Abstract
Study Objectives:
To establish the extent to which the developmental changes in sleep timing experienced by Australian adolescents meet the International Classification of Sleep Disorders (ICSD-2) diagnostic criteria for delayed sleep phase disorder (DSPD), and whether adolescents with DSPD engage in poorer lifestyle choices, and are more impaired compared to good sleeping adolescents.
Methods:
Three-hundred seventy-four Australian adolescents (mean age 15.6 years, SD 1.0) participants completed a 7-day sleep diary, wore wrist actigraphy, and completed a battery of questionnaires to assess DSPD criteria.
Results:
The ICSD-2 criteria for DSPD were met by 1.1% (N = 4) of the adolescents sampled. The majority of adolescents (51.9%, N = 194) met one criterion, 14% (N = 52) of the adolescents met 2 criteria, while 33.2% (N = 124) did not fulfill any DSPD criteria. Despite having significantly delayed sleep timing, adolescents who met all criteria for DSPD reported similar lifestyle habits and daytime functioning. However, there were trends for greater alcohol and caffeine consumption, less sport participation, yet more time spent on extracurricular activities (i.e., learning to play a musical instruments for adolescents with DSPD.
Conclusions:
Despite the majority of adolescents reporting DSPD symptoms, only a small minority met full diagnostic criteria. Adolescents with DSPD reported similar lifestyle habits and daytime functioning to those with some or no symptoms. Future investigations of non-school-attending DSPD adolescents are needed to confirm the trends for lifestyle behaviors found in the present study.
Citation:
Lovato N; Gradisar M; Short M; Dohnt H; Micic G. Delayed sleep phase disorder in an australian school-based sample of adolescents. J Clin Sleep Med 2013;9(9):939-944.
Keywords: Adolescents, delayed sleep phase disorder, ICSD-2, daytime functioning
Delayed sleep phase disorder (DSPD) is an abnormal delay of the major sleep period in relation to the desired clock time.1,2 Individuals with DSPD report a chronic inability to fall asleep and awaken at socially acceptable times, which causes distress and/or significant impairment.1,2 The prevalence of DSPD is reported to be 7% to 16%.1,2 However, the prevalence is higher in adolescents, possibly due to the normative delay in sleep timing observed in this population.3–6 However, rates as low as 0.17% and 0.4% have been reported.7–9 Although not a formal assessment of DSPD, Saxvig and colleagues assessed the prevalence of delayed sleep timing (operationalized as difficulties falling asleep before 02:00 ≥ 3 nights/week, together with problems awakening at the desired time) in 1,285 Norwegian high school students to be 8.4%.6
A number of factors are likely to contribute to this disparity in prevalence rates. Firstly, higher prevalence rates are likely to result from less stringent classifications of DSPD; for example, classifying DSPD based only on the presence of delayed sleep timing without consideration of other diagnostic criteria. The use of such criteria results in prevalence estimates of “symptoms” rather than the “disorder” per se. Secondly, school-based samples are likely to result in more conservative estimates, given many adolescents with DSPD may not attend school on a regular basis.5 Finally, the rate of DSPD is likely reduced when studies consider differential diagnosis, such as an insomnia disorder or depression.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Despite the ubiquitous nature of delayed sleep timing during adolescence, there are few data estimating the extent of Delayed Sleep Phase Disorder in adolescent populations. The present study adds to the few investigations into this area that have reported statistics ranging from < 1% to 16%.
Study Impact: Despite the majority of adolescents reporting DSPD symptoms, only a small minority met full diagnostic criteria. Adolescents with DSPD reported similar lifestyle habits and daytime functioning to those with some or no symptoms.
Prevalence estimates of DSPD in adolescents have typically been derived using self-report questionnaires to assess sleep misalignment.6–10 To the authors' knowledge, no study has used sleep diaries or objective measures (i.e., actigraphy) to confirm the delay in sleep timing as per contemporary diagnostic criteria (ICSD-2). Therefore, it remains largely disputable whether the delay in the sleep period typically experienced during adolescence represents a common clinically significant problem within this population. Chronically late sleep onset times coupled with the need to rise at a socially conventional time to meet school commitments experienced by DSPD sufferers ultimately truncates the sleep period, thereby increasing daytime sleepiness and associated impairments.11,12 To date, one study has directly investigated the lifestyle habits and daytime functioning of adolescents with delayed sleep compared to good sleepers. Saxvig et al.6 reported delayed sleep timing was associated with lower average school grades, smoking, alcohol use, and elevated anxiety and depression scores. More independent studies are needed to confirm the influence of such lifestyle habits.
The primary aim of the current study was to establish the extent to which the developmental changes in sleep timing experienced by Australian adolescents meet the diagnostic criteria for DSPD as outlined in the ICSD-2. A second aim of the current study was to investigate whether adolescents with DSPD engage in significantly poorer lifestyle choices (e.g., excessive alcohol consumption) and are more impaired (e.g., school performance) compared to adolescents without DSPD. Such findings will help to identify potential risk factors pushing adolescents from a typical sleep delay to disordered sleep.
METHODS
Participants and Procedures
The initial sample included 385 adolescents aged 13-18 years (M = 15.6, SD 0.95, 59% male) who were recruited from 8 schools in Adelaide, South Australia. The schools were selected from a stratified sample based on socioeconomic status and included 7 coeducational and one single-sex boy's school. The study was promoted as a “health survey.” Adolescents completed questionnaires during school class time and maintained a record of their sleep habits using a 7-day sleep diary and wrist actigraphy (see Measures). During the 7 days of diary completion, adolescents telephoned the Flinders University Sleep Laboratory morning and night to record their bedtimes and wake times. These calls served as a validity check, to ensure diaries were completed twice daily and not retrospectively. Of the initial 385 students, 11 did not complete questionnaires or maintain an adequate record of their sleep habits. The final sample therefore comprised 374 adolescents, with a mean age of 15.6 (SD 1.0) years (59% male). Data collection occurred from April 2008 to April 2010, during school terms, at least 2 weeks either side of school holidays13 and not during daylight savings.14 All adolescents provided informed consent. This study was approved by the Flinders University Social and Behavioral Research Ethics Committee and the Department of Education and Children's Services Ethics Committee.
Measures
The ICSD-2 defined 4 diagnostic criteria for DSPD, including: (a) A delay in the phase of the major sleep period in relation to the desired sleep time and wake-up time, as evidenced by a chronic complaint of inability to fall asleep at a desired conventional clock time together with the inability of awaken at a desired and socially acceptable time; (b) When allowed to choose their preferred schedule, patients will exhibit normal sleep quality and duration for age and maintain a delayed, but stable, phase of entrainment to the 24-h sleep-wake pattern; (c) Sleep log or actigraphy monitoring for at least 7 days demonstrates a stable delay in the timing of the habitual sleep period; (d) The sleep disturbance is not better explained by another current sleep disorder, medical or neurological disorder, mental disorder, medication use, or substance disorder. The measures used to assess each ICSD-2 criterion for delayed sleep phase disorder (DSPD) are outlined in Table 1.
Table 1.
Measures used to diagnose ICSD-2 delayed sleep phase disorder (DSPD)
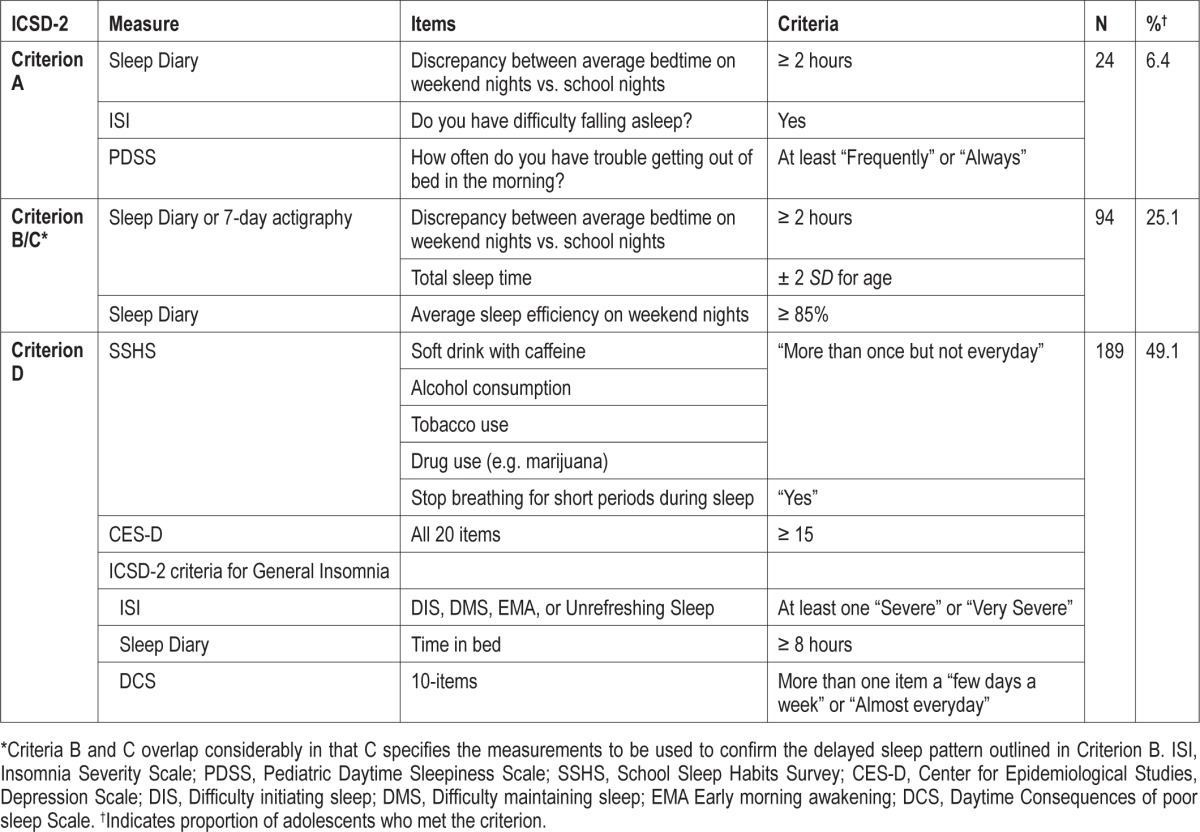
A 7-day sleep diary was used to obtain a self-report measure of adolescents' sleeping patterns, in particular bedtime, total sleep time, time in bed, and sleep efficiency. The discrepancy between average bedtime on weekend nights versus school nights was used to address the delay in the phase of the major sleep period in relation to the desired sleep/wake time. Total sleep time for each adolescent was compared to age normative data15 to address whether the adolescent experienced normal sleep duration for age. Sleep efficiency > 85% on weekend nights was used to assess whether the adolescent exhibited normal sleep quality. Adolescents meeting criteria for ICSD General Insomnia16 (see Table 1 for explicit criteria) were excluded from the DSPD classification. Wrist actigraphy (Ambulatory Monitoring Inc., Ardsley, NY) was used in conjunction with the sleep diaries to provide an objective measure of the adolescents' sleep timing.
The ISI (Insomnia Severity Index17) is a 7-item self-report measure, which assessed complaints of difficulty initiating (DIS) or maintaining sleep (DMS), or unrefreshing sleep. Each item was rated from 0 “not at al” to 4 “very severe.” The item “Do you have difficulty falling asleep” from the ISI was used to address a chronic complaint of inability to fall asleep at a desired conventional clock time.
The Pediatric Daytime Sleepiness Scale (PDSS18) was used to address the inability to awaken at a desired and socially acceptable time outlined in Criterion A (i.e., item #5 “How often do you have trouble getting out of bed in the morning?”).
The School Sleep Habits Survey (SHSS19) comprises questions about sleep/wake behaviors, sleep hygiene practices (e.g., caffeine/alcohol consumption, drug use), sleep and medical conditions, and non-school activities (e.g., sport and part-time work). The SHSS was used to exclude excessive caffeine and alcohol consumption, tobacco and drug use, or other respiratory problems during sleep as alternate explanations for adolescents' sleep disturbance. The SHSS was also used to compare the lifestyle habits and daytime functioning of adolescents with and without DSPD.
The Centre for Epidemiological Studies Depression Scale (CES-D20) is a 20-item self-report measure that was used to identify clinical levels of depression and hence exclude this as an alternate explanation for sleeping difficulties. Adolescents rated statements, such as “I felt depressed,” using a 4-point Likert scale (1 “rarely or none of the time [less than 1 day]” to 4 “most or all of the time [5 to 7 days]).”
RESULTS
Of the 374 adolescents with complete data, 1.1% (N = 4) met the full ICSD-2 criteria for DSPD, while 33.2% (N = 124) did not fulfill any of the criteria. The majority of adolescents (51.9%, N = 194) met one criterion, and 14% (N = 52) met 2 criteria. Table 1 summarizes the proportion of adolescents who fulfilled each of the criteria separately.
A series of between group nonparametric comparisons were conducted to assess potential demographic, subjective sleep, and daytime functioning differences between adolescents with and without DSPD. Between-group comparisons involving adolescents who met all criteria are statistically underpowered (N = 4). Therefore, effect sizes are also reported for marginally nonsignificant (p = 0.05 to 0.10) comparisons involving this group to provide an index of the relative strength of any differences between groups (See Table 3). Table 2 display demographic information, subjective sleep, and daytime functioning variables between these groups. Information on lifestyle practices such as sleep hygiene practices and sleeping aid use were also analyzed.
Table 3.
Effect sizes for comparisons of sleep hygiene practices and daytime behaviors for adolescents without DSPD, those who met 1 criterion, and those who met 2 or more criteria
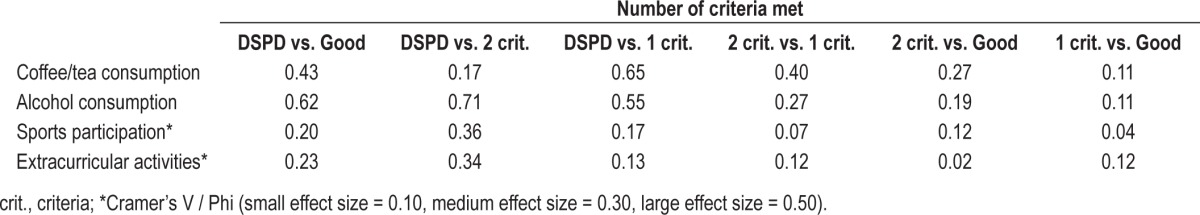
Table 2.
Demographic, subjective sleep, daytime functioning, sleep hygiene practices, and use of sleeping aids (presented as median values or proportions) for good sleepers, those without DSPD, and those who met either 1 or 2 criteria
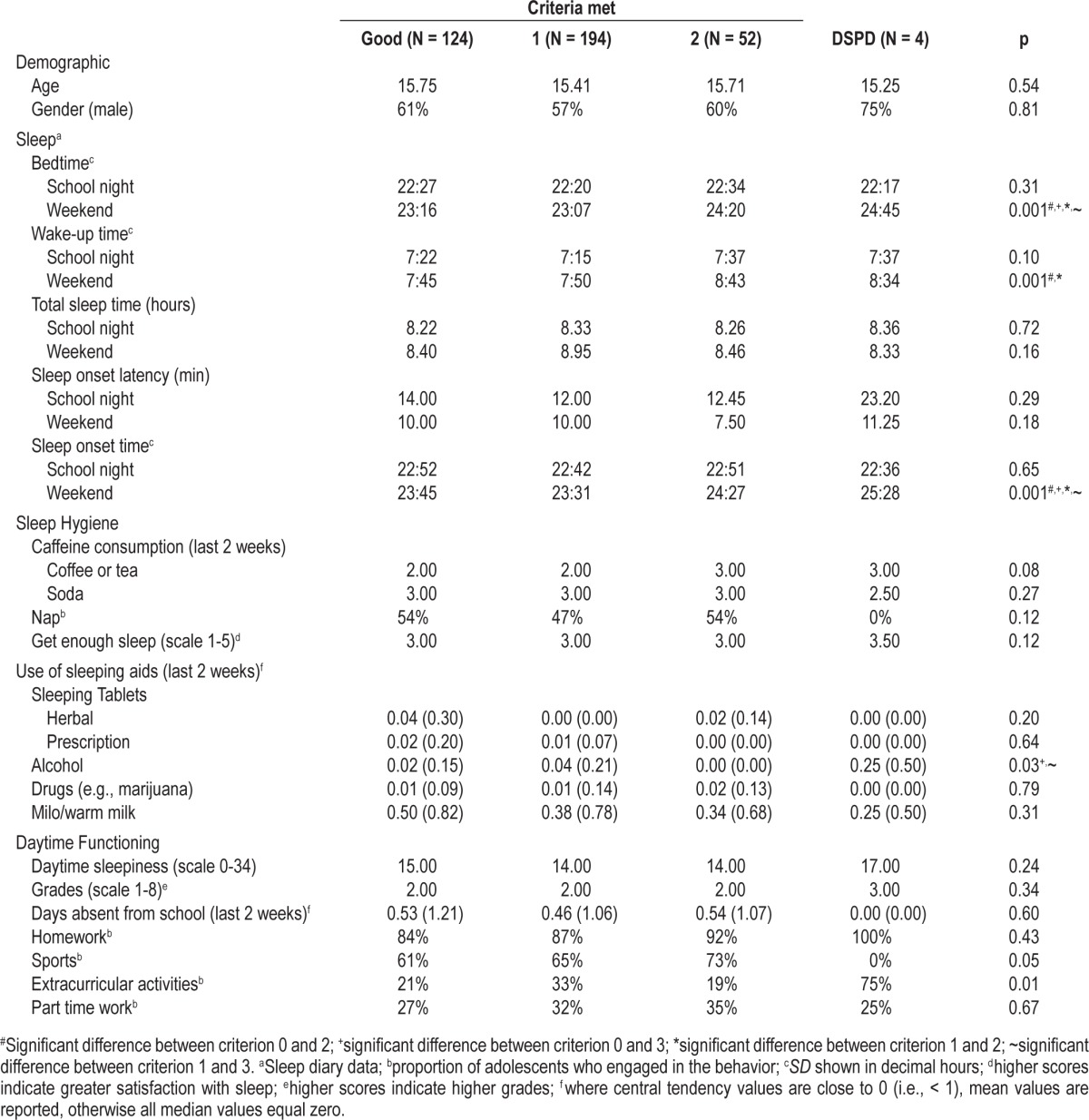
Age and gender did not differ significantly between groups (p > 0.05). Despite reporting similar total sleep time of about 8.5 h on both weekends and school nights, the 4 groups differed significantly in bedtime (p = 0.001), sleep onset time (p = 0.001), and wake up time (p = 0.001), but only on weekends. Adolescents who met all criteria for DSPD reported going to bed at 00:45, 1 h 29 min later than those who did not meet any criteria (p = 0.037), 1 h 38 min later than those adolescents who met 1 criterion (p = 0.023), and 25 min later than those adolescents who met 2 criteria (p = 0.31). The sleep onset time of adolescents who met all criteria was 01:28, which was about 2 h later than the sleep onset time reported by adolescents who did not meet any criteria (p = 0.04) or met only 1 criterion (p = 0.009). Adolescents who met all criteria reported waking at 08:34, which was moderately later than the wake up time reported by adolescents who met either 1 criterion or no criteria, but earlier than those who met 2 criteria (p values = 0.31-0.37 ds = 0.27- 0.45). Although sleep onset latency on weekends did not differ significantly among the 4 groups (p > 0.05), there was a small trend for DSPD adolescents to fall asleep faster than adolescents who met either 1 or 2 criteria (d = 0.15 to 0.35).
Adolescents reported similar sleep hygiene practices (all p values > 0.05); however, there was a moderate trend towards more alcohol and caffeine consumption (from tea/coffee) among DSPD adolescents compared to adolescents classified into the other 3 groups. Despite the reported use of sleeping aids being very low among all adolescents sampled (all p values > 0.05), there was a moderately strong tendency for DSPD adolescents to report being more satisfied with the amount of sleep they get relative to adolescents in the other groups (d = 0.68-0.99).
The daytime functioning of the adolescents in the current sample did not differ statistically among the 4 groups on any measure (grades obtained, levels of daytime sleepiness; all p values > 0.05). Adolescents who met all criteria did, however, tend to report spending less time participating in sporting activities (d = 0.17 to 0.36) and more time engaging in extracurricular activities relative to adolescents in the other 3 groups.
DISCUSSION
The current study aimed to establish the extent to which the delay in sleep timing experienced by many Australian adolescents meet the ICSD-2 criteria for DSPD, as well as to examine whether these adolescents with DSPD engage in poorer lifestyle habits and experience impaired daytime functioning. Of the adolescents sampled, 1.1% met the ICSD-2 criteria for DSPD. This proportion is lower than those reported in previous studies (range 7% to 16%).1,2,6 These earlier studies diagnosed DSPD based on a delay of sleep timing independent of other diagnostic characteristics (e.g., daytime impairments), and did not screen for alternate explanations for the delay in sleep timing (e.g., insomnia disorders), which would have lowered their rate. Acknowledging this limitation, Saxvig and colleagues6 incorporated the presence of daytime impairment (e.g., over-sleeping in the morning or sleepiness at school) in addition to delayed sleep timing in their sample of Norwegian adolescents. In doing so, they concluded a prevalence of 8.4%. A similar proportion of 6.4% was found among our sample when using only self-report measures of delayed sleep timing and difficulty waking in the morning (see Criterion A, Table 1). Including differential diagnosis and the significant distress the sleep problem has on functioning are likely to reduce estimates. Many more studies of the prevalence rate for DSPD in adolescents are needed to confirm our data.
All adolescents in our Australian sample reported similar lifestyle habits and daytime functioning. The use of sleeping aids and sleep hygiene practices, such as daytime napping, were comparable between adolescents with and without DSPD. However, adolescents with more DSPD symptoms (i.e., met 2 or 3 criteria) consumed significantly more caffeine from coffee and/or tea, as well as alcohol, when compared to those who only met 1 criterion. DSPD adolescents may use caffeine in the morning to increase daytime alertness21 yet use alcohol to assist with sleep onset.6 Daytime functioning did not differ between groups, although there was a trend for adolescents who met DSPD criteria to participate in fewer sporting activities but more extracurricular activities (e.g., learning to play a musical instrument; see small effect sizes in Table 3) when compared to those who met fewer criteria. Approximately 60% of Australian adolescents participate in sporting activities,22 and sports are often played on weekend mornings, which may prevent adolescents from sleeping in on weekends, further delaying their circadian timing.23
The lack of differences in the lifestyle habits and daytime functioning of adolescents with and without DSPD observed in the current sample is inconsistent with previous research. Although research directly comparing the lifestyle habits and daytime functioning of adolescents with and without DSPD is limited, Saxvig et al.6 reported delayed sleep timing was associated with lower average school grades, smoking, alcohol use, and elevated anxiety and depression. Their delayed Norwegian adolescents were only receiving 6 hours 53 minutes of sleep; 1 hour less than those without (7 h 53 min). Our Australian adolescents received ∼8 hours 30 minutes sleep, which did not differ among the four groups. Therefore, poorer daytime functioning and lifestyle choices of delayed adolescents may be a function of restricted nocturnal sleep rather than circadian influences per se.
Limitations
Our current sample size was somewhat limited due to the use of sleep diaries, and especially, wrist actigraphy. Therefore, it is difficult to draw a precise prevalence of DSPD among Australian adolescents. We recommend that future research endeavors use sleep diaries in the assessment of adolescent DSPD but avoid the time and expense of actigraphy for the benefit of a larger and more representative sample. Using semi-structured interviews alongside sleep diaries would also be recommended, as interviews provide more rich data than using cutoff scores on single items from questionnaires. Ideally future research should sample a broader cross-section of Australian adolescents, including those living in remote and rural regions, to provide an accurate estimate of DSPD. Finally, our sampling was conducted solely within schools. This may explain minimal differences in school week sleep patterns, as these DSPD adolescents are able to attend school. Sampling both attenders and non-attenders will not only provide more accurate results but likely produce a higher estimate. For example, in a previous study, 16% of Australian adolescents seeking treatment for their DSPD did not currently attend school.24 If we apply this weighted factor of 16% to the current sample, the prevalence rate would produce a modest rise from 1.1% to 1.3%.
CONCLUSION
The current study is one of the first to assess the extent to which developmental changes in adolescent sleep timing meet ICSD-2 diagnostic criteria for DSPD. The proportion of adolescents experiencing DSPD in our Australian sample was 1 in 100. DSPD arises due to a conflict between an individual's biology and society's expectations. Notwithstanding different methods of measurement, and assuming the biological etiology of DSPD is consistent across adolescent samples, variable prevalence rates are likely due to varying societal factors between countries.5 More studies assessing rates of DSPD are needed to provide a contemporary picture of the impact of this sleep disorder on the ∼1 billion adolescents in the developing world.25,26
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Gradisar has performed paid speaking engagements for the Australian Psychological Society. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This research was supported through grants from the Australian Research Council and the Faculty of Social and Behavioral Sciences at Flinders University. The authors thank Jason Gill, Anna Johnston, Emma Currie, and Lisa-Marie Colton who assisted with data collection, the school principals, and the 385 adolescents and their parents for their participation in this project. This study was funded by an Australian Research Council Discovery Project grant (#DP0881261).
REFERENCES
- 1.American Academy of Sleep Medicine. The international classification of sleep disorders: diagnostic and coding manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders test revision. 4th ed. Washington, DC: American Psychiatric Association; 2001. [Google Scholar]
- 3.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–62. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 4.Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8:602–12. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12:110–8. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Saxvig IW, Pallesen S, Wilhelmsen-Langeland A, Molde H, Bjorvatn B. Prevalence and correlates of delayed sleep phase in high school students. Sleep Med. 2012;13:193–9. doi: 10.1016/j.sleep.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 7.Schrader H, Bovim G, Sand T. The prevalence of delayed and advanced sleep phase syndromes. J Sleep Res. 1993;2:51–5. doi: 10.1111/j.1365-2869.1993.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 8.Hazama GI, Inoue Y, Kojima K, Ueta T, Nakagome K. The prevalence of probable delayed-sleep-phase syndrome in students from junior high school to university in Tottori, Japan. Tohoku J Exp Med. 2008;216:95–8. doi: 10.1620/tjem.216.95. [DOI] [PubMed] [Google Scholar]
- 9.Ohayon MM, Roberts RE, Zulley J, Smirne S, Priest RG. Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39:1549–56. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 11.Alvarez B, Dahlitz MJ, Vignau J, Parkes JD. The delayed sleep phase syndrome: clinical and investigative findings in 14 subjects. J Neurol Neurosurg Psychiatry. 1992;55:665–70. doi: 10.1136/jnnp.55.8.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hansen M, Janssen I, Schiff A, Zee PC, Dubocovich ML. The impact of school daily schedule on adolescent sleep. Pediatrics. 2005;115:1555–61. doi: 10.1542/peds.2004-1649. [DOI] [PubMed] [Google Scholar]
- 13.Warner S, Murray G, Meyer D. Holiday and school-term sleep patterns of Australian adolescents. J Adolesc. 2008;31:595–608. doi: 10.1016/j.adolescence.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Schneider A, Randler C. Daytime sleepiness during transition into daylight saving time in adolescents: Are owls higher at risk? Sleep Med. 2009;10:1047–50. doi: 10.1016/j.sleep.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–7. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 16.Dohnt H, Gradisar M, Short MA. Insomnia and its symptoms in adolescents: comparing DSM-IV and ICSD-II diagnostic criteria. J Clin Sleep Med. 2012;8:295–9. doi: 10.5664/jcsm.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morin C. Insomnia: psychological assessment and management. New York: The Guilford Press; 1993. [Google Scholar]
- 18.Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Pietro B. The pediatric daytime sleepiness scale (PDSS): sleep habits and school outcomes in middle-school children. Sleep. 2003;26:455–8. [PubMed] [Google Scholar]
- 19.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1997;1:385–401. [Google Scholar]
- 21.Calamaro CJ, Thornton BAM, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 22.Australian Bureau of Statistics. Participation in sport and physical recreation, Australia, 2011-12 (4177.0) Canberra, Australia: Australian Bureau of Statistics; 2012. [Google Scholar]
- 23.Crowley SJ, Carskadon Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol Int. 2010;27:1469–92. doi: 10.3109/07420528.2010.503293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gradisar M, Dohnt H, Gardner G, et al. A randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep. 2011;34:1671–80. doi: 10.5665/sleep.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.United Nations. World population prospects: The 2004 revision: File 1: Total population both sexes by age group, major area, region and country, annually for 1950-2050 (in thousands) (Pop/DB/WPP/Rev.2004/4/F1) New York, USA: Population Division, Department of Economic and Social Affairs, United Nations; 2005. [Google Scholar]
- 26.United Nations Population Fund. State of world population: Adolescent fact sheet. 2005. Retrieved from: http://www.unfpa.org/swp/2005/presskit/factsheets/facts_adolescents.htm(1/11/12)


