Abstract
Previous studies have reported that majority of antiretroviral (ARV) treatment-naïve patients use traditional medicine (TM). Given that TM use is ubiquitous in South Africa especially for chronic conditions, there is a potential for ARV non-adherence and serious drug interactions among patients with HIV/AIDs who use TM. The motivating factors for TM use in HIV/AIDS patients on ARV and prophylaxis treatment have not been well defined in South Africa. This study aimed to investigate the prevalence, facilitators, predictors, and types of TM used among persons living with HIV/AIDS on antiretroviral treatment. The study was a cross-sectional survey which involved 100 participants enrolled at ARV clinics in two South African provinces. Univariate and bivariate analyses were performed to assess the relationships between variables and potential predictors of TM. Sixteen percent of participants on ARV reported TM use. Seventy-nine percent used TM prior to a diagnosis of HIV. Participants were more likely to use TM if they were from a rural province, female, older, unmarried, employed, had limited education, or were HIV-positive for less than five years. TM users reported utilizing herbal or medicinal mixtures that were claimed to heal all conditions. This study provides insights into the treatment modalities selected by patients with HIV/AIDS in South Africa who are receiving ARV. This study revealed that less than 20% of participants co-used TM and ARV. However, close to 80% of participants utilize TM before contracting HIV, which is in keeping with approximate estimates by the WHO.
Keywords: AIDS, HIV infection, traditional medicine, alternative medicine, ARV
Introduction
Currently, there are approximately 20.8 million to 24.1 million individuals in sub-Saharan Africa living with the Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (HIV/AIDS) (UNAIDS and WHO, 2009). Compared to other countries, South Africa is among the most severely affected by the HIV pandemic, with approximately 5.2 million people living with HIV and 1,000 AIDS-related deaths occurring every day (Statistics South Africa, 2009). The availability of antiretroviral (ARV) drug treatment for HIV-positive people enables them to maintain their health and lead relatively normal lives. Access to ARV therapy (ART) was initially limited to relatively few, due to the slow response of the South African Government to make ARV available to those who needed it. The Ministry of Health however, was actively promoting the use of traditional medicines (TM) (Mills et al., 2005).
According to the World Health Organisation, Traditional medicine is defined as the sum total of knowledge, skills and practices based on the theories, beliefs and experiences indigenous to different cultures that are used to maintain health, as well as to prevent, diagnose, improve or treat physical and mental illnesses (WHO, 2003). In developing countries, the use of traditional medicine has been based on availability, accessibility, cultural and social acceptability and mind/body/spirit connection (Bodeker and Kroneberg, 2002; Elujoba et al., 2005; Homsy et al., 2004; Liverpool et al., 2004). The World Health Organisation estimates that up to 80% of people in Africa make use of traditional medicine for primary health care (WHO, 2003). Many South Africans weigh the benefits of using TM against benefits offered by conventional “western” medicine, especially when considering the treatment of chronic conditions. There is limited information about the use of TM among patients with HIV/AIDS receiving ART in South Africa, and if it is a common practice, little is known about how it is being used and how the use of TM may affect patient outcomes. A particular concern among healthcare practitioners is that the use of TM may promote non-adherence to life-prolonging ART regimens. Also, the use of TM in combination with ARV may reduce the efficacy of ARV or produce adverse drug effects. Alternatively, TM may diminish side effects and toxicities of ARV and promote adherence. All of these are questions yet to be answered. There is a need for better understanding of the use of TM among patients already receiving treatment for HIV/AIDS, especially in South Africa.
This pilot study aimed to provide an assessment of the prevalence, facilitators, barriers and predictors of TM use with and without prophylaxis, and/or ARV among people living with AIDS (PLWA). The objectives were to identify how patients self-manage their symptoms of HIV/AIDS; to identify patients receiving prophylaxis and/or ARV who also use TM and/or other therapies; to identify the types of TM being used; to identify patients who discontinued ARV and utilize TM; and to explore reasons for use of TM among patients.
Methodology
Study setting
This pilot study was conducted in two sites in South Africa: (1) Khayelitsha sub-district, an urban township in Cape Town with the highest antenatal HIV rate (32%) in the Western Cape Province; and (2) in the Sisonke Health District in rural KwaZulu-Natal (KZN) province with an estimated antenatal HIV rate of 28%.
Study Design and Sample
This study used a cross-sectional study design and was conducted from January through August 2009. A non-random sampling procedure was used to select 50 patients per each facility surveyed. Using this sampling procedure, all patients meeting the inclusion criteria described below were recruited at the facility on the day of the interview until the required sample size was achieved. Patients were excluded if they did not wish to participate, or refused informed consent.
Study participants
Eligible participants were either men or women aged18 years and older. In addition, eligible participants were required to have a diagnosis of HIV/AIDS, had attended one of the clinic sites, and had received an ARV treatment regimen and/or prophylaxis as recommended by the South African National Guidelines for People Living with HIV/AIDS (National Department of Health, South Africa, 2004).
Data Collection
Data were collected utilizing a questionnaire administered by experienced interviewers. A structured questionnaire was developed based on the existing literature from studies of TM and ARV (Challand, 2005; Risa et al., 2002). The survey questionnaire which was administered to the patients included data on demographic information—gender, age, education, employment, income; health status and medical care; ARV treatment/regimen; traditional medicine knowledge and practice. The symptoms section of the questionnaire was derived from a standardized instrument (Banda et al., 2007; Peltzer and Phaswana-Mafuya, 2008). The following information was also collected from each participant: socio-demographic data; health status; knowledge and use of TM; perceptions of TM; symptoms; and symptom management. All interviewers had been trained for one week on the tools and operating procedures for data collection. Furthermore, prior to the start of data collection, each interviewer completed a refresher course on general research methodology. Informed consent was obtained from all participants. Questionnaires were administered in the local language for each region (i.e.: Zulu in KwaZuluNatal and isiXhosa in the Western Cape Province).
Ethical Considerations
The study protocol was approved by the Institutional Review Board and Ethics Committees at the Universities of KwaZulu Natal and Stellenbosch University in South Africa as well as the University of Missouri-Columbia in the United States of America (USA). Permission to conduct the study at both ARV sites was granted by the Department of Health.
Statistical Methods
Due to the small sample size used for this study, descriptive statistics were utilized predominantly. However, for exploratory purposes bivariate logistic regression analyses were implemented. The distribution of HIV/AIDS symptoms were ranked by the frequency in which they were reported in order to compare TM users to those who reported use of conventional medicines. The ranks were also evaluated to compare symptoms reported by patient's gender. Additionally, symptoms of HIV/AIDS in the present study were compared to those described in Makoae et al (2005). All statistical analyses were performed using SAS 9.1.3.
Results
Demographic and Clinical Characteristics
Of the 100 participants recruited in this study, 97 participants, including 50 (51.5%) from the urban, KZN region and 47 (48.5%) from the rural Khayelitsha completed the study questionnaire. There were 29 (29.9%) male participants and 68 (70.1%) females. Three participants were excluded due to incomplete data. Demographic characteristics are described in Table (i) a & b. The median age for the sample was 37years (interquartile range 12.0). More than 79% of the respondents were classified as WHO HIV stage I or II. The majority of participants (73.2%) were never married; 16.5% were married or cohabiting, and 10.3% were either divorced or widowed. Most participants (83.5%) reported having children and majority were unemployed (79.4%). However, 39.2% reported that they had received funding from a government grant, whereas 38.1% reported not having any income at all. Nearly all respondents (92.8%) reported that they did not have health insurance.
Table 1 a.
Distribution of Social and Demographic Characteristics for Total HIV/AIDS Sample by gender
| Personal Characteristics | Female 68(70.1%) |
Male 29(29.9%) |
Total 97(100%) |
| Age (yr) | |||
| Median | 35 | 43 | 37 |
| IQR | 11.5 | 12.5 | 12.0 |
| Education level | |||
| No schooling | 7(10.3) | 9(31.0) | 16(16.5) |
| Less than high school | 52(76.5) | 19(65.5) | 71(73.2) |
| Metric and higher education | 9(13.2) | 1(3.4) | 10(10.3) |
| Where do you live? | |||
| Urban (WC) | 39(57.4) | 11(37.9) | 50(51.5) |
| Rural (KZN) | 29(42.6) | 18(62.1) | 47(48.5) |
| Marital status | |||
| Never married | 57(83.8) | 14(48.3) | 71(73.2) |
| Married or cohabitating | 7(10.3) | 9(31.0) | 16(16.5) |
| Divorced or widowed | 4(5.9) | 6(20.7) | 10(10.3) |
| Employment Status | |||
| Employed | 15(22.1) | 5(17.2) | 20(20.6) |
| Unemployed | 53(77.9) | 24(82.8) | 77(79.4) |
| What is your source of income? | |||
| None | 30(44.1) | 7(24.1) | 37(38.1) |
| Monthly salary (formal employment) | 10(14.7) | 2(6.9) | 12(12.4) |
| Informal employment | 8(11.8) | 2(6.9) | 10(10.3) |
| Grant | 20(29.4) | 18(62.1) | 38(39.2) |
| Do you have health insurance? | |||
| Yes | 6(8.8) | 1(3.4) | 7(7.2) |
| No | 62(91.2) | 28(96.6) | 90(92.8) |
| Do you have children? | |||
| Yes | 56(82.4) | 25(86.2) | 81(83.5) |
| No | 12(17.6) | 4(13.8) | 16(16.5) |
| When were you diagnosed HIV positive? | |||
| Less than a year | 11(16.2) | 9(31.0) | 20(20.6) |
| 1–5 years | 45(66.2) | 16(55.2) | 61(62.9) |
| More than five years | 12(17.6) | 4(13.8) | 16(16.5) |
| Which WHO HIV stage have you been told you are in? | |||
| Stage I | 34(50.0) | 18(62.1) | 52(53.6) |
| Stage II | 21(30.9) | 4(13.8) | 25(25.8) |
| Stage III | 11(16.2) | 4(13.8) | 15(15.5) |
| Stage IV (AIDS stage) | 1(1.5) | 1(3.4) | 2(2.1) |
| Not indicated/unknown | 1(1.5) | 2(6.9) | 3(3.1) |
| Which medication currently taking? | |||
| Only Prophylaxis | 4(5.9) | 4(13.8) | 8(8.2) |
| Only ART | 36(52.9) | 8(27.6) | 44(45.4) |
| Prophylaxis and ART | 16(23.5) | 6(20.7) | 22(22.7) |
| Traditional Medicine and other | 4(5.9) | 3(10.3) | 7(7.2) |
| Other | 8(11.8) | 8(27.6) | 16(16.5) |
| In general, how are you self-managing the symptoms? | |||
| Conventional medicine | 24(35.8) | 15(51.7) | 39(40.6) |
| Conventional medicine and TM | 3(4.5) | 3(10.3) | 6(6.3) |
| Conventional medicine and other | 10(14.9) | 2(6.9) | 12(12.5) |
| Traditional medicine and other | 3(4.5) | 1(3.4) | 4(4.2) |
| Assistance of family, Spiritual care & Prayers | 26(38.8) | 7(24.1) | 33(34.4) |
| Other | 1(1.5) | 1(3.4) | 2(2.1) |
| Are you using any Traditional Medicine? | |||
| Yes | 11(16.2) | 4(13.8) | 15(15.5) |
| No | 57(83.8) | 25(86.2) | 82(84.5) |
| Is anyone monitoring your CD4 count/ viral load? | |||
| Yes | 68(100) | 29(100) | 97(100) |
| In addition to HIV, do you have other medical conditions? | |||
| Yes | 17(25.0) | 9(31.0) | 26(26.8) |
| No | 51(75.0) | 20(69.0) | 71(73.2) |
Table 1b.
Distribution of Select Characteristics for Traditional Medicine Users by gender (n=14 one missing from 15 respondents)
| Characteristics | Female n(%) |
Male n(%) |
Total n(%) |
| TM use prior to HIV diagnosis | |||
| Yes | 7(70.0) | 4(100.0) | 11(78.6) |
| No | 3(30.0) | 0(0.0) | 3(21.4) |
| Who advised you to use TM? | |||
| Self | 4(40.0) | 2(50.0) | 6(42.9) |
| Parents and Friends | 4(40.0) | 2(50.0) | 6(42.9) |
| Other | 2(20.0) | 0(0.0) | 2(14.3) |
| Traditional Medicine is administered by | |||
| Self | 9(90.0) | 4(100.0) | 13(92.9) |
| Traditional healer | 1(10.0) | 0(0.0) | 1(7.1) |
| Have you told your doctor/nurse that you are using TM? | |||
| Yes | 0(0.0) | 1(25.0) | 1(7.1) |
| No | 10(100.0) | 3(75.0) | 13(92.9) |
| Have you told your traditional practitioner/healer that you are on ART? |
|||
| Yes | 4(40.0) | 2(50.0) | 6(42.9) |
| No | 6(60.0) | 2(50.0) | 8(57.1) |
| Have you ever discontinued ART? | |||
| No | 10(100) | 4(100) | 14(100) |
Most respondents (63%) reported living with HIV for a period of 1 to 5 years. All respondents stated that their CD4 count and viral load was being monitored regularly (this was also confirmed from the patient treatment card). Twenty-seven percent of the participants reported having other medical conditions besides HIV/AIDS.
Respondents employed a variety of methods for self-managing their symptoms of HIV/AIDS. Most patients indicated that they had been managing their symptoms using conventional medicine (41%) or were being assisted by their family who provided them with spiritual care and prayers (34%). The remaining respondents indicated that they were using either a combination of therapies or “other” treatment type. Regardless of the treatment type reported, none of the respondents indicated that they had ever discontinued using ART for HIV/AIDS.
Traditional Medicine
Compared to conventional medicine, fewer patients reported that they had used any TM (84.5% versus 15.5%, respectively). When TM was used it was generally self-administered (92.9%) and rarely administered by a traditional healer (7.1%). Most of the patients who responded to this question reported using TM prior to being diagnosed with HIV (78.6%). An equal proportion of respondents also indicated that either they had decided to use TM on their own, or that their decision to use TM was influenced by family and friends (42.9%, respectively).
The participants provided a variety of reasons for why they had chosen to use TM. A similar number of respondents indicated that they had used TM to gain strength, increase their appetite, and relieve symptoms of numbness, ulcers, and bad dreams (33%, respectively). Participants also indicated that they had used TM to stop the spread of shingles (8.3%) or for some other, unspecified reason (24.8%). The types of TM used also differed between patients. Approximately half of the patients indicated that they had taken a form of TM consisting of herbal mixtures and other medicinal mixtures. The most popular herbal mixture used was ubhejane which is believed to effectively treat all bodily conditions.
Most patients (92.9%) who had used TM chose not to disclose their use to a healthcare professional. However, 42.9% of respondents indicated that they had shared information regarding their use of ARV with a TM practitioner/healer. An exploration of the reasons why most patients chose not to disclose their use of TM to a healthcare provider revealed that respondents believed that that disclosing this information would result in a lack of support and understanding, as well as the potential for punitive repercussions.
Symptoms of HIV/AIDS
Table (ii) presents the 25 most common symptoms of HIV/AIDS reported by study participants. The top 10 reported symptoms were weakness (61.9%); headache (59.8%); fever (58.8%); muscle aches (55.7%); thirst (50.5%); numbness/tingling of feet or toes, painful joints, and fatigue (47.4%, respectively); depression and chills (46.4%, respectively). Most respondents reported experiencing more than one symptom, and 5 symptoms were experienced by at least 50% of the sample. When all of the reported symptoms were evaluated, it was determined that 29 symptoms were experienced by at least 33% of the sample.
Table 2.
Top 25 Ranked HIV/AIDS Symptoms Reported
| Symptoms | Rank | Frequency | Percentage |
| Weakness | 1 | 60 | 61.9 |
| Headache | 2 | 58 | 59.8 |
| Fever | 3 | 57 | 58.8 |
| Muscle Aches | 4 | 54 | 55.7 |
| Thirst | 5 | 49 | 50.5 |
| Numbness: Tingling of feet or toes | 7 | 46 | 47.4 |
| Painful Joints | 7 | 46 | 47.4 |
| Fatigue | 7 | 46 | 47.4 |
| Depression | 9.5 | 45 | 46.4 |
| Chills | 9.5 | 45 | 46.4 |
| Memory Loss | 11 | 44 | 45.4 |
| Headache & Dizziness | 12 | 42 | 43.3 |
| Blurred vision | 13 | 41 | 42.3 |
| Itchy Skin | 15 | 40 | 41.2 |
| Coughing | 15 | 40 | 41.2 |
| Shortness of Breath with Activity | 15 | 40 | 41.2 |
| Night Sweats | 17 | 38 | 39.2 |
| Difficulty Concentrating | 18 | 37 | 38.1 |
| Fear & Worries | 22 | 34 | 35.1 |
| Gastrointestinal: Gas or Bloating | 22 | 34 | 35.1 |
| Gastrointestinal: Nausea | 22 | 34 | 35.1 |
Only two symptoms were experienced by at least 50% of the sample and 15 symptoms were experienced by at least 33%. The most prevalent symptoms were more likely to be experienced by a greater percentage of patients with HIV/AIDS in this South African study than in the study reported by Makoae et al. (2005).
Descriptive Data for Personal Characteristics and Severity of Illness (N=97)
Symptoms of HIV/AIDS in Conventional Medicine and TM Users
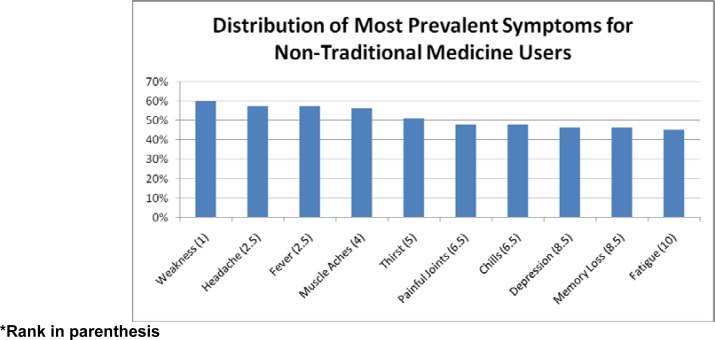
Figures 1 and 2 present the distribution of the most prevalent HIV/AIDS symptoms among conventional medicine and TM users, respectively. The most prevalent symptoms reported by conventional medicine users were: weakness, headache, fever, muscle aches, thirst, painful joints, chills, depression, memory loss, and fatigue.
Figure 1.
Distribution of most prevalent symptoms for non-traditional medicine users*
*Rank in parenthesis
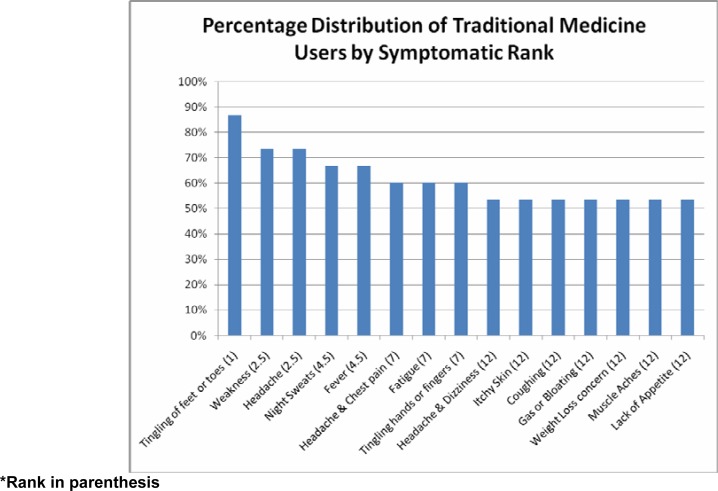
Figure 2.
Distribution of most prevalent symptoms for traditional medicine users*
*Rank in parenthesis
The top ranked symptoms reported by patients who used TM are shown in Figure 2. Five of the top 10 symptoms from conventional medicine users (thirst, painful joints, chills, depression and memory loss) were not the top symptoms reported by the TM users.
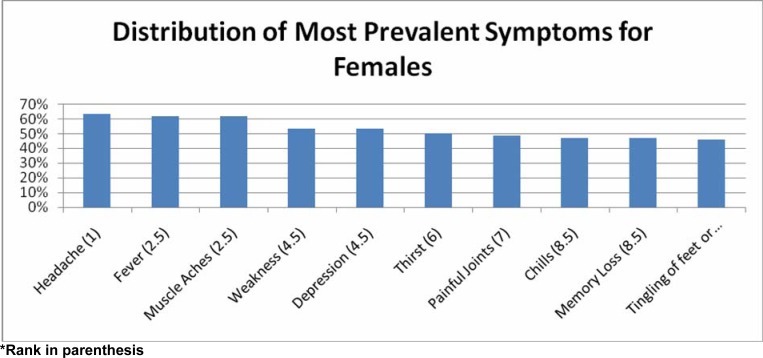
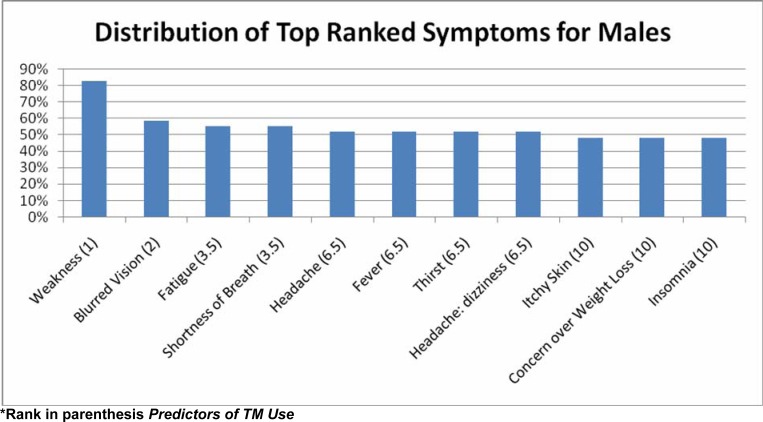
The top ranked symptoms by gender are presented in Figures 3 and 4. The prevalence and types of symptoms reported differed by the participant's gender. Six of the 10 top ranked symptoms experienced by females (muscle aches, depression, painful joints, chills, memory loss and tingling of feet or toes) were not among the top ranked symptoms reported by males.
Figure 3.
Distribution of most prevalent symptoms for females*
*Rank in parenthesis
Figure 4.
Distribution of most prevalent symptoms for males*
*Rank in parenthesis Predictors of TM Use
Selected potential predictors of TM use are reported in Table (iii). Respondents were more likely to report using TM if they were from the rural setting in KZN province (21.3%, n=10) than from the urban setting in the Western Cape Province (10%; n=5). More females (16.2%; n=11) were likely to report using TM than males (13.8%; n=4). In addition, older respondents (ages 38 to 62) were more likely than younger respondents (ages 19 to 37) to use TM (17.4% vs. 13.7%, respectively). Those with no formal education were more likely than those with at least some formal education (31.3% vs. 12.4%) to report usage of TM. Furthermore, patients who were not married were more likely to report using TM than patients who were (25% vs. 13.6%, respectively), the employed were more likely than the unemployed (20% vs. 14.3%, respectively), and those who had been HIV-positive for less than five years were more likely to report using TM than those who had been HIV-positive for five years or more (16.1% vs. 12.5, respectively).
Table 3.
Traditional Medicine by Select Potential Predictors
| PREDICTOR | Traditional Medicine, % (N) | |
| Gender | Male | 13.8 (4) |
| Female | 16.2 (11) | |
| Age | Young (ages 19–37) | 13.7 (7) |
| Older (ages 38–62) | 17.4 (8) | |
| Residence | Urban | 10.0 (5) |
| Rural | 21.3 (10) | |
| Education | No Schooling | 31.3 (5) |
| Some Education | 12.4 (10) | |
| Province | WC | 10.0 (5) |
| KZN | 21.3 (10) | |
| Marital Status | Married | 13.6 (11) |
| Not Married | 25.0 (4) | |
| Household Type | Spouse and/or Kids | 14.8 (12) |
| Other | 20.0 (3) | |
| Employment Status | Employed | 20.0 (4) |
| Not Employed | 14.29 (11) | |
| Income Source | No Income Source | 6.5 (2) |
| Source of Income | 21.7 (13) | |
| Health Insurance | Insurance | 14.3 (1) |
| No Insurance | 15.6 (14) | |
| Children | Yes | 17.8 (14) |
| No | 6.3 (1) | |
| HIV positive 5+ yrs | Yes | 12.5 (2) |
| No | 16.1 (13) | |
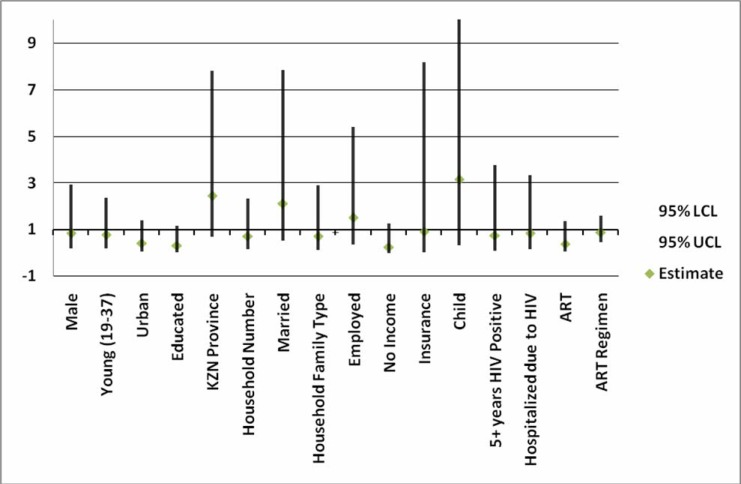
Bivariate logistic regression results from selected potential predictors of TM usage are shown in Figure 5.
Figure 5.
Bivariate Logistic Regression of Traditional Medicine by Select Potential Predictors
None of the relationships between patient characteristics and TM use were statistically significant. This is most likely due to the small sample size analyzed in this pilot study. However, some of the findings are worth noting. Those in the rural setting in KZN province who were married and those with children were more than twice as likely to use TM. In the urban setting in the Western Cape Province, those with some formal education, no income sources, and those reporting using ART, were all twice as unlikely to use TM.
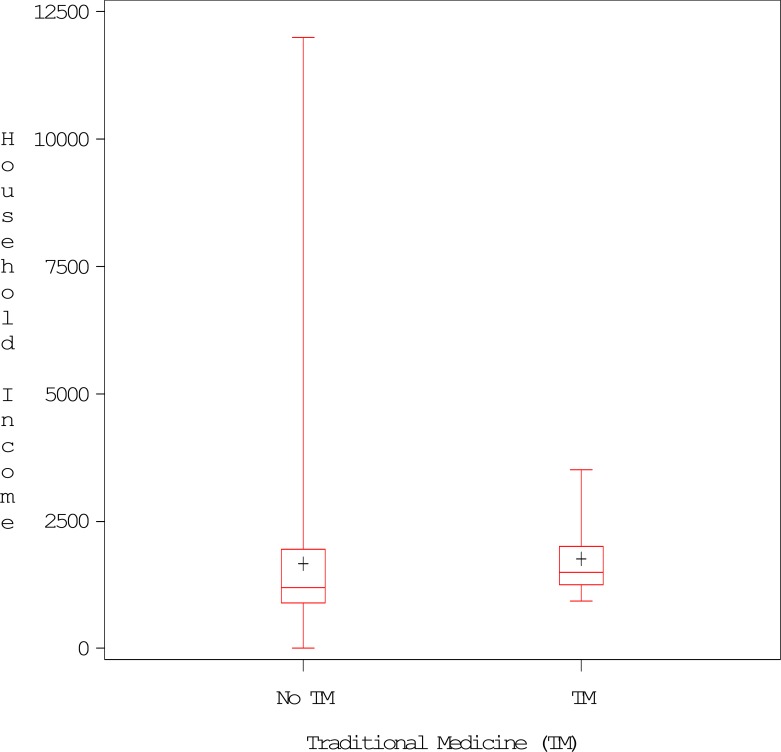
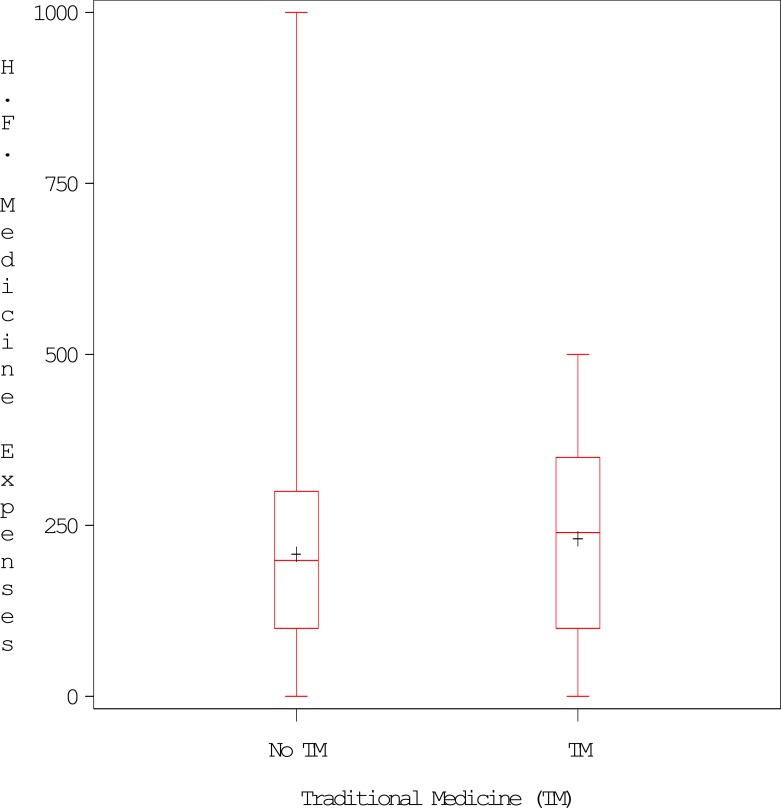
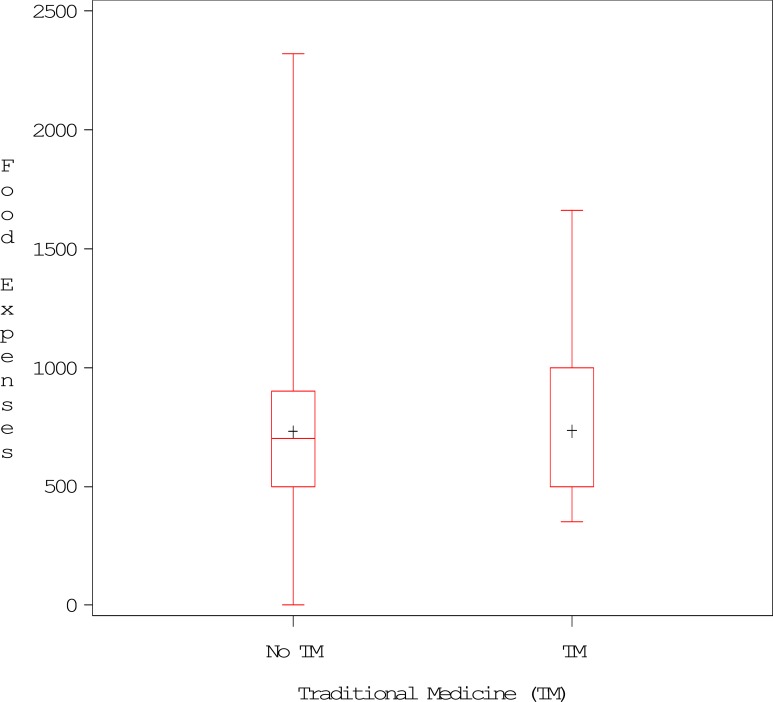
Figures 6 to 8 display TM usage by monthly household income; monthly food expenses; and by monthly healthcare-facility-related medical expenses, respectively. In this study, TM users had higher median household incomes (displayed in the local currency of South African Rands [R]) than conventional medicine users (R1500 vs R1200, respectively). Users of TM also had lower monthly food expenses (R500 vs R700, respectively) and higher healthcare-facility-related medical expenses than non-users (R240 vs. R200, respectively).
Figure 6.
Box plots of Traditional Medicine Usage by Monthly Household Income*
Figure 8.
Box plots of Traditional Medicine Usage by Monthly Healthcare Facility Medicine Expenses‡
Figure 7.
Box plots of Traditional Medicine Usage by Monthly Food Expenses†
Discussion
This pilot study provides a foundation for future research by determining the prevalence of and predictors for TM use among PLWA on prophylaxis treatment and ARV in both rural and urban settings. Approximately 15% of participants reported using TM; however, this percentage is lower than the estimates reported in other surveys (Challand, 2005; Dhalla et al., 2006; Kasilo, 2000; Peltzer et al., 2008; Risa et al., 2002; Wiwanitikit, 2003). Most participants in this pilot study admitted that they did not disclose their use of TM to healthcare workers out of fear of repercussions (because they were combining prescribed treatments with TM against the advice of healthcare workers). The participants also stated that admitting to use of TM may negatively impact the healthcare they received (Banda et al., 2007). It is believed that the true prevalence of TM use exceeds the prevalence observed during this study. Respondents in rural areas were more likely to use TM in combination with ART or prophylaxis, while the respondents from the urban site tended to rely on family support, spiritual care and prayer. Participants who reported using TM indicated that they started using it before they were diagnosed with HIV/AIDS. Once ART were prescribed, respondents continued to use TM, but did not disclose their use to a healthcare provider due to the reasons previously described. However, the respondents did disclose their use of TM to their traditional healer. Patients who disclosed their use of TM to a traditional healer did so because they had spent time with the traditional healer and had established a relationship of trust and a cultural connection. Traditional healers have been known to provide client-centered, personalized care that is tailored to meet the needs and expectations of their patients. This establishes traditional healers as strong agents for communicating health and social issues. In South Africa, traditional healers enjoy greater credibility than do health workers, especially with respect to social and spiritual matters (Dambisya and Tindimwebwa, 2003; UNAIDS, 2002). Most participants who had used TM were in the early stages of HIV. These respondents reported that they had been using TM for reasons other than HIV and continued with TM after they had been diagnosed with HIV. Once the HIV had progressed, these participants tended to rely primarily on family support, prayer, spiritual healing, and other forms of treatment. However, additional studies may be useful for exploring the reasons why patients in a higher disease stage choose to use treatments other than TM or conventional medicine.
There was a difference in the ARV regimens prescribed at the two study sites, with most participants in the KZN province (85.1%) receiving regimen 1A (DAT, 3TC, EFV), while participants in the Western Cape Province, received a variety of regimens. However, all of the prescribed regimens were in alignment with the South African Antiviral Treatment Guidelines for ART (National Department of Health South Africa, 2004). It is therefore not surprising that 45% of all patients were on regimen 1A (D4T, 3TC, EFV) and 1B; and 2.7% were on regimen 1A, 1B and 2.
The South African National Guidelines states that cotrimoxazole prophylaxis must be continued in all patients on ART until the CD4 count is >200 cells/mm3 (National Department of Health South Africa, 2004). In this study, 22 (22.7%) respondents were on both prophylaxis and ARV, which adheres to the guidelines.
There was some uncertainty with regards to the patient's knowledge of their disease stage. Only 2 (2.06%) patients reported being in stage IV, while 95% reported that they were in stages I–III. However, these data contradict the number of years each patient reported that they had been living with HIV. Twenty-one percent of participants reported living with HIV for less than one year, 63%reported that they had been living with HIV for one to five years, and 17% for more than five years. In addition, according to South African guidelines, the criteria for ARV treatment includes a CD4 count of <200 cells/mm3 irrespective of WHO stage, or WHO Stage IV disease irrespective of CD4 count; the patient must also express a willingness and readiness to adhere to their ARV regimen. These criteria confirm that more than the reported 2% of patients were actually in WHO stage IV.
As reported, the top 10 symptoms of HIV/AIDS included: weakness, headaches, fever, muscle aches, thirst, painful joints, fatigue, tingling of feet/toes, depression and chills. Most of the symptoms were similar to those previously reported in the literature (Banda et al., 2007; Peltzer and Phaswana-Mafuya, 2008; Voss et al., 2007). Makoae et al. (2005) also ranked symptoms of HIV/AIDS. In their report of participants in Botswana, Lesotho, South Africa, and Swaziland, the top 10 reported symptoms were similar to those reported by our South African study population. However, instead of thirst, numbness/tingling of feet and toes, and fever reported by participants in the current study, respondents in the Makoae et al. (2005) study reported concerns over weight loss (47.9%), various fears or worries (45.4%), coughing (45.2%), lack of appetite (44.4%) and night sweats (40.6%).
The majority of participants using TM reported doing so in order to increase their level of energy and to improve their strength. These results correlate with reported symptoms of muscle weakness and fatigue. There were many other reasons why some participants chose to use TM including a belief that TM could counteract the effects of witchcraft. Most respondents who reported using TM indicated that they had taken a medicinal mixture that was believed to heal all conditions (zifozonke). The most popular medicinal mixture was ubhejane. This was most likely because using the mass media to disseminate this message, the former Minister of Health recommended the use of this mixture (Bateman, 2006). In addition, some participants reported taking vitamins. Similar findings of participants using a variety of remedies including vitamins and herbs have been reported (Kroesena et al., 2002).
There were several limitations to this pilot study including the small sample size; the small number of male participants; an inability to verify each participant's response to questions regarding their disease stage; and possible selection bias due to recruitment occurring at the two ARV clinics. Due to the small sample size, the results are not generalizeable and are limited to similar populations with HIV/AIDS who attend ARV/ART clinics.
There were numerous challenges experienced during the execution of this study. According to the field workers, there was an inability for most participants to understand the differences between HIV and AIDS; to most participants, they were one and the same. In addition, only one participant was able to differentiate between prophylaxis and ARV. None of the participants knew what treatment regimen they were receiving, instead, field workers had to obtain this information from medical cards and/or medical records; and only one participant was able to recall their prescribed tablets and pills by name. TM is used as a complement to ART regimens and less often as a replacement. Therefore healthcare providers should openly and non-judgmental ask patients about their TM use for better understanding and appropriate treatment.
Conclusion
This pilot study provides insight into the treatment modalities selected by patients with HIV/AIDS in South Africa who are receiving ARV. However, attempts at estimating the prevalence of TM use in the current study revealed TM usage at a lower rate than reported in other surveys. There is a need to better understand the use of traditional medicine with conventional medicine for HIV/AIDS prophylaxis and/or treatment. Understanding that patient's may use both of these treatment types and others, is especially important in rural areas where traditional medicine is also utilized for the treatment of chronic conditions including those related and unrelated to HIV/AIDS. As patients advance in their HIV/AIDS disease, they are more likely to use alternative therapies such as prayer, spirituality, and family support to treat their condition. These alternative therapies need to be better understood and assessed as viable forms of healing. In the current study, respondents with fewer years of education were unable to differentiate between HIV and AIDS. In general, patients had limited knowledge about their disease stage and only a small proportion of participants were aware of their prescribed treatment regimen. Therefore, it is important that the healthcare workers remain vigilant in their efforts to educate patients with HIV/AIDS. The failure of governments to appropriately and quickly respond to the AIDS pandemic is especially disconcerting and ethically challenging. Currently, many individuals with CD4 counts below 350 are not able to access treatment. The high-cost of treatment, governments incapable of or unwilling to provide ART, and the available selection of treatments may limit access to life-prolonging therapies. Many believe that the peak response of ART has been reached and the future looks very grim. The need to find low-cost, local alternatives that can help individuals manage their disease as best as possible is both ethical and imperative. There is also a need to better understand the role of traditional healers in the treatment of HIV/AIDS and to explore whether collaboration or cooperation with traditional healers will ultimately improve patient outcomes and provide healthcare professionals with more reliable estimates of the prevalence, frequency, and the duration of TM use. Subsequent studies utilizing larger and more diverse samples are needed to provide a more accurate estimate of the true prevalence of TM among patients already on ARV, as they will be better powered to detect significant differences in potential clinical and demographic predictors of use. Additional goals of any future research endeavour include an assessment of the benefits and/or risks associated with TM use, an exploration of the impact of HIV/AIDS treatment availability and cost on health outcomes in South Africa; and an evaluation of the role of TM in ameliorating access to inexpensive treatment options.
Acknowledgment
The authors extend sincere gratitude to field workers, Sybil Xapa and Thabisile Mkhize for their assistance in the collection of the data. Appreciation extended to the patients and staff at the clinics in Khayelitsha and KwaZulu Natal. In addition, appreciation is expressed to UWC SOPH staff, especially, Jeannine Uwimana for her role as coordinator in KZN, Moise Muzigaba for assisting with the coordination and logistics during the study period and Oluwaseyi Aboyade who assisted in the preparation of this manuscript. This project was supported by Grant U19AT003264 from the National Centre for Complementary & Alternative Medicine and the Fogarty International Centre. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Centre for Complementary & Alternative Medicine, the National Institutes of Health or the Fogarty International Centre
List of Abbreviations
- AIDS
Acquired Immune Deficiency Syndrome
- ART
ARV treatments
- ARV
Antiretroviral
- HIV
Human Immunodeficiency Virus
- KZN
Kwa-Zulu Natal
- PLWA
People living with AIDS
- TM
Traditional medicine
- WHO
World Health Organisation
- UNAIDS
Joint United Nations Program on HIV/AIDS
Footnotes
Income is in ZAR units
Monthly food expenses are in ZAR units
Medicine expenses are in ZAR units
References
- 1.Banda Y, Chapman V, Goldenberg RL, Stringer JS, Culhane JF, Sinkala M, Vermund SH, Chi BH. Use of Traditional Medicine among Pregnant Women in Lusaka, Zambia. J Alternative Compl Med. 2007;13(1):123–127. doi: 10.1089/acm.2006.6225. [DOI] [PubMed] [Google Scholar]
- 2.Bateman C. Taking ubhejane by the horn(s) SAMJ. 2006;96(5):382–386. [PubMed] [Google Scholar]
- 3.Bodeker G, Kronenberg F. A public health agenda for traditional, complementary, and alternative medicine. Am J Publ Health. 2002;92(10):1582–1591. doi: 10.2105/ajph.92.10.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Challand S. A survey of the use of medicinal plants and other traditional medicine in Kasese District. Uganda Trop Doct. 2005;35:222–224. doi: 10.1258/004947505774938512. [DOI] [PubMed] [Google Scholar]
- 5.Dambisya YM, Tindimwebwa G. Traditional Remedies in Children around Eastern Cape, South Africa. East Afr Med J. 2003;80(8):402–405. doi: 10.4314/eamj.v80i8.8730. [DOI] [PubMed] [Google Scholar]
- 6.Dhalla S, Chan KJ, Montaner JS, Hogg RS. Complementary and alternative medicine use in British Columbia -a survey of HIV positive people on antiretroviral therapy. Complement Ther Clin Pract. 2006;12(4):242–248. doi: 10.1016/j.ctcp.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Elujoba AA, Odeleye OM, Ogunyemi CM. Review- Traditional medicine development for medical and dental primary health care delivery system in Africa. AJTCAM. 2005;2(1):46–61. [Google Scholar]
- 8.Homsy J, King R, Tenywa J, Kyeyune P, Opio A, Balaba D. Defining minimum standards of practice for incorporating African traditional medicine into HIV/AIDS prevention, care, and support: A Regional Initiative in Eastern and Southern Africa. J Alternative Compl Med. 2004;10(5):905–910. doi: 10.1089/acm.2004.10.905. [DOI] [PubMed] [Google Scholar]
- 9.Kasilo O WHO, author. Traditional medicine, better science, policy and services for health development. Awaji Island, Japan: Hyogo Prefecture; 2000. Traditional African medicine; pp. 86–94. [Google Scholar]
- 10.Kroesena K, Baldwina CM, Brooks AJ, Bella IR. US Military Veterans' Perceptions of the Conventional Medical Care System and their Use of Complementary and Alternative Medicine. Family Practice. 2002;19(1):57–64. doi: 10.1093/fampra/19.1.57. [DOI] [PubMed] [Google Scholar]
- 11.Liverpool J, Alexander R, Johnson M, Ebba EK, Francis S, Liverpool C. Western medicine and traditional healers: partners in the fight against HIV/AIDS. J Natl Med Assoc. 2004;96(6):822–825. [PMC free article] [PubMed] [Google Scholar]
- 12.Makoae LN, Seboni NM, Molosiwa K, Moleko M, Human SP, Sukati NA, Holzemer WL. The Symptom Experience of People Living with HIV/AIDS in Southern Africa. J Assoc Nurses AIDS Care. 2005;16(3):22–23. doi: 10.1016/j.jana.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Mills E, Cooper C, Dugald S, Kanfer I. African herbal medicines in the treatment of HIV: Hypoxis and Sutherlandia. An overview of evidence and pharmacology. Nutrition Journal. 2005;4:19. doi: 10.1186/1475-2891-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Department of Health, South Africa, author. “National Antiretroviral Treatment Guidelines”. Jacana Printed by Minuteman Press; 2004. ISBN: 1-919931-69-4. [Google Scholar]
- 15.Peltzer K, Phaswana-Mafuya N. The Symptom Experience of People Living with HIV and AIDS in the Eastern Cape, South Africa. BMC Health Serv Res. 2008;8:271. doi: 10.1186/1472-6963-8-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peltzer K, Friend-du Preez N, Ramlagan S, Fomundam H. Use of traditional complementary and alternative medicine for HIV patients in KwaZulu-Natal, South Africa. BMC Publ Health. 2008;8:255. doi: 10.1186/1471-2458-8-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Risa KJ, Nepon L, Justis JC, Panwalker A, Berman SM, Cinti S, Wagener MM, Singh N. Alternative Therapy Use in HIV-Infected Patients Receiving Highly Active Antiretroviral Therapy. Int J STD AIDS. 2002;13(10):706–713. doi: 10.1258/095646202760326471. [DOI] [PubMed] [Google Scholar]
- 18.Statistics South Africa, author. Mid-year population estimates. 2009. [cited March 16, 2010]. Available from: http://www.statssa.gov.za/Publications/P0302/P03022009.pdf.
- 19.UNAIDS, author. Sub-saharan Africa:latest epidemiological trend. Fact sheet 09. World Health Organisation; 2009. [Cited February 13, 2012]. Available from: http://data.unaids.org/pub/FactSheet/2009/20091124_fs_ssa_en.pdf. [Google Scholar]
- 20.UNAIDS, author. Ancient Remedies, New Disease : Involving Traditional Healers in Increasing Access to AIDs Care and Prevention in East Africa. 2002. [cited March 16, 2010]. Available from: http://data.unaids.org/Publications/IRC-pub02/jc761-ancientremedies_en.pdf. [Google Scholar]
- 21.Voss JG, Sukati NA, Seboni NM, Makoae LN, Moleko M, Human S, Molosiwa K, Holzemer W. Symptom Burden of Fatigue in Men and Women Living with HIV / AIDS in Southern Africa. J Assoc Nurses AIDS Care. 2007;18(4):22–31. doi: 10.1016/j.jana.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Wiwanitkit V. The use of CAM by HIV-positive patients in Thailand. Complement Ther Med. 2003;11:39–41. doi: 10.1016/s0965-2299(02)00108-5. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization, author. Traditional Medicine, Factsheet No.134. 2003. [cited August 22, 2009]. Available from: http://www.who.int/mediacentre/factsheet/fs134/en/