Abstract
Sleep disturbances are core symptoms of posttraumatic-stress disorder (PTSD), yet they bear less stigma than other PTSD symptoms. Given the growing number of returning military veterans, brief, valid assessments that identify PTSD in a minimally stigmatizing way may be highly useful in both research and clinical practice. The Pittsburgh Sleep Quality Index Addendum for PTSD (PSQI-A) was examined for the ability to identify cases of PTSD among male military veterans. Male military veterans (N = 119) completed the PSQI-A, as well as measures of sleep quality, combat exposure, posttraumatic stress, depression, and anxiety. Veterans with PTSD had higher PSQI-A identified disruptive nocturnal behaviors than veterans without PTSD. The PSQI-A had good internal consistency and had convergent validity with sleep quality, combat exposure, PTSD symptoms, depression, and anxiety. A cutoff score ≥ 4 provided an area-under-the-curve = .81, with 71% sensitivity, 82% specificity, and 60% positive and 83% negative predictive value for a clinical diagnosis of PTSD; correct classification was 74%. The PSQI-A is a valid measure to possibly detect PTSD among male military veterans without directly probing trauma reactions. Assessment of disruptive nocturnal behaviors may provide a cost-effective, non-stigmatizing approach to PTSD screening among male military veterans.
Keywords: Nightmares, Psychometric, Trauma, Military, Combat, PTSD
INTRODUCTION
There are currently 22.6 million United States military veterans (U.S. Census Bureau, 2010). As reported by the Veterans Health Study, approximately 20% of Veterans Affairs patients meet criteria for posttraumatic stress disorder (PTSD [Spiro, Hankin, Mansell, & Kazis, 2006]). Currently, approximately two million United States military personnel have served in Iraq and Afghanistan while engaged in Operations Iraqi / Enduring Freedom or Operation New Dawn. Upon return from Iraq and Afghanistan, 11.5%-18.9% of veterans experience posttraumatic stress symptoms (Hoge et al., 2004). Among Army and National Guard Personnel, the prevalence of posttraumatic stress disorder (PTSD) and depression may be as high as 26.3% to 33.2%. These psychiatric conditions are also comorbid with high rates of alcohol misuse, aggression, and other problem behaviors (Thomas et al., 2010).
Mental health treatment and health care utilization among returning military veterans are currently high priorities for those who provide care for veterans (see: [(Hoge et al., 2006; Milliken et al., 2007; Ramchand et al., 2010)]). However, the stigma associated with mental health disorders in military personnel is well recognized (Vogt, 2011), and significantly impedes enrollment into and compliance with adequate mental health care (Hoge et al., 2006). Although the Department of Defense conducts pre- and post-deployment mental health assessments with military personnel, there is some suspicious that these may be associated with stigma despite their brief and confidential nature. For example, among an Army infantry brigade, reports of psychological disturbances were 2- to 4-fold higher on an anonymous survey compared to the non-anonymous routine mental health assessment (Warner et al., 2011). Thus, it is imperative to develop non-stigmatizing assessment measures that can facilitate the rapid identification of returning military personnel who may be in need of mental health care. The assessment of sleep disturbances may provide a unique route to meet this complicated demand.
Sleep disturbances are a core feature of PTSD (see reviews [(Ross et al., 1989; Spoormaker & Montgomery, 2008; Babson & Feldner, 2010)]), and increase concurrently with PTSD severity (Germain, Buysse, Shear, Fayyad, & Austin, 2004). The American Psychiatric Association DSM-IV-TR diagnostic criteria for PTSD identifies sleep disturbance as a contributor to the PSTD symptoms of re-experiencing (e.g. nightmares), as well as hyperarousal (e.g. difficulty falling or staying asleep) (American Psychiatric Association, 2000). Additional disruptive nocturnal behaviors that are associated with PTSD include nocturnal panic attacks, awakenings with startle or panic, and thrashing movements (Mellman, Kulick-Bell, Ashlock, & Nolan, 2003; Sheikh, Woodward, & Leskin, 2003). Prospective studies have indicated that both subjective and objective sleep disturbances following trauma exposure predict the subsequent development of PTSD in civilians and military samples (Mellman et al., 2002; Koren et al., 2002). Conversely, the presence of sleep complaints prior to trauma exposure heightens the risk of subsequently developing PTSD or other stress-related psychiatric disorders (Bryant, Creamer, O’Donnell, Silove, & McFarlane, 2010).
Sleep disturbance is a well known risk factor that adversely affects mental health (Breslau, Roth, Rosenthal, & Andreski, 1996). Military personnel in particular, demonstrate increased sleep disturbances during and following their deployment (Capaldi, Guerrero, & Killgore, 2011; Seelig et al., 2010). Insomnia is a sleep disturbance that is frequently experienced among military personnel following their deployment, with rates that reach approximately 41% (McLay, Klam, & Volkert, 2010). Insomnia immediately following deployment is particularly concerning because it has been associated with increased PTSD severity three months later (McLay et al., 2010; Wright et al., 2011).
The co-occurrence of post-deployment sleep disturbances with mental health problems is acknowledged and has led to the inclusion of sleep assessment in post-deployment mental health screening procedures (Bliese, Wright, Adler, Hoge, & Prayner, 2005; Bliese, Wright, Alder, & Thomas, 2006). When assessment of sleep disturbances is added to mental health screening procedures, the ability to detect individuals in need of mental health care is increased (Bliese et al., 2005). According to the U.S. Army Medical Research Unit-Europe, “Sleep problems also may have less stigma than other mental health problems and may serve as a socially acceptable conduit to mental health services.” (Wright, Adler, Bliese, & Eckford, 2008, p. 414). Together, these observations suggest that the assessment of sleep disturbances may be an efficacious, and military-relevant, mode for entry into mental health care services.
The Pittsburgh Sleep Quality Index-Addendum for PTSD (PSQI-A) is a seven-item self-report questionnaire that can be used to examine the frequency of seven disruptive nocturnal behaviors that are common to PTSD among adults (Germain et al., 2005). This instrument has been validated among female sexual assaults survivors (Germain et al., 2005) and has been used among earthquake survivors and military veterans (Farrahi, Nakhaee, Sheibani, Garrusi, & Amirkafi, 2009; Jetović et al., 2011; Insana, Kolko, & Germain, under review). However, the psychometric properties of the PSQI-A have not been evaluated among military veterans. Thus, the purpose of the current study was to evaluate the psychometric properties of the PSQI-A, and more specifically, to assess its ability to identify PTSD among male military veterans.
METHOD
The current study is a secondary analysis of data that were collected for projects that investigated the neural correlates and effects of sleep treatments among military veterans (R34 MH-080696-01, R21 MH-083035-01, PR054093, and PT073961). All projects were approved by the institutional review board at the University of Pittsburgh. Informed consent was obtained from all participants prior to each project procedures.
Participants
Participants in the current study were a convenience sample of 119 military veterans who were recruited from community advertisements via local television and radio commercials, newspaper advertisements, bus signs, and flyers. For the current analyses, participants were ≥ 18 years old, were exclusively men, were medically stable, and were free from current (past three months) substance abuse, free from lifetime psychotic or bipolar disorder, and free from sleep-disordered breathing—as determined by a sleep disorders screening study.
Measures
Pittsburgh Sleep Quality Index-Addendum for PTSD (PSQI-A)
The PSQI-Addendum (PSQI-A) was used to identify disruptive nocturnal behaviors that are characteristic to PTSD (Germain et al., 2005). The PSQI-A is comprised of seven different sleep disturbance items that are commonly reported by adults with PTSD (e.g., hot flashes, memories or nightmares of the traumatic experience, and episodes of terror during sleep). Items are rated on a 0 (not in the past month) to 3 (three or more times a week) point scale, and can be summed to create a total score. The total scores can range from 0 (normal) to 21 (severe). Based on the initial validation study, total scores ≥ 4 can be used to identify participants with PTSD (Germain et al., 2005). The PSQI-A has a sensitivity and specificity of 94% and 82% respectively (Germain et al., 2005).
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI) was used to determine sleep quality from the previous month (Buysse et al., 1989). The PSQI is comprised of 18 items that yield seven component scores. Component scores are summed to create a total score. The total score can range from 0 (better) to 21 (worse). PSQI scores ≤ 5 are associated with good sleep quality, whereas scores > 5 are associated with poor sleep quality. The PSQI has a sensitivity and specificity of 89.6% and 86.5% respectively (Buysse et al., 1989).
Structured Clinical Interview for Axis I, and Sleep Disorders
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) was used to for the assessment of clinical diagnoses (First, Spitzer, Gibbon, & Williams, 1995). The SCID has high sensitivity, specificity, and positive and negative predictive value across diagnoses (Ramirez Basco et al., 2000). The SCID typically has good inter-rater reliability with an average Kappa of 0.71 (Lobbestael, Leurgans, & Arntz, 2011). The Structured Interview for Sleep Disorders (SIS-D) according to DSM-III-R was used to for the assessment of insomnia diagnosis (Schramm et al., 1993). The SIS-D typically has high inter-rater reliability of 97% agreement (Schramm et al., 1993).
Clinician-Administered PTSD Scale
Current PTSD diagnosis and symptomatology was determined with the Clinician-Administered PTSD Scale (CAPS) (Blake et al., 1990) according to the 1-2 scoring rules (Weathers et al., 1999). The CAPS is a structured interview that is comprised of 17-symptom questions. Symptom questions form three symptom clusters that are each described by a severity score. The CAPS symptom clusters have good internal consistency (range α = 0.85-0.87) (Blake et al., 1995). The CAPS has a sensitivity and specificity of 74% and 84%, respectively (Hovens et al., 1994). The CAPS was administered by certified assessors. Inter-rater reliability among assessors was kappa = 0.98.
Combat Exposure Scale
The Combat Exposure Scale (CES) was used to determine combat exposure severity (Keane et al., 1989). The CES is a self-report measure that comprises seven likert items that describe severity of combat experience, each scaled from one (No) to five (≥ 51 times). The total CES score can range from 0 (less combat exposure) to 41(more combat exposure). The CES has good internal consistency Cronbach’s α = .85, test-retest reliability r = .97, and previously discriminated (p < .005) between PTSD and non-PTSD combat-exposed veterans (Keane et al., 1989).
Beck Depression Inventory
The Beck Depression Inventory (BDI) was used to determine depression symptoms within the past week (BECK et al., 1961). The BDI is a 21-item self-report measure that describes depressive symptoms. BDI items are scaled from 0 (lower intensity) to 3 (higher intensity). Items are summed to create total scores that can range from 0 (minimal depression) to 63 (severe depression). The BDI can discriminate between depressed and non-depressed samples (Salkind, 1969) and has high internal consistency Cronbach’s α = 0.80 (BECK et al., 1961).
Beck Anxiety Inventory
The Beck Anxiety Inventory (BAI) was used to determine anxiety symptoms within the past week (BECK et al., 1988). The BAI is a 21-item self-report measure that describes anxiety symptoms. BAI items are scaled from 0 (not at all) to 3 (severely). Items are summed to create total scores that can range from 0 (minimal anxiety) to 63 (severe anxiety). The BAI has high test-retest reliability r = 0.75, and high internal consistency Cronbach’s α = 0.92 (BECK et al., 1988).
Statistical Analyses
Chi-square analysis and Student’s t-test comparisons were calculated to examine differences in demographic characteristics among veterans with and without PTSD, as defined by the CAPS. Analyses of covariance were used to control for age while examining the differences among veterans with and without PTSD on their experiences of disruptive nocturnal behaviors, sleep quality, combat exposure, PTSD symptomatology, depression, and anxiety. Hedge’s g effect sizes for unequal sample sizes were calculated among comparisons (small = .20–.30; medium = >.30–.80; large = >.80 [(Cohen, 1988)]). Cronbach’s α coefficient was calculated to examine PSQI-A inter-item internal consistency. Partial correlations were calculated to control for age to examine the PSQI-A associations with sleep quality, combat exposure, PTSD symptoms, depression, and anxiety. A receiver operating characteristic (ROC) analysis was conducted to examine sensitivity, specificity, both positive and negative predictive value, and correct classification of the PSQI-A to detect PTSD among the current military veteran sample. Both positive and negative likelihood ratios were also calculated to assess the value of the PSQI-A to detect PTSD among the current sample.
Age was controlled during analyses of internal consistency and correlations. Where indicated, PTSD associated sleep items were removed from the CAPS (“Difficulty falling or staying asleep,” and “Nightmares”), and the BDI (“Sleeps Less” and “Tired”).
RESULTS
Veterans served in the Army (70.6%), Navy (14.3%), Marines (9.2%), and Air Force (5.9%). Veterans were deployed to combat theatres that included Operation Iraq/Enduring Freedom (68.1%), Persian Gulf War (10.1%), Vietnam (9.2%), a different peace keeping mission (5.9%), or were not exposed to combat (6.7%). The most frequently observed current psychiatric conditions included Insomnia (56.3%), Posttraumatic Stress Disorder (55.5%), Major Depressive Disorder (11.8%), Adjustment Disorder (9.2%), and Anxiety Disorder (5.0%). The most frequently observed past psychiatric conditions included Alcohol use Disorder (51.3%), Major Depressive Disorder (50.4%), PTSD (27.7%), Specific Phobia (19.3%), and Cannabis Use Disorder (19.3). Veterans with PTSD (n = 41; age M = 34.3, SD = 10.7 years) were younger than veterans without PTSD (n = 78; age M = 40.1, SD = 12.9 years), t = 2.36, p = 0.02, g = 0.47. Veterans with PTSD (92.1% White, 5.3% Black, 2.6% Asian) did not ethnically differ from veterans without PTSD (84.1% White, 15.9% Black), X2 = 4.3, p = 0.11. Veterans without PTSD had missing data on the BDI (n = 2), and BAI (n = 9). Veterans with PTSD had missing data on the PSQI (n = 2), CES (n = 7), and BDI (n = 3). Analyses were conducted on all available data.
Descriptive statistics: Clinical Measures
Descriptive statistics and comparisons among veterans who did and did not meet PTSD diagnostic criteria are shown in Table 1. As expected, veterans with PTSD had worse PTSD symptoms, and also endorsed more frequent disruptive nocturnal behaviors, more combat exposure, and worse sleep quality compared to veterans without PTSD.
Table 1.
Descriptive statistics and comparisons among participants who were and were not clinically diagnosed with having PTSD while controlling for age.
| Total N = 119 | Without PTSD n = 78 | With PTSD n = 41 | Difference | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Variable | M (SD) | M (SD) | M (SD) | F | df | g |
| PSQI-A | 3.18 (3.15) | 2.03 (2.40) | 5.37 (3.28) | 40.16*** | 1, 117 | 1.21 |
| A: Hot flashes | 0.21 (0.62) | 0.13 (0.52) | 0.37 (0.77) | 4.02* | 1, 117 | 0.38 |
| B: Nervousness | 0.75 (0.96) | 0.53 (0.83) | 1.15 (1.06) | 11.80*** | 1, 117 | 0.67 |
| C: Traumatic memories |
0.66 (0.84) | 0.33 (0.57) | 1.29 (0.90) | 50.05*** | 1, 117 | 1.35 |
| D: Anxiety or panic |
0.33 (0.60) | 0.17 (0.44) | 0.63 (0.73) | 18.91*** | 1, 117 | 0.81 |
| E: Bad dreams | 0.64 (0.85) | 0.51 (0.79) | 0.90 (0.92) | 5.89* | 1, 117 | 0.46 |
| F: Terror or screaming |
0.20 (0.53) | 0.10 (0.35) | 0.39 (0.74) | 8.41** 1, | 117 | 0.55 |
| G: Acting out dream |
0.38 (0.66) | 0.24 (0.54) | 0.63 (0.80) | 10.02** | 1, 117 | 0.60 |
| PSQI | 9.39 (4.18) | 8.94 (4.17) | 10.31 (4.10) | 2.85 | 1, 115 | 0.33 |
| CES | 15.02 (10.93) | 13.15 (10.74) | 18.47 (10.74) | 5.05* | 1, 110 | 0.49 |
| CAPS | 34.60 (22.25) | 21.37 (12.82) | 59.76 (12.43) | 245.95*** | 1, 117 | 3.01 |
| †CAPS | 27.07 (19.74) | 15.38 (10.90) | 49.29 (12.17) | 239.91*** | 1, 117 | 2.97 |
| BDI | 8.09 (7.00) | 6.50 (6.10) | 11.10 (7.67) | 12.43** | 1, 114 | 0.68 |
| ‡BDI | 6.22 (6.14) | 4.83 (5.16) | 8.88 (7.01) | 12.51** | 1, 114 | 0.69 |
| BAI | 5.74 (6.11) | 3.96 (4.25) | 8.73 (7.51) | 18.16*** | 1, 108 | 0.85 |
Note: = p < .05
= p < .01
= p < .001
= sleep items removed (“Difficulty falling or staying asleep,” and “Nightmares”)
= sleep items removed (“Sleeps Less” and “Tired”); g = Hedge’s g effect size for unequal sample sizes. Posttraumatic Stress Disorder (PTSD); Pittsburgh Sleep Quality Index Addendum for PTSD (PSQI-A); Pittsburgh Sleep Quality Index (PSQI); Combat Exposure Scale (CES); Clinician-Administered PTSD Scale (CAPS); Beck Depression Inventory (BDI); Beck Anxiety Inventory (BAI); A = Feel hot flashes; B = feel general nervousness; C = had memories of a traumatic experience; D = Had severe anxiety or panic; E = Had bad dreams; F = Had episodes of terror or screaming without fully awakening; G = had episodes of “acting out” dreams.
Psychometric properties of the PSQI-A
The seven PSQI-A items had a Cronbach’s α = 0.72, with an average inter-item correlation with the PSQI-A total score, r = 0.44 (range: 0.27—0.57). Table 2 shows the PSQI-A correlations with all study variables. The PSQI-A was positively associated with worse sleep quality, more combat exposure, worse PTSD symptomatology, worse depression symptomatology, and worse anxiety symptomatology.
Table 2.
Correlations among PSQI-A and clinical measures while controlling for age among total participants, and participants who were and were not clinically diagnosed with having PTSD
| Variable | Total N = 119 |
|---|---|
| PSQI | 0.44*** |
| CES | 0.34*** |
| CAPS | 0.58*** |
| †CAPS | 0.55*** |
| BDI | 0.59*** |
| ‡BDI | 0.57*** |
| BAI | 0.73*** |
Note: = p < .05
= p < .01
= p < .001
= sleep items removed (“Difficulty falling or staying asleep,” and “Nightmares”)
= sleep items removed (“Sleeps Less” and “Tired”).
Posttraumatic Stress Disorder (PTSD); Pittsburgh Sleep Quality Index Addendum for PTSD (PSQI-A); Pittsburgh Sleep Quality Index (PSQI); Combat Exposure Scale (CES); Clinician-Administered PTSD Scale (CAPS); Beck Depression Inventory (BDI); Beck Anxiety Inventory (BAI).
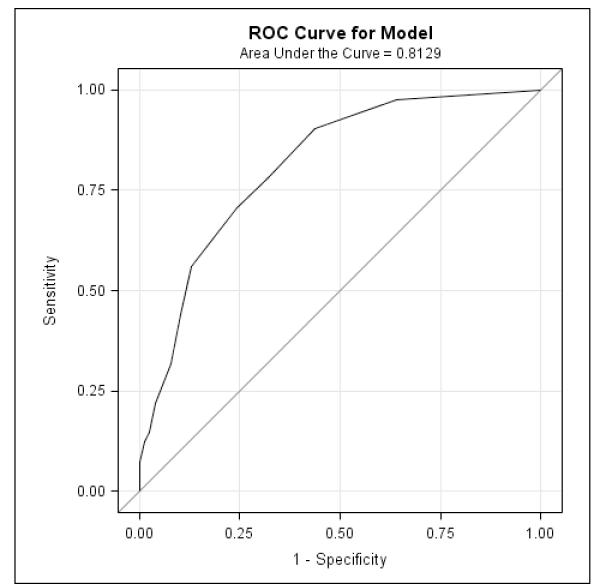
ROC analyses lead to an area under the curve that was 0.81 (Figure 1). That is, the PSQI-A score yielded an 81% probability that a random participant who would meet diagnostic criteria for PTSD, based on the CAPS, would have a higher PSQI-A score than a random participant not diagnosed with PTSD. A cut-off score ≥ 4 provided a 71% sensitivity, i.e., correct identification of PTSD cases according to the CAPS. A cut-off score ≥ 4 provided a 76% specificity, i.e., correct identification of non-PTSD cases according to the CAPS. A cut-off score ≥ 4 also provided 60% positive and 83% negative predictive values that a randomly selected participant would be correctly identified as meeting or not meeting PTSD diagnostic criteria, respectively. The same cut-off score ≥ 4 correctly classified 74% of participants as having or not having PTSD. Finally, a cut-off score ≥ 4 had a 2.9 positive likelihood ratio, and a .39 negative likelihood ratio that PTSD was and was not present, respectively. Measurement classification values based on different PSQI-A cut-off scores are provided in Table 3.
Figure 1.
Receiver Operator Characteristics curve to examine sensitivity and specificity of the PSQI-A to identify PTSD among male military veterans.
Table 3.
Measurement classification scores based on the full range of PSQI-A values
| PSQI-A Cut-off score |
Sensitivity | Specificity | Predictive Value+ |
Predictive Value− |
Correctly Classified |
Likelihood Ratio+ |
Likelihood Ratio− |
|---|---|---|---|---|---|---|---|
| 0 | 100% | 0% | 35% | 100% | 35% | - | - |
| 1 | 97% | 36% | 44% | 97% | 57% | 1.52 | 0.07 |
| 2 | 90% | 56% | 52% | 92% | 68% | 2.07 | 0.17 |
| 3 | 78% | 68% | 56% | 86% | 71% | 2.44 | 0.32 |
| 4 | 71% | 76% | 60% | 83% | 74% | 2.90 | 0.39 |
| 5 | 56% | 87% | 70% | 79% | 76% | 4.38 | 0.50 |
| 6 | 44% | 90% | 69% | 75% | 74% | 4.28 | 0.63 |
| 7 | 32% | 92% | 68% | 72% | 71% | 4.12 | 0.74 |
| 8 | 22% | 96% | 75% | 70% | 71% | 5.71 | 0.81 |
| 9 | 15% | 97% | 75% | 69% | 70% | 5.71 | 0.88 |
| 10 | 12% | 99% | 83% | 68% | 69% | 9.51 | 0.89 |
| 11 | 7% | 100% | 100% | 67% | 68% | - | 0.93 |
| 12 | 5% | 100% | 100% | 67% | 67% | - | 0.95 |
| 15 | 2% | 100% | 100% | 66% | 66% | - | 0.98 |
Note. Values were not calculated for PSQI-A total scores 13 and 14 because these scores were not represented in the present sample. Likelihood Ratios + and − were not calculated because the model was saturated. Likelihood Ratio + was not calculated for PSQI-A total scores 11, 12, and 15 because these scores were not represented in the sample without PTSD. Bold represents values for the suggested cutoff score.
DISCUSSION
In this sample of male military veterans, the PSQI-A internal consistency was comparable to the reports in the initial PSQI-A validation study among female sexual assault survivors (Germain et al., 2005). Veterans with PTSD demonstrated significantly greater PSQI-A scores than veterans without PTSD. PSQI-A scores were significantly correlated with overall poor sleep quality, combat exposure, PTSD symptoms. PSQI-A scores were also significantly depression and anxiety. A PSQI-A threshold score ≥ 4 yielded a sensitivity and specificity of 71% and 76%, respectively, and was recognized to accurately identify male military veterans who met diagnostic criteria for current PTSD. The original PSQI-A validation study concluded that cutoff value ≥ 4 provided adequate discrimination among participants who do and do not meet PTSD diagnostic criteria (94% sensitivity, 82% specificity, 93% positive predictive validity) (Germain et al., 2005). For the current study a cutoff value ≥ 4 yielded adequate sensitivity, specificity, negative predictive value, correct classification, and likelihood ratios. However, this cutoff score yielded low positive predictive value. The positive predictive value, as well as specificity, could be increased by increasing the PSQI-A cutoff score. Ultimately, determination of the appropriate cut-off score in a given sample should be determined by the need to either broadly identify veterans with potential PTSD (high sensitivity [lower cutoff score]), or to more accurately detect individuals with a high likelihood of PTSD (high specificity [higher cutoff score]). An informed decision about the adequate PSQI-A cutoff score to be employed may also be determined by the need to optimize assessment and treatment resources.
Significant positive correlations between the PSQI-A and poor sleep quality, combat exposure, PTSD symptoms, depression, and anxiety were detected even when the sleep items were removed from these compared measures. This suggests that the correlations between the PSQI-A and measures of psychiatric symptoms were not artificially inflated by possible multicollinearity effects of sleep questions within these measures. Similar to the initial validation study, PSQI-A scores were significantly correlated with increased PTSD symptoms and poor sleep quality; thus, suggesting convergent validity between the PSQI-A with the CAPS. Significant correlations between PSQI-A scores and sleep quality, depression, and anxiety may reflect the frequent co-occurrence disruptive nocturnal behaviors with poor sleep quality, depression, and anxiety among military veterans. In addition, these findings suggest that disruptive nocturnal behaviors among male military veterans may reflect a transdiagnostic feature of stress-related psychiatric disorders that arise from combat deployments. As such, disruptive nocturnal behaviors may not be specific to PTSD in military veterans, but rather, may reflect a common global sleep disruption that follows combat exposure. Evaluation of the latter possibility will require a larger and more heterogeneous sample of military veterans that includes higher comorbidity rates among PTSD and other anxiety and mood disorders.
Some limitations must be acknowledged. First, the prevalence of PTSD in the current study sample (34.5%) is higher than PTSD prevalence estimates in veterans currently returning from Iraq and Afghanistan (12%-19% [Hoge et al., 2004; RAND, 2008]), veterans of the Gulf War (8% [Wolfe, Erickson, Sharkansky, King, & King, 1999]), and veterans of the Vietnam War (30% [Weiss et al., 1992]). Thus, assessment of PSQI-A cutoff scores to use for PTSD diagnosis may be affected by the high rates of PTSD that are present within the current study sample. Second, the ROC may have yielded a relatively low cutoff score because of the sample assembled for this study was mainly composed young, male, military veterans. The generalizability of the present findings in a more heterogeneous sample of male military veterans is uncertain and could be influenced by a larger variety of individual differences (e.g. trauma history, trauma types, and psychiatric comorbidities). Third, the parent studies did not conduct multiple administrations of the PSQI-A to permit the examination of test-retest reliability. Fourth, although women make-up approximately 14% of military personnel across all service branches (Defense Advisory Committee on Women in the Services, 2011), this study did not include a sufficient number of women to adequately evaluate psychometrics of the PSQI-A in female veterans. However, because sex differences in PTSD-related sleep disturbances have not be detected (Green, 2003), the current PSQI-A results would not be expected to differ between female and male military veterans. Despite study limitations, the psychometric properties examined suggest that the PSQI-A is a valid, brief, self-report instrument to detect PTSD among male military veterans, without directly probing trauma reactions and mental health issues. Assessment of disruptive nocturnal behaviors with the PSQI-A, thus, may provide a cost-effective, non-stigmatizing approach to PTSD screening among returning military veterans.
The current study has important clinical utility for researchers and practitioners who work with military veterans, especially in light of ongoing conflicts and the influx of veterans returning home. Specifically, the current study provides the first validation of a sleep-focused measure that may serve as a cost-effective and non-stigmatizing instrument to identify PTSD among military veterans. The selected PSQI-A cutoff score for use among military veterans is flexible, and can be modified to match sensitivity or specificity needs determined by the researcher or practitioner, and may be adapted to optimize assessment and treatment resource utilization.
ACKNOWLEDGEMENTS
The authors thank Noelle Rode, Jean Miewald, Amy Begley, and Khaleelah Glover for their data entry, management, and processing. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the US Department of Defense, nor the U.S. Government.
This research was supported by: The Clinical and Translational Science Institute UL1RR024153; The National Institutes of Health R34 MH-080696-03(AG), R21 MH-083035-02 (AG), PR054093 (AG); and The Department of Defense PT073961 (AG). Dr. Insana is supported by NHLBI T32 HL-082610-04. Dr. Germain received federal funding from the National Institute of Mental Health, and the US Department of Defense Congressionally Directed Medical Research Program; she also received consultancy honoraria from Concurrent Technologies Corporation. Dr. Buysse serves as a paid consultant for Eisai, Merck, Pfizer, Philips, Purdue Pharma, L.P., sanofi-aventis, and Transcept Pharmaceuticals, Inc. Consulting fees for each company are less than $10,000 annually. Dr. Buysse has been paid for and lectures at non-CME educational meetings supported by Servier.
Footnotes
FINANCIAL DISCLOSURES The authors declare no potential conflicts of interest.
REFERENCES
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Revised 4th ed Washington, DC; 2000. [Google Scholar]
- Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. Journal of Anxiety Disorders. 2010;24:1–15. doi: 10.1016/j.janxdis.2009.08.002. doi:10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. doi:10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. doi:10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi:10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Blake DK, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, et al. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;13:187–188. [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Hoge C, Prayner R. U.S. Army Medical Research Unit-Europe Research Report 2005-003. U.S. Army Medical Research Unit-Europe; Heidelberg, Germany: 2005. Post-deployment psychological screening interpreting and scoring DD Form 2900. [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Thomas JL. Psychological screening validation with soldiers returning from combat. In: Roy MJ, editor. Novel Approaches to the Diagnosis and Treatment of Posttraumatic Stress Disorder. IOS Press; Amsterdam, Netherlands: 2006. pp. 78–86. [Google Scholar]
- Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbances and psychiatric disorders: a longitudinal epidemiological study of young adults. Biological Psychiatry. 1996;39:411–418. doi: 10.1016/0006-3223(95)00188-3. doi:10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33:69–74. doi: 10.1093/sleep/33.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. doi:10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Capaldi VF, 2nd, Guerrero ML, Killgore WD. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Military Medicine. 2011;176:879–888. doi: 10.7205/milmed-d-10-00440. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for Behavioral Sciences. 2 ed Lawrence Erlbaum Associates; Hillsdale,NJ: 1988. [Google Scholar]
- Defense Advisory Committee on Women in the Services [Retrieved December 1, 2011];Defense Advisory Committee on Women in the Services: 2010 Report. 2011 from http://dacowits.defense.gov/Reports/2010/Annual%20Report/dacowits2010report.pdf.
- Farrahi J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Psychometric properties of the Persian version of the Pittsburgh Sleep Quality Index addendum for PTSD (PSQI-A) Sleep & Breathing. 2009;13:259–262. doi: 10.1007/s11325-008-0233-3. doi:10.1007/s11325-008-0233-3. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Unpublished manuscript. Version 2.0 Biometrics Research Department, New York State Psychiatric Institute; 1995. Users guide for the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P) [Google Scholar]
- Germain A, Hall M, Krakow B, Katherine SM, Buysse DJ. A brief sleep scale for Posttraumatic Stress Disorder: Pittsburgh Sleep Quality Index Addendum for PTSD. Journal of Anxiety Disorders. 2005;19:233–244. doi: 10.1016/j.janxdis.2004.02.001. doi:10.1016/j.janxdis.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Germain A, Buysse DJ, Shear MK, Fayyad R, Austin C. Clinical correlates of poor sleep quality in posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17:477–484. doi: 10.1007/s10960-004-5796-6. doi:10.1007/s10960-004-5796-6. [DOI] [PubMed] [Google Scholar]
- Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. Journal of Affective Disorders. 2010;123:249–257. doi: 10.1016/j.jad.2009.08.006. doi:10.1016/j.jad.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Green B. Post-traumatic stress disorder: symptom profiles in men and women. Current Medical Research and Opinion. 19:200–204. doi: 10.1185/030079903125001604. doi:10.1185/030079903125001604. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. doi:10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. doi:10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hovens JE, van der Ploeg HM, Klaarenbeek MT, Bramsen I, Schreuder JN, Rivero VV. The assessment of posttraumatic stress disorder: with the Clinician Administered PTSD Scale: Dutch results. Journal of Clinical Psychology. 1994;50:325–340. doi: 10.1002/1097-4679(199405)50:3<325::aid-jclp2270500304>3.0.co;2-m. doi:10.1002/1097-4679(199405)50:3<325::AID-JCLP2270500304>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Insana SP, Kolko DJ, Germain A. Early-life trauma is associated with rapid eye movement sleep fragmentation among military veterans. doi: 10.1016/j.biopsycho.2012.01.001. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a measure to assess combat exposure. Psychological Assessment. 1989;1:53–55. doi:10.1037/1040-3590.1.1.53. [Google Scholar]
- Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: a 1-year prospective study of injured survivors of motor vehicle accidents. American Journal of Psychiatry. 2002;159:855–857. doi: 10.1176/appi.ajp.159.5.855. doi:10.1176/appi.ajp.159.5.855. [DOI] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the structured clinical interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clinical Psychology and Psychotherapy. 2011;18:75–79. doi: 10.1002/cpp.693. doi:10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. American Journal of Psychiatry. 2002;159:1696–1701. doi: 10.1176/appi.ajp.159.10.1696. doi:10.1176/appi.ajp.159.10.1696. [DOI] [PubMed] [Google Scholar]
- Mellman TA, Kulick-Bell R, Ashlock L, JE., Nolan B. Sleep events among veterans with combat-related posttraumatic stress disorder. American Journal of Psychiatry. 2003;152:110–115. doi: 10.1176/ajp.152.1.110. [DOI] [PubMed] [Google Scholar]
- McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U. S. service members returning from military deployments. Military Medicine. 2010;175:759–762. doi: 10.7205/milmed-d-10-00193. [DOI] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. doi:10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Schell TL, Karney BR, Osilla KC, Burns RM, Caldarone LB. Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: possible explanations. Journal of Traumatic Stress. 2010;23:59–68. doi: 10.1002/jts.20486. doi:10.1002/jts.20486. [DOI] [PubMed] [Google Scholar]
- Ramirez Basco M, Bostic JQ, Davies D, Rush JA, Witte B, Hendrickse W, Barnett V. Methods to improve diagnostic accuracy in a community mental health setting. American Journal of Psychiatry. 2000;157:4599–1605. doi: 10.1176/appi.ajp.157.10.1599. doi:10.1176/appi.ajp.157.10.1599. [DOI] [PubMed] [Google Scholar]
- RAND. Tanielian T, Jaycox LH. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. RAND Corporation; Santa Monica, CA: 2008. [Google Scholar]
- Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. American Journal of Psychiatry. 1989;146:697–707. doi: 10.1176/ajp.146.6.697. [DOI] [PubMed] [Google Scholar]
- Salkind MR. Beck depression inventory in general practice. Journal of the Royal College of General Practitioners. 1969;18:267–271. [PMC free article] [PubMed] [Google Scholar]
- Schramm E, Hohagen F, Grasshoff U, Riemann D, Hajak G, Weeb H, Berger M. Test-retest reliability and validity of the Structured Interview for Sleep Disorders According to DSM-III-R. American Journal of Psychiatry. 1993;150:867–872. doi: 10.1176/ajp.150.6.867. [DOI] [PubMed] [Google Scholar]
- Seelig AD, Jacobson IG, Smith B, Hooper TI, Boyko EJ, Gackstetter GD, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–1622. doi: 10.1093/sleep/33.12.1615. doi:10.2337/dc10-0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh JL, Woodward SH, Leskin GA. Sleep in post-traumatic stress disorder and panic: convergence and divergence. Depression and Anxiety. 2003;18:187–197. doi: 10.1002/da.10066. doi:10.1002/da.10066. [DOI] [PubMed] [Google Scholar]
- Spiro A, Hankin CS, Mansell D, Kazis LE. Posttraumatic stress disorder and health status: The Veterans Health Study. Journal of Ambulatory Care Management. 2006;29:71–86. doi: 10.1097/00004479-200601000-00008. [DOI] [PubMed] [Google Scholar]
- Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Medicine Reviews. 2008;12:169–184. doi: 10.1016/j.smrv.2007.08.008. doi:10.1016/j.smrv.2007.08.008. [DOI] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, Mc Gurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry. 2010;67:614–623. doi: 10.1001/archgenpsychiatry.2010.54. doi:10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau [Retrieved December 1, 2011];National Security & Veterans Affairs: Veterans by Sex, Period of Service, and State: 2010. 2010 from http://www.census.gov/compendia/statab/cats/national_security_veterans_affairs/veterans.html.
- Vogt D. Mental health-related beliefs as a barrier to service use for military personnel and veterans: a review. Psychiatric Services. 2011;62:135–142. doi: 10.1176/ps.62.2.pss6202_0135. doi:10.1176/appi.ps.62.2.135. [DOI] [PubMed] [Google Scholar]
- Warner CH, Appenzeller GN, Grieger T, Belenkiy S, Breitbach J, Parker J, et al. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Archives of General Psychiatry. 2011;68:1065–1071. doi: 10.1001/archgenpsychiatry.2011.112. doi:10.1001/archgenpsychiatry.2011.112. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. doi:10.1037//1040-3590.11.2.124. [Google Scholar]
- Weiss DS, Marmar CR, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, et al. The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater Veterans. Journal of Traumatic Stress. 1992;5:365–376. doi:10.1002/jts.2490050304. [Google Scholar]
- Wolfe J, Erickson DJ, Sharkansky EJ, King DW, King LA. Course and predictors of posttraumatic stress disorder among Gulf War veterans: a prospective analysis. Journal of Consulting and Clinical Psychology. 1999;67:520–528. doi: 10.1037//0022-006x.67.4.520. doi:10.1037//0022-006X.67.4.520. [DOI] [PubMed] [Google Scholar]
- Wright KM, Adler AB, Bliese PD, Eckford RD. Structured clinical interview guide for postdeployment psychological screening programs. Military Medicine. 2008;173:411–421. doi: 10.7205/milmed.173.5.411. [DOI] [PubMed] [Google Scholar]
- Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as a predictor versus outcome of PTSD and depression among Iraq combat veterans. Journal of Clinical Psychology. 2011;67:1240–1258. doi: 10.1002/jclp.20845. doi:10.1002/jclp.20845. [DOI] [PubMed] [Google Scholar]