Abstract
OBJECTIVE
To estimate leiomyoma-related inpatient care in the United States for 2007 with predictions for the ensuing 40 years.
STUDY DESIGN
We used the 2007 Nationwide Inpatient Sample to estimate hospitalizations and inpatient surgeries for uterine leiomyoma in US women 15 to 54 years. We used the US Census Bureau population projections to predict leiomyoma-related inpatient care through 2050.
RESULTS
In 2007, 355,135 women were hospitalized for leiomyoma (rate = 42 per 10,000 women-years). Black women had increased rates of hospitalization, hysterectomy, and myomectomy (relative risk, 3.5, 2.4, 6.8, respectively) compared with white women. Leiomyoma-related hospitalizations are predicted to increase 23% (to 437,874) between 2007 and 2050, with 20% and 31% increases in leiomyoma-related hysterectomies and myomectomies.
CONCLUSION
Leiomyoma-related inpatient care and major surgery remains substantial despite advances in less invasive treatment options. Given population growth, the projected burden of leiomyoma-related inpatient care will increase significantly by 2050, differentially impacting black vs white women.
Keywords: fibroids, health care costs, health disparities, hysterectomy, leiomyoma, myomectomy
Uterine leiomyoma, (fibroids) and their treatment are arguably the most significant women’s health issue facing reproductive-aged women in the United States today. Leiomyoma are the most common reproductive tumor in women. By age 50, cumulative incidence of ultrasound-detected fibroids for white women is almost 70% and more than 80% for black women; moreover, for women in their thirties and forties with ultrasound-detected leiomyoma, up to 35% of white and 50% of black women will have symptoms. 1 Leiomyoma-related symptoms are associated with a dramatically decreased quality of life and health.2Common symptoms from leiomyoma are heavy, painful menstrual bleeding, often leading to anemia, and “bulk” symptoms such as pelvic pressure and urinary frequency. Women with leiomyoma are more likely to miss work3 and to experience certain pregnancy complications.4
Women with leiomyoma incur total health care costs over twice that of their counterparts without leiomyoma and the majority of costs come from inpatient care.3,5 Absenteeism and disability from fibroids results in indirect costs equivalent to direct healthcare costs.6 Though not all women seek treatment for their symptoms, leiomyoma are the primary indication for hysterectomy in this country, accounting for 33% to more than 40% of the approximately 600,000 hysterectomies each year.7,8 Hysterectomy for leiomyoma exceeds the number of hysterectomies performed for all types of gynecologic cancers combined.8 Minimally invasive treatments, such as uterine artery embolization (UAE) and magnetic resonance guided focused ultrasound surgery (MRgFUS), are available but underused, and most leiomyoma treatment still involves an inpatient hospital stay with its associated disadvantages, including cost.
Age and race are the 2 major determinants of fibroid burden. Premenopausal women, generally between ages 35 and 45, are the most affected group. Although white, Asian, and Hispanic women are currently thought to have similar incidence of leiomyoma, black women bear a disproportionate burden from fibroids.9,10
As a pressing women’s health issue, uterine leiomyoma and their treatment patterns demand informed planning as we navigate the current health care environment. Our first objective in this study was to update the data describing current leiomyoma-related hospitalizations and surgery. To reflect the growing US population and projected racial distribution changes, we also created predicted scenarios for the coming decades. These predictions are illustrations of the future public health burden of fibroid care, intended to guide researchers, policymakers, and healthcare agencies. These predictions will also equip training programs to calculate the number of graduates needed to meet the demands for well-trained gynecologic surgeons and women’s health care providers.11
Materials AND Methods
Data source
We used the 2007 data from the Nationwide Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project (HCUP) to calculate the number of hospitalization, hysterectomy, and myomectomy for US women aged 15 to 54 with a diagnosis of uterine leiomyoma.12 The NIS is the largest US inpatient database, containing information on 7 million hospital discharges from 800 to 1000 hospitals, representing all payers. The data (patient characteristics, diagnoses, surgeries) approximate a 20% stratified sample of US community hospitals and is retained for all discharges for each hospital for the year, capturing all hospital stays with an inpatient designation. Women with uterine leiomyoma as any of their hospital diagnoses, based on the International Classification of Diseases, 9th revision, (ICD-9) Clinical Modification (codes 218.0, 218.1, 218.2, 218.9), were included. Procedures were identified using ICD-9 procedure codes: for hysterectomy (68.3–68.9) and for myomectomy (68.29 and 68.19). Reporting of data on race is not required in the NIS and varies by state and hospital. However, given the importance of race in the study of fibroids, we examined and analyzed available race data for black and white women.
Analysis
We calculated the 2007 age-specific rates of leiomyoma-related hospitalization, hysterectomy, and myomectomy (events) for women aged 15–54 using the US Census Bureau 2007 population data.13 These rates were estimated individually for each 5-year age group regardless of race and then stratified for race. For example, to calculate an age and race-specific rate, we took the NIS data for the number of leiomyoma-related hospitalizations in white women, aged 40–44, and divided it by the total number of white women, aged 40–44, in the United States in 2007 as reported by the US Census. We multiplied these rates by the US Census Bureau population projections for 2010 to 2050 for each 5-year age group individually, then summed these numbers to report results by the decade (2010, 2020).14,15 These values yield age and race-specific predictions for the magnitude of future leiomyoma-related inpatient care. We used the middle series of the US Census Bureau population projections for each year and applied the 95% CI around the 2007 rates to calculate a range of leiomyoma-related events predicted for each decade.
Given the complex sampling design of the NIS, we used STATA 9.2 (StataCorp, College Station, TX) to account for sampling weights, strata, and clusters and to provide national estimates. Rate calculations and projections were performed using Microsoft Excel (Microsoft, Redmond, WA). The NIS contains only de-identified data and thus, this study was granted exemption status by the Mayo Clinic Institutional Review Board (Jacksonville, FL).
Results
In 2007, there were 355,137 leiomyoma-related hospitalizations in women aged 15–54 for a rate of 42 per 10,000 women years (95% confidence interval [CI], 39–46). There were 538,719 hysterectomies, of which 43% had a diagnosis of leiomyoma. Although nearly one-third (101,616) of women in the NIS had missing race data, 77,001 black women and 120,688 white women allowed us to examine racial differences in this subset. For black women, the calculated rate of hospitalization was 3.5 times that in white women. For all races, combined, leiomyoma-related hysterectomy was 27 per 10,000 women-years (95% CI, 25–30), and 2.4 times more common in black women than in white women. Myomectomy rate was 4.4 per 10,000 women-years (95% CI, 3.7–5.2). According to available data, black women had 6.8 times the rate f myomectomy compared with white women (Table 1).
TABLE 1.
Rates of leiomyoma-related hospitalization, hysterectomy, and myomectomy in 2007, in women 15–54 years old, including all races, black and white
| Event | All races | Black | White |
|---|---|---|---|
| Hospitalization | |||
| Rate | 42 | 65 | 18 |
| 95% CI | 39–46 | 54–75 | 16–20 |
| Hysterectomy | |||
| Rate | 27 | 33 | 14 |
| 95% CI | 25–30 | 28–38 | 12–15 |
| Myomectomy | |||
| Rate | 4.4 | 9.2 | 1.3 |
| 95% CI | 3.7–5.2 | 6.9–11 | 1.0–1.6 |
Rate per 10,000 women-years.
CI, confidence interval.
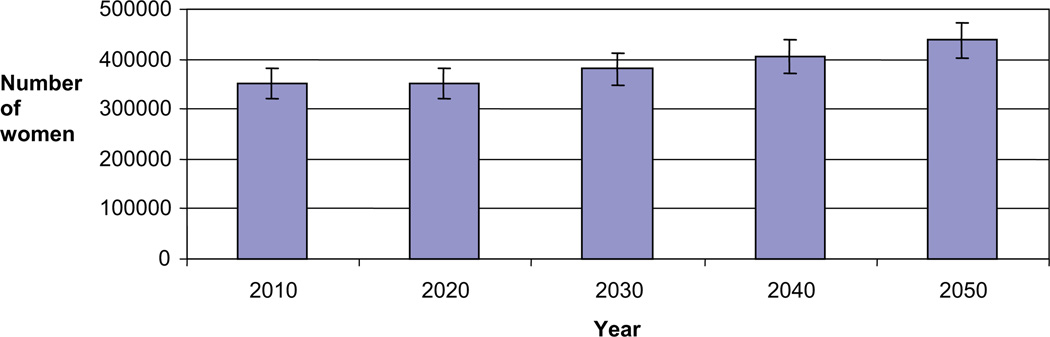
Assuming stable rates of these leiomyoma-related events, compared 2007 data, the number of hospitalizations should increase 23%( to 437,873) by 2050 because of an increase in the female US population and changing demographics.16 The number of leiomyoma-related inpatient hysterectomies is predicted to increase by 20%, with an increase of 22% in black women and 8% in white women as compared with 2007 numbers. Inpatient myomectomies are predicted to increase in number by 31%, to nearly 50,000, in 2050, with a 26% increase in black women and a 21% increase in white women compared with these figures in 2007 (Figure and Table 2).
FIGURE.
Projections for leiomyoma-related hospitalizations, 2010–2050, all races
TABLE 2.
Projected numbers of women with leiomyoma-related hospitalization, hysterectomy, and myomectomy in 2010–2050, in women 15–54 years old, including all races
| Event | 2010 | 2020 | 2030 | 2040 | 2050 |
|---|---|---|---|---|---|
| Hospitalization | |||||
| Number of women | 351,554 | 350,943 | 380,203 | 406,318 | 437,874 |
| 95% CI | (322,354–380,754) | (321,474–380,412) | (348,368–412,037) | (372,279–440,355) | (401,123–474,624) |
| Hysterectomy | |||||
| Number of women | 228,939 | 222,800 | 243,127 | 259,485 | 278,419 |
| 95% CI | (211,288–194,199) | (205,578–181,747) | (224,353–194,452) | (239,438–204,284) | (256,904–216,981) |
| Myomectomy | |||||
| Number of women | 37,134 | 39,461 | 42,211 | 45,032 | 49,154 |
| 95% CI | (30,751–43,515) | (32,675–46,246) | (34,951–49,471) | (37,289–52,774) | (40,700–57,607) |
Hospitalization for fibroids differed by age and peaked in women 40–44 and 45–49 years old (85 and 86 per 10,000). The same trend is seen for hysterectomy (62 and 71 per 10,000), accounting for more than 150,000 hysterectomies in 2007 in this age group alone. Myomectomy was most common in 30–34 and 35–39 year-olds (8.9 and 11 per 10,000) (Table 3).
TABLE 3.
Rates of leiomyoma-related hospitalization, hysterectomy, myomectomy in 2007, in women 15–54 years old
| All races | Age groups in years | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Event | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 15–54 |
| Hospitalization | 0.30 | 2.8 | 13 | 35 | 61 | 85 | 86 | 45 | 42 |
| Hysterectomy | 0.00 | 0.09 | 1.6 | 9.0 | 30 | 62 | 71 | 37 | 27 |
| Myomectomy | 0.05 | 0.62 | 3.4 | 8.9 | 11 | 7.5 | 2.9 | 0.99 | 4.4 |
| Black | |||||||||
| Hospitalization | 0.58 | 6.3 | 25 | 66 | 111 | 140 | 122 | 57 | 65 |
| Hysterectomy | 0.00 | 0.07 | 2.5 | 14 | 48 | 85 | 83 | 37 | 33 |
| Myomectomy | 0.00 | 1.4 | 6.8 | 18 | 25 | 16 | 5.5 | 1.2 | 9.2 |
| White | |||||||||
| Hospitalization | 0.07 | 0.75 | 3.8 | 12 | 22 | 36 | 41 | 24 | 18 |
| Hysterectomy | 0.01 | 0.07 | 0.74 | 3.8 | 12 | 29 | 36 | 21 | 14 |
| Myomectomy | 0.02 | 0.14 | 0.90 | 2.5 | 3.2 | 2.3 | 1.2 | 0.51 | 1.3 |
Rate per 10,000 women-years
Comment
Leiomyoma-related inpatient care is substantial and predicted to increase significantly by 2050. Approximately 42 per 10,000 women, aged 15–54, are hospitalized annually for leiomyoma-related treatments. Major surgery, including hysterectomy and myomectomy, occurs in the majority of these hospitalizations. Such leiomyoma-related health care events appear, from this data, to occur much more often in black women than in white women. Given the increasing population and the projected increasing diversity and changing demographics of the US population16 the absolute magnitude of this common female health problem will increase 20 to more than 30% by the year 2050. If current trends continue, there will be more than 400,000 leiomyoma-related hospitalizations in 2050 with the associated morbidity and cost. Because indirect costs (disability and absenteeism) are a significant proportion of the health care costs for leiomyoma, these trends could also have substantial implications for workforce productivity.3,6
Uterine leiomyoma have a differential impact for black women for several reasons. 1 Incidence rates for black women are 2- to 3-fold higher than for white women.9,17 Black women, as compared with white women, are more likely to be hospitalized and to have a hysterectomy for fibroids; they are much more likely to have a myomectomy. They are also more likely to have a more severe disease at the time of presentation and the time of surgery as well as a higher prevalence and relative risk of fibroids.9,18–20 Finally, leiomyomas affect black women over a wider age span with an earlier age of onset and no growth deceleration as women approach menopause.18,21 These factors magnify the importance of the changes anticipated by this study.
Our results point toward an increasing financial burden related to leiomyoma-related inpatient care for our country’s future. Health care costs related to leiomyoma are already high; costs for total health care and for inpatient care in women with fibroids are 2.6 times and 6.6 times those for women without fibroids. 3 Inpatient stays, generally 2–3 days for leiomyoma care, represent a large part of treatment costs.6,22 Inpatient myomectomy costs $5425–11,839 and inpatient hysterectomy costs $5012–7934 in 2004 dollars.23 Using data from 1999–2004, leiomyoma-related direct (medical) and indirect (productivity) costs for women 25–54 with symptomatic leiomyoma were examined: direct 12-month costs were $11,720 for women with leiomyoma, compared with $3257 for women without such leiomyoma, and indirect health-related costs over a year were an additional $11,752 compared with $8083 for controls (P < .0001).6 Other costs (pregnancy complications, infertility, urinary symptoms) are not easily represented or measured, but are substantial.3 Furthermore, myomectomy and other uterine-sparing treatments are likely to increase as more women delay childbearing or opt for minimally invasive procedures such as uterine artery embolization. These treatments are not infrequently followed by additional medical symptom management, UAE, repeat myomectomy, and hysterectomy, compounding the overall per-person cost for fibroid-related care.
Conclusions from this study must be evaluated within the context of its limitations. One limitation is the number of necessary assumptions. We assume that the rates of hospitalizations, hysterectomies, and myomectomies going forward will remain similar to 2007 rates. This assumption is supported by Whiteman et al,24 using NIS data to demonstrate no significant change in leiomyoma-related hospitalizations over 7 years to 2005. Given the importance of racial difference in the impact of uterine leiomyoma, we chose to analyze and report difference by black and white race, despite awareness that race data in the NIS is incomplete. Our calculations are valid only under the assumption that black and white race categories are equally likely to have missing data. We intend the race data and predictions from this data only to stimulate discussion and further research in this arena; yet our findings are not incongruous with known increased prevalence and fibroid burden born by black women but also previous research suggesting that black women are more likely to undergo major surgery for fibroids.17,25 Age differences in this data are presented without complex analysis to identify statistical differences among age and race categories. Though rates of events differed somewhat by age, age standardization in similar studies did not make a significant difference to overall rates.7 The NIS uses only ICD-9 codes, and the ICD-9 codes available to identify myomectomy are nonspecific and may miss some procedures or include nonspecific uterine surgery not myomectomy. The data were also searched by using ICD-9 codes 68.29 with 69.19, resulting in minimal change in estimates of myomectomy numbers and rates. Also, the ICD-9 codes we used to identify hysterectomy may include surgeries performed for gynecologic cancer with leiomyoma as a secondary finding.
Our calculated rates likely underestimate total leiomyoma-related health care delivery for a number of reasons. The NIS does not capture treatments associated with admission not designated as inpatient. This would exclude from the NIS data most minimally invasive fibroid treatments: laparoscopic, robotic, and many vaginal hysterectomies, nearly all hysteroscopic myomectomies, and most UAE, not to mention MRgFUS. Also important is that estimates of hysterectomy rates, including ours, do not routinely correct for the number of women in the population who have already had hysterectomies and are therefore no longer “at risk” for the outcome (ie, they should not be in the denominator for calculating rate), making the estimated rates artificially lower than actuality.26
A major strength of this study is that the 2007 Nationwide Inpatient Sample is a reliable and recent source, and in fact, the best available data on leiomyoma-related US hospitalizations, hysterectomies, and myomectomies. US Census Bureau predictions for future population size and demographics are readily available. The combination of these data sources represents a new application of a proven strategy to illustrate the predicted current and future impact of leiomyoma-related inpatient care, a critically important women’s health issue.27 Our conclusions are supported by similar analyses in the literature, though reported rates of inpatient leiomyoma care are lower if inclusion is limited to leiomyoma only as the principal diagnosis. Though arguably less specific, we include all patients with diagnoses of leiomyoma to include those patients whose principal diagnosis may have leiomyoma as the underlying disease process (eg, abnormal uterine bleeding).
Symptomatic uterine leiomyoma are a critical issue in women’s health. Common and with an often devastating impact on quality of life, leiomyoma are also a primary source of resource consumption. Inpatient care and major surgery for uterine leiomyoma remains substantial despite advances in less-invasive treatment options. Assuming stable rates of hospitalization and surgery, this study also illustrates the magnitude of leiomyoma-related hospitalizations and inpatient procedures as predicted to occur in the next 4 decades. Unless fibroid incidence decreases or outpatient, minimally invasive treatments become more accessible, effective, and used, the burden of leiomyoma-related health care will increase with the increasing population and changing demographics as we move toward 2050. These projections differentially impact black vs white women and may serve as a tangible tool to inform surgeon availability, healthcare distribution policies, and research fund allocation for the management of uterine leiomyoma.
For future direction, it will be important to look at the upcoming years’ NIS data to identify changes in the rates of inpatient leiomyoma-related care, particularly as there have been large advances and more popular acceptance of minimally invasive treatment of fibroids (eg, robotic surgery, UAE), allowing more outpatient and short-stay treatments. Such changes will hopefully reduce inpatient care of uterine leiomyoma and alter the course of the health care demands projected in this study. In addition, there is a growing body of recent literature that examines cost and compares treatment modalities using validated outcomes (eg, quality of life); such studies are providing the data that will allow a more analytical approach to leiomyoma treatment, mindful of economic and health benefits on both an individual patient and population basis. Perhaps most importantly, our projections in this study mandate a commitment to research in uterine leiomyoma, focused on cause, prevention, medical treatment, and racial disparities, as a high-yield target for dramatically improving the future of women’s health.
Acknowledgments
Supported in part by Grant nos. K12HD043446 (J.M.W.) and RC1HD063312 and R01HD060503 (E.A.S.), Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health.
Footnotes
The authors report no conflicts of interest.
Presented at the 37th Annual Society of Gynecologic Surgeons Scientific Meeting, San Antonio, TX, April 11-13, 2011.
REFERENCES
- 1.Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–107. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 2.Spies JB, Bradley LD, Guido R, Maxwell GL, Levine BA, Coyne K. Outcomes from leiomyoma therapies: comparison with normal controls. Obstet Gynecol. 2010;116:641–652. doi: 10.1097/AOG.0b013e3181ed36b3. [DOI] [PubMed] [Google Scholar]
- 3.Hartmann KE, Birnbaum H, Ben-Hamadi R, et al. Annual costs associated with diagnosis of uterine leiomyomata. Obstet Gynecol. 2006;108:930–937. doi: 10.1097/01.AOG.0000234651.41000.58. [DOI] [PubMed] [Google Scholar]
- 4.Klatsky PC, Tran ND, Caughey AB, Fujimoto VY. Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. Am J Obstet Gynecol. 2008;198:357–366. doi: 10.1016/j.ajog.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 5.Flynn M, Jamison M, Datta S, Myers E. Health care resource use for uterine fibroid tumors in the United States. Am J Obstet Gynecol. 2006;195:955–964. doi: 10.1016/j.ajog.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 6.Lee DW, Ozminkowski RJ, Carls GS, Wang S, Gibson TB, Stewart EA. The direct and indirect cost burden of clinically significant and symptomatic uterine fibroids. J Occup Environ Med. 2007;49:493–506. doi: 10.1097/JOM.0b013e31805f6cf2. [DOI] [PubMed] [Google Scholar]
- 7.Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000–2004. Am J Obstet Gynecol. 2008;198:34.e1-7. doi: 10.1016/j.ajog.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 8.Keshavarz H, Hillis SD, Kieke Ba, Marchbanks PA. Hysterectomy surveillance—United States, 1994–1999. MMWR CDC Surveill Summ. 2002;51:1–8. [PubMed] [Google Scholar]
- 9.Marshall LM, Spiegelman D, Barbieri RL, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997;90:967–973. doi: 10.1016/s0029-7844(97)00534-6. [DOI] [PubMed] [Google Scholar]
- 10.Wise LA, Palmer JR, Stewart EA, Rosenberg L. Age-specific incidence rates for self-reported uterine leiomyomata in the Black Women’s Health Study. Obstet Gynecol. 2005;105:563–568. doi: 10.1097/01.AOG.0000154161.03418.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wallace AH, Havrilesky LJ, Valea FA, Barnett JC, Berchuck A, Myers ER. Projecting the need for gynecologic oncologists for the next 40 years. Obstet Gynecol. 2010;116:1366–1372. doi: 10.1097/AOG.0b013e3181fc3a22. [DOI] [PubMed] [Google Scholar]
- 12.HCUP Nationwide Inpatient Sample (NIS) [Accessed July 18, 2009];Agency for Healthcare Research and Quality. 2007 Available at: www.hcup-us.ahrq.gov/nisoverview.jsp.
- 13.Annual estimates of the population by sex and five-year age groups for the United States: April 1, 2000 to July 1, 2007 (NC-EST2007-01) U.S. Census Bureau; 2008. [Accessed July 1, 2010]. Available at: http://www.census.gov/popest/national/asrh/NCEST2007-sa.html. [Google Scholar]
- 14. [Accessed July 1, 2010];NP2008_D1: Projected population by single year of age, sex, race, and Hispanic origin for the United States: July 1, 2000 to July 1, 2050. 2008 Aug 14; Available at: http://www.census.gov/population/www/projections/files/nation/download/NP2008_D1.xls.
- 15.Methodology and Assumptions for the Population Projections of the United States: 1999 to 2100. Population Division, Bureau of the Census, U.S. Department of Commerce; 2000. [Accessed July 1, 2010]. Available at: http://www.census.gov/population/www/documentation/twps0038/twps-0038.html. [Google Scholar]
- 16.Day JC. Population projections of the united states by age, sex, race, and Hispanic origin: 1995 to 2050. Washington, DC: U.S. Bureau of the Census; 1996. [Google Scholar]
- 17.Templeman C, Marshall SF, Clarke CA, et al. Risk factors for surgically removed fibroids in a large cohort of teachers. Fertil Steril. 2009;92:1436–1446. doi: 10.1016/j.fertnstert.2008.08.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huyck KL, Panhuysen CI, Cuenco KT, et al. The impact of race as a risk factor for symptom severity and age at diagnosis of uterine leiomyomata among affected sisters. Am J Obstet Gynecol. 2008;198:168.e1-9. doi: 10.1016/j.ajog.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kjerulff KH, Langenberg P, Seidman JD, Stolley PD, Guzinski GM. Uterine leiomyomas: racial differences in severity, symptoms and age at diagnosis. J Reprod Med. 1996;41:483–490. [PubMed] [Google Scholar]
- 20.Laughlin SK, Baird DD, Savitz DA, Herring AH, Hartmann KE. Prevalence of uterine leiomyomas in the first trimester of pregnancy: an ultrasound-screening study. Obstet Gynecol. 2009;113:630–635. doi: 10.1097/AOG.0b013e318197bbaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peddada SD, Laughlin SK, Miner K, et al. Growth of uterine leiomyomata among premenopausal black and white women. Proc Natl Acad Sci U S A. 2008;105:19887–19892. doi: 10.1073/pnas.0808188105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National hospital discharge survey: 2007 summary. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 23.Mauskopf J, Flynn M, Thieda P, Spalding J, Duchane J. The economic impact of uterine fibroids in the United States: a summary of published estimates. J Womens Health (Larchmt) 2005;14:692–703. doi: 10.1089/jwh.2005.14.692. [DOI] [PubMed] [Google Scholar]
- 24.Whiteman MK, Kuklina E, Jamieson DJ, Hillis SD, Marchbanks PA. Inpatient hospitalization for gynecologic disorders in the United States. Am J Obstet Gynecol. 2010;202:541.e1-6. doi: 10.1016/j.ajog.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 25.Jacoby VL, Fujimoto VY, Giudice LC, Kuppermann M, Washington AE. Racial and ethnic disparities in benign gynecologic conditions and associated surgeries. Am J Obstet Gynecol. 2010;202:514–521. doi: 10.1016/j.ajog.2010.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luoto R, Raitanen J, Pukkala E, Anttila A. Effect of hysterectomy on incidence trends of endometrial and cervical cancer in Finland 1953–2010. Br J Cancer. 2004;90:1756–1759. doi: 10.1038/sj.bjc.6601763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstet Gynecol. 2009;114:1278–1283. doi: 10.1097/AOG.0b013e3181c2ce96. [DOI] [PubMed] [Google Scholar]