Abstract
Functional studies of human primary immune cells have been hampered by the lack of tools to silence gene functions. Here we report the application of a lentiviral RNAi library in primary human T cells. Using a subgenomic shRNA library targeting ~1,000 signaling genes, we identified novel genes that control the levels of IL-10 produced. IL-10 is a potent anti-inflammatory cytokine secreted by several cell types, including Tr1 cells, a subset of Tregs that exert their suppressive activity through IL-10 secretion. FLT3, a known hematopoeitic growth factor, was found to be a negative regulator of IL-10 levels in activated T cells. This was based on several observations. First, FLT3 and its ligand, FL, were both induced by T cell activation. Second, silencing of FLT3 led to increased IL-10 levels while addition of FL suppressed IL-10 secretion and increased FLT3 surface levels. Third, engagement of CD46, a known inducer of Tr1 regulatory T cells, upregulated surface FLT3 and secreted FL, which then inhibited IL-10 production in T cells. Hence, FL and FLT3 form a novel regulatory feedback loop that limits IL-10 production in T cells. Our results identified Flt3 as a new regulator of T cell function and offer a strategy to genetically dissect specific pathways in T cells.
INTRODUCTION
Cytokine production is of major importance in controlling the outcome of the immune response. Among them, IL-10 was first described as the cytokine synthesis inhibitory factor (CSIF) (1) due to its potent regulatory functions. It downmodulates Th1 response, and has potent anti-inflammatory properties. It notably characterizes a subset of regulatory T cells, called Tr1, which attenuate immune responses by secreting large amount of IL-10 that mediates bystander suppression (2). Animal models further reinforce the regulatory functions of IL-10. While IL-10 deficient mice develop colitis (3), IL-4 and IL-10 treatments can inhibit the development of Type I diabetes in NOD mice (4, 5). Hence, IL-10 is a central cytokine, and the generation of IL-10-producing cells as well as the understanding of the mechanisms controlling IL-10 secretion, have generated a large interest in the community for clinical purposes. A recent cohort of papers demonstrated the role of IL-27 along with TGFβ and IL-6 in inducing IL-10 in murine models (6–9). Human IL-10-producing cells (or Tr1) can be generated in vitro by stimulation with vitamin D3 and dexamethasone (10), or by stimulation with CD46 (11), a complement binding receptor that activates T cells (12). In the mouse model of multiple sclerosis (MS), vitamin D(3) strongly inhibits myelin oligodendrocyte peptide-induced experimental autoimmune encephalomyelitis (EAE). This is dependent on functional IL-10 and IL-10R, demonstrating the role of IL-10 in preventing EAE (13). Similarly, in humans, increasing evidence shows a regulatory role of IL-10 in pathologies. In most patients with MS in the relapsing-remitting stage, IL-10 production by CD46-induced Tr1 cells is defective (14–17). Likewise, IL-10 plays a role in asthma. A subgroup of patients with asthma is resistant to glucocorticoid treatment. However, treatment with vitamin D3 and dexamethasone reverses this resistance by inducing IL-10 producing cells (18, 19). Nevertheless, the signaling pathways that lead to IL-10 production in human immune cells are not well understood.
While there has been effective progress in our understanding of T cell differentiation in animal models, our ability to develop human therapeutics requires a better understanding of human-specific mechanisms that animal models may not be able to recapitulate. However, human studies have been challenging in part due to lack of tools to carry out causal experiments in primary immune cells.
Systematic loss-of-function genetic screens provide an unbiased approach to deciphering genetic networks across many model organisms. More recently, advances in gene silencing using RNA interference (RNAi) have enabled loss-of-function genetic studies in diverse organisms and cell types (20–22). Using an RNAi-based approach to dissect the molecular pathways that control the balance of cytokines secreted by helper T cells, we identified regulators of cytokine production that had not been previously described. Among them, FLT3 (fms-related tyrosine kinase 3) was selected for further studies. We show that the FLT3-FL ligand-receptor pair acts in a negative feedback loop to limit IL-10 levels in response to activation of human T cells. FLT3 (also called FLK2) is part of a class of receptor tyrosine kinases that includes KIT, FMS and PDGFR (23). It is characterized by five extracellular immunoglobulin-like domains and a short cytoplasmic tail with kinase activity (24). Human FLT3 (or CD135) was first identified as STK1 (stem cell tyrosine kinase), and is highly homologous to its murine counterpart (25, 26). It is highly expressed in CD34+ hematopoietic cells, which defines progenitor cells, and has a role in hematopoiesis. Disruption of FLT3 doesn’t affect the viability of the mice. However transplantation of these cells failed to reconstitute both T and myeloid cell compartments (27). Here, we demonstrate a new role of FLT3 in regulating IL-10 production. FLT3 and its ligand, FL, were both induced by T cell activation. Silencing of FLT3 led to increased IL-10 levels while addition of FL suppressed IL-10 secretion and increased FLT3 surface levels. Moreover, CD46 activation, a known inducer of Tr1 regulatory T cells, upregulated surface FLT3 and secreted FL, which then inhibited IL-10 production in T cells. Hence, FL and FLT3 form a novel regulatory feedback loop that limits IL-10 production in T cells. These results demonstrate the inducible expression of FLT3 in primary human T cells and its novel role in the regulation of IL-10 secretion by activated and/or differentiated T cells. Therefore, by using an RNAi library, we were able to identify new proteins involved in the regulation of cytokine production. Moreover, our studies demonstrate that a lentiviral RNAi library can be readily used to silence genes in human T cells and paves the way for diverse screens to dissect primary human T cell functions.
Materials and Methods
TRC RNAi library
The complete description of the RNAi Consortium lentiviral RNAi library used in this study has been reported(28). Briefly, human genes were targeted with ~5 shRNAs expressed under the control of the U6 Pol III promoter in a lentiviral vector (pLKO.1) vector that also confers puromycin resistance. Plasmid DNA purification and lentiviral production were performed as described(28) and http://www.broad.mit.edu/rnai/trc/lib.
T cell stimulation and infection
PBMC were isolated from heparinized venous blood by Ficoll-Hypaque density gradient centrifugation (Pharmacia LKB Biotechnology) from healthy donors after informed consent. CD4+ T cells were then negatively isolated using magnetic beads (CD4 isolation kit II, Miltenyi Biotec, purification > 90%). T cells were then cultured in 96-well plates pre-coated with anti-CD3 (OKT3, 2.5µg/ml), anti-CD28 (2D10, 2.5µg/ml), in presence of human recombinant IL-2, (Tecin (TM), National Cancer Institute, Frederick, Maryland)(20U/ml) for 24 hours before infection. The infection was carried out by centrifugation for 90 min at 2300 rpm at room temperature, in presence of the viral supernatant and polybrene (8 µg/ml). After removal of the virus, fresh medium was added. Infected cells were then selected by addition of puromycin (2,5 µg/ml) 48 hrs after infection, and the cells were expanded in IL-2 for 10 days. Secondary stimulation was then performed in conditions similar to the primary stimulation. 24hrs later, supernatants and cells were harvested. Cell numbers and viability were assessed by flow cytometry. For the primary RNAi screen, ~8 96-well plates were infected per experiment (with one well per shRNA), and the full screen consisted of more than 6 independent experiments using different donors.
For stimulation of non-infected primary T cells, 50,000 CD4+T cells were stimulated as mentioned above, in presence or absence of FL (as indicated, R&D) for 48–72 hrs, before analysis by flow cytometry or determination of cytokine production in the supernatants by ELISA.
Proliferation, ELISA and FACS
Proliferation was determined by incorporation of 3H-thymidine, or by flow cytometry by gating on the live cell population. Cytokine production was determined in cell culture supernatants using ELISA specific for human IL-10 (BD Pharmingen), IL-13 and IFNγ (Endogen). FL concentrations in supernatants were determined by ELISA (Quantikine ELISA from R&D Systems). FLT3 expression was assessed by flow cytometry using anti-FLT3-PE (BD), or an irrelevant control IgG1-PE. PCR amplification of FLT3 was performed according to (25).
Z-score calculation
We calculated a Z-score to assess changes in cytokine levels in a single well relative to the mean level of the cytokine across all wells of the same plate. Levels of secreted T cell cytokines were measured using cytokine ELISAs for each 96-well plate well and represented as C={C1, C2, ….C96}, excluding wells for which cell counts were below 500 cells. We calculated a score for the cytokine level in a well as: Zi=(Ci-µ)/σ, in which is the µ and σ are the mean and standard deviation of C, respectively.
Statistics
The data were analyzed using the Prism software and compared using the Mann-Whitney test, a non-parametric test that does not assume Gaussian variation. ELISA and proliferation data are the average of triplicate wells.
RESULTS
Effective lentiviral infection and gene silencing enable loss-of-function RNAi screening in primary human T cells
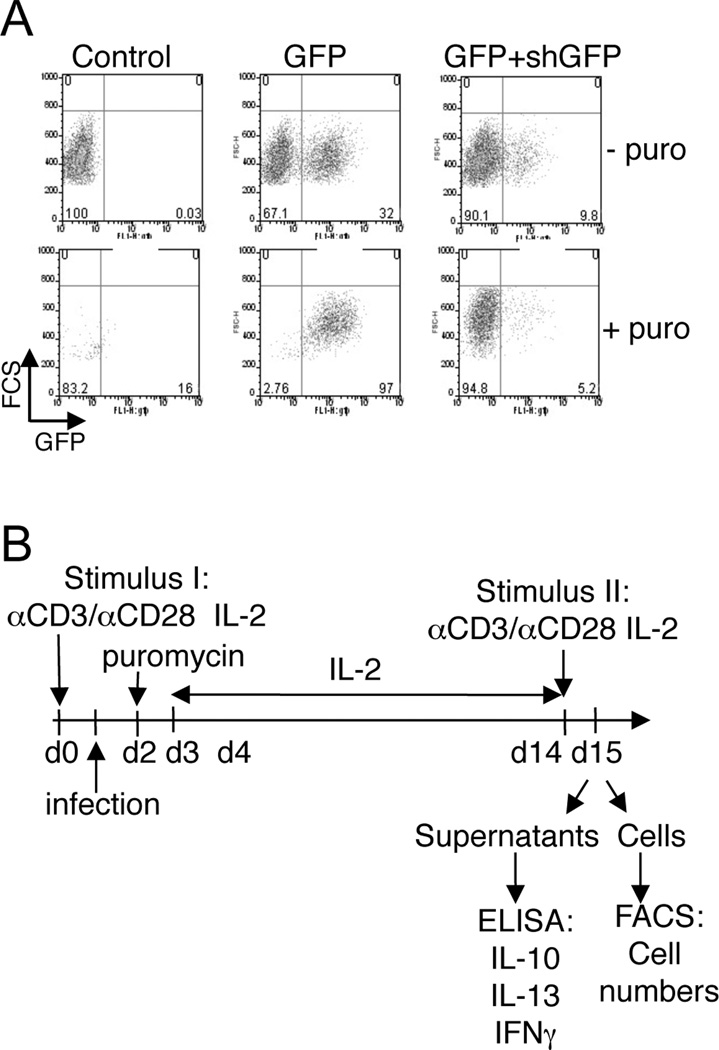
In order to identify genetic elements required for primary human T cell functions, we were interested in applying large-scale RNAi libraries to unbiased genetic screens in primary human T cells. To develop such a strategy, we first demonstrated that primary human T cells could be efficiently infected by lentiviruses from the TRC1 RNAi library (28). Primary CD4+ T cells isolated from blood were activated with anti-CD3/CD28 antibodies, in the presence of IL-2 for 3 days and infected with a GFP-expressing lentivirus. GFP expression was detected in 30% of primary T cells by flow cytometry (Figure 1A) or fluorescence microscopy (data not shown). Puromycin selection of infected cells resulted in 97% of T cells expressing GFP (Figure 1A, lower panels). As in previous reports, naïve T cells were not appreciably infected with HIV-derived lentivirus (29, 30). Second, to test for RNAi-mediated gene silencing activity in primary T cells, T cells were co-infected with a lentivirus expressing an shRNA targeting GFP, resulting in almost complete knockdown of GFP (Figure 1A, right panels). These data demonstrate both efficient infection and gene silencing in primary human T cells.
Figure 1. Infection of primary human T cells by GFP-lentivirus.
(A) CD4+ primary human T cells were either not infected (control), infected by lentivirus encoding GFP (GFP) (LKO.3pgw) or co-infected by lentivirus encoding GFP and shGFP (GFP+shGFP). Twenty-four hours later, puromycin (2.5µg/ml) was added. Three days after infection, the percentage of infected cells (FL1+) was assessed by flow cytometry. (B) The optimized protocol used for the RNAi screen is depicted.
In preparation for larger scale screening, we next optimized infection protocols and restimulation conditions to assess cytokine production in infected T cells. Cells were stimulated as above, infected with a GFP-expressing virus, allowed to rest in fresh plates for 7–10 days with IL-2, and stimulated again with anti-CD3/CD28 antibodies (Figure 1B). The delay in 7–10 days before secondary stimulation of T cells allowed us to avoid contamination by cytokines produced in response to the primary pre-infection stimulation and to reduce levels of pre-existing proteins corresponding to targeted mRNAs due to cell division. As the titer of added lentivirus was different from well to well, we sought to find cell culture conditions for which the phenotypic measurements were not significantly altered by variability in virus titer. We titrated the amount of viruses and seeded T cells, and assessed the viability, infection rate and IL-10 production resulting from secondary stimulation. While variability in IL-10 secretion was observed when infecting with different amounts of virus at lower cell seeding densities, an initial culture of 25,000 cells per well minimized this variability (data not shown). By optimizing several conditions, we thus developed a protocol to infect cells and assess cytokine production in a way that was mostly independent of variations in virus titer between distinct library constructs.
An RNAi screen identifies novel genes that regulate cytokine production
We carried out an RNAi screen using a sub-genomic library targeting ~1,000 genes, focused on kinases and phosphatases, and containing 3–5 shRNAs per gene. Our goal was to identify regulators of cytokines that reflect key T cell states. This included IFNγ and IL-13 for Th1 and Th2 differentiated T cells, respectively, and IL-10, a potent anti-inflammatory cytokine produced by a variety of cells, and hallmark of regulatory Tr1 cells. T cells from each well were stimulated with anti-CD3/CD28 antibodies, infected with lentivirus particles expressing a distinct and unique shRNA, selected for infection with puromycin and expanded in IL-2 for 10 days. At 10–14 days post-infection, cells were restimulated with anti-CD3/CD28 antibodies in the presence of IL-2. At 24 hours post-restimulation, the numbers of viable cells were assessed by flow cytometry, and the levels of IL-10, IL-13 and IFNγ were determined by ELISA. Cell numbers assessed by flow cytometry and proliferation measured using 3H-thymidine were highly correlated (data now shown). We excluded wells containing less than 500 viable cells from the analysis. Using a statistical Z-score (see methods), to quantify the deviation of cytokine levels from the mean of all measurements for that cytokine within the same plate, we selected shRNAs that induced significantly higher or lower levels of IL-10, IL-13 and IFNγ. The amounts of each cytokine produced after infection with control shRNAs (against non-mammalian reporter genes) were not significantly altered (Figure 2A). We selected 55 hit genes for which two or more hairpins induced a similar effect on cytokine production, which were reanalyzed in a secondary screen. The Z-scores for each individual hairpin across independent experiments (including the primary screen and additional tests) using different donors are shown in supplementary Figure S1 and Table I. Supporting the selection criteria, we found that ZAP70 knockdown led to reduced IFNγ production, in agreement with prior studies in patients with ZAP70 deficiencies exhibiting reduced IFNγ production(31) and that PRKR knockdown increased IFNγ production which was again in accordance with former studies indicating that PRKR controls IFNγ translation (Figure 2A).
Figure 2. Summary of cytokine measurement across multiple RNAi experiments.
(A) The mean of the Z scores obtained for the best constructs of the selected genes modulating IL-10, IL-13 and IFNγ in both primary and secondary screens, and other experiments for some genes, are plotted. The Z-score is defined as the difference between the value of a cytokine measurement in a particular well and the mean of the plate, divided by the standard deviation of the plate (i.e. how many standard deviations a particular measurement is from the mean). (B) Z-scores obtained for each individual shRNA construct targeting FLT3, across multiple independent experiments. (C) Correlation between the efficacy of knockdown and phenotype. The remaining gene expression of FLT3 after infection with the different hairpins was quantified by qRT-PCR. We determined the expression levels compared to T cells infected with controls hairpins, and calculated the percentage of remaining expression. This was plotted relative to the Z-score phenotype obtained for each construct.
The importance of IL-10 in controlling inflammation and autoimmunity and our previous observation of lower IL-10 levels in multiple sclerosis patients (14, 32) led us to focus on a novel regulator of IL-10 identified in our screen. Two shRNAs targeting FLT3, a receptor tyrosine kinase, led to an increase in IL-10 secretion (Figure 2B), suggesting that FLT3 is a negative regulator of IL-10 secretion upon T cell activation. Moreover, using qRT-PCR to assess knockdown of FLT3, we found an inverse correlation between the amount of knockdown and the phenotypic score (Figure 3C).
Figure 3. FLT3 expression in T cells and effect of FLT3 ligand (FL) on FLT3 expression.
(A) FLT3 expression on human CD4+ T cells. Human CD4+ T cells were purified and stimulated by anti-CD3/CD28 antibodies in the presence of IL-2. Forty-eight hrs later, FLT3 expression was analyzed by flow cytometry using an anti-FLT3-PE or irrelevant IgG1-PE control antibody. Data shown was representative of 6 experiments. (B) T cells were activated as in (A), before analysis of FLT3 expression by RT-PCR. (C) FLT3-L (FL) modulates FLT3 expression at the cell surface. Human CD4+ T cells were stimulated by anti-CD3/CD28 antibodies in the presence of increasing doses of FL. FLT3 expression was assessed after 3 days of culture. The relative percentage of FLT3 expressing cells is also plotted. Representative of 4 experiments. (D) CD4+ T cells were left unstimulated (Ctrl), stimulated by anti-CD3 or anti-CD3/CD28 antibodies for 3 days. The concentrations of FL in the supernatants were then determined by ELISA.
FLT3, a negative regulator of IL-10 secretion, and its ligand are expressed in activated human T cells
Since FLT3 was known to be expressed in CD34+ progenitor cells and thymocytes, but its expression in mature T cells was not previously reported (25), we first examined whether FLT3 and its ligand, FLT3-ligand (FL), were expressed in resting and activated human T cells. Using purified human CD4+ T cells, we found that while FLT3 expression was undetectable by flow cytometry in resting cells, it was detectable at low but significant levels upon stimulation with anti-CD3/CD28 antibodies in the presence of IL-2 (Figure 3A). Moreover, the presence of FLT3 in activated T cells could be also detected by PCR (Figure 3B). Second, it could be further upregulated by addition of FL to activated T cells (Figure 3C), suggesting a positive feedback loop between ligand and receptor.
Finally, we hypothesized that the original phenotype observed in FLT3 KD cells (Figure 2) would have required expression of FL by activated T cells to engage FLT3, as no exogenous FL was added to the culture. The predominant human FL form is a transmembrane protein that can undergo proteolytic cleavage to generate a soluble form of the protein (33). An alternatively-spliced FL mRNA, encoding a soluble form of the human FL, has also been identified (33, 34). Consistent with our prediction, we found significantly higher levels of FL in the supernatants of CD3/CD28 stimulated T cells (Figure 3D). Supporting this observation, FL is known to have a broad RNA expression in human tissues and a high level of expression in peripheral blood lymphocytes (33, 35), and T cells (34). These observations demonstrate that expression of FLT3 and its ligand, FL, are both induced by engagement of CD3 and CD28 in T cells, and that FLT3 levels could be further increased in response to its ligand in a positive feedback loop.
Exogenous FL inhibits IL-10 secretion by activated T cells
To directly test whether FLT3 activation by FL results in IL-10 production, we added recombinant human FL at several concentrations to T cell cultures stimulated with anti-CD3/CD28 antibodies in the presence of IL-2. The resulting changes in proliferation, IL-10 and IFNγ production were assessed after 3 days (Figure 4A). Addition of FL to T cell culture decreased IL-10 production to ~50% of control levels but had minimal effect on proliferation and IFNγ production. We next determined whether the strength of TCR stimulation could modulate the inhibition of IL-10 mediated by FL. Increasing the doses of anti-CD3 antibodies led to a stronger inhibition of IL-10 by FL (Figure 4B). To further demonstrate a role of FLT3 in IL-10 production, we next assessed the effect of FL on IL-10 secretion in T cells infected with different shRNA constructs targeting FLT3. Only efficient knockdown of FLT3 in T cells abolished the repression of IL-10 by added FL (Figure 4C). FL inhibited IL-10 production by T cells infected with a non-silencing shRNA (#3), similarly to T cells infected with GFP-control, while it had no effect on T cells infected with a silencing shRNA construct (#4). These results are consistent with the hypothesis that FL acts through FLT3 on activated T cells to reduce IL-10 levels.
Figure 4. FLT3 ligand (FL) inhibits IL-10 production.
(A) CD4+ T cells were stimulated by anti-CD3 (10 µg/ml) and anti-CD28 antibodies (5 µg/ml) in the presence of IL-2 with increasing concentrations of recombinant human FL. Three days later, the supernatants were collected to assess IL-10 and IFNγ production, and proliferation was determined by 3H-thymidine incorporation. Representative of 4 experiments. (B) IL-10 inhibition is dependent on the strength of TCR stimulation. T cells were activated with increasing doses of anti-CD3 as indicated, and anti-CD28 (2.5 ug/ml) in presence or absence of FL, and IL-10 and IFNγ secretion determined by ELISA. (C) IL-10 inhibition by FL in activated T cells is dependent on the presence of FLT3 expression. T cells were infected with shFLT3-3 (non-silencing) and shFLT3-4 (silencing) prior to stimulation in activated T cells (as in A) in the presence of FL. IL-10 secretion was measured by ELISA, and shown relative to T cells without FL treatment.
FLT3 is induced on CD46-induced Tr1 cells and inhibits IL-10 production
Stimulation of CD4+ T cells by CD3 and CD46 in the presence of IL-2 induces the differentiation of Tr1 cells, regulatory T cells that produce IL-10 (11). To find out whether FLT3 plays a role in the production of IL-10 in Tr1 cells, we first measured FLT3 expression on CD46-induced Tr1 cells and found that FLT3 expression was indeed induced on Tr1 cells by anti-CD3 and anti-CD46 antibodies and IL-2 (Figure 5A). When we next added FL to CD46-differentiated Tr1 cells, we found that IL-10 levels decreased while IFNγ production and proliferation did not change (Figure 5B). To assess whether the FL-FLT3 regulatory loop is present in Tr1 cells, we determined if IL-10-producing Tr1 cells could themselves secrete FL. When CD4+ T cells were stimulated with CD3 alone or with CD3/CD46 antibodies in the presence of IL-2, only the combination of CD46 and CD3 antibodies, which led to differentiation of Tr1 cells, could induce significant amounts of FL (Figure 5C). Lastly, we determined the effects of FLT3 knockdown on IL-10 production by CD46-stimulated T cells. Purified T cells were stimulated with CD3/CD46 antibodies in presence of IL-2 and infected with the efficient shRNA lentiviruses targeting FLT3 (constructs number 4 and 6), or with shRNA control. Since CD3/CD46 stimulated cells did not survive long enough for a secondary stimulation (in contrast to CD3/28 stimulated cells), we measured the level of IL-10 production 48 hrs after infection and found that FLT3 knockdown led to an increase in IL-10 secretion, while IFNγ levels did not change (Figure 5D).
Figure 5. Tr1 cells express FLT3, secrete FL, and FL inhibits their IL-10 production.
(A) CD4+ T cells were differentiated into Tr1 cells by stimulation with anti-CD3/CD46 antibodies in the presence of IL-2. Three days later, FLT3 expression was assessed by flow cytometry using an anti-FLT3-PE or irrelevant IgG1-PE control antibody. (B) CD4+ T cells were left unstimulated (Ctrl), stimulated by anti-CD3 antibodies or differentiated into Tr1 cells by stimulation with anti-CD3/CD46 antibodies in presence of IL-2 (Tr1) for 3 days, in presence or absence of FL. The production of IFNγ and IL-10 by CD46-induced Tr1 cells was then quantified by ELISA. Representative of 4 experiments (C) The concentrations of FL in the supernatants of activated T cells (as indicated) were determined by ELISA. (D) CD4+ primary human T cells were first stimulated with anti-CD3/CD46 antibodies in the presence of IL-2 for 24 hrs before infection by lentivirus encoding the two best shRNA targeting FLT3 (#4 and #6), or shRNA-GFP as a control (FACS plots shown). Twenty-four hours later, the supernatants were harvested and the levels of IL-10 and IFNγ determined by ELISA.
DISCUSSION
A large-scale lentiviral RNAi screen in primary human T cells has allowed us to uncover roles for several new genes in the control of cytokine secretion, including a previously unappreciated function for the cell surface receptor, FLT3, in regulating IL-10 production. While RNAi screens have proven to effective in elucidating gene functions in T cell lines (36, 37), our studies demonstrate the application of this technology to primary human T cells, thus allowing us to study the normal processes of T cell activation and cytokine production. Future studies can take advantage of this tool to study diverse processes in normal T cells -- such as differentiation, activation, migration or HIV infection -- as well as in abnormal T cells from patients with immune disorders. Consistent with our observation of enhanced IFNγ production in knockdown cells, PRKR (Interferon-induced, double-stranded RNA activated protein kinase) has previously been shown to inhibit IFNγ mRNA translation(38). This data provided a positive control for our screen.
Our main goal was to identify regulators of IL-10 production. IL-10 is a critical regulator of inflammation (39) and it plays an important role in human pathologies such as asthma (40) and MS (14, 32). We found that knockdown of FLT3 led to an increase in IL-10 secretion. Hence, FLT3 may act a negative regulator of IL-10 secretion. Our findings that FLT3 and FL play a role in mature T cell activation were unexpected. FLT3 was previously described a haematopoeitic growth factor, not expressed by mature human T cells (25), but expressed by thymocytes and playing a role in thymopoeisis (41). FLT3 deficiencies result in defects in multi-potent stem cells and lymphoid differentiation (27). In addition, FL has been shown to synergize with a wide variety of hematopoietic cytokines to stimulate the growth and differentiation of early hematopoietic progenitors (42). Finally, FLT3 mutations are the most frequent genetic aberrations that have been described in acute myeloid leukemia (43). Importantly, FLT3 expression was not detected on monocytes, which sometimes contaminate purified T cells (not shown), in accordance with a recent report (44). Moreover, the staining obtained with EOL-1, a leukemia cell line known to express FLT3, although stronger than on activated T cells, was also low (not shown). The expression of FLT3 upon T cell activation and the inhibitory effect of FL on IL-10 secretion were also observed using >98% pure positively selected CD4+ T cells (not shown). Our finding that FLT3 and FL are induced in activated T cells and function in a negative feedback loop to dampen IL-10 production was not previously reported. Our results, however, may help explain some observations in published studies. First, consistent with our observation that FLT3 is a repressor of IL-10 production, an increase in IL-10 levels was observed in FLT3-deficient mice with an allogeneic aorta graft (45). While this effect was attributed to dendritic cells, our results suggest an additional role for T cells. Second, administration of FL has been shown to promote tumor rejection (46, 47), by enhancing NK activity (48) and skewing the response toward a Th1 phenotype, as FL-stimulated DCs secrete high amounts of IL-12 (49). Our data suggests that FL could also play a role in rejecting tumors by reducing IL-10 levels in T cells and thus enhancing immunity.
Importantly, our data also demonstrate that the expression of FLT3 and FL is induced on Tr1 regulatory T cells that produce IL-10. IL-10 levels in CD46-induced Tr1 cells were possible to suppress by addition of FL or to enhance by silencing of FLT3, consistent with a negative feedback role for FLT3 in IL-10 regulation, perhaps acting to terminate the regulatory responses of Tr1 cells (see model presented in Figure 6). While the source of FL in our system appears to be the T cells themselves, thus forming a negative feedback loop, other sources may also be active in vivo and may act to modulate regulatory T cells in specific tissues and physiological states (34, 42). Given our previous observation that CD46-induced Tr1 cells are defective in patients with MS (14), it will now be important to test the role of the FLT3 and other IL-10 regulating mechanisms in autoimmune and inflammatory pathologies.
Figure 6. Proposed model of the regulation of IL-10 secretion by the FLT3-FL regulatory feedback loop.
Activated T cells or CD46-differentiated Tr1 cells produce IL-10, while they also upregulate FLT3 at their cell surface and produce soluble FL. The activation of FLT3 results then in a downregulation of IL-10 production.
Supplementary Material
Acknowledgements
We would like to thank Alice Pannerec and Siobhan Ni Choileain for their excellent technical skills.
Footnotes
The work was supported by NIH grants to NH (U19 AI070352) and by grants from the National Multiple Sclerosis Society and from the NIH to DAH (P01 AI045757, U19 AI046130, U19 AI070352, P01 AI039671). DAH is a Jacob Javits Merit Award (NS24247) from the National Institute of Neurological Disorders and Stroke. AA was supported by an advanced fellowship from the NMSS followed by a research grant from the MS society (UK)(859/07).
Disclosure of Conflicts of Interest
The authors have no conflicts of interest.
References
- 1.Vieira P, de Waal-Malefyt R, Dang MN, Johnson KE, Kastelein R, Fiorentino DF, deVries JE, Roncarolo MG, Mosmann TR, Moore KW. Isolation and expression of human cytokine synthesis inhibitory factor cDNA clones: homology to Epstein-Barr virus open reading frame BCRFI. Proc Natl Acad Sci U S A. 1991;88:1172–1176. doi: 10.1073/pnas.88.4.1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Groux H, O'Garra A, Bigler M, Rouleau M, Antonenko S, de Vries JE, Roncarolo MG. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature. 1997;389:737–742. doi: 10.1038/39614. [DOI] [PubMed] [Google Scholar]
- 3.Kuhn R, Lohler J, Rennick D, Rajewsky K, Muller W. Interleukin-10-deficient mice develop chronic enterocolitis. Cell. 1993;75:263–274. doi: 10.1016/0092-8674(93)80068-p. [DOI] [PubMed] [Google Scholar]
- 4.Battaglia M, Stabilini A, Draghici E, Migliavacca B, Gregori S, Bonifacio E, Roncarolo MG. Induction of Tolerance in Type 1 Diabetes via Both CD4+CD25+ T Regulatory Cells and T Regulatory Type 1 Cells. Diabetes. 2006;55:1571–1580. doi: 10.2337/db05-1576. [DOI] [PubMed] [Google Scholar]
- 5.Pennline KJ, Roque-Gaffney E, Monahan M. Recombinant human IL-10 prevents the onset of diabetes in the nonobese diabetic mouse. Clin Immunol Immunopathol. 1994;71:169–175. doi: 10.1006/clin.1994.1068. [DOI] [PubMed] [Google Scholar]
- 6.Awasthi A, Carrier Y, Peron JP, Bettelli E, Kamanaka M, Flavell RA, Kuchroo VK, Oukka M, Weiner HL. A dominant function for interleukin 27 in generating interleukin 10-producing anti-inflammatory T cells. Nat Immunol. 2007;8:1380–1389. doi: 10.1038/ni1541. [DOI] [PubMed] [Google Scholar]
- 7.Fitzgerald DC, Zhang GX, El-Behi M, Fonseca-Kelly Z, Li H, Yu S, Saris CJ, Gran B, Ciric B, Rostami A. Suppression of autoimmune inflammation of the central nervous system by interleukin 10 secreted by interleukin 27-stimulated T cells. Nat Immunol. 2007;8:1372–1379. doi: 10.1038/ni1540. [DOI] [PubMed] [Google Scholar]
- 8.Stumhofer JS, Silver JS, Laurence A, Porrett PM, Harris TH, Turka LA, Ernst M, Saris CJ, O’Shea JJ, Hunter CA. Interleukins 27 and 6 induce STAT3-mediated T cell production of interleukin 10. Nat Immunol. 2007;8:1363–1371. doi: 10.1038/ni1537. [DOI] [PubMed] [Google Scholar]
- 9.McGeachy MJ, Bak-Jensen KS, Chen Y, Tato CM, Blumenschein W, McClanahan T, Cua DJ. TGF-beta and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain T(H)-17 cell-mediated pathology. Nat Immunol. 2007;8:1390–1397. doi: 10.1038/ni1539. [DOI] [PubMed] [Google Scholar]
- 10.Barrat FJ, Cua DJ, Boonstra A, Richards DF, Crain C, Savelkoul HF, de Waal-Malefyt R, Coffman RL, Hawrylowicz CM, O'Garra A. In vitro generation of interleukin 10-producing regulatory CD4(+) T cells is induced by immunosuppressive drugs and inhibited by T helper type 1 (Th1)- and Th2-inducing cytokines. J Exp Med. 2002;195:603–616. doi: 10.1084/jem.20011629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kemper C, Chan AC, Green JM, Brett KA, Murphy KM, Atkinson JP. Activation of human CD4(+) cells with CD3 and CD46 induces a T-regulatory cell 1 phenotype. Nature. 2003;421:388–392. doi: 10.1038/nature01315. [DOI] [PubMed] [Google Scholar]
- 12.Astier A, Trescol-Biemont MC, Azocar O, Lamouille B, Rabourdin-Combe C. Cutting edge: CD46, a new costimulatory molecule for T cells, that induces p120CBL and LAT phosphorylation. J Immunol. 2000;164:6091–6095. doi: 10.4049/jimmunol.164.12.6091. [DOI] [PubMed] [Google Scholar]
- 13.Spach KM, Nashold FE, Dittel BN, Hayes CE. IL-10 signaling is essential for 1,25-dihydroxyvitamin D3-mediated inhibition of experimental autoimmune encephalomyelitis. J Immunol. 2006;177:6030–6037. doi: 10.4049/jimmunol.177.9.6030. [DOI] [PubMed] [Google Scholar]
- 14.Astier AL, Meiffren G, Freeman S, Hafler DA. Alterations in CD46-mediated Tr1 regulatory T cells in patients with multiple sclerosis. J Clin Invest. 2006;116:3252–3257. doi: 10.1172/JCI29251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Astier AL, Hafler DA. Abnormal Tr1 differentiation in multiple sclerosis. J Neuroimmunol. 2007;191:70–78. doi: 10.1016/j.jneuroim.2007.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma A, Xiong Z, Hu Y, Qi S, Song L, Dun H, Zhang L, Lou D, Yang P, Zhao Z, Wang X, Zhang D, Daloze P, Chen H. Dysfunction of IL-10-producing type 1 regulatory T cells and CD4+CD25+ regulatory T cells in a mimic model of human multiple sclerosis in Cynomolgus monkeys. International Immunopharmacology. 2009;9:599–608. doi: 10.1016/j.intimp.2009.01.034. [DOI] [PubMed] [Google Scholar]
- 17.Martinez-Forero I, Garcia-Munoz R, Martinez-Pasamar S, Inoges S, Lopez-Diaz de Cerio A, Palacios R, Sepulcre J, Moreno B, Gonzalez Z, Fernandez-Diez B, Melero I, Bendandi M, Villoslada P. IL-10 suppressor activity and ex vivo Tr1 cell function are impaired in multiple sclerosis. Eur J Immunol. 2008;38:576–586. doi: 10.1002/eji.200737271. [DOI] [PubMed] [Google Scholar]
- 18.Xystrakis E, Kusumakar S, Boswell S, Peek E, Urry Z, Richards DF, Adikibi T, Pridgeon C, Dallman M, Loke TK, Robinson DS, Barrat FJ, O'Garra A, Lavender P, Lee TH, Corrigan C, Hawrylowicz CM. Reversing the defective induction of IL-10-secreting regulatory T cells in glucocorticoid-resistant asthma patients. J Clin Invest. 2006;116:146–155. doi: 10.1172/JCI21759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xystrakis E, Urry Z, Hawrylowicz CM. Regulatory T cell therapy as individualized medicine for asthma and allergy. Curr Opin Allergy Clin Immunol. 2007;7:535–541. doi: 10.1097/ACI.0b013e3282f14d7c. [DOI] [PubMed] [Google Scholar]
- 20.Chang K, Elledge SJ, Hannon GJ. Lessons from Nature: microRNA-based shRNA libraries. Nat Methods. 2006;3:707–714. doi: 10.1038/nmeth923. [DOI] [PubMed] [Google Scholar]
- 21.Downward J. RNA interference libraries prove their worth in hunt for tumor suppressor genes. Cell. 2005;121:813–815. doi: 10.1016/j.cell.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Fraser A. RNA interference: human genes hit the big screen. Nature. 2004;428:375–378. doi: 10.1038/428375a. [DOI] [PubMed] [Google Scholar]
- 23.Ullrich A, Schlessinger J. Signal transduction by receptors with tyrosine kinase activity. Cell. 1990;61:203–212. doi: 10.1016/0092-8674(90)90801-k. [DOI] [PubMed] [Google Scholar]
- 24.Rosnet O, Marchetto S, deLapeyriere O, Birnbaum D. Murine Flt3, a gene encoding a novel tyrosine kinase receptor of the PDGFR/CSF1R family. Oncogene. 1991;6:1641–1650. [PubMed] [Google Scholar]
- 25.Rosnet O, Schiff C, Pebusque MJ, Marchetto S, Tonnelle C, Toiron Y, Birg F, Birnbaum D. Human FLT3/FLK2 gene: cDNA cloning and expression in hematopoietic cells. Blood. 1993;82:1110–1119. [PubMed] [Google Scholar]
- 26.Small D, Levenstein M, Kim E, Carow C, Amin S, Rockwell P, Witte L, Burrow C, Ratajczak MZ, Gewirtz AM, et al. STK-1, the human homolog of Flk-2/Flt-3, is selectively expressed in CD34+ human bone marrow cells and is involved in the proliferation of early progenitor/stem cells. Proc Natl Acad Sci U S A. 1994;91:459–463. doi: 10.1073/pnas.91.2.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mackarehtschian K, Hardin JD, Moore KA, Boast S, Goff SP, Lemischka IR. Targeted disruption of the flk2/flt3 gene leads to deficiencies in primitive hematopoietic progenitors. Immunity. 1995;3:147–161. doi: 10.1016/1074-7613(95)90167-1. [DOI] [PubMed] [Google Scholar]
- 28.Moffat J, Grueneberg DA, Yang X, Kim SY, Kloepfer AM, Hinkle G, Piqani B, Eisenhaure TM, Luo B, Grenier JK, Carpenter AE, Foo SY, Stewart SA, Stockwell BR, Hacohen N, Hahn WC, Lander ES, Sabatini DM, Root DE. A lentiviral RNAi library for human and mouse genes applied to an arrayed viral high-content screen. Cell. 2006;124:1283–1298. doi: 10.1016/j.cell.2006.01.040. [DOI] [PubMed] [Google Scholar]
- 29.Amado RG, Chen IS. Lentiviral vectors--the promise of gene therapy within reach? Science. 1999;285:674–676. doi: 10.1126/science.285.5428.674. [DOI] [PubMed] [Google Scholar]
- 30.Ostrowski MA, Chun TW, Justement SJ, Motola I, Spinelli MA, Adelsberger J, Ehler LA, Mizell SB, Hallahan CW, Fauci AS. Both memory and CD45RA+/CD62L+ naive CD4(+) T cells are infected in human immunodeficiency virus type 1-infected individuals. J Virol. 1999;73:6430–6435. doi: 10.1128/jvi.73.8.6430-6435.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meinl E, Lengenfelder D, Blank N, Pirzer R, Barata L, Hivroz C. Differential requirement of ZAP-70 for CD2-mediated activation pathways of mature human T cells. J Immunol. 2000;165:3578–3583. doi: 10.4049/jimmunol.165.7.3578. [DOI] [PubMed] [Google Scholar]
- 32.Krakauer M, Sorensen P, Khademi M, Olsson T, Sellebjerg F. Increased IL-10 mRNA and IL-23 mRNA expression in multiple sclerosis: interferon-beta treatment increases IL-10 mRNA expression while reducing IL-23 mRNA expression. Mult Scler. 2008;14:622–630. doi: 10.1177/1352458507087136. [DOI] [PubMed] [Google Scholar]
- 33.Lyman SD, James L, Johnson L, Brasel K, de Vries P, Escobar SS, Downey H, Splett RR, Beckmann MP, McKenna HJ. Cloning of the human homologue of the murine flt3 ligand: a growth factor for early hematopoietic progenitor cells. Blood. 1994;83:2795–2801. [PubMed] [Google Scholar]
- 34.McClanahan T, Culpepper J, Campbell D, Wagner J, Franz-Bacon K, Mattson J, Tsai S, Luh J, Guimaraes MJ, Mattei MG, Rosnet O, Birnbaum D, Hannum CH. Biochemical and genetic characterization of multiple splice variants of the Flt3 ligand. Blood. 1996;88:3371–3382. [PubMed] [Google Scholar]
- 35.Lyman SD, James L, Vanden Bos T, de Vries P, Brasel K, Gliniak B, Hollingsworth LT, Picha KS, McKenna HJ, Splett RR, et al. Molecular cloning of a ligand for the flt3/flk-2 tyrosine kinase receptor: a proliferative factor for primitive hematopoietic cells. Cell. 1993;75:1157–1167. doi: 10.1016/0092-8674(93)90325-k. [DOI] [PubMed] [Google Scholar]
- 36.Willingham AT, Orth AP, Batalov S, Peters EC, Wen BG, Aza-Blanc P, Hogenesch JB, Schultz PG. A strategy for probing the function of noncoding RNAs finds a repressor of NFAT. Science. 2005;309:1570–1573. doi: 10.1126/science.1115901. [DOI] [PubMed] [Google Scholar]
- 37.Oberdoerffer S, Moita LF, Neems D, Freitas RP, Hacohen N, Rao A. Regulation of CD45 alternative splicing by heterogeneous ribonucleoprotein, hnRNPLL. Science. 2008;321:686–691. doi: 10.1126/science.1157610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ben-Asouli Y, Banai Y, Pel-Or Y, Shir A, Kaempfer R. Human interferon-gamma mRNA autoregulates its translation through a pseudoknot that activates the interferon-inducible protein kinase PKR. Cell. 2002;108:221–232. doi: 10.1016/s0092-8674(02)00616-5. [DOI] [PubMed] [Google Scholar]
- 39.O'Garra A, Barrat FJ, Castro AG, Vicari A, Hawrylowicz C. Strategies for use of IL-10 or its antagonists in human disease. Immunol Rev. 2008;223:114–131. doi: 10.1111/j.1600-065X.2008.00635.x. [DOI] [PubMed] [Google Scholar]
- 40.Hawrylowicz CM. Regulatory T cells and IL-10 in allergic inflammation. J Exp Med. 2005;202:1459–1463. doi: 10.1084/jem.20052211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kenins L, Gill JW, Boyd RL, Hollander GA, Wodnar-Filipowicz A. Intrathymic expression of Flt3 ligand enhances thymic recovery after irradiation. J Exp Med. 2008;205:523–531. doi: 10.1084/jem.20072065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lyman SD. Biology of flt3 ligand and receptor. Int J Hematol. 1995;62:63–73. doi: 10.1016/0925-5710(95)00389-a. [DOI] [PubMed] [Google Scholar]
- 43.Kelly LM, Liu Q, Kutok JL, Williams IR, Boulton CL, Gilliland DG. FLT3 internal tandem duplication mutations associated with human acute myeloid leukemias induce myeloproliferative disease in a murine bone marrow transplant model. Blood. 2002;99:310–318. doi: 10.1182/blood.v99.1.310. [DOI] [PubMed] [Google Scholar]
- 44.Matsumura N, Mandai M, Hamanishi J, Yamaguchi K, Fukuhara K, Yagi H, Higuchi T, Takakura K, Fujii S. Immunostimulatory effect of Fms-like tyrosine kinase 3 ligand on peripheral monocyte-derived dendritic cells and natural killer cells: utilization for ovarian cancer treatment. Oncol Rep. 2008;19:505–515. [PubMed] [Google Scholar]
- 45.Wang Z, Taner T, Morelli AE, Thomson AW. Hosts lacking fms-like tyrosine kinase 3 ligand exhibit marked reductions in transplant vascular sclerosis. Transplantation. 2005;79:869–875. doi: 10.1097/01.tp.0000157120.43052.3a. [DOI] [PubMed] [Google Scholar]
- 46.Esche C, Subbotin VM, Maliszewski C, Lotze MT, Shurin MR. FLT3 ligand administration inhibits tumor growth in murine melanoma and lymphoma. Cancer Res. 1998;58:380–383. [PubMed] [Google Scholar]
- 47.Lynch DH, Andreasen A, Maraskovsky E, Whitmore J, Miller RE, Schuh JC. Flt3 ligand induces tumor regression and antitumor immune responses in vivo. Nat Med. 1997;3:625–631. doi: 10.1038/nm0697-625. [DOI] [PubMed] [Google Scholar]
- 48.Braun SE, Chen K, Blazar BR, Orchard PJ, Sledge G, Robertson MJ, Broxmeyer HE, Cornetta K. Flt3 ligand antitumor activity in a murine breast cancer model: a comparison with granulocyte-macrophage colony-stimulating factor and a potential mechanism of action. Hum Gene Ther. 1999;10:2141–2151. doi: 10.1089/10430349950017130. [DOI] [PubMed] [Google Scholar]
- 49.Parajuli P, Mosley RL, Pisarev V, Chavez J, Ulrich A, Varney M, Singh RK, Talmadge JE. Flt3 ligand and granulocyte-macrophage colony-stimulating factor preferentially expand and stimulate different dendritic and T-cell subsets. Exp Hematol. 2001;29:1185–1193. doi: 10.1016/s0301-472x(01)00722-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.