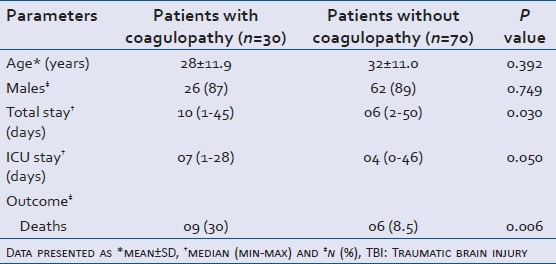
A total of 208 patients of isolated head injury presenting to the apex trauma center were included in the study and were further categorized into moderate and severe head injury on the basis of GCS. The patients with GCS 3-8 were categorized as Severe Head injury (n = 108) and patients with GCS 9-12 were categorized as moderate head injury (n = 100). The cases of head injury had been in the age range of 4-70 years. Males comprised 89% of the total study population and the mean age of the study population was 32 ± 11 years. Coagulopathy as defined in the methodology above was present in 96 (46%) patients, irrespective of the severity of head trauma. Among severe head injury (GCS 3-8) group, 66 (61%) patients out of 108 developed coagulopathy and in moderate head injury group 30 (30%) patients out of 100 developed coagulopathy (Baseline parameters of the two groups are shown in Tables 1 and 2).
Table 1.
Association of demographic parameters, hospital stay and in-house mortality severe TBI in presence or absence of coagulopathy
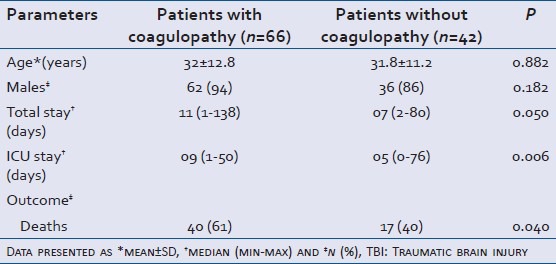
Table 2.
Association of demographic parameters, hospital stay and in-house mortality moderate TBI in presence or absence of coagulopathy
The most common intracranial lesion in the study subjects in decreasing order of frequency were contusion, hemorrhage, midline shift, intracranial fracture, effaced cisterns and diffuse axonal injury. Out of these, effaced cistern in the CT scan was found to have association with development of coagulopathy (P = 0.02).
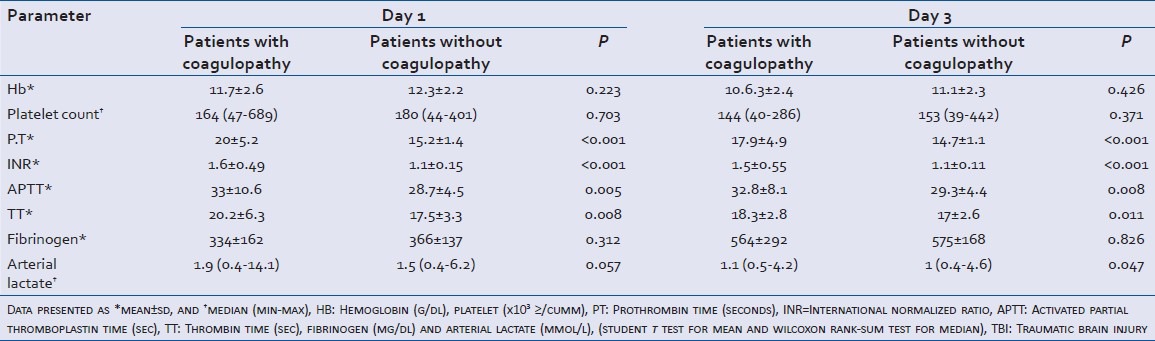
Patients with coagulopathy in both the subgroups were found to have significantly increased PT, INR, APTT and thrombin time at the time of admission and also on third day of admission [Tables 3 and 4]. Acidosis was also found to be associated with development of coagulopathy significantly (P = 0.042).
Table 3.
Association of laboratory parameters in severe TBI in presence and absence of coagulopathy
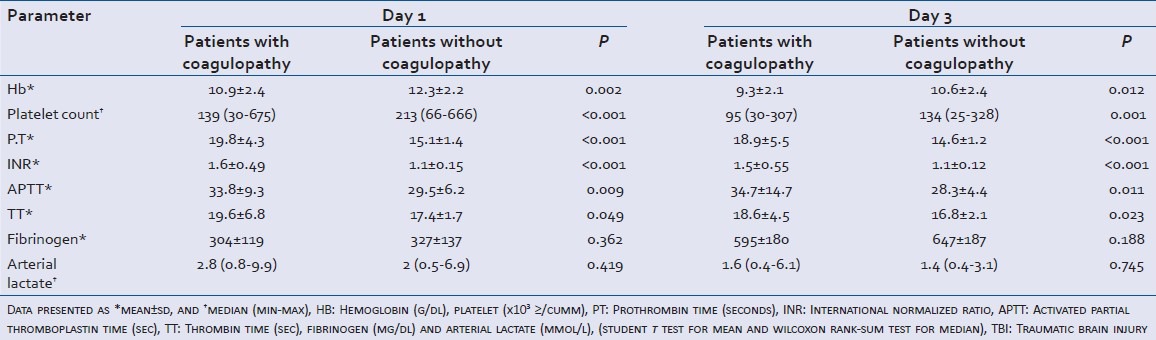
Table 4.
Association of laboratory parameters in moderate TBI in presence and absence of coagulopathy
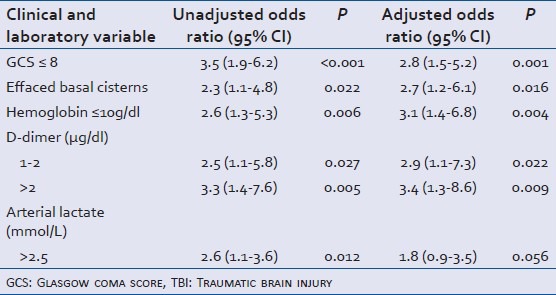
Bivariate analysis was carried out to identify the risk factors associated with the development of coagulopathy [Table 5]. On bivariate analysis, severity of TBI, effaced basal cisterns on CT scan, low hemoglobin level, elevated D-dimer level at admission, and elevated arterial lactate level were found to predict the development of coagulopathy. However, on multivariate logistic regression analysis, only severity of head injury (GCS ≤ 8), effaced basal cisterns on CT scan, hemoglobin < 10 g/dl and D-dimer > 1 μg/dl were found to predict the development of coagulopathy independently.
Table 5.
Risk factors for development of coagulopathy (96 out of 208) following isolated TBI
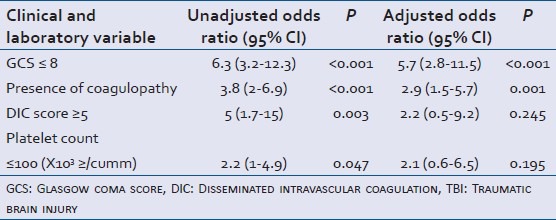
Similar analysis was carried out to predict the risk factors associated with poor outcome following TBI [Table 6]. On bivariate analysis, severity of head injury (GCS ≤ 8), presence of midline shift, decreased platelet count at admission, presence of coagulopathy, DIC score greater than 5, presence of acidosis and undergoing surgery was associated with poor outcome. However, on multivariate logistic regression. severity of head injury and presence of coagulopathy were found to predict the poor outcome following head injury independently.
Table 6.
Risk factors associated with poor outcome (72 out of 208) following isolated TBI
Kaplan-Meier curves against the length of hospital stay were used to estimate the median survival time. The median survival time for various parameters such as GCS scores, presence or absence of coagulopathy, thrombin time, platelet count, D-dimer levels, DIC score ≥ and < 5, presence or absence of acidosis at admission, blood products (RBC, FFP, Platelet) transfusion, CT findings (contusion, fracture, intracranial bleeding, cisterns effaced, midline shift), arterial lactate levels of > and < 2.5 were calculated using log rank test, and Kaplan-Meier survival analysis curves were prepared for significant variable. P < 0.05 was taken as significant [Table 7 and Figures 1-4].
Table 7.
Kaplan Meir analysis for median survival time following isolated TBI
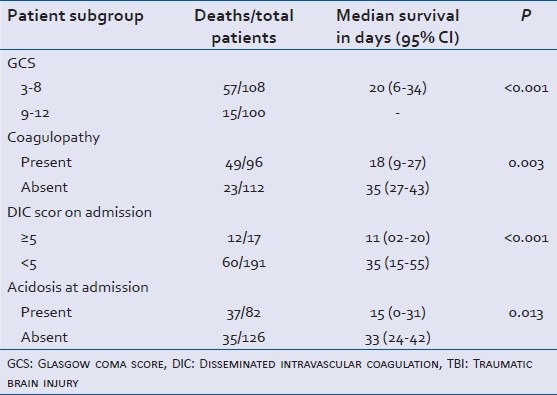
Figure 1.
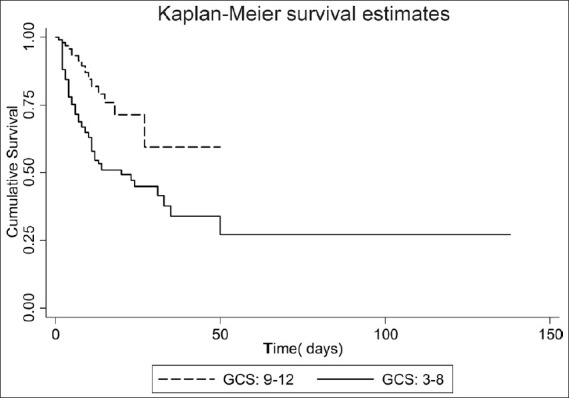
Kaplan-Meier survival estimate by GCS. Log rank P ≤ 0.001
Figure 4.
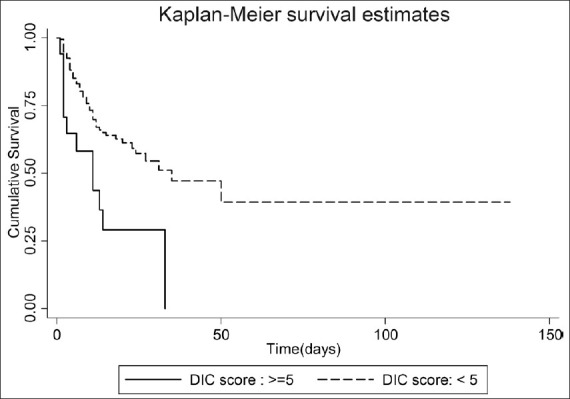
Median survival estimate by DIC Score ≥ 5. Log rank P ≤ 0.001
Figure 2.
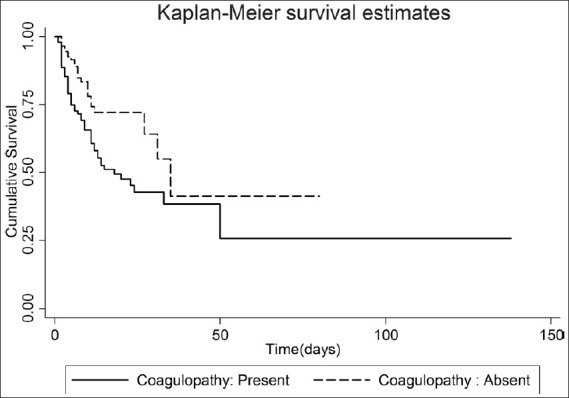
Kaplan-Meier survival estimate by coagulopathy. Log rank P = 0.003
Figure 3.
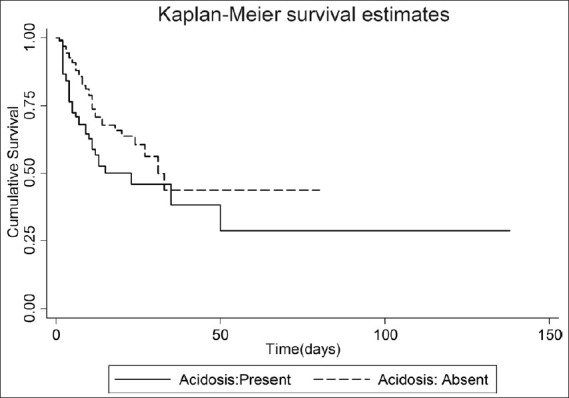
Kaplan-Meier survival estimate by acidosis. Log rank P = 0.01
The result of the curves show that the patients with GCS score ≤ 8 with coagulopathy, having DIC score ≥ 5 and who have developed acidemia following head injury died early during the hospital stay [Figures 1-4]. The median survival time was lowest for patients who developed acidemia and had a DIC score ≥ 5 (1 and 2 days, respectively).
DISCUSSION
This is one of the large series of patients with isolated TBI which has looked into the prognostic factors like coagulopathy and severity of TBI. Coagulopathy frequently occurs following head injury and is a well recognized confounding phenomenon. If this coagulative derangement is severe, this coagulopathy may disseminate resulting in deposition of thrombi in microvasculature and activation of fibrinolysis leading to development of DIC and uncontrollable bleeding.[8,9]
In the present study, the prevalence of coagulopathy was found to be 46%, irrespective of the severity of brain injury. In the literature the incidence of coagulopathy varies considerably among different studies. The reported incidence ranges between 10 and 97%.[10,11,12,13,14,15] This wide variation in incidence among various studies could be attributed to different criteria used by different authors to define coagulopathy (as no standard definition is available so far), varying inclusion criteria, and varying severity of the head trauma among different studies.
Release of tissue factor from the injured brain cortex is implicated in development of coagulopathy following TBI. This tissue factor released from the brain activates the extrinsic coagulation pathway leading to increased consumption of clotting factors and development of coagulopathy. Also the exposure of negatively charged collagen vascular layer contributes to activation of coagulation pathway by stimulating the intrinsic pathway. This was evident in the present study from a significant increase in PT, INR, and APTT on day one and three of admission among patients who developed coagulopathy in comparison to patients who did not develop coagulopathy following TBI. Findings of the present study are similar to as reported by Bayer, Kalkan et al. who in their study on 62 patients of isolated head trauma, found a prolonged mean PT and APTT within first three hours of head injury.[16] Similar findings were also reported by Stein, Spettell et al. They reported that mean PT and PTT at admission were significantly longer in patients developing delayed brain injury.[17] A recent study by Talving, Benfield et al. on 436 patients also supported the results of this study. Greuters et al. in their study including 107 patients have reported significantly increased mean PT and APTT following head injury.[18] Not many studies are available that had assessed TT with TBI. Neither TT has been found to be associated with development of coagulopathy. In contrast, our study shows that TT was significantly prolonged among the patients who developed coagulopathy both on day one and day three. This study supports the findings of Vecht et al. who also reported the prolongation of TT following head injury;[19] although, Auer L in his study on thirty patients did not find any significant changes in thrombin time.[20]
Plasma fibrinogen concentration was found to be significantly lower among the patients who developed coagulopathy at admission, however it showed a steep rise on the subsequent days. D-dimer levels were significantly elevated in patients who developed coagulopathy indicating the activation of the fibrinolytic system. Olson et al. and Antovic et al.[21] in their study also reported similar results.
To add, to the best of our knowledge very few studies have mentioned the risk factors associated with the development of coagulopathy. In this study, severity of head injury (GCS ≤ 8), D-dimer level of more than 1 mg/dl, arterial lactate level of more than 2.5 mmol/L, effaced cisterns on CT scan and hemoglobin level less than 10 g/dl strongly predicted the development of coagulopathy. Talving et al. had also reported GCS ≤ 8 and presence of cerebral edema, SAH, SBP < 90 mm Hg, midline shift as the factors, which independently predicted development of coagulopathy. Similar findings were also reported by Affonseca et al.[22] in their study on pediatric patients where they found severity of head injury, presence of brain swelling, and injuries to chest and abdomen being associated with the development of coagulopathy.
In this study the development of coagulopathy following severe isolated head injury was associated with longer ICU stay, although coagulopathy did not bear any impact on the length of the total hospital stay. Similar findings were reported by Talving et al.
The overall mortality in the present study was 72 (35%). Patients with coagulopathy were found to be significantly associated with poor survival as compared to patients who did not develop coagulopathy as shown in Table 1. Development of coagulopathy and severity of head trauma (GCS ≤ 8) independently predicted poor outcome. The result is similar to the findings reported by Macleod et al. who in 7638 patients found presence of coagulopathy and GCS ≤ 8 as the predictors for poor outcome.[23] Olson et al. reported decreased GCS, elevated DIC score and increased fibrin degradation product as independent predictors for poor outcome. Peep Talving et al. also found coagulopathy to be independent risk factor for mortality. However the finding of our study was contrary to findings of Affonseca et al. who found coagulopathy following TBI was not associated with increase in mortality. This difference in results may be probably attributed to the fact that our definition for coagulopathy was based on firm criteria, which very few studies comply with. Also we had controlled other factors such as severity of head trauma, presence or absence of other injuries etc., which could affect the outcome. In this study, the Kaplan-Meier survival curves show that the patients who developed coagulopathy with DIC score > 5 along with the severity of head injury died early during their stay in the hospital. This finding is consistent with the findings by Macleod et al., who also reported a decreased median survival for the patients who developed coagulopathy. These findings support the results of Kumara et al.[24] and other,[20,23] who have reported that coagulopathy is predictor for poor outcome.
In spite of the best efforts to tighten all the loose ends, our study has some limitations since we did not take into account the soft tissue injuries, which could have also possibly triggered the coagulation cascade. Sepsis, which is commonly present in traumatic injury patients is associated with decreased protein C levels, and this decreased protein C has also been implicated in the mechanism of coagulopathy.[14] The strength of present study is the large number of cases, extensive review of all the routine haemostatic parameters following head trauma and analysis of several possible risk factors for the development of coagulopathy with identification of the factor predicting poor outcome following isolated TBI.
CONCLUSION
The present study leads to conclusion that coagulopathy occurs frequently following TBI. Presence of coagulopathy as well as severity of head injury are two strong predictors of in-hospital mortality in these patients and is associated with decreased median survival. The risk factors for development of coagulopathy include severity of head injury and elevated D-dimer concentration at admission. On the basis of our findings, we emphasize prompt diagnosis and management of trauma-induced coagulopathy in patients with TBI.
ACKNOWLEDGMENT
Prof. R.M Pandey and Mr. Ashish Upadhyay for doing statistical analysis for this study, ICMR for funding the project and the technical staff of laboratory medicine, JPNATC, for their technical support.
Footnotes
Source of Support: This project was funded by ICMR (Indian Council of Medical Research).
Conflict of Interest: None declared.
REFERENCES
- 1.Harhangi BS, Kompanje EJO, Leebeek FW, Maas AI. Coagulation disorders after traumatic brain injury. Acta Neurochir. 2008;150:165–75. doi: 10.1007/s00701-007-1475-8. [DOI] [PubMed] [Google Scholar]
- 2.Talving P, Benfield R, Hadjizacharia P, Inaba K, Chan LS, Demetriades D. Coagulopathy in severe traumatic brain injury: A prospective study. J Trauma. 2009;66:55–61. doi: 10.1097/TA.0b013e318190c3c0. [DOI] [PubMed] [Google Scholar]
- 3.Goodnight SH, Kenoyer G, Rapaport SI, Patch MJ, Lee JA, Kurze T. Defibrination after brain-tissue destruction: A serious complication of head injury. N Engl J Med. 1974;290:1043–7. doi: 10.1056/NEJM197405092901903. [DOI] [PubMed] [Google Scholar]
- 4.Stein SC, Chen XH, Sinson GP, Smith DH. Intravascular coagulation: A major secondary insult in nonfatal traumatic brain injury. J Neurosurg. 2002;97:1373–7. doi: 10.3171/jns.2002.97.6.1373. [DOI] [PubMed] [Google Scholar]
- 5.Lapointe LA, Von Rueden KT. Coagulopathies in trauma patients. AACN Clin Issues. 2002;13:192–203. doi: 10.1097/00044067-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Bellamy RF, Maningas PA, Vayer JS. Epidemiology of trauma: Military experience. Ann Emerg Med. 1986;15:1384–8. doi: 10.1016/s0196-0644(86)80920-9. [DOI] [PubMed] [Google Scholar]
- 7.Taylor FB, Jr, Toh CH, Hoots WK, Wada H, Levi M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86:1327–30. [PubMed] [Google Scholar]
- 8.Bredbacka S, Blombäck M, Wiman B, Pelzer H. Disseminated intravascular coagulation in neurosurgical patients: Diagnosis by new laboratory methods. J Neurosurg Anesthesiol. 1992;4:128–33. doi: 10.1097/00008506-199204000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Stein SC, Smith DH. Coagulopathy in traumatic brain injury. Neurocrit Care. 2004;1:479–88. doi: 10.1385/NCC:1:4:479. [DOI] [PubMed] [Google Scholar]
- 10.Miner ME, Kaufman HH, Graham SH, Haar FH, Gildenberg PL. Disseminated intravascular coagulation fibrinolytic syndrome following head injury in children: Frequency and prognostic implications. J Pediatr. 1982;100:687–91. doi: 10.1016/s0022-3476(82)80565-9. [DOI] [PubMed] [Google Scholar]
- 11.Olson JD, Kaufman HH, Moake J, O’Gorman TW, Hoots K, Wagner K, et al. The incidence and significance of hemostatic abnormalities in patients with head injuries. Neurosurgery. 1989;24:825–32. doi: 10.1227/00006123-198906000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Selladurai BM, Vickneswaran M, Duraisamy S, Atan M. Coagulopathy in acute head injury--a study of its role as a prognostic indicator. Br J Neurosurg. 1997;11:398–404. doi: 10.1080/02688699745880. [DOI] [PubMed] [Google Scholar]
- 13.Kearney TJ, Bentt L, Grode M, Lee S, Hiatt JR, Shabot MM. Coagulopathy and catecholamines in severe head injury. J Trauma. 1992;32:608–11. doi: 10.1097/00005373-199205000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Cohen MJ, Brohi K, Ganter MT, Manley GT, Mackersie RC, Pittet JF. Early coagulopathy after traumatic brain injury: The role of hypoperfusion and the protein C pathway. J Trauma. 2007;63:1254–61. doi: 10.1097/TA.0b013e318156ee4c. [DOI] [PubMed] [Google Scholar]
- 15.Kaufman HH, Hui KS, Mattson JC, Borit A, Childs TL, Hoots WK, et al. Clinicopathological correlations of disseminated intravascular coagulation in patients with head injury. Neurosurgery. 1984;15:34–42. doi: 10.1227/00006123-198407000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Bayir A, Kalkan E, Koçak S, Ak A, Cander B, Bodur S. Fibrinolytic markers and neurologic outcome in traumatic brain injury. Neurol India. 2006;54:363–5. doi: 10.4103/0028-3886.28106. [DOI] [PubMed] [Google Scholar]
- 17.Stein SC, Spettell C, Young G, Ross SE. Delayed and progressive brain injury in closed-head trauma: Radiological demonstration. Neurosurgery. 1993;32:25–30. doi: 10.1227/00006123-199301000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Greuters S, van den Berg A, Franschman G, Viersen VA, Beishuizen A, Peerdeman SM, et al. Acute and delayed mild coagulopathy are related to outcome in patients with isolated traumatic brain injury. Crit Care. 2011;15:R2. doi: 10.1186/cc9399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vecht CJ, Sibinga CT, Minderhoud JM. Disseminated intravascular coagulation and head injury. J Neurol Neurosurg Psychiatr. 1975;38:567–71. doi: 10.1136/jnnp.38.6.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Auer L. Disturbances of the coagulatory system in patients with severe cerebral trauma. I. Acta Neurochir. 1978;43:51–9. doi: 10.1007/BF01809225. [DOI] [PubMed] [Google Scholar]
- 21.Jovan A, Milorad B, Goran I, Zoran M, Stojanka D, Jovan T, et al. Blood coagulation and fibrinolysis parameter changes after various types of brain damage. Med Biol. 1998;5:44–9. [Google Scholar]
- 22.Affonseca CA, Carvalho LF, Guerra SD, Ferreira AR, Goulart EM. Coagulation disorder in children and adolescents with moderate to severe traumatic brain injury. J Pediatr. 2007;83:274–82. doi: 10.2223/JPED.1639. [DOI] [PubMed] [Google Scholar]
- 23.MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma. 2003;55:39–44. doi: 10.1097/01.TA.0000075338.21177.EF. [DOI] [PubMed] [Google Scholar]
- 24.Kumura E, Sato M, Fukuda A, Takemoto Y, Tanaka S, Kohama A. Coagulation disorders following acute head injury. Acta Neurochir. 1987;85:23–8. doi: 10.1007/BF01402365. [DOI] [PubMed] [Google Scholar]


