Abstract
Purpose
The current study examines the prevalence and demographic correlates of self-reported substance use and identifies subgroups of polysubstance users among a cohort of US 10th grade students.
Methods
A nationally representative school-based cohort of US 10th grade students completed the NEXT Generation Health Study baseline survey in the spring of 2010 (N = 2,524).
Results
Past-year use of marijuana was most common among illicit drugs (26%), followed by misuse of medication (9%) and use of other illicit drugs (8%). During the past month, alcohol use was reported by more than one-third (35%), binge drinking by 27%, and cigarette smoking by 19%. Results further show that substance use varied somewhat by demographic characteristics. Results from the latent class analysis of polysubstance use indicated a 4-class solution as the best-fitting model; Class 1 (59%) included the ‘non-user’ group; Class 2 (23%) comprised the ‘predominant alcohol user’ group; Class 3 (11%) formed the ‘predominant marijuana user’ group; Class 4 (8%) was characterized as the ‘predominant polysubstance user’ group. Somatic and depressive symptoms varied significantly by class membership, with predominant polysubstance users reporting elevated levels of somatic and depressive symptoms.
Conclusions
The findings from this national study of 10th-grade students indicate high rates of substance and polysubstance use. The high level of depressive and somatic symptoms among polysubstance users indicates the need for mental health screening and referral.
Keywords: Substance Abuse, Polysubstance Use, Latent Class Analysis, Medication Misuse, Depression, Substance Use, Adolescence, Comorbidity, Drug Abuse
Introduction
National epidemiological studies estimate that most adolescents will engage in some form of substance use by the time they graduate from high school. The 2011 Monitoring the Future Survey (MTF) found that 26.4% have tried an illicit drug by 8th grade, 40.8% by 10th grade, and 51.8% by 12th grade [1]. MTF findings further show that adolescent users tend to report using a variety of specific substances at an early age. Among 10th graders, for example, rates of past-year use were 49.8% for alcohol, 28.8% for marijuana/hashish, 6.6% for amphetamines, and a range from 2.6–5.9% for misuse of medications (e.g. Oxycontin, cough medicine) [1].
Polysubstance use, defined as using multiple substances within a specified period of time, remains an understudied characteristic of youthful substance use [2–6]. Previous findings on polysubstance use come largely from studies applying latent class analyses to identify multiple classes/groups of adolescents defined by their patterns of substance use. Among the school-based surveys of adolescents in middle- or high-school, between 15% and 39% of adolescents could be classified as polysubstance users, with precise estimates varying by sample, reporting period, and definition of polysubstance use [2–6]. Results from the 2005 Youth Risk Behavior Surveillance (YRBS) [6] depict four classes based upon past-month use among grades 9–12, as follows: alcohol experimenters (38%), non-users/abstainers (27%), occasional polysubstance users (23%), and frequent polysubstance users (13%). The 2001–02 Add Health data [5] identified five classes of students in grades 7–12 based upon use during the past month/year: low use (55%), alcohol only (15%), alcohol-marijuana (8%), cigarettes (8%), three-substance use (14%) [5]. Given that medication is now the most commonly abused substance after alcohol, marijuana, and tobacco [1;7], it seems both timely and useful that these substances be examined separately to better characterize contemporary patterns of use.
In addition to examining prevalence of classes defined by polysubstance use, several studies have linked adolescent polysubstance use with deleterious outcomes, including substance dependence [4], smoking in adulthood [5], and risky sexual behavior [6]. Furthermore, many studies have reported that substance abuse commonly co-occurs with mental health problems in epidemiologic samples of adults [8–12] and adolescents [13–15], with psychopathology onset often predating substance abuse [13;14;16]. However, past research has been limited in two key ways. First, most studies focus on a specific substance (e.g. cannabis) or on substance use at an aggregate level (e.g., any substance use), rather than a more detailed characterization that is based upon profiles of polysubstance use. Second, most studies of comorbidity report disorder-level associations between specific substance use disorders and specific psychiatric disorders [9–11] or between any substance use disorder and specific psychiatric disorders [8;12]. Although polysubstance use has been associated with depressive symptoms in college students [17], to our knowledge only two studies examined polysubstance use and depressive symptoms among adolescents [3;5]. Additional research is needed not only on the association between adolescent polysubstance use and depressive symptomatology in particular, but also on somatic complaints such as headaches, stomach aches, and other musculoskeletal pains, which are common expressions of underlying depression in adolescents [18;19].
The purposes of the current study are threefold: (1) to examine the prevalence and demographic correlates of substance use; (2) to identify classes/subgroups according to substance use patterns; and (3) to examine associations between classes/subgroups and depressive and somatic symptoms.
Methods
The NEXT Generation Health Study is a longitudinal study of a cohort of 10th-grade U.S. students beginning in the spring of 2010. School-based assessments included a survey of health behaviors with a focus on four areas: obesity and obesity-related behaviors (e.g., physical activity, sedentary behavior, diet, and sleep); substance use; dating violence; and driving.
Sample and Procedure
A nationally representative cohort of U.S. students in grade 10 was recruited using a multistage stratified design. Primary-sampling units consisted of school districts or groups of school districts stratified across the nine U.S. Census divisions. Within this sampling framework 137 schools were randomly selected and formally recruited; 80 (58.4%) agreed to participate. Tenth-grade classes were randomly selected within each recruited school and 3,796 students were recruited to participate; youth assent and parental consent were obtained from 2,619 (69.0%) students. Of those consented, 2,524 completed the Wave 1 survey for an overall completion rate of 66.5%. African-American students were oversampled to provide better prevalence estimates and permit comparisons across subpopulations; given the prevalence of Hispanic youth in this sample, the cohort already included an adequate sample of Hispanic youth to meet these criteria. In Wave 1 (baseline), confidential self-report surveys were administered by trained research assistants in the 10th-grade classrooms. The study protocol was reviewed and approved by the Institutional Review Board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Measures
Demographics
Students provided information about race/ethnicity and family composition. Parental education was provided by parents of youth via a paper survey completed when parents gave informed consent for their child’s participation. The item, obtained from the Add Health study, indicates the highest grade completed at the time of the interview.
Substance Use
Prevalence in the past month was reported separately for cigarette smoking, alcohol use, and binge drinking. On a seven-point scale (1=never, 2=once or twice, 3=3–5 times, 4=6–9 times, 5=10–19 times, 6=20–39 times, 7=40 times or more), respondents reported on how many occasions in the last 30 days they had smoked cigarettes and on how many occasions they drank alcohol. To assess binge drinking, on a six-point scale (1=none, 2=1, 3=2, 4=3–5, 5=6–9, 6=10 or more times) respondents reported how many times in the last month they had four or more (females) or five or more (males) drinks in a row on an occasion. The alcohol questions came from the European School Survey Project on Alcohol and Other Drugs and the National Longitudinal Study of Adolescent Health study (Add Health), with the measure of binge drinking conforming to the NIAAA standard [20]. Prevalence in the past year was reported separately for marijuana/hashish use, medication use to get high, and other illicit drug use. On a seven-point scale (1=never, 2=once or twice, 3=3–5 times, 4=6–9 times, 5=10–19 times, 6=20–39 times, 7=40 times or more), respondents reported how often in the last twelve months they had used marijuana, ecstasy, amphetamines (meth, ice, glass, speed), opiates (heroin, morphine, smack), medication to get high, cocaine, glue or solvents, LSD, anabolic steroids, and other drugs (open-ended). For reporting prevalence of substance use and conducting latent class analyses, six dichotomous variables were created (never vs. ever used during past month or past year) on cigarette smoking, alcohol use, binge drinking, marijuana use, medication misuse, and other illicit drug use.
Depressive and Somatic Symptomatology
Depressive symptomatology was assessed by a self-reported screener for DSM-III-R depression [21]. On a five-point scale (1=never, 2=seldom, 3=sometimes, 4=often, 5=always), respondents reported how often they endorsed the following 6 items over the last 30 days: feeling very sad, feeling grouchy/irritable or in a bad mood, feeling hopeless about the future, feeling like not eating or eating more than usual, sleeping a lot more or a lot less than usual, and experiencing difficulty concentrating on school work. The internal reliability of this scale was high (Chronbach alpha = 0.82). In addition, somatic symptoms were assessed through self-report [22]. On a 5-point scale (1=rarely or never, 2=about every month, 3=about every week, 4=more than once a week, 5=about every day), respondents reported how often they endorsed the following 4 items over the last 6 months: having a headache, having a stomachache, having a backache, and feeling dizzy. The internal reliability of this scale was moderate (Chronbach alpha = 0.70).
Analytical Approach
A series of latent class analyses (LCA) were conducted in two steps. The first step was to choose the optimal number of classes by specifying separate LCA models with various numbers of classes. The models were tested with and without demographic covariates, which included gender, race/ethnicity and parent education. The most parsimonious 1-class model was first conducted, and then successive models with 2–5 classes were estimated. For LCA with covariates, with class membership as outcome and demographic variables as predictors, the model is analogous to a logistic or multinomial logistic regression. Models were compared on a series of statistical fit indices, as well as conceptual considerations, including: 1) Information criteria, including the Akaike Information Criterion (AIC) [23], Bayesian Information Criterion (BIC) [24], and sample size adjusted BIC (ABIC) were compared; 2) The Pearson and likelihood ratio chi-square statistics were reported, with non-significant p-values indicating good fit; 3) The selected model should have adequate classification quality, as shown by relative entropy and average classification probabilities (ACPs) with entropy and ACPs values near one indicate high certainty and reliability in the classification; and 4) the practical interpretability of the classes was considered in comparing models with similarly adequate fit statistics. More weight was given to BIC and ABIC in choosing the number of classes, as a recent simulation study has shown that BIC performs better than other information criteria and likelihood ratio tests in identifying the appropriate number of latent classes [25]. After the appropriate number of classes was chosen, depressive and somatic symptoms were compared across the extracted latent classes. The posterior probability-based multiple imputations were used to conduct paired mean comparisons.
The statistical software package Mplus 6.1 [26] was used for model-fitting. To accommodate the complex sampling structure of the data, LCA models were examined with stratification, cluster and sampling weights. Furthermore, Mplus enabled us to make use of all available data, including cases with some missing responses, through estimation by Full Information Maximum Likelihood, FIML [27]. Depressive and somatic symptoms were compared across latent class membership with the AUXILIARY option in Mplus.
Results
Sample
The demographic characteristics of the sample appear in Table 1. There were slightly more females than males; 54.4% female, 45.6% male. Race/ethnicity, parent education, family structure, and region of residence in the U.S. are also reported.
Table 1.
Sample Characteristics of NEXT Generation Health Study(N=2524)
| Categories | N | Weighted % | SE |
|---|---|---|---|
| Gender (n = 2519) | |||
| Male | 1132 | 45.6 | 1.7 |
| Female | 1387 | 54.4 | 1.7 |
| Race/Ethnicity (n = 2510) | |||
| White | 1092 | 57.9 | 5.5 |
| African-American | 485 | 17.5 | 3.7 |
| Hispanic | 801 | 19.6 | 3.3 |
| (other)* | (132) | (4.9) | (1.1) |
| Asian | 79 | 1.7 | 0.5 |
| Hawaiian/Pacific Islander | 13 | 0.4 | 0.2 |
| American Indian/Alaskan Native | 40 | 2.8 | 1.0 |
| Parent education (highest of both) (n = 2361) | |||
| Less than HS diploma | 334 | 8.4 | 2.0 |
| High school diploma/GED | 602 | 25.1 | 2.1 |
| Some college or technical school | 865 | 39.7 | 1.7 |
| Bachelor degree | 321 | 14.4 | 1.6 |
| Graduate degree | 239 | 12.4 | 2.0 |
| Family Structure (n =2524) | |||
| Both biological | 1320 | 52.1 | 2.2 |
| Step-parents | 419 | 19.2 | 1.3 |
| Single parent-mother | 457 | 16.8 | 1.6 |
| Single parent-father | 59 | 2.7 | 0.6 |
| Others | 269 | 9.2 | 1.1 |
| Region (n =2524) | |||
| South | 1098 | 39.3 | 3.4 |
| Northeast | 368 | 17.0 | 4.1 |
| West | 682 | 24.7 | 2.8 |
| Midwest | 376 | 19.0 | 3.3 |
Note: The “other” group includes Asian, Hawaiian/Pacific Islander, and American Indian/Alaskan Native.
The prevalence of substance use, by sex, race, parent education, family structure, and geographic region, appears in Table 2. Of the 2524 respondents, 29% reported using any illicit drugs in the past year (data not shown). During the past month, alcohol use was reported by 35%, binge drinking by 27%, and cigarette smoking by 19%. Past-year use of marijuana was 26%, misuse of medication was 9%, and other illicit drugs (ecstasy, amphetamine, LSD, opiates, cocaine, anabolic steroids, and glue/solvents) was 8%.
Table 2.
Prevalence of Illicit Drug Use (Past 12 Months) and Nicotine, Alcohol Use, Binge Drinking (Past Month) in U.S. adolescents in the NEXT Generation Health Study(N=2524)
| Past Year | Past 30 Day | |||||
|---|---|---|---|---|---|---|
| Marijuana (N = 2485) |
Medication to Get High (N = 2482) |
Other Illicit Drug (N = 2482) |
Smoked Cigarettes (N =2498) |
Drank alcohol (N =2497) |
Binge Drinking (on one occasion) (N =2477) |
|
| Category | % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | % (SE) |
| Total (N = 2524) | 26.3 (2.2) | 8.7 (1.3) | 8.3 (.97) | 18.9 (2.6) | 35.3 (2.3) | 27.2 (1.9) |
| Gender | ||||||
| Male (n = 1132) | 30.0 (3.5) a | 10.5 (2.2) | 6.9 (1.3) | 20.0 (3.0) | 34.2 (2.7) | 28.8 (2.3) |
| Female (n =1386) | 23.1 (1.8) b | 7.2 (1.3) | 9.5 (1.3) | 17.9 (2.7) | 36.1 (2.9) | 25.9 (2.4) |
| Race/Ethnicity | ||||||
| White (n =1092) | 25.9 (2.7) | 8.7 (1.2) | 6.7 (1.1) a | 21.3 (2.6) | 36.4 (3.0) | 29.4 (2.4) |
| African-American (n = 485) | 20.5 (3.2) | 6.7 (3.7) | 8.2 (2.7) ab | 9.7 (3.2) | 31.8 (5.6) | 18.6 (4.4) |
| Hispanic (n = 801) | 32.1 (4.6) | 10.1 (3.0) | 11.7 (1.6) b | 18.8 (6.2) | 34.5 (4.3) | 27.7 (4.2) |
| Other (n = 132) | 28.1 (7.6) | 10.7 (6.6) | 14.4 (5.7) b | 23.5 (8.3) | 39.0 (10.2) | 30.1 (7.5) |
| Parent education | ||||||
| Less than HS diploma (n =334) | 26.1 (4.3) ab | 4.0 (1.9) | 11.0 (2.9) | 16.4 (7.0) ab | 33.9 (5.4) ab | 26.1 (4.9) ab |
| High school diploma/GED (n = 602) |
30.5 (3.2) a | 9.3 (2.1) | 7.7 (2.0) | 25.3 (3.9) a | 34.6 (2.4) ab | 30.4 (3.6) a |
| Some college or technical school (n = 865) |
27.1 (3.8) ab | 8.1 (1.8) | 10.3 (2.5) | 18.2 (3.2) b | 35.2 (3.1) ab | 27.4 (2.9) ab |
| Bachelor degree (n = 321) | 2 5 . 6 ( 7 .3) ab | 13.1 (4.2) | 5.1 (1.5) | 16.8 (3.7) ab | 41.3 (6.3) a | 30.0 (6.0) a |
| Graduate degree (n =239) | 1 5 . 0 ( 3 .8) b | 8.1 (3.3) | 3.6 (1.7) | 14.4 (3.2) b | 31.4 (4.7) b | 17.6 (3.4) b |
| Family Structure | ||||||
| Both biological (n = 1320) | 22.2 (2.1) a | 6.9 (1.5) | 5.6 (1.0) a | 15.4 (1.7) a | 33.4 (2.6) | 23.9 (2.5) a |
| Step-parents (n = 594) | 32.7 (2.7) b | 12.3 (2.3) | 12.8 (2.4) bc | 20.3 (2.5) b | 37.6 (3.2) | 34.4 (3.7) b |
| Single parent – mother (n = 859) |
25.9 (4.1) ab | 9.0 (2.5) | 6.4 (1.7) a | 20.0 (4.3)ab | 36.6 (4.7) | 29.1 (4.3)ab |
| Single parent – father (n = 321) |
23.0 (9.6) ab | 8.8 (6.9) | 11.5 (7.0) abc | 28.6 (5.3) b | 31.0 (2.9) | 20.2 (7.0)ab |
| Others (n = 269) | 37.3 (7.4) b | 11.2 (3.9) | 16.5 (5.0) c | 30.6 (9.2) b | 40.6 (5.7) | 29.3 (5.9)ab |
| Region | ||||||
| South (n = 1098) | 22.9 (3.8) | 6.8 (1.5) | 8.5 (1.3) | 18.6 (3.8) ab | 33.7 (3.0) | 25.1 (3.1) |
| Northeast (n = 368) | 23.4 (3.1) | 6.6 (1.9) | 5.0 (2.3) | 11.7 (1.9) a | 37.1 (5.7) | 25.8 (5.1) |
| West (n= 682) | 34.8 (5.0) | 12.0 (3.5) | 11.7 (2.2) | 20.4 (7.4) ab | 36.5 (6.9) | 29.6 (4.7) |
| Midwest (n = 376) | 24.8 (4.5) | 10.4 (3.5) | 6.5 (2.0) | 23.7 (4.2) b | 35.6 (1.5) | 29.8 (1.7) |
Note: Prevalence was a weighted percentage controlling for the complex survey design. For each demographic characteristic, separate logistic regression models were conducted for each of the six substance use variables. Pairwise contrast analyses were conducted when an overall difference was detected. The “Other” group for race/ethnicity includes Asian, Hawaiian/Pacific Islander, and American Indian/Alaskan Native. Analyses were conducted with SAS, version 9.2.
Within each model, two categories with different superscripts were significantly different in using the particular substance, according to Wald Chi-square test statistics at an alpha of 0.05. Categories with significant differences are bolded. For example, there was a significant racial/ethnic difference with regard to prevalence of other illicit drug. Further contrast analyses showed a significant difference between the White and Hispanics, and between White and other racial/ethnic group.
Other findings indicate that substance use varied somewhat by demographic characteristics. Marijuana use was more prevalent among males than females. Compared to Whites, Hispanics and those in the ‘Other’ race/ethnicity category (including Asian, Hawaiian/Pacific Islander, and American Indian/Alaska Native) were more likely to use other illicit drugs. There were several differences by parent education category. For example, the prevalence of marijuana use, cigarette smoking and binge drinking was lower among children of parents with graduate degrees compared to high-school diploma/GED. By family structure, significantly lower prevalence was found among children with biological parents than children whose family structure falls into other categories, including step-parents (marijuana use, other illicit drug us, cigarette smoking and binge drinking), single father (cigarette smoking), and other family structure (marijuana use, other illicit drug use, and cigarette smoking). In addition, children from single-mother families reported lower use of other illicit drugs compared to step-parents and other family structure. Last, prevalence of smoking cigarettes was lower among those living in Northeast than Midwest.
Latent classes
Results of fit statistics are reported in Table 3 for the LCA models with 1–5 classes, and for the LCA with covariates models with 2–5 classes. Pearson and likelihood Chi-square statistics test departure of the model from the observed data and were significant for models with 1–3 classes but not significant for models with 4–5 classes. In terms of the information criteria, the 4-class solution without covariates had the minimum values on BIC and ABIC, and the 4-class solution with covariates had the minimum values on BIC. In addition, the 4-class solution also had acceptably high values on entropy (without covariates: .832; with covariates .806) and ACPs (without covariates: range = .869–.921; with covariates: range=.846–.915). Thus, by model fit statistics, the 4-class solution was chosen as the best-fitting model. An examination on class interpretability for models with 2–5 classes further indicates the 4-class model as optimal in terms of practical implication and distinctiveness of each latent class.
Table 3.
Model Fit Statistics for Models with 1–5 Latent Classes
| Without Covariates N =2524 Tests of Model Fit |
1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|
| Information Criteria a | ||||||
| AIC | 14343.7 | 11533.1 | 11315.2 | 11147.0 | 11135.5 | |
| BIC | 14378.7 | 11608.9 | 11431.9 | 11304.5 | 11333.8 | |
| Adjusted BIC | 14359.7 | 11567.6 | 11368.3 | 11218.7 | 11225.8 | |
| Chi-Square Test b | ||||||
| Pearson X2 | 582.7 | 221.2 | 145.6 | 42.3 | 27.4 | |
| df | 55 | 50 | 43 | 36 | 29 | |
| p | .000 | 0.000 | 0.000 | 0. 217 | 0. 550 | |
| Likelihood Ratio G2 | 255.0 | 177.3 | 101.5 | 41.5 | 31.5 | |
| df | 55 | 50 | 43 | 36 | 29 | |
| p | 0.000 | 0.000 | 0.000 | 0. 243 | 0. 342 | |
| Entropy c | -- | 0.854 | 0.831 | 0.832 | 0.849 | |
| Range of ACPs d | -- | .958–.964 | .859–.957 | .869–.921 | .787–.954 | |
|
With Covariates, N = 2350 Tests of Model Fit |
2 | 3 | 4 | 5 | ||
| Information Criteria a | ||||||
| AIC | 10783.7 | 10568.2 | 10365.6 | 10304.0 | ||
| BIC | 10893.1 | 10752.6 | 10624.9 | 10638.2 | ||
| Adjusted BIC | 10832.8 | 10650.9 | 10481.9 | 10453.9 | ||
| Chi-Square Test b | ||||||
| Pearson X2 | 211.6 | 121.9 | 44.1 | 40.8 | ||
| df | 50 | 43 | 36 | 29 | ||
| p | 0.000 | 0.000 | 0. 167 | 0.072 | ||
| Likelihood Ratio G2 | 169.9 | 113.7 | 43.1 | 41.3 | ||
| df | 50 | 43 | 36 | 29 | ||
| p | 0.000 | 0.000 | 0.195 | 0.065 | ||
| Entropy c | -- | 0.849 | 0.828 | 0.806 | 0.819 | |
| Range of ACPs d | -- | .944–.969 | .823–.976 | .846–.915 | .695–.920 | |
Note AIC = Akaike’s Information Criteria; BIC = Bayesian Information Criteria; Adjusted BIC is BIC adjusted for sample size. Model with smaller AIC, BIC and Adjusted BIC value is considered to have a better fit.
Pearson and likelihood Chi-square statistics test departure of the model from the observed data.
The entropy statistics ranges from 0 to 1, with values closer to 1 indicating a better classification quality.
ACP = Average Latent Class Probabilities for Most Likely Latent Class Membership.
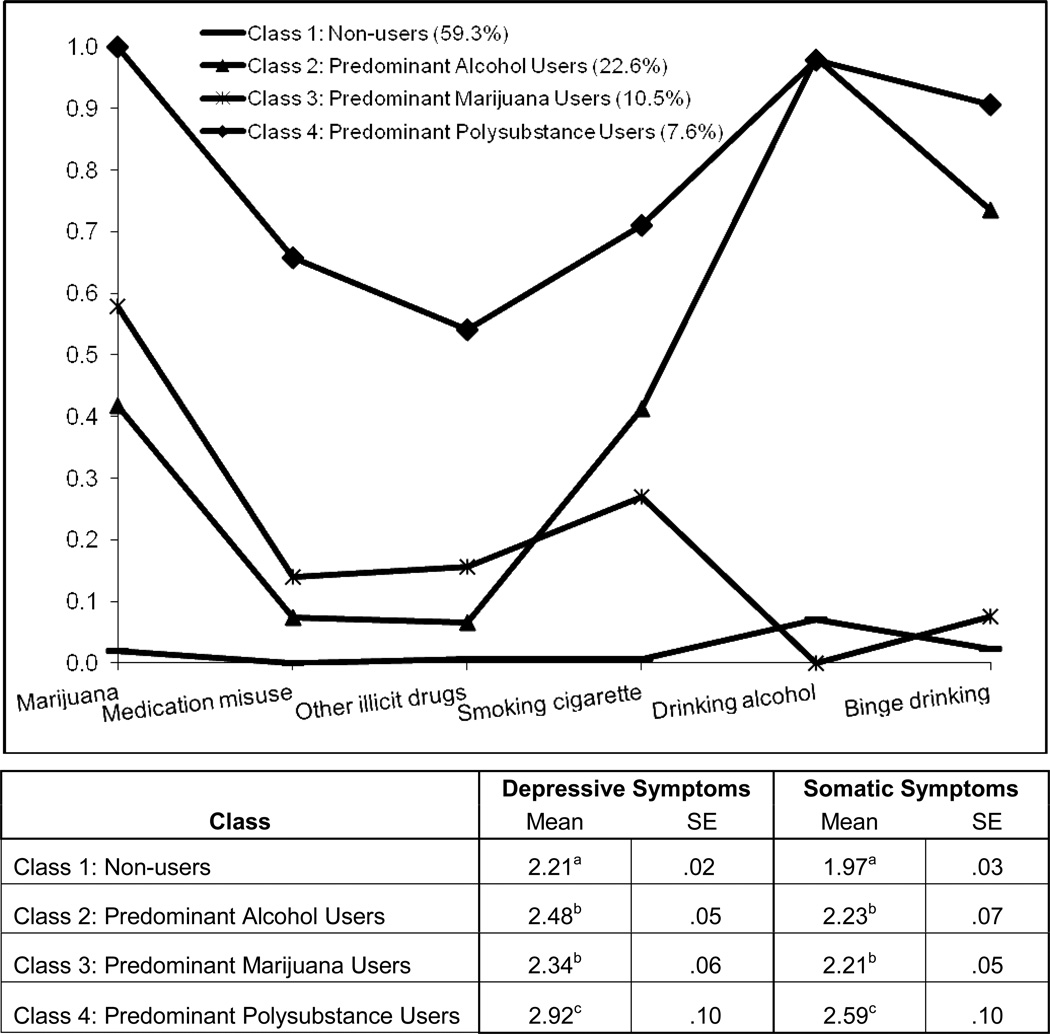
For the 4-class solution of LCA with covariates, Figure 1 reports the latent class prevalence, i.e., the proportion of the sample composing each class, and item probability, i.e., the likelihood of reporting each behavior within a particular latent class. Adolescents in Class 1 (59.3%) formed the ‘non-user’ group, with very low probabilities of using any of the substances, such as medication to get high (.000), illicit drugs (.006), cigarettes (.007), marijuana (.019), alcohol (.071) and binge drinking (.023). Adolescents in Class 2 (22.6%) comprised the ‘predominant alcohol user’ group, with high probability of drinking (.982) and moderately high probability of binge drinking (.735), moderate probabilities of using marijuana (.418) and smoking cigarettes (.413), and low probabilities of misusing medication (.074) and using other illicit drugs (.066). Adolescents in Class 3 (10.5%) formed the ‘predominant marijuana user’ group, with much higher probability of using marijuana (.578) than using other substances, such as cigarettes (.270) or medication to get high (.139) or other illicit drugs (.156), and virtually no use of alcohol (.000) or binge drinking (.076). Adolescents in Class 4 (7.6%) formed the ‘predominant polysubstance user’ group who had moderate to very high probabilities of using each of the substances, including marijuana (1.000), alcohol (.979), binge drinking (.906), cigarettes (.711), medication to get high (.658), and other illicit drugs (.541).
Figure 1.
Item Probability for Each Latent Class in the Four-Class Model and Associations with Depressive and Somatic Symptomatology
Note. Classification of individuals was based on their most likely latent class membership; the model included demographic covariates.
Two categories with different superscripts were significantly different in mean report of symptoms, according to Wald Chi-square test statistics at an alpha of 0.05. The response options for depressive symptoms were 1=never, 2=seldom, 3=sometimes, 4=often, 5=always; and the response options for somatic symptoms were 1=rarely or never, 2=about every month, 3=about every week, 4=more than once a week, 5=about every day.
Latent Class Analysis with Covariates
Covariates included gender (male as reference), race/ethnicity (White as reference), and parent education (three categories: low, median, and high, with high as reference). Family structure and region were excluded because of possible multicollinearity (with race/ethnicity and parent education) and the negative impact on statistical power of including many covariates. The ‘non-user’ class was set as the reference group. The results are reported in Table 4. Females were less likely than males to be in the ‘predominant marijuana user’ compared to the ‘non-user’ class (OR = 0.34, 0.18–0.65). Compared to children with high parent education (Bachelor or Graduate degrees), those with low parent education (<=high school degree) were more likely to be in the ‘predominant alcohol user’ class (OR = 1.57, 105–2.33) or the ‘predominant marijuana user’ class (OR = 3.32, 1.06–10.37).
Table 4.
Results of LCA with Covariates: Socio-demographic Differences (n= 2350)
| OR | [95% C.I.] | |
|---|---|---|
| Class 2. Predominant Alcohol User | ||
| Female vs Male | 0.86 | [0.56–1.31] |
| Race/Ethnicity (vs White) | ||
| African-American | 0.65 | [0.29–1.48] |
| Hispanic | 0.80 | [0.32–1.97] |
| Other | 0.82 | [0.31–2.15] |
| Parent Education (vs High) | ||
| Low (<=High school) | 1.57 | [1.05–2.33] |
| Median (Some college or technical school) | 1.15 | [0.86–1.54] |
| Class 3. Predominant Marijuana User | ||
| Female vs Male | 0.34 | [0.18–0.65] |
| Race/Ethnicity (vs White) | ||
| African-American | 0.97 | [0.23–4.07] |
| Hispanic | 1.26 | [0.76–2.08] |
| Other | 1.55 | [0.54–4.49] |
| Parent Education (vs High) | ||
| Low (<=High school) | 3.32 | [1.06–10.37] |
| Median (Some college or technical school) | 2.28 | [0.93–5.61] |
| Class 4. Predominant Polysubstance User | ||
| Female vs Male | 0.95 | [0.51–1.75] |
| Race/Ethnicity (vs White) | ||
| African-American | 0.47 | [0.07–3.16] |
| Hispanic | 1.52 | [0.58–3.99] |
| Other | 1.75 | [0.27–11.57] |
| Parent Education (vs High) | ||
| Low (<=High school) | 0.85 | [0.30–2.39] |
| Median ( Some college or technical school) | 1.02 | [0.32–3.25] |
Note. Significant odds ratios are in bold print. The latent class of Non-user was set as the reference group for the multinomial logistic regression model. For gender, race/ethnicity and parent education, the reference groups were male, White and high parent education (Bachelor and Graduate degree). Due to missing information on covariates, 174 participants were excluded for this analysis.
Associations
The four classes differed with respect to depressive and somatic symptomatology, which were included as distal outcomes with AUXILIARY option in Mplus, shown in Figure 1. Covariates were not adjusted for in this analysis. Non-users reported significantly lower levels of depressive and somatic symptoms than any other class, i.e., predominant polysubstance users (p < .01), predominant alcohol users (p < .01), and predominant marijuana users (p < .05). Predominant polysubstance users reported significantly (p < .01) higher levels of depressive symptoms than those in all other classes. Predominant polysubstance users also reported significantly (p < .01) higher levels of somatic symptoms when compared with non-users and predominant alcohol users. Predominant alcohol users and predominant marijuana users did not significantly differ in their reports of depressive or somatic symptoms.
Discussion
The primary study findings are (1) the existence of 4 classes of drug users: non-users, predominant drinkers, marijuana users, and polysubstance users; and (2) the predominant polysubstance users scored higher on depressive and somatic symptomatology. The overall prevalence of substance use in this sample is consistent with other national studies, such as the Monitoring the Future Study, and highlights its ubiquitousness among American youth. Past-year rates of marijuana use among 10th graders, for example, were very similar between the NEXT study (26%) and the 2011 MTF study (29%) [1]. Past-year rates of medication misuse among 10th graders were slightly higher in the NEXT study (8.7%) compared to the 2011 MTF study (range of 2.6–5.9%). This difference may stem from a definitional difference of medication misuse: NEXT asks about use of “medication to get high” whereas MTF asks about use of specific medications (e.g. Oxycontin, Vicodin, Ritalin) “not under a doctor’s orders.”
Regarding noteworthy demographic factors associated with substance use, children who live with both biological parents were less likely than children who live with step-parents to use marijuana, medication to get high, other illicit drugs, cigarettes, and binge drink. This finding is consistent with the well-supported notion that lack of parental monitoring is a risk factor for substance use [7;28].
The multiple classes defined by polysubstance use reported here compare with other studies [5;6], and underscore the considerable heterogeneity that exists among young substance users. In our sample, as in Add Health, abstainers comprised the largest and majority class of substance users[5]. By comparison, the 2009 YRBS, with a wider age range in the sample, alcohol users formed the largest class[6]. All three studies found that polysubstance users formed a smaller class of youth: NEXT with 7.6% of the sample characterized as predominant polysubstance users; YRBS with 13% frequent polysubstance users and 23% occasional polysubstance users; Add Health with 14% three substance use. Both the NEXT and YRBS identified that one poly drug class stood apart from the others in the seriousness of their substance-use patterns, symptomatology, and risk behaviors [6].
In addition to these findings, several results are particularly important and novel. First, the analyses found a strong representation of medication misuse in the predominant polysubstance user class (66%). Medication misuse is associated with serious adverse consequences including addiction and unintentional overdose [29;30]. Second, the predominant polysubstance users reported binge drinking at rates equal to, or even higher than, predominant alcohol users. Binge drinking during adolescence is a hazardous practice associated with significant short- and long-term negative consequences [31;32]. And while our study measures the use of various substances over a period of time and not simultaneous polysubstance use (e.g., misusing medications while drinking alcohol), other research reports high rates and negative consequences of simultaneous use in adolescents and college students [17;33]. Third, the predominant polysubstance users reported elevated levels of depressive symptoms and more somatic complaints such as headaches, stomachaches, and backaches, which often underlie depression [18;19]. The association of polysubstance use with mental health symptoms is concerning, as comorbid depressive psychopathology often predicts substance use, worsened clinical course, and medical illnesses among substance abusers [34–36]. Our findings strongly suggest that polysubstance users in the 10th grade may already be experiencing significant impairments and may be at high-risk for deleterious outcomes, and interpretation warranting confirmation by longitudinal analysis. Finally, polysubstance use may be a broad indicator of severity prevalent in over 7% of 10th graders, and reinforce the call for better substance use and mental health screening as well as referral to and availability of care are needed, as recommended by the American Academy of Pediatrics Association and the Society for Adolescent Medicine [37–40].
The results reported here should be considered in light of several limitations and strengths. Study limitations include the somewhat attenuated response rate, limited sample size relative to other national epidemiological studies, and the cross-sectional design. The strengths include the nationally representative sampling frame, oversampling of African-American and Hispanic youth to allow for robust comparisons across certain race/ethnic groups, assessment of depressive and somatic symptoms, and the examination of misuse of medications separately from other illicit drugs.
Implications and Contribution.
These findings underscore the ubiquitous yet heterogeneous nature of adolescent substance use and reveal that the multiple classes of substance users differ in terms of use patterns, somatic complaints, and depressive symptomatology. The differences among classes implicate polysubstance use as a broad indicator of severity deserving research and clinical attention.
Acknowledgements
Sources of funding and acknowledgements of support and assistance.
This project (contract number HHSN267200800009C) was supported in part by the intramural research program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the National Heart, Lung and Blood Institute (NHLBI), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and Maternal and Child Health Bureau (MCHB) of the Health Resources and Services Administration (HRSA), with supplemental support from the National Institute on Drug Abuse (NIDA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimer:
The views and opinions expressed in this paper are those of the authors and do not necessarily represent the views of the National Institute on Drug Abuse, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, or any other governmental agency.
Conflicts of Interest: No conflicts of interest are reported.
Reference List
- 1.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Ann Arbor, Institute for Social Research, The University of Michigan; 2012. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2011. [Google Scholar]
- 2.Mitchell CM, Plunkett M. The Latent Structure of Substance Use Among American Indian Adolescents: An Example Using Categorical Variables. American Journal of Community Psychology. 2000;28:105–125. doi: 10.1023/A:1005146530634. [DOI] [PubMed] [Google Scholar]
- 3.Connell C, Gilreath T, Aklin W, Brex R. Social-Ecological Influences on Patterns of Substance Use Among Non-Metropolitan High School Students. American Journal of Community Psychology. 2010;45:36–48. doi: 10.1007/s10464-009-9289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitesell NR, Beals J, Mitchell CM, Novins DK, Spicer P, Manson SM. Latent class analysis of substance use: comparison of two American Indian reservation populations and a national sample. J Stud Alcohol. 2006;67:32–43. doi: 10.15288/jsa.2006.67.32. [DOI] [PubMed] [Google Scholar]
- 5.Dierker LC, Vesel F, Sledjeski EM, Costello D, Perrine N. Testing the dual pathway hypothesis to substance use in adolescence and young adulthood. Drug Alcohol Depend. 2007;87:83–93. doi: 10.1016/j.drugalcdep.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Connell CM, Gilreath TD, Hansen NB. A multiprocess latent class analysis of the co-occurrence of substance use and sexual risk behavior among adolescents. J Stud Alcohol Drugs. 2009;70:943–951. doi: 10.15288/jsad.2009.70.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. [HHS Publication No. (SMA) 11–4658]. 9-1-2011. Rockville, MD, Substance Abuse and Mental Health Services Administration. NSDUH Series H-41 [Google Scholar]
- 8.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 9.Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- 10.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 11.Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- 12.Merikangas KR, Mehta RL, Molnar BE, et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- 13.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 14.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marmorstein NR, Iacono WG, Malone SM. Longitudinal associations between depression and substance dependence from adolescence through early adulthood. Drug Alcohol Depend. 2010;107:154–160. doi: 10.1016/j.drugalcdep.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burke JD, Jr, Burke KC, Rae DS. Increased rates of drug abuse and dependence after onset of mood or anxiety disorders in adolescence. Hosp Community Psychiatry. 1994;45:451–455. doi: 10.1176/ps.45.5.451. [DOI] [PubMed] [Google Scholar]
- 17.McCabe SE, Cranford JA, Morales M, Young A. Simultaneous and concurrent polydrug use of alcohol and prescription drugs: prevalence, correlates, and consequences. J Stud Alcohol. 2006;67:529–537. doi: 10.15288/jsa.2006.67.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchardt CM, Crosby RD. Somatic symptoms in anxious-depressed school refusers. J Am Acad Child Adolesc Psychiatry. 1997;36:661–668. doi: 10.1097/00004583-199705000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Egger HL, Costello EJ, Erkanli A, Angold A. Somatic complaints and psychopathology in children and adolescents: stomach aches, musculoskeletal pains, and headaches. J Am Acad Child Adolesc Psychiatry. 1999;38:852–860. doi: 10.1097/00004583-199907000-00015. [DOI] [PubMed] [Google Scholar]
- 20.National Institute on Alcohol Abuse and Alcoholism. NIAAA Newsletter. (NIH Publication No. 04-5346). 1-1-2004. [Google Scholar]
- 21.Dahlberg L, oal S, Swahn M, Behrens C. Measuring Violence-Related Attitudes, Behaviors, and Influences Among Youths: A Compendium of Assessment Tools. 2. 1-1-2005. Atlanta, GA, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control [Google Scholar]
- 22.Hetland J, Torscheim T, Aura L. Subjective health complaints in adolescence: Dimensional structure and variation across gender and age. Scandinavian Journal of Public Health. 2002;30:223–230. doi: 10.1080/140349402320290953. [DOI] [PubMed] [Google Scholar]
- 23.Akaike H. On the entropy maximization principle. In: Krishnaiah P, editor. Applications of statistics. Amsterdam: North-Holland; 1977. pp. 27–41. [Google Scholar]
- 24.Raftery A. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. [Google Scholar]
- 25.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- 26.Muthén LK, Muthén BO. Mplus User's Guide Fifth Edition. 1998 [Google Scholar]
- 27.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 28.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 29.Compton WM, Volkow ND. Abuse of prescription drugs and the risk of addiction. Drug Alcohol Depend. 2006;83(Suppl 1):S4–S7. doi: 10.1016/j.drugalcdep.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 30.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 31.Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: predictors and substance abuse outcomes. J Consult Clin Psychol. 2002;70:67–78. [PubMed] [Google Scholar]
- 32.Donath C, Grassel E, Baier D, Pfeiffer C, Bleich S, Hillemacher T. Predictors of binge drinking in adolescents: ultimate and distal factors – a representative study. BMC Public Health. 2012;12:263. doi: 10.1186/1471-2458-12-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCabe SE, West BT, Teter CJ, Boyd CJ. Co-ingestion of prescription opioids and other drugs among high school seniors: Results from a national study. Drug Alcohol Depend. 2012;126:65–70. doi: 10.1016/j.drugalcdep.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Arch Gen Psychiatry. 1987;44:505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- 35.Compton WM, III, Cottler LB, Jacobs JL, Ben-Abdallah A, Spitznagel EL. The role of psychiatric disorders in predicting drug dependence treatment outcomes. Am J Psychiatry. 2003;160:890–895. doi: 10.1176/appi.ajp.160.5.890. [DOI] [PubMed] [Google Scholar]
- 36.Harter MC, Conway KP, Merikangas KR. Associations between anxiety disorders and physical illness. Eur Arch Psychiatry Clin Neurosci. 2003;253:313–320. doi: 10.1007/s00406-003-0449-y. [DOI] [PubMed] [Google Scholar]
- 37.American Academy of Pediatrics. Coding for Pediatrics. 16 ed. Elk Grove Village, IL: American Academy of Pediatrics; 2011. [Google Scholar]
- 38.American Academy of Pediatrics. Policy statement - alcohol use by youth and adolescents: a pediatric concern. Pediatrics. 2010;5:1078–1087. doi: 10.1542/peds.2010-0438. [DOI] [PubMed] [Google Scholar]
- 39.U.S.PreventativeServices Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse. 2004 12-3-2012. [PubMed] [Google Scholar]
- 40.Kapphahn CJ, Morreale MC, Rickert VI, Walker LR. Financing mental health services for adolescents: a position paper of the Society for Adolescent Medicine. J Adolesc Health. 2006;39:456–458. doi: 10.1016/j.jadohealth.2005.12.013. [DOI] [PubMed] [Google Scholar]