Abstract
Study Objectives:
Compliance with CPAP therapy remains an issue despite its effectiveness. Mask selection is likely to affect a patients experience with CPAP, and multiple mask options are currently available. Nasal pillows have less contact with the face compared to nasal masks and may benefit patients by minimizing side effects; however, they are infrequently used at high CPAP pressures. The aim of this study was to examine the performance of nasal pillows at pressures ≥ 12 cm H2O compared with nasal masks.
Methods:
Twenty-one subjects were recruited. Participants were randomized to Swift FX nasal pillows and their current nasal mask for 7 consecutive nights each in a prospective crossover trial. Objective device data and subjective feedback were collected.
Results:
There were no differences in objective device data of nasal pillows vs. nasal masks: Daily Usage 7.4 ± 1.4 vs 7.2 ± 1.4 (h/night); 95th%ile Leak 28.6 ± 13.5 vs 27.9 ± 17.9 (L/min); AHI 1.9 ± 1.3 vs 1.7 ± 1.1, respectively (all p-values > 0.05). There were no differences between the nasal pillows and nasal masks for subjective ratings of comfort, seal, red marks, side effects such as jetting and dry nose/mouth, and overall performance (all p-values > 0.05). The nasal pillows were rated to be less obtrusive and claustrophobic (both p-values < 0.01), but less stable (p = 0.04). Overall preference was 50% nasal pillows, 45% nasal masks; 5% found no difference.
Conclusion:
Nasal pillows are as efficacious as nasal masks at CPAP pressures ≥ 12 cm H2O and are a suitable option for patients requiring high CPAP pressures.
Clinical Trial Registration:
NIH Clinical Trials Registry. http://clinicaltrials.gov. Title: Nasal Pillows at High CPAP Pressure. Identifier: NCT01690923.
Citation:
Zhu X; Wimms AJ; Benjafield AV. Assessment of the performance of nasal pillows at high CPAP pressures. J Clin Sleep Med 2013;9(9):873-877.
Keywords: Obstructive sleep apnea, OSA, continuous positive airway pressure, CPAP, masks
Obstructive sleep apnea (OSA) is associated with serious consequences, including cardiovascular disease1–3 and metabolic disorders.4,5 Continuous positive airway pressure (CPAP) is proven to be highly effective in treating OSA6,7 and related comorbidities.1,8 Despite the effectiveness and known benefits of CPAP, previous studies using the cutoff point at least 4 hours per night to define compliance have shown that between 29% to 83% patients are non-compliant.9
Mask selection is likely to affect a patient's experience with CPAP therapy and compliance. Weaver listed patient-centered mask and machine selection as one of the critical elements to CPAP compliance.10 Nasal pillows have less contact with the face than nasal masks and may benefit patients by minimizing side effects such as claustrophobia, pressure sores, and air leak into the eyes. Massie and Hart conducted a randomized crossover study comparing nasal pillows and nasal mask, and found use of nasal pillows was associated with fewer adverse events and better sleep quality.11 Ryan and colleagues found use of nasal pillows resulted in less reported pressure on the face and subjects found nasal pillows more comfortable, but there was no difference in compliance, apnea hypopnea index (AHI), or patient preferences.12
Nasal pillows, however, are infrequently used at high CPAP pressures. There is some debate on the performance of pillows at higher CPAP pressures. Massie and Hart suggested that nasal pillows may not be considered for patients who require higher CPAP pressure levels because of concerns regarding the nature of the mask seal and the possibility of inadequate pressure delivery.11 The pressure range studied was 5-14 cm H2O and the authors concluded that nasal pillows are a well-tolerated and effective interface for OSA patients receiving CPAP at ≤ 14 cm H2O. Ryan and colleagues compared treatment parameters in groups with CPAP pressures < 10 cm H2O and ≥ 10 cm H2O and found no difference between nasal pillows and nasal masks.12 They further suggested nasal pillows could be considered as an initial choice for CPAP treatment. However, they did not study patients with pressure > 15 cm H2O.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Mask selection is likely to affect a patient's experience with CPAP however nasal pillows are not frequently used on patients requiring high CPAP pressures and their performance at these pressures has not been systematically evaluated. This study examined the treatment efficacy and user satisfaction of nasal pillows compared with nasal masks at CPAP pressures ≥ 12 cm H2O.
Study Impact: This study found that nasal pillows are as efficacious and subjectively acceptable as nasal masks when treating OSA patients with high CPAP pressures. This study will allow readers to adjust their clinical practice to allow CPAP patients the option of choosing the most suitable mask type regardless of pressure requirements.
The current literature on CPAP mask interfaces is scarce, and few studies have compared different mask types in the same patient population. A Cochrane review on CPAP interfaces by Chai and colleagues suggested that nasal pillows are a useful alternative for patients unable to tolerate conventional nasal masks. The authors recommended further trials comparing different interfaces for CPAP treatment.13 The performance of nasal pillows at higher pressures has not been systematically evaluated. The aim of this study was to examine mask efficacy and participant preference of nasal pillows compared with nasal masks at CPAP pressures ≥ 12 cm H2O.
METHODS
Subjects
Patients were recruited from the ResMed Sleep Trials Registry, a voluntary Registry open to all OSA patients using CPAP. Inclusion criteria were age > 18 years; established on CPAP therapy for ≥ 6 months; currently using a nasal mask, fixed CPAP pressure, or 95% APAP (Auto-adjusting positive airway pressure) ≥ 12 cm H2O; naive to nasal pillows; and willingness to provide written informed consent. Patients who were pregnant, using bilevel therapy, or had a preexisting lung condition that would predispose them to pneumothorax were excluded.
Study Design
The study protocol was approved by the University of New South Wales Human Research Ethics Committee. Each subject gave written informed consent. Participants were randomized to either Swift FX nasal pillows (ResMed Ltd, Sydney, Australia) or a new version of their current nasal mask for 7 consecutive nights each in a prospective crossover trial. Participants used the S9 device (ResMed) with their prescribed therapy settings. H5i heated humidifier and ClimateLine heated tube (ResMed) were provided to patients who were using humidification with their current device. All participants were encouraged to contact the study coordinators in the event of any problems developing during the trial.
After trialing each treatment mask for 7 days, a download of the S9, including usage hours, AHI, pressure, and leak was performed. Subjective feedback regarding the treatment mask was collected using an 11-point Likert scale questionnaire (0 = major issue, 5 = ok, and 10 = highly positive). The self-administered questionnaire addressed comfort, seal, stability, severity of red marks, perceived obtrusiveness, and overall performance of the treatment mask. CPAP related side effects of claustrophobia, feeling of pressure, dry mouth/throat, nasal symptoms, breathing comfort, jetting, eye irritation, and sleep quality were also assessed in the same questionnaire. Subjects also selected which mask system they preferred overall (nasal pillows, nasal mask, or no preference).
Statistical Analysis
Compliance data, leak, and pressure downloaded from the S9 devices were analyzed using the paired t-test. Subjective data from the questionnaires were analyzed using the Mann-Whitney test. Two proportions test were performed to assess the differences in mask preferences. Objective device data are presented as mean ± standard deviation, and subjective feedback ratings are presented as median and interquartile range (IQR). Statistical tests were considered significant when p ≤ 0.05. Analysis was undertaken with MiniTab (version 16, PA, USA) data analysis software. The primary outcome variable in the study was treatment efficacy as indicated by AHI on therapy. A priori power calculation undertaken on an unpublished pilot study indicated the required sample size to detect an AHI difference of 0.75 events/h with 80% confidence at the 5% significance level was 18 subjects.
RESULTS
Study Sample
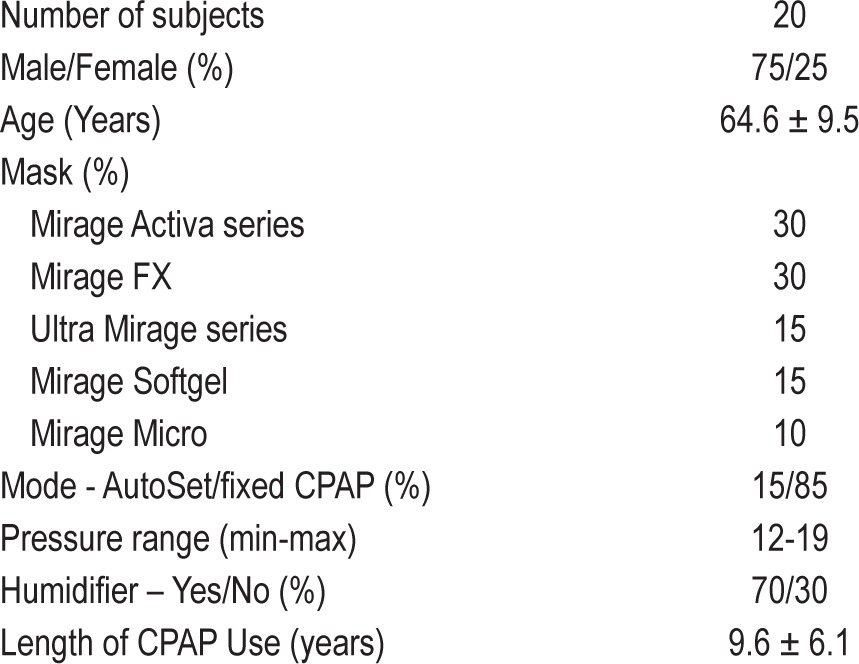
Twenty-one patients who met the inclusion criteria were invited to participate in the study. One subject was excluded due to inadequate fitting of nasal pillows. All remaining 20 patients completed the study protocol and were included in the final analysis. Patient characteristics of the study population are described in Table 1.
Table 1.
Baseline characteristics of study population
Objective Device Data
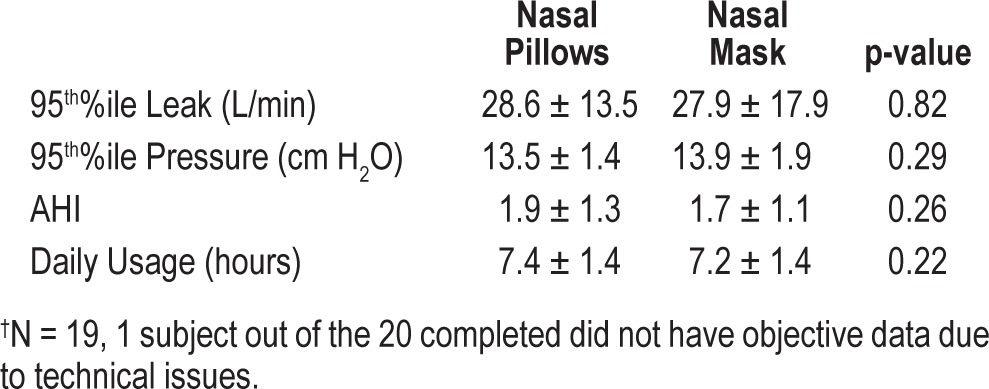
As demonstrated in Table 2, there were no statistical differences in objective device data for nasal pillows vs. nasal masks including average daily usage 7.4 ± 1.4 vs 7.2 ± 1.4 (h/night); 95th%ile Leak 28.6 ± 13.5 vs 27.9 ± 17.9 (L/min); 95th%ile pressure 13.5 ± 1.4 vs 13.9 ± 1.9 (cm H2O), and AHI 1.9 ± 1.3 vs 1.7 ± 1.1, respectively (all p-values > 0.05).
Table 2.
Data downloaded from CPAP devices†
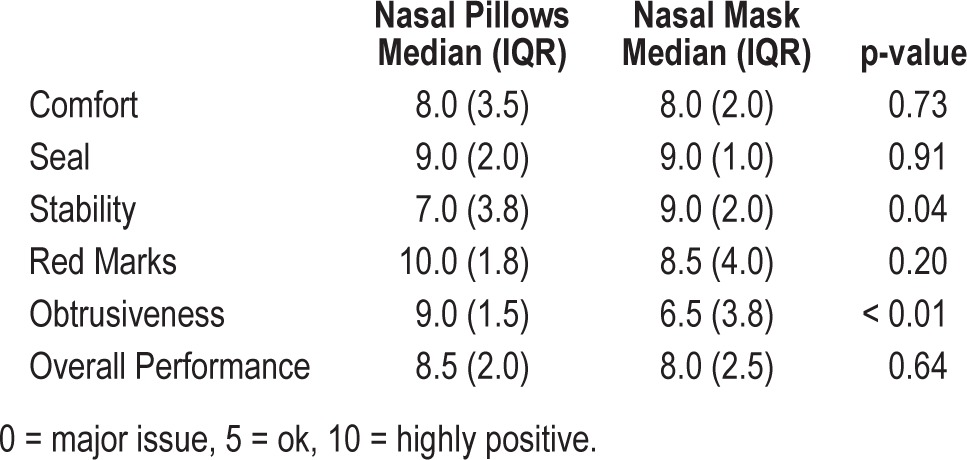
Mask Usability
There were no statistical differences between the nasal pillows and nasal masks for subjective ratings of mask comfort, seal, severity of red marks, and overall performance (Table 3). Nasal pillows were found to be significantly less obtrusive (p < 0.01) but less stable (p = 0.04).
Table 3.
Subjective ratings of mask performance
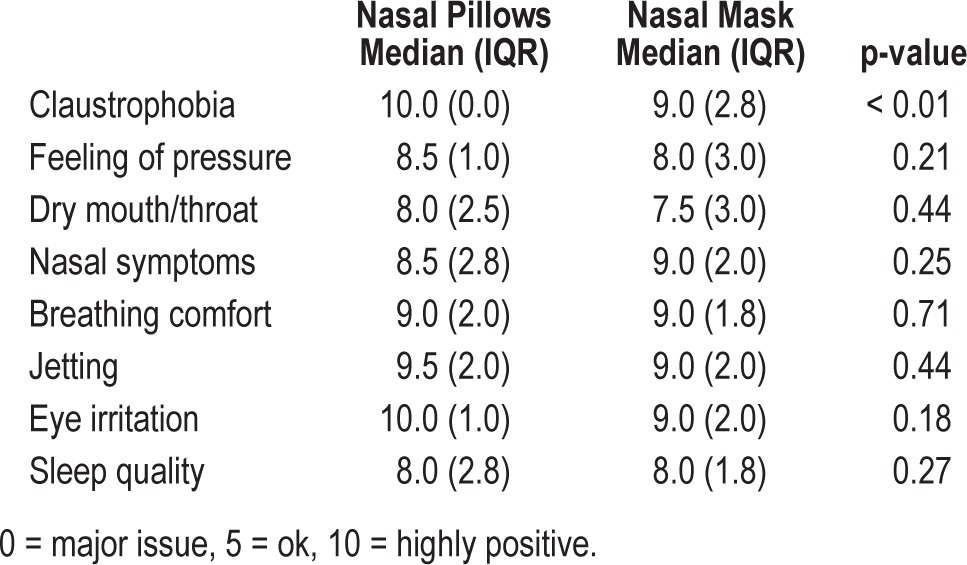
Side Effects
Comparison for self-reported CPAP and mask related side effects are shown in Table 4. Nasal pillows were found to be significantly less claustrophobic (p < 0.01). There were no statistical differences between the nasal pillows and nasal masks for subjective ratings of other side effects from CPAP use including feeling of pressure, dry mouth/throat, nasal symptoms, breathing comfort, jetting, eye irritation, and sleep quality.
Table 4.
Subjective ratings of side effects
Humidification Use
Seventy percent of the subjects completing the study reported frequent use of humidification and were provided with the H5i humidifier and ClimateLine heated tube for the duration of the study. Humidification settings were consistent between periods of nasal pillows and nasal mask use, and there was no reported need for humidification setting changes. Thirty percent of the completed subjects did not use humidification as their usual practice. Two of these 6 patients reported nasal dryness using nasal pillows which they did not experience when using the nasal mask.
Mask Preference
Participants were also asked to select their preferences for the masks regarding seal, comfort, stability, obtrusiveness, and overall preference. Results are displayed in Figure 1. Regarding overall mask preference, 50% preferred nasal pillows, 45% preferred nasal masks, and 5% found no difference between nasal pillows and nasal masks (Figure 1). There was a significant preference for nasal pillows in the “less obtrusive” category, but a significant preference for nasal masks in the “stability” category. There were no significant findings in the other areas.
Figure 1. Subject preferences.
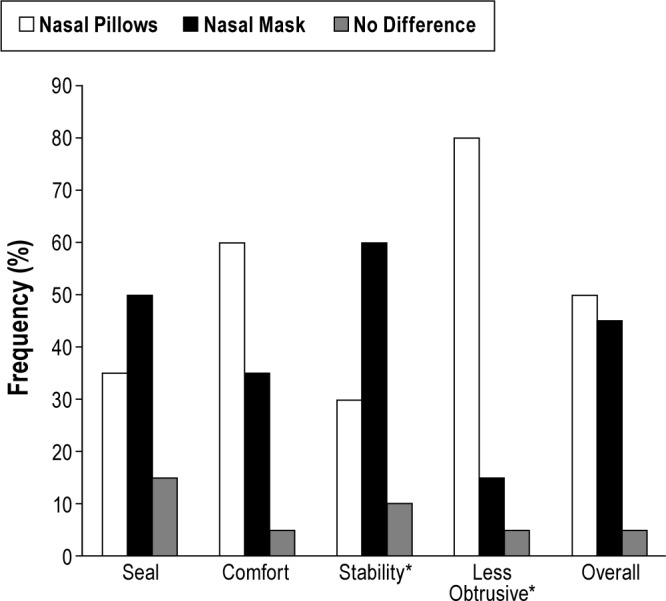
*p < 0.05
Participants with CPAP pressures ≥ 15 cm H2O
Six participants had a therapy pressure (fixed CPAP pressure or 95th percentile APAP pressure) ≥ 15 cm H2O (nasal pillows vs. nasal mask 15.6 ± 0.6 vs 15.4 ± 0.5 cm H2O). Five of the 6 participants preferred nasal pillows overall. There were no significant differences between 95th%ile leak (nasal pillows 31.2 ± 11.3 vs nasal mask 34.3 ± 19.9 L/min) and AHI (nasal pillows 1.27 ± 0.7 vs nasal mask 0.98 ± 0.5). However, average daily usage was found to be significantly higher on nasal pillows (nasal pillows 7.68 ± 1.2 vs nasal mask 7.09 ± 1.3 h/night, p = 0.02). Total subjective ratings scores of all categories was observed to have a higher trend towards nasal pillows, but was not statistically significant (nasal pillows median 121.5 [43] vs nasal mask 108.5 [12]).
DISCUSSION
The results of this study demonstrate that nasal pillows are as efficacious as nasal masks at CPAP pressures ≥ 12 cm H2O. Nasal pillows were found to be significantly less obtrusive and less claustrophobic than nasal masks. Subjective feedback shows nasal pillows are a suitable option for patients at high CPAP pressures.
The equity in objective machine downloaded data between nasal pillows and nasal mask is an important finding of this study. Massie and Hart raised concerns regarding the nature of the mask seal and the possibility of inadequate pressure delivery.11 The results of this study results do not support these concerns. There was no significant difference between nasal pillows and nasal masks in terms of objective leak data downloaded from the CPAP machines, compliance, subjective ratings of mask seal, and side effect profiles. AHI was similarly within a clinically acceptable range on both mask types despite the slightly higher leak levels, which is probably related to higher therapy pressures. In the small group of six participants with 95th%ile pressure ≥ 15 cm H2O, nasal pillows had similar performance comparing to the whole study population, and five of these participants preferred nasal pillows overall. Interestingly, average daily usage was found to be significantly higher on nasal pillows for these six participants, possibly due to positive overall experience with nasal pillows. This study is the first report to show performance of nasal pillows at pressure ≥ 15 cm H2O, though on a small group of participants.
CPAP therapy is the current gold standard for OSA treatment; however, compliance is often suboptimal.14 Findings from previous studies suggest that a multiplicity of factors that are highly variable between individuals are predictive of CPAP adherence. To date, there is not any single predictive factor that has been identified.14 Side effects and complaints are common, perhaps affecting 30% to 70% of patients to varying degrees.15 Common side effects related to CPAP use include pressure intolerance, dryness of nasal and pharyngeal membranes, nasal symptoms, and eye irritation.16 Recent advancements in mask designs provide better mask fit and more selections to the patients that may provide more positive CPAP experiences and increased compliance. There are concerns in the field that use of nasal pillows at higher CPAP pressure may lead to more CPAP related side effects such as nasal symptoms and jetting. This present study found no significant difference in the side effects profile between nasal pillows and nasal masks, suggesting nasal pillows are a suitable mask choice for this patient population. The interesting finding on improved compliance in the small group of participants with pressures ≥ 15 cm H2O suggests that the use of nasal pillows could be beneficial to certain patients.
The present study found nasal pillows were rated significantly less claustrophobic and obtrusive than nasal masks by the participants. However, nasal pillows are generally not the first-line mask choice for CPAP titration and are often reserved for patients who cannot tolerate conventional nasal masks, partly due to the concerns about their performance at higher CPAP pressures. A systematic review done by Weaver and Sawyer suggested that self-reported claustrophobic tendencies, evident in 15% of patients, have been associated with more variability in CPAP use and lower overall adherence.14 Multiple studies have suggested that early CPAP experience is associated with long-term CPAP adherence.17–19 Use of nasal pillows as a first-line mask of choice regardless of CPAP pressures should be further investigated, as this study was unable to find any reasons why nasal pillows should not be used on high pressure patients.
We did not provide heated humidification at the initial visit to six participants, as they did not usually use a humidifier. Two of these six patients reported nasal dryness associated with nasal pillows use in the patient questionnaire at study completion. The effect of the negative nasal pillows experience of these two patients may have minimal effect of the overall results of the study, but we suggest that nasal dryness and irritation should be carefully monitored and heated humidification provided in future practices and trials when such symptoms are reported. The two patients who experienced nasal dryness were not on higher CPAP pressures compared to the rest of the study population; therefore, we speculate that need for heated humidification with nasal pillows use is probably patient specific rather than pressure related. This is further supported by the fact that four participants who do not currently use humidification with their nasal mask did not develop symptoms when they moved to nasal pillows.
A limitation of this study is that only established CPAP users on nasal masks were included. Long-term nasal mask users and even clinicians may have the perception that the nasal mask is more stable and seals better with conventional 4-pointed headgear, which is evident by significantly higher ratings for nasal mask stability compared to nasal pillows in this study. Leak data downloaded from the S9 machines showed no difference between nasal masks and nasal pillows despite the perceived instability of nasal pillows. This may be because, mechanically, nasal pillows require less restraining force than a given nasal mask (air pressure acting on a smaller mask cross-sectional area creates a smaller reaction force and will result in less headgear tension).
Users might be more biased positively towards nasal masks after years of usage; however, this adds weight to the finding that nasal pillows perform equivalently to nasal masks at high CPAP pressures, and preference for nasal pillows is slightly higher. On the other hand, experienced CPAP users might be less sensitive to side effects than new CPAP users going through acclimation of the therapy. A similar study could be performed on CPAP naïve patients in the future. Secondly we did not choose a “standard” nasal mask and included various nasal mask types in this study, while Swift FX which is the newest generation design in nasal pillows was used as the “standard” nasal pillows in this trial. Newer generations of nasal masks may have improved in potential problem areas such as seal, comfort, and stability; however, there was no observed difference in results between the newer generation of nasal mask (Mirage FX) and older generations (Activa and Ultra Mirage series). Therefore, we do not believe this factor has great influence on the study results.
In summary, this study has shown that nasal pillows are as efficacious as conventional nasal masks at CPAP pressure ≥ 12 cm H2O. Nasal pillows are significantly less claustrophobic and obtrusive and therefore could be recommended to patients regardless of CPAP pressures.
DISCLOSURE STATEMENT
This study was funded by ResMed Ltd. Xueling Zhu, Alison Wimms, and Adam Benjafield are employees of ResMed Ltd. A subset of this study was presented at the 24th Annual Scientific meeting of the Australasian Sleep Association and the Australasian Sleep Technologists Association. Abstract ID: 0155.
REFERENCES
- 1.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 2.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 3.McNicholas WT, Bonsigore MR. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007;29:156–78. doi: 10.1183/09031936.00027406. [DOI] [PubMed] [Google Scholar]
- 4.Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005;172:1590–5. doi: 10.1164/rccm.200504-637OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Angelico F, del Ben M, Augelletti T, et al. Obstructive sleep apnoea syndrome and the metabolic syndrome in an internal medicine setting. Eur J Intern Med. 2010;21:191–5. doi: 10.1016/j.ejim.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1:862–5. doi: 10.1016/s0140-6736(81)92140-1. [DOI] [PubMed] [Google Scholar]
- 7.Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29:381–401. doi: 10.1093/sleep/29.3.381. [DOI] [PubMed] [Google Scholar]
- 8.Sharma SK, Agrawal S, Damodaran D, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med. 2011;365:2277–86. doi: 10.1056/NEJMoa1103944. [DOI] [PubMed] [Google Scholar]
- 9.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weaver TE. Adherence to positive airway pressure therapy. Curr Opin Pulm Med. 2006;12:409–13. doi: 10.1097/01.mcp.0000245715.97256.32. [DOI] [PubMed] [Google Scholar]
- 11.Massie CA, Hart RW. Clinical outcomes related to interface type in patients with obstructive sleep apnea/hypopnea syndrome who are using continuous positive airway pressure. Chest. 2003;123:1112–8. doi: 10.1378/chest.123.4.1112. [DOI] [PubMed] [Google Scholar]
- 12.Ryan S, Garvey JF, Swan V, Behan R, McNicholas WT. Nasal pillows as an alternative interface in patients with obstructive sleep apnoea syndrome initiating continuous positive airway pressure therapy. J Sleep Res. 2011;20:367–73. doi: 10.1111/j.1365-2869.2010.00873.x. [DOI] [PubMed] [Google Scholar]
- 13.Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006:CD005308. doi: 10.1002/14651858.CD005308.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–58. [PMC free article] [PubMed] [Google Scholar]
- 15.Catcheside PG. Predictors of continuous positive airway pressure adherence. F1000 Med Rep. 2010:2. doi: 10.3410/M2-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14:323–35. doi: 10.1007/s11325-010-0391-y. [DOI] [PubMed] [Google Scholar]
- 17.Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30:320–4. [PubMed] [Google Scholar]
- 18.Rosenthal L, Gerhardstein R, Lumley A, et al. CPAP therapy in patients with mild OSA: implementation and treatment outcome. Sleep Med. 2000;1:215–20. doi: 10.1016/s1389-9457(00)00012-5. [DOI] [PubMed] [Google Scholar]
- 19.Popescu G, Latham M, Allgar V, Elliott MW. Continuous positive airway pressure for sleep apnoea/hypopnoea syndrome: usefulness of a 2 week trial to identify factors associated with long term use. Thorax. 2001;56:727–33. doi: 10.1136/thorax.56.9.727. [DOI] [PMC free article] [PubMed] [Google Scholar]


