Abstract
Study Objectives:
Studies of continuous positive airway pressure (CPAP) adherence in multi-ethnic samples are lacking. This study explores previously described factors associated with therapeutic CPAP use in South Florida veterans with obstructive sleep apnea-hypopnea syndrome (OSAHS).
Methods:
We performed a retrospective, cross-sectional analysis of CPAP adherence comparing white, black, and Hispanic veterans returning to the Miami VA sleep clinic over a 4-month period. Participants had CPAP use download and completed questionnaires on demographics, sleepiness, insomnia, and social cognitive measures related to adherence. Linear regression modeling was used to explore the impact of measured variables and potential interactions with race-ethnicity on mean daily CPAP use.
Results:
Participants (N = 248) were 94% male with mean age of 59 ± 11 years and included 95 blacks (38%), 91 whites (37%), and 62 Hispanic (25%) veterans. Blacks had less mean daily CPAP use than whites (-1.6 h, p < 0.001) and Hispanics (-1.3 h, p < 0.01). Blacks reported worse sleep onset insomnia symptoms compared to whites. In the final multivariable regression model, black race-ethnicity (p < 0.01), insomnia symptoms (p < 0.001), and self-efficacy (p < 0.001) were significantly associated with mean daily CPAP use. In addition, the black race by age interaction term showed a trend towards significance (p = 0.10).
Conclusions:
In agreement with recent studies, we found that mean daily CPAP use in blacks was 1 hour less than whites after adjusting for covariates. No CPAP adherence differences were noted between whites and Hispanics. Further investigations exploring sociocultural barriers to regular CPAP use in minority individuals with OSAHS are needed.
Citation:
Wallace DM; Shafazand S; Aloia MS; Wohlgemuth WK. The association of age, insomnia, and self-efficacy with continuous positive airway pressure adherence in black, white, and Hispanic US veterans. J Clin Sleep Med 2013;9(9):885-895.
Keywords: Veterans, race-ethnicity, continuous positive airway pressure, adherence, sleep apnea, insomnia
Obstructive sleep apnea-hypopnea syndrome (OSAHS) may affect up to 2% of women and 4% of men in the US population.1 It is associated with lower quality of life, greater healthcare utilization, neurobehavioral deficits, and increased risk of hypertension, cardiovascular events, and all-cause mortality.1–4 Continuous positive airway pressure (CPAP), the first-line treatment for moderate to severe OSAHS, completely or partially reverses many of these deleterious consequences when used consistently.5 However, despite its efficacy, empirical studies suggest that rates for regular CPAP use (≥ 4 h daily) range from 30% to 60%.6
Studies in predominantly white OSAHS populations have identified demographic, polysomnographic, social, and psychological factors affecting CPAP adherence.7 For example, age, body mass index (BMI), daytime sleepiness, OSAHS severity, CPAP pressure, optimal CPAP titration, outcome expectancies associated with CPAP use, and perceived confidence in one's ability to use CPAP (self-efficacy) have all been associated with CPAP adherence.6–9 Although race-ethnicity and cultural influences have been found to be important in other health behaviors, their role in CPAP adherence have been relatively understudied. The most well-characterized race-ethnic CPAP differences have been those between black and white individuals with OSAHS. Five recent American studies (2 prospective and 3 cross-sectional) found that blacks use CPAP at least one hour less than whites. The etiology for this disparity in treatment adherence is unclear.8,10–13 There are fewer data about CPAP use in Hispanic individuals, the largest ethnic minority group in the US.14
BRIEF SUMMARY
Current Knowledge/Study Rationale: Although CPAP adherence differences between blacks and whites have been studied, few studies have examined CPAP adherence of US Hispanics or the influence of race-ethnicity on predictor variables for CPAP use. This study describes the influence of demographics, disease severity, sleepiness, insomnia, social cognitive measures, and the interaction of race-ethnicity with these variables on CPAP adherence in a South Florida veteran sleep clinic sample.
Study Impact: Our study adds to the growing awareness of the importance of insomnia symptoms and self-efficacy in CPAP use regardless of race-ethnicity. We found an interaction of black race with age and CPAP adherence, suggesting that generational effects may be considered when developing programs to enhance CPAP adherence in blacks.
Although there are many potential sources of race-ethnic differences in CPAP adherence, we focused on demographic/ anthropometric characteristics, OSAHS severity, CPAP treatment factors (e.g., pressure, duration of CPAP ownership), and self-reported symptoms and thoughts about OSAHS. All of the above have been shown to impact CPAP adherence.6,7 Some American studies have found that blacks have worse OSAHS severity and greater body mass index (BMI) than whites, factors thought to influence CPAP adherence.11,15 American studies in community and sleep clinic samples have shown that OSAHS symptoms, including daytime sleepiness and coexisting insomnia symptoms may vary by race-ethnicity.14,16–18 In the Home-PAP study, Billings and colleagues found that sleep onset insomnia complaints were significantly more common in blacks than whites/Hispanics.19 This study also reported that participants with prolonged subjective sleep onset latency (> 30 min) at baseline used CPAP 70 minutes less per night at 3 months than participants with shorter sleep onset latency after adjusting for apnea-hypopnea index (AHI) and study arm.19 Similarly, our prospective data in US Hispanic veterans has shown that greater baseline insomnia symptoms predict poorer future CPAP use.14 Although social cognitive factors like self-efficacy and outcome expectancies have been shown to be independent predictors of future CPAP use, to our knowledge, no American study has specifically examined potential race-ethnic differences in these measures.6,7 As black and Hispanic individuals comprise approximately 20% of the veteran population, identifying therapeutic targets for enhancing CPAP use in these groups is an important first step in improving adherence.20 Our study aims were (1) to examine previously established variables (demographics, disease-severity, daytime sleepiness, insomnia symptoms, social cognition) associated with CPAP adherence in a culturally diverse sample, and (2) to explore race-ethnic variation in these established factors associated with regular CPAP use in South Florida veterans with OSAHS.
METHODS
Participants
We performed a retrospective, cross-sectional analysis of adult white, black, and Hispanic veterans with OSAHS who attended the Miami VA Healthcare System (VAHS) Sleep Clinic from July 2011 to October 2011 for a scheduled CPAP adherence visit. Inclusion criteria included: (1) OSAHS diagnosis and CPAP prescription at the Miami VAHS within the last 5 years, (2) completion of study questionnaires, and (3) possession of CPAP ≥ 7 days. Veterans were excluded if they (1) were unable to read or comprehend English, (2) had previous surgery for OSAHS, or (3) were prescribed supplemental oxygen.
Procedure
As part of their routine adherence visit to the Miami VAHS, veterans with OSAHS treated with CPAP complete questionnaires about demographics, medical history, and residual sleep symptoms. Race-ethnic group was determined by self-report (non-Hispanic white, non-Hispanic black, Hispanic/Latino, or other). By this method of categorizing participants, individuals with mixed race-ethnicity (i.e., black Hispanics, n = 2) were included in the Hispanic group. Participants were asked to complete validated questionnaires to determine subjective daytime sleepiness, insomnia severity, and social cognitive factors associated with OSAHS and CPAP treatment (described in section below). Anthropometric measures (height and weight) were recorded on the day of their clinic visit and used to calculate the BMI. Questionnaires were completed in English as all veterans were fluent English speakers. Objective CPAP adherence was verified as described below. The Miami VA Healthcare System Institutional Review Board approved the protocol.
Assessments
Questionnaires
Demographic questionnaires assessed participant age on the day of clinical visit, gender, medical history, marital status (married or partnered vs single or widowed), and highest educational attainment (high school graduate or lower, some college, or college graduate or higher). Medical history, comorbidities, and medications were obtained from questionnaires and review of medical records. Weighted medical comorbidities were calculated using the Charlson Comorbidity Index (CCI).21
Subjective daytime sleepiness was determined using the Ep-worth Sleepiness Scale (ESS), with 8 items rated on a scale of 0-3, with higher scores indicating a greater propensity to fall asleep in different situations.22 An ESS score > 10/24 defined excessive daytime sleepiness.22,23
Participants completed the insomnia severity index (ISI), a 7-item instrument measuring the individual's perception of his or her insomnia. The total scores range from 0 to 28, with higher scores indicating greater insomnia severity. Its internal consistency, concurrent validity, and sensitivity to clinical improvements are well established.24 In this study, insomnia was defined as a global ISI score ≥ 15 corresponding to a level of at least “moderate clinical insomnia.” We explored insomnia complaint subtype (i.e., onset, maintenance, premature awakenings) by comparing the means of the first 3 items of the ISI among the race-ethnic groups.
Social cognitive factors associated with treatment were assessed with the Self-Efficacy Measure for Sleep Apnea (SEMSA). The SEMSA is a 26-item questionnaire assessing CPAP adherence-related cognitions based on principles of social cognitive theory.25 The instrument is divided into 3 subscales that measure risk perception of OSA (e.g., cardiovascular risk), outcome expectancies of CPAP use (e.g., improved alertness), and treatment perceived self-efficacy (the individual's confidence in using CPAP treatment despite challenges). Items are rated from 1 to 4 on a 4-point Likert scale. Higher scores indicate greater risk perception, higher outcome expectancies with treatment, and greater perceived self-efficacy, respectively. Social cognitive measures after using CPAP treatment have been previously shown to be independent predictors of future CPAP adherence.6,7
Polysomnography and OSAHS Diagnosis
All veterans completed diagnostic and titration PSGs performed at the Miami VAHS. Attended in-lab PSGs were performed using EMBLA N7000 hardware and REMLOGIC version 1.1 software. Portable PSGs were performed with Embletta x100 portable recording units (Embla, Thorton, CO). We conducted diagnostic in-lab and portable PSG and manual titration PSGs in accordance with standards established by AASM.26–28 A split-night PSG was performed if ≥ 40 obstructive respiratory events were observed in the first 2 h of recorded sleep. All individuals completed either (1) an in-lab diagnostic PSG followed by a manual titration PSG (n = 84), (2) an unattended diagnostic portable PSG followed by a manual titration PSG (n = 17), or (3) an in-lab split-night PSG (n = 147). Scoring was performed manually by a certified sleep technologist, using 30-sec epochs and standardized scoring techniques.27 Hypopnea scoring followed the recommended definition (≥ 30% reduction in nasal pressure relative to baseline associated with ≥ 4% oxygen desaturation). The AHI was defined as the number of apneas and hypopneas per hour of sleep. OSAHS diagnosis was made per ICSD-2 criteria.29 Polysomnography variables of interest (diagnostic and titration study type, diagnostic AHI) were extracted from the medical record.
CPAP Treatment
All veterans accepting CPAP treatment undergo a standardized 30-min mask-fitting and equipment educational session by our sleep-certified respiratory technologist at the time of CPAP distribution. They were also provided with printed information about OSA, its medical consequences, and CPAP troubleshooting techniques. After split-night or in-lab titration PSG, patients received CPAP units (Remstar M series with C-flex and heated humidifier, Philips-Respironics, Murrysville, PA) fixed at the prescribed pressure obtained from the titration PSG and distributed by our laboratory staff. As a standard procedure, CPAP units were set to a C-flex setting of 3 cm H2O. All devices contained software (Philips-Respironics Encore Pro 2) that measured and recorded CPAP mask-on time onto a microchip within a secure digital memory card.
CPAP Adherence
After CPAP distribution, veterans were scheduled for standard clinical follow up for CPAP adherence. These visits occurred at varying intervals, but usually after 3-6 months of use and then annually. Individuals were encouraged to return to our sleep center earlier if they encountered ongoing difficulties. The sample included recently diagnosed individuals having their first CPAP adherence download as well as those who were long-term CPAP users who may have had prior downloads. Adherence measures included all days since initial CPAP distribution (mean of 512 ± 484 days; range: 7-1,818 days). On the day of the clinical visit, the following variables were collected from CPAP SD memory cards: prescribed CPAP pressure, days since CPAP distribution (duration of ownership), % of days used, % of days used > 4 h, mean daily use, and residual AHI.
Data Analysis
Demographic and clinical characteristics, CPAP adherence variables, and questionnaire responses were compared between whites, blacks and Hispanics. Data are reported as means and SDs for continuous variables. Categorical data are presented as frequencies (%). Categorical and continuous data were compared among race-ethnic groups using χ2 or ANOVA, respectively. Post hoc pairwise comparisons employed Tukey test. As the duration of CPAP ownership varied widely among our participants (7-1,818 days), duration subgroup comparisons were performed to examine differences in the predictors and adherence. Mean daily hours of CPAP use was used as the primary outcome adherence measure. The assumptions for use of parametric inferential statistics were met for all variables.
Linear regression modeling was used to explore the association of predictor variables with CPAP adherence (mean daily hours). Hispanic and black race-ethnicity was analyzed referent to white race-ethnicity. Variables selected to predict CPAP adherence were chosen based on previous research (age, BMI, marital status, educational level, AHI, CPAP pressure, ESS, insomnia symptoms, outcome expectancies, and self-efficacy).6–9,23 Separate linear regression models were performed assessing 2 domains: (1) demographic/anthropometric variables (race-ethnicity, age, educational level, marital status, and BMI), (2) disease severity, CPAP treatment factors (AHI, CPAP pressure, duration of CPAP ownership), and sleep-related questionnaires responses (ESS, insomnia symptoms measured by the ISI, and SEMSA outcome expectations and perceived self-efficacy scores). In an attempt to control across domains, a final regression model was also tested, which included variables significantly associated with mean daily CPAP use in Models 1 and 2.
For Models 1 and 2, regression analysis was performed in 2 steps: (1) all variables in each domain were entered simultaneously testing for main effects, (2) the product of race-ethnicity and each variable in the domain was entered separately to test for interaction. These interaction terms were of primary interest to determine if race-ethnicity moderated the relationship of the predictors with CPAP adherence. For example, does insomnia impact CPAP adherence differentially in blacks than whites? Continuous interaction variables were mean centered. Each interaction term was added separately and retained in each regression model only if found to be significantly associated with CPAP adherence.
Additional interaction terms were entered into Model 2 and the final model. Because of the possibility of confounding of self-efficacy and insomnia symptoms with duration of CPAP ownership, interaction terms of CPAP ownerships with these variables were also included in these models.
For all 3 models, multicollinearity among predictors was examined by scrutinizing their Pearson correlations, variance inflation factors, eigenvalues, and condition indexes. For all analyses, p < 0.05 was defined as statistically significant. Statistical analyses were performed with SPSS Statistics 20.0 (SPSS, Chicago, IL).
RESULTS
Characteristics of Study Participants
Two hundred forty-eight veterans (94% male, with a mean age of 59 ± 11 years) fulfilled inclusion criteria (Table 1). Forty-six veterans were excluded (36 for incomplete questionnaires, 3 for prior OSAHS surgery, 7 for using supplemental oxygen). Ninety-five (38%) participants self-reported as black, 91 participants (37%) as white, and 62 participants (25%) as Hispanic/Latino. Five veterans (3 Asian, 2 Pacific Islander) were of “Other” race-ethnicity and were also excluded from analysis. Sixty percent of the participants were married or partnered, and most (71%) had some college education or greater. Seventy-seven percent of the sample had hypertension, 35% had diabetes, 17% had heart disease, 51% reported depression, and 28% posttraumatic stress disorder diagnosis (Table 1).
Table 1.
Demographic and clinical characteristics by race-ethnicity
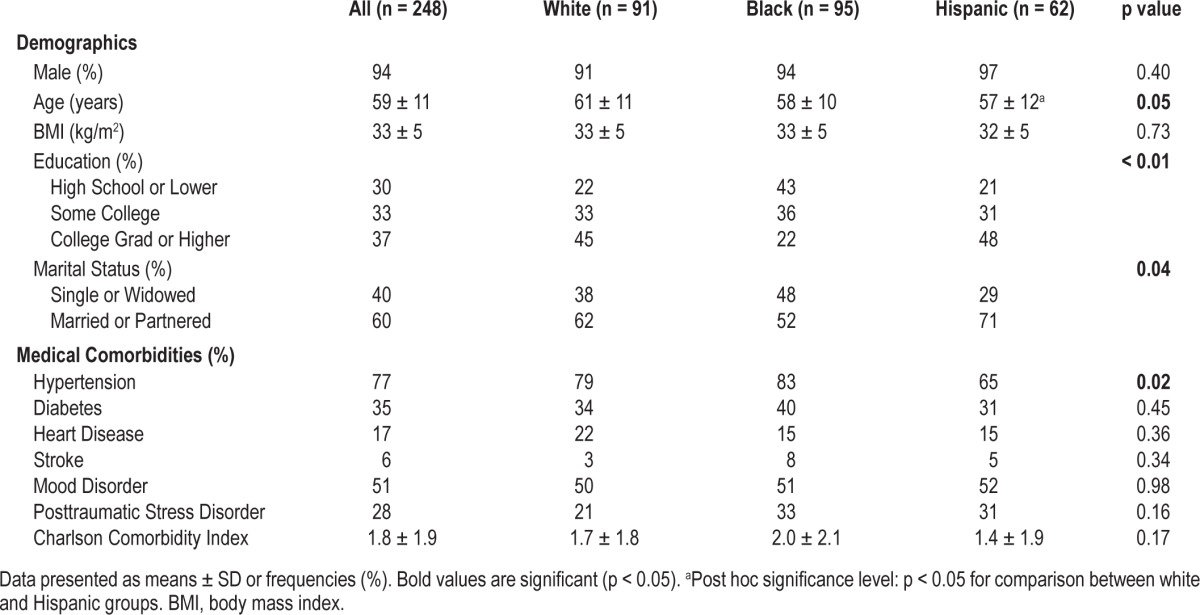
Demographic and Clinical Comparisons by Race-Ethnicity
Hispanics were significantly younger than whites but not different in age when compared to blacks. Hypertension diagnosis and “single or widowed” status was significantly more common among blacks than Hispanics, but not different when compared to whites. Blacks reported lower levels of education compared to both other groups. There were no significant group differences in gender distribution, mean BMI or mean Charlson comorbidity index (Table 1).
Polysomnography and CPAP Adherence Measures by Race-Ethnicity
Participants had a mean AHI of 40 ± 30 events/h of sleep and were prescribed a mean CPAP pressure of 9.8 ± 2.8 cm H2O (Table 2). There were no significant race-ethnic differences in OSAHS severity, mean AHI, prescribed CPAP pressure, or CPAP residual AHI at clinical follow-up. Averaged across all participants, CPAP had been distributed 512 ± 484 days prior to their adherence visit. The entire cohort used CPAP on 58% ± 34% of the nights, with mean daily use of 3.2 ± 2.8 hours. Overall, about one-third of participants had mean daily use ≥ 4 hours.
Table 2.
Comparisons of polysomnography and CPAP adherence by race-ethnicity
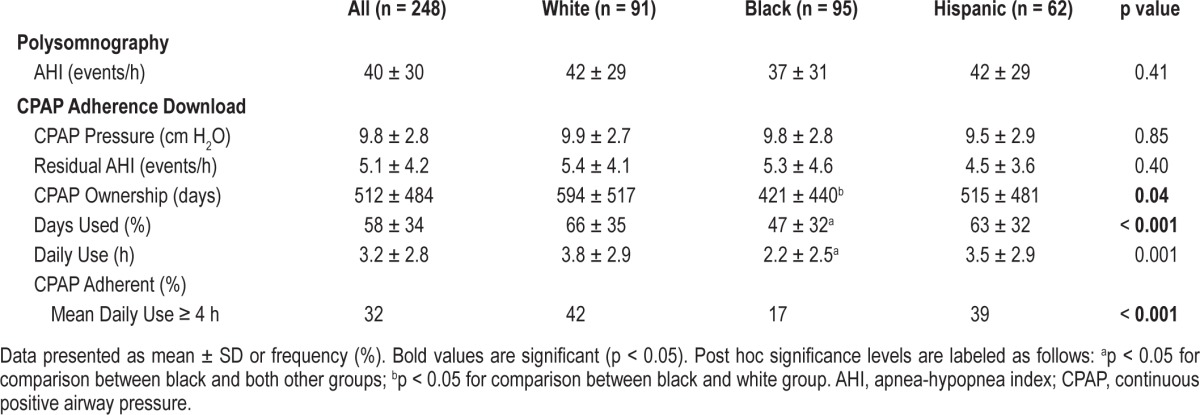
The duration of CPAP ownership was significantly shorter in blacks than whites, but not different when compared to Hispanics (Table 2). Blacks used CPAP on significantly fewer days and used CPAP over 1 hour less daily than whites and Hispanics. Similarly, blacks had a significantly lower proportion of participants with mean CPAP use ≥ 4 h daily than whites and Hispanics. No CPAP adherence differences were noted between whites and Hispanics.
CPAP Adherence Measures by Duration of CPAP Ownership
To examine the relationship between treatment duration and variables of interest, subgroups of duration of CPAP ownership (i.e., < 6 months, 6-12 months, > 12 months) were compared (Table 3). Seventy-five, 63, and 110 participants had been distributed CPAP < 6 months, 6-12 months, and > 12 months prior to study visit, respectively. There were no race-ethnic frequency differences among the CPAP ownership duration categories (Table 3). This is in contrast to the significant race-ethnic finding above which used continuous mean CPAP ownership duration (Table 2). This discrepancy may be due categorizing the continuous treatment duration variable as well as using a nonparametric statistic. Also, veterans using CPAP > 2 years were significantly less likely to be black than non-black (18% vs 30%, p = 0.04).
Table 3.
Comparisons of CPAP adherence by duration of CPAP ownership
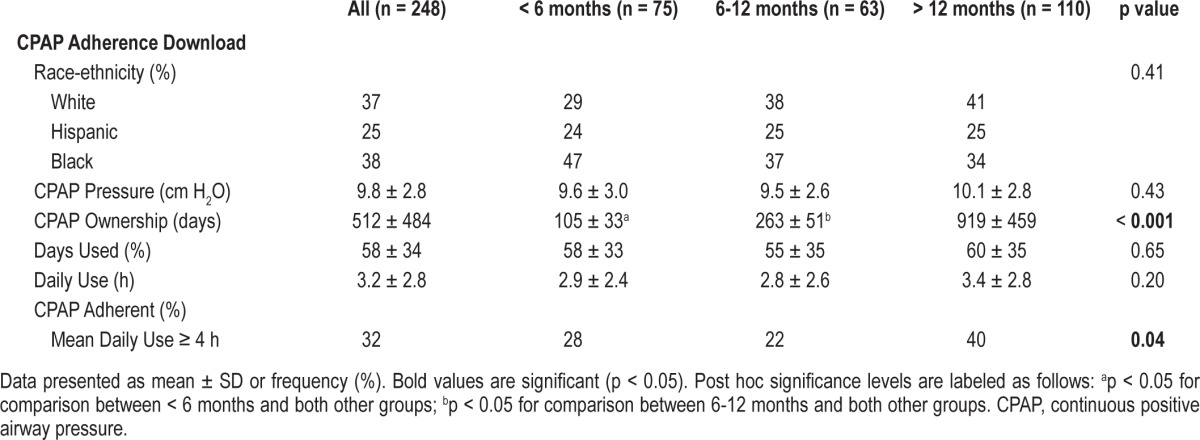
There were no differences among the CPAP ownership duration subgroups in prescribed CPAP pressure, percentage of days used, or mean daily hours of usage. However, veterans who had owned CPAP for > 12 months had a significantly higher proportion of mean daily CPAP use > 4 h compared to veterans who received CPAP < 6 months and 6-12 months prior to study visit (40% vs 28% vs 22%, p = 0.04). Based on these findings, the interaction of CPAP ownership duration with predictor variables (i.e., insomnia, self-efficacy) were entered into the linear models.
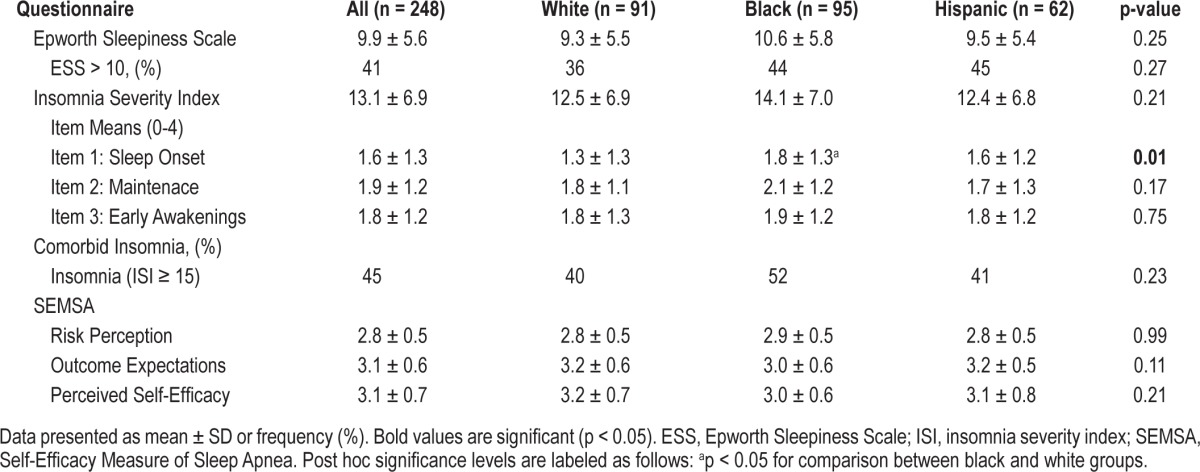
Questionnaire Responses by Race-Ethnicity
Forty-one percent of all participants met the cutoff for significant subjective daytime sleepiness at the adherence clinic visit (Table 4). There were no significant race-ethnic differences in mean ESS or proportion of participants reporting daytime sleepiness. Forty-five percent of participants reported insomnia symptoms (ISI ≥ 15). There were no race-ethnic differences in mean ISI scores. However, blacks had a significantly higher mean ISI item for sleep onset insomnia symptoms than whites but not significantly different from Hispanics. There were no significant differences in the mean ISI items for sleep maintenance insomnia or premature awakening complaints among the race-ethnic groups. Furthermore, there were no race-ethnic differences in SEMSA risk perception, outcome expectations, or perceived self-efficacy scores.
Table 4.
Comparisons of questionnaire responses by race-ethnicity
Linear Regression Models
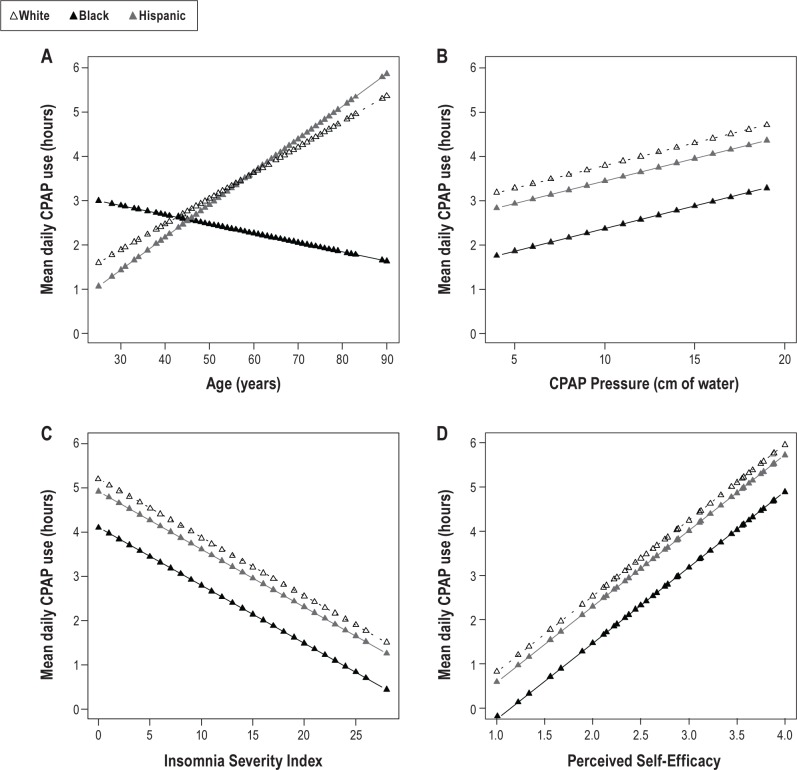
Linear regression analyses were performed to identify variables that were significantly related to mean daily CPAP use. The reported models used (1) previously described variables associated with regular CPAP use, and (2) significant race-ethnicity interactions terms.6–8,23 There was no significant evidence of multicollinearity between predictors in any of the models. The first model included demographic and anthropometric variables (race-ethnicity, age, BMI, education level, marital status, and race-ethnicity by age). The overall model for demographic/ anthropometric characteristics explained 14.1% of the observed variance (r2 = 0.141, adj. r2 = 0.112, p < 0.001; Table 5). In this model, black race, increased age, higher BMI, and race-ethnicity by age interaction were associated (p < 0.05) with mean daily CPAP use. Figure 1A shows a negative age-adherence relationship for blacks but positive for whites and Hispanics. No other interactions of race-ethnicity with other variables were found to be significant in Model 1.
Table 5.
Regression analysis of measures associated with mean daily CPAP use
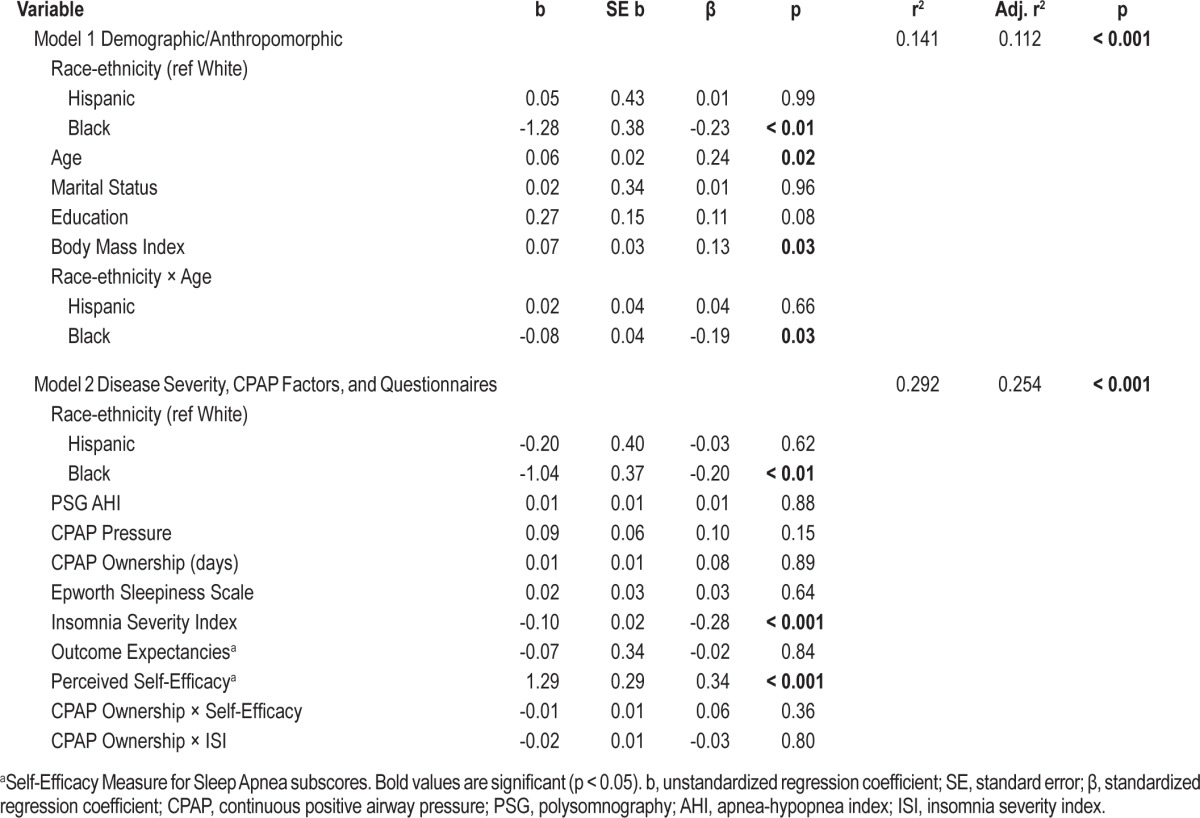
Figure 1. Regression lines for predictors and CPAP adherence.
Regression lines for predictors and CPAP adherence among whites (dotted), blacks (black) and Hispanics (gray) in Models 1-2. Each regression line is controlled for the additional variables in each individual model (Table 5). Panel A shows a significant race-ethnicity-age interaction while Panels B-D show no race-ethnicity-predictor interaction. All panels show significantly less CPAP use by blacks. CPAP, continuous positive airway pressure.
The second model included race-ethnicity, OSAHS severity (PSG AHI), CPAP adherence download variables (CPAP pressure and duration of CPAP ownership), and sleep-related questionnaire responses (ESS, insomnia severity index, and SEMSA outcome expectancies and perceived self-efficacy scores). Because of subgroup differences in adherence (Table 3), interaction terms were also entered to examine if the relationship between insomnia symptoms and self-efficacy and adherence depended on CPAP ownership duration. The overall model for disease severity/CPAP download variables, sleep-related questionnaires, and CPAP ownership interaction terms explained 29.2% of the observed variance (r2 = 0.292, adj. r2 = 0.254, p < 0.001; Table 5). In this model, black race, greater insomnia symptoms, and higher self-efficacy were associated (p < 0.05) with mean daily CPAP use. No other interactions of race-ethnicity with other variables were found to be significant in Model 2. Figure 1B-D shows a similar relationship between CPAP pressure, ISI, and SEMSA perceived self-efficacy score, and predicted mean daily CPAP use for the 3 race-ethnic groups, respectively.
In the final regression model (Table 6), we included race-ethnicity in addition to the statistically significant variables (p < 0.05) from the 2 models (age, BMI, insomnia severity index, SEMSA perceived self-efficacy score, and race-ethnicity by age interaction). Educational level was also included as this showed a trend towards significance in Model 1 (Table 5) and has been associated with CPAP adherence.23 In addition, we included CPAP ownership duration, CPAP ownership by self-efficacy, and CPAP ownership by insomnia symptoms interaction terms to control for potential confounding effects of treatment duration. The final model was significant and explained 31.4% of the adherence variance at clinical follow-up (r2 = 0.314, adj. r2 = 0.274, p < 0.001; Table 6). In the final model, the black race by age interaction term showed a trend towards significance (p = 0.10).
Table 6.
Final regression analysis of measures associated with mean daily CPAP use
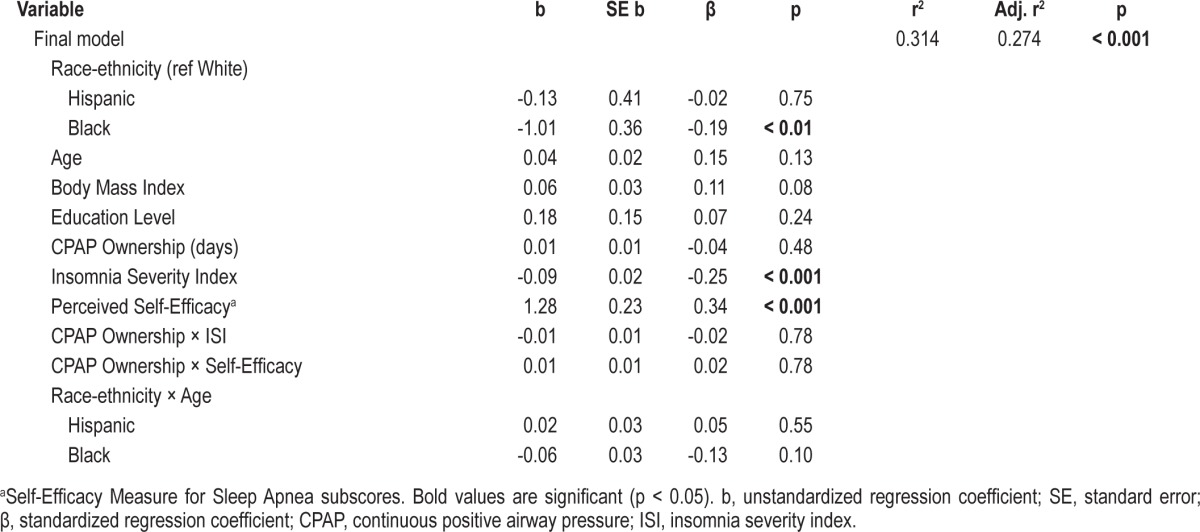
Black race alone accounted for 5.8% of the variance in the final model. In all 3 models, blacks used CPAP about 1 h less than whites after adjusting for the listed variables (Tables 5, 6). We repeated the linear regression models employing 2 other alternative CPAP adherence outcomes (% of days used and % of days using > 4 h) with similar findings.
DISCUSSION
As stated previously, our goals were two-fold: (1) to examine previously described variables associated with CPAP adherence in a culturally diverse OSAHS sample of American veterans in a sleep clinic sample, and (2) to determine if race-ethnicity moderated predictors of CPAP adherence in South Florida veterans with OSAHS. Limited data exist for direct comparisons among these three race-ethnic groups.12 Our study findings replicate those of other investigations which have noted about a 1-h adjusted difference in mean daily CPAP use between blacks and whites.8,10–12 Similar to a recent multi-city prospective study in the US, no difference in CPAP adherence was noted between whites and Hispanics.12 Overall, our sample of South Florida veterans returning for objective CPAP adherence follow-up had suboptimal CPAP adherence with mean daily use of only 3.2 ± 2.8 hours. These CPAP adherence rates are disappoint-ingly low but within the range of reported American OSAHS cohorts.7,8,10,14 In contrast with most OSAHS populations reported in the literature, the majority of our OSAHS cohort was non-white.7 Two American studies (one prospective, one retrospective) with predominantly black samples had overall CPAP adherence rates similar to ours (3.4 ± 2.7 h, 3.9 ± 2.6 h).8,13 In addition, our CPAP adherence was collected after longer treatment duration (mean of 512 ± 484 days of CPAP use) than most studies. Thus, our findings consist of predictors of long-term (> 3 months) CPAP use in a diverse veteran sample.
Similar to other investigations, we found three main effects for black race-ethnicity, insomnia severity index, and self-efficacy and CPAP adherence in South Florida veterans.8,11,12,14 First, black race was associated with worse CPAP adherence. Second, a higher insomnia severity index score was associated with worse daily CPAP use; and third, greater self-efficacy was associated with greater daily CPAP adherence. Additionally, we found a significant interaction between black race, age, and CPAP adherence in one of our models. However, we did not find interactions between race-ethnicity and insomnia symptoms or race-ethnicity and self-efficacy and CPAP adherence. This indicates that the relationship between insomnia and CPAP adherence and self-efficacy and CPAP adherence was similar across race-ethnic groups. In the final model with covariates, the CPAP adherence difference between blacks and whites was attenuated (1.6 h to 1.0 h). This smaller difference indicates that insomnia symptoms and self-efficacy partially explained the difference in adherence between blacks and whites. In our final model, the combination of race-ethnicity, age, BMI, duration of CPAP ownership, ISI score, SEMSA self-efficacy, and race-ethnicity-age interaction explained 31% of the variance in mean daily CPAP use at clinical follow-up. Given the wide range of CPAP ownership duration, our models were adjusted to account for potential confounding of treatment duration with insomnia symptoms and self-efficacy.
As we have shown previously, the South Florida Hispanic veteran population is highly acculturated, given the requirements necessary to enlist for military service (i.e., minimum high school education or equivalent, English proficiency).14,30 Thus, from a cultural standpoint, it may not be surprising that their CPAP adherence is similar to that of white veterans. Whether unacculturated US Hispanic immigrants have different CPAP adherence rates remains an unanswered question. Our South Florida veteran population was predominantly male, had a high prevalence of psychiatric comorbidities, and had low-cost access to medical care. Therefore, our veteran sample is not representative of the US population with OSAHS, and these characteristics limit the generalization of our findings.
Black Veterans Use CPAP Less
In all of our regression models, black race was independently associated with 1 hour less mean daily CPAP use than whites despite adjusting for a number of factors (Tables 5, 6). In addition, blacks attempted to use CPAP on fewer days than whites and Hispanics (Table 2). Our findings are consistent with those of previous retrospective and recent prospective studies. In a retrospective analysis at the Durham VA (n = 501), Means and colleagues found that black veterans had a significantly lower mean daily use (3.90 ± 1.94 vs 4.91 ± 2.07 h) and used CPAP on significantly fewer nights (54% vs 68%) after 3 months of treatment compared to white veterans.11 In another retrospective analysis of 100 consecutive participants (39% black) presenting to a Detroit sleep center, blacks were found to have a significantly lower CPAP daily use after 1 month than whites (4.4 ± 1.5 vs 5.5 ± 2.2 h), despite similarities in other demographic and polysomnographic variables.10 In the Home PAP study, a randomized controlled trial in five US cities comparing home diagnosis of OSAHS and treatment to attended in-lab care, Billings and colleagues prospectively examined the predictive value of race, education, and SES on CPAP adherence in participants with moderate to severe OSAHS and excessive daytime sleepiness.12 After 1 month, blacks had a significantly lower mean daily CPAP use (about 1.5 h less) than whites after adjusting for SES, AHI, and study arm. Black race accounted for 6% to 12% of the observed CPAP use variance at 1 and 3 months. In another prospective study with 91 participants (57% black), Ye and colleagues reported that black race was the strongest predictor of 7-day CPAP adherence, independently explaining 12.9% of the variability in the mean daily use.8 In our study, black race alone accounted for 5.8% of the variance of mean daily CPAP use.
Insomnia Symptoms and Self-Efficacy Predict CPAP Adherence but Do Not Vary by Race-Ethnicity
We found a negative relationship between insomnia symptoms and CPAP adherence regardless of race-ethnicity. We did not observe any interactions between race-ethnicity, ISI scores, or insomnia complaints and CPAP use. The negative relationship of insomnia symptoms on CPAP use was not influenced by race-ethnicity. That is, the influence of insomnia symptoms was equivalent across all race-ethnic groups. In our study, the rate of coexisting insomnia symptoms in the race-ethnic groups are similar to reported estimates (39% to 58%) in sleep clinic cohorts with untreated OSAHS.16,31 In agreement with the Home PAP study, we found that sleep onset insomnia complaints were greater in blacks than whites.19 In our final linear regression model, a 10-point increase in the ISI at follow-up was associated with approximately 1 hour less of CPAP use (Table 6). In our study, insomnia symptoms were assessed after CPAP initiation. This is important in that it reflects the level of insomnia that may directly affect adherence. Insomnia present prior to CPAP initiation may improve or worsen with CPAP, making assessment of insomnia a potential therapeutic target to enhance CPAP adherence. Our findings provide additional data underscoring the importance of assessing insomnia symptoms in all CPAP users.14,31
Similar to insomnia symptoms, the influence of social cognitive variables on CPAP adherence was equivalent across the race-ethnic groups (Table 4, Figure 1D). Our data were in agreement with previous investigations showing that individuals with higher self-efficacy persevere with regular CPAP treatment.6,7 Participants completed questionnaires after varying lengths of CPAP treatment; therefore, after experiencing CPAP, they were able to accurately report cognitive perceptions of OSAHS and CPAP. Surprisingly, blacks did not have lower SEMSA self-efficacy scores than whites/Hispanics, despite their poorer overall adherence. Even in individuals who have been suboptimally adherent with CPAP, assessment of self-efficacy may identify individuals amenable to motivational enhancement for CPAP therapy, an intervention based on the methods of motivational interviewing.32 Other psychological variables that have been associated with CPAP adherence (locus of control, coping strategy styles, decisional balance) await exploration in these race-ethnic groups.6,7
The Influence of Age Was Moderated by Black Race
We found a significant interaction between black race, age, and CPAP adherence in Model 1; however, this finding was attenuated in the final model (Figure 1A; Table 6, p = 0.10). In Model 1, increasing age was associated with greater mean daily CPAP use in white and Hispanics but less CPAP use in blacks. This attenuation was likely due to the addition of insomnia and self-efficacy, suggesting its shared variance between age and these variables. This “generational effect” may be mediated by varying levels of trust in the healthcare system, perceived discrimination, or other factors.33,34 Further research on possible generational issues in blacks with OSAHS could help to clarify its contributing factors.
Race-Ethnicity and CPAP Adherence
Adherence to CPAP treatment is a complex behavior impacted by multiple factors.6,7,9 Our model explained about 31% of the variance in mean daily CPAP use. Although insomnia and self-efficacy have a strong association with CPAP adherence and the difference in CPAP use between blacks and whites/Hispanics is attenuated by adjusting for these variables, a 1-hour difference remains to be explained. Thus, other factors contribute to the CPAP adherence differences observed between blacks and whites/Hispanics. For example, in the Home-PAP study, reduced sleep duration has been recently shown to partially mediate the worse CPAP adherence in blacks compared to whites/ Hispanics.19 Also, recent evidence suggests that the home sleeping environments of blacks may be more disruptive than those of whites, which may also contribute to irregular CPAP use.35 Furthermore, inadequate sleep may not be viewed as a serious health issue in the black community, a belief which may also interfere with regular CPAP use.33 In the 2010 National Sleep Foundation Sleep in America Poll, fewer blacks (76%) than whites (83%) recognized that short or poor sleep was related to worse overall health.36 Further research is needed to identify other cultural beliefs or healthcare system factors which may be detrimental to CPAP use among blacks.
Limitations
Our study has several noteworthy limitations. One limitation is absence of comprehensive assessments of socioeconomic status, which has been associated to CPAP adherence in diverse race-ethnic samples.12,23,37 Low SES individuals have been shown to have worse CPAP adherence.12,23,37 In our sample, blacks were found to have a significantly lower educational level than Hispanics and whites, but educational level was not associated with CPAP adherence in our final model. Another limitation is the cross-sectional design which precludes determining if the race-ethnic differences observed (i.e., sleep onset insomnia complaints) were present prior to CPAP initiation or caused by the treatment. Additionally, we used a convenience sample of patient returning to our CPAP adherence clinic, so we do not have data on patients who abandoned treatment altogether. However, the mean daily CPAP adherence for Hispanic veterans in this study is similar to that we observed in a recent 30-day prospective study (3.5 ± 2.9 vs 3.6 ± 2.0 h).14 Because of the possibility that CPAP non-users did not return for clinical follow-up, the sample may be biased towards better adherence in those with longer CPAP ownership (Table 3). We did not measure other variables that have been associated with CPAP adherence, including neighborhood factors, sleep duration, or detailed measures of social support.7,12,37 Finally, limited power may have hindered our ability to detect interactions of race-ethnicity with variables of interest.
Given the vast health consequences OSAHS, understanding barriers to regular CPAP use in race-ethnic groups is of economic and public health importance.4,38 The strong association between insomnia symptoms, self-efficacy, and adherence suggests that these behavioral factors may represent therapeutic targets. For example, cognitive behavioral therapy for comorbid insomnia and motivational enhancement to improve self-efficacy for CPAP therapy could be used in individuals with insomnia symptoms or low self-efficacy.32,39 Our finding of a significant interaction of black race-ethnicity with age in CPAP adherence merits further investigation. Other explanatory etiologies of the disparity in CPAP adherence between blacks and whites/Hispanics await characterization. Future studies should examine the influence of sociocultural barriers in minority veterans with OSAHS to improve CPAP use and help narrow existing health disparities within the VAHS.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Aloia is a paid employee and stock holder of Philips-Respironics, Inc. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Dr. Sandeep Dayanand for database management and the respiratory technologists (Daniel Mora, Rafael Sepulveda, Herblay Alonso, Luis Jinete) at the Miami VA Healthcare System for their contributions to this study. The work was completed at the Bruce W. Carter Department of Veterans Affairs Medical Center, Miami, FL.
REFERENCES
- 1.Young T. Rationale, design, and findings from the Wisconsin Sleep Cohort Study: Toward understanding the total societal burden of sleep disordered breathing. Sleep Med Clin. 2009;4:37–46. doi: 10.1016/j.jsmc.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallace DM, Ramos AR, Rundek T. Sleep disorders and stroke. Int J Stroke. 2012;7:231–42. doi: 10.1111/j.1747-4949.2011.00760.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lal C, Strange C, Bachman D. Neurocognitive impairment in obstructive sleep apnea. Chest. 2012;141:1601–10. doi: 10.1378/chest.11-2214. [DOI] [PubMed] [Google Scholar]
- 4.Leger D, Bayon V, Laaban JP, Philip P. Impact of sleep apnea on economics. Sleep Med Rev. 2012;16:455–62. doi: 10.1016/j.smrv.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29:381–401. doi: 10.1093/sleep/29.3.381. [DOI] [PubMed] [Google Scholar]
- 6.Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: Implications for future interventions. Indian J Med Res. 2010;131:245–58. [PMC free article] [PubMed] [Google Scholar]
- 7.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of cpap adherence across age groups: Clinical and empiric insights for developing cpap adherence interventions. Sleep Med Rev. 2011;15:343–56. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye L, Pack AI, Maislin G, et al. Predictors of continuous positive airway pressure use during the first week of treatment. J Sleep Res. 2012;21:419–26. doi: 10.1111/j.1365-2869.2011.00969.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stepnowsky CJ, DiNicola G, Edward C, Zamora T. Meta-analysis of factors associated with cpap adherence. Sleep. 2012;35:A173. [Google Scholar]
- 10.Budhiraja R, Parthasarathy S, Drake CL, et al. Early cpap use identifies subsequent adherence to cpap therapy. Sleep. 2007;30:320–4. [PubMed] [Google Scholar]
- 11.Means MK, Ulmer CS, Edinger JD. Ethnic differences in continuous positive airway pressure (CPAP) adherence in veterans with and without psychiatric disorders. Behav Sleep Med. 2010;8:260–73. doi: 10.1080/15402002.2010.509255. [DOI] [PubMed] [Google Scholar]
- 12.Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of cpap adherence. Sleep. 2012;34:1653–8. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joo MJ, Herdegen JJ. Sleep apnea in an urban public hospital: Assessment of severity and treatment adherence. J Clin Sleep Med. 2007;3:285–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Wallace DM, Vargas SS, Schwartz SJ, Aloia MS, Shafazand S. Determinants of continuous positive airway pressure adherence in a sleep clinic cohort of South Florida Hispanic veterans. Sleep Breath. 2013;17:351–63. doi: 10.1007/s11325-012-0702-6. [DOI] [PubMed] [Google Scholar]
- 15.Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Sleep disorders in African Americans and Caucasian Americans: A meta-analysis. Behav Sleep Med. 2010;8:246–59. doi: 10.1080/15402002.2010.509251. [DOI] [PubMed] [Google Scholar]
- 16.Krakow B, Melendrez D, Ferreira E, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120:1923–9. doi: 10.1378/chest.120.6.1923. [DOI] [PubMed] [Google Scholar]
- 17.Ramos AR, Wohlgemuth WK, Dong C, et al. Race-ethnic differences of sleep symptoms in an elderly multi-ethnic cohort: The Northern Manhattan Study. Neuroepidemiology. 2011;37:210–5. doi: 10.1159/000334315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Connor GT, Lind BK, Lee ET, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: The Sleep Heart Health Study. Sleep. 2003;26:74–9. [PubMed] [Google Scholar]
- 19.Billings ME, Rosen CL, Wang R, et al. Is the relationship between race and continuous positive airway pressure adherence mediated by sleep duration? Sleep. 2013;36:221–7. doi: 10.5665/sleep.2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United States Department of Veterans Affairs. National Center for Veteran Analysis and Statistics. [cited 2012 October 8]; Available from: http://www.va.gov/vetdata/Veteran_Population.asp.
- 21.D'Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;49:1429–33. doi: 10.1016/s0895-4356(96)00271-5. [DOI] [PubMed] [Google Scholar]
- 22.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 23.Bakker JP, O'Keeffe KM, Neill AM, Campbell AJ. Ethnic disparities in cpap adherence in new zealand: Effects of socioeconomic status, health literacy and self-efficacy. Sleep. 2011;34:1595–603. doi: 10.5665/sleep.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 25.Weaver TE, Maislin G, Dinges DF, et al. Self-efficacy in sleep apnea: Instrument development and patient perceptions of obstructive sleep apnea risk, treatment benefit, and volition to use continuous positive airway pressure. Sleep. 2003;26:727–32. doi: 10.1093/sleep/26.6.727. [DOI] [PubMed] [Google Scholar]
- 26.Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable monitoring task force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2007;3:737–47. [PMC free article] [PubMed] [Google Scholar]
- 27.Iber C, Ancoli-Israel S, Chesson A, Quan SF for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 28.Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4:157–71. [PMC free article] [PubMed] [Google Scholar]
- 29.American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and coding manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 30.Shafazand S, Wallace DM, Vargas SS, et al. Sleep disordered breathing, insomnia symptoms, and sleep quality in a clinical cohort of US Hispanics in South Florida. J Clin Sleep Med. 2012;8:507–14. doi: 10.5664/jcsm.2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luyster FS, Buysse DJ, Strollo PJ., Jr Comorbid insomnia and obstructive sleep apnea: Challenges for clinical practice and research. J Clin Sleep Med. 2010;6:196–204. [PMC free article] [PubMed] [Google Scholar]
- 32.Aloia MS, Arnedt JT, Riggs RL, Hecht J, Borelli B. Clinical management of poor adherence to CPAP: motivational enhancement. Behav Sleep Med. 2004;2:205–22. doi: 10.1207/s15402010bsm0204_3. [DOI] [PubMed] [Google Scholar]
- 33.Shaw RN, Mckenzie S, Taylor T, et al. Beliefs and attitudes towards OSA evaluation and treatment among blacks. Sleep. 2012;35:A152. doi: 10.1016/s0027-9684(15)30217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adenekan B, Pandey A, Mckenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: role of racial/ethnic differences. Sleep Med Rev. 2013. http://dx.doi.org/10.1016/j.smrv.2012.07.002. [DOI] [PMC free article] [PubMed]
- 35.Ruiter ME, Decoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: A meta-analysis. Sleep Med. 2011;12:209–14. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 36.National Sleep Foundation. Summary of findings of 2010 Sleep in America Poll. 2010 [Google Scholar]
- 37.Platt AB, Field SH, Asch DA, et al. Neighborhood of residence is associated with daily adherence to cpap therapy. Sleep. 2009;32:799–806. doi: 10.1093/sleep/32.6.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: A systematic review. J Gen Intern Med. 2008;23:654–71. doi: 10.1007/s11606-008-0521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garb LR, Bootzin R, Dawson S, et al. Cognitive behavioral treatment for insomnia improves sleep efficiency and ISI in insomnia co-morbid with sleep apnea or periodic limb movements. Sleep. 2012;35:A243. [Google Scholar]