Abstract
Background
This study aimed to investigate the influence of deep sternal wound infection on long-term survival following cardiac surgery.
Material/Methods
In our institutional database we retrospectively evaluated medical records of 4732 adult patients who received open-heart surgery from January 1995 through December 2005. The predictive factors for DSWI were determined using logistic regression analysis. Then, each patient with deep sternal wound infection (DSWI) was matched with 2 controls without DSWI, according to the risk factors identified previously. After checking balance resulting from matching, short-term mortality was compared between groups using a paired test, and long-term survival was compared using Kaplan-Meier analysis and a Cox proportional hazard model.
Results
Overall, 4732 records were analyzed. The mean age of the investigated population was 69.3±12.8 years. DSWI occurred in 74 (1.56%) patients. Significant independent predictive factors for deep sternal infections were active smoking (OR 2.19, CI95 1.35–3.53, p=0.001), obesity (OR 1.96, CI95 1.20–3.21, p=0.007), and insulin-dependent diabetes mellitus (OR 2.09, CI95 1.05–10.06, p=0.016). Mean follow-up in the matched set was 125 months, IQR 99–162. After matching, in-hospital mortality was higher in the DSWI group (8.1% vs. 2.7% p=0.03), but DSWI was not an independent predictor of long-term survival (adjusted HR 1.5, CI95 0.7–3.2, p=0.33).
Conclusions
The results presented in this report clearly show that post-sternotomy deep wound infection does not influence long-term survival in an adult general cardio-surgical patient population.
Keywords: surgical complications, post-sternotomy wound infections, mediastinitis, multi-organ failure, sepsis
Background
Incidence of surgical site infections (SSI) ranges between 0.3% and 8%. Deep sternal wound infection (DSWI) is a severe and life-threatening complication of median sternotomy after cardiac surgery, with an incidence ranging from 1% to 3% [1,2] and a mortality rate ranging from 19% to 29% [1,3]. This complication is associated with prolonged hospital stay, augmented surgical load due to repeated wound revision, chest wall instability and consequent respiratory impairment, and elevated financial impact on hospital stay [4,5]. Although the predictive factors and risk profile of patients are well identified, the exact mechanism of DSWI has not been clearly described. Regarding the risk factors, there is a strong suggestion that impairment of vascular supply of the sternum may be one of the most important factors influencing the incidence of DSWI, including obesity, diabetes mellitus, chronic obstructive pulmonary disease (COPD), connective tissue disease, steroid use, smoking, peripheral vascular disease (PVD), and renal insufficiency. In addition, intraoperative factors (e.g., use of bilateral internal mammary arteries) and postoperative variables (e.g., prolonged mechanical ventilation; reoperation for bleeding; postoperative transfusions; and gastrointestinal, nephrologic, and respiratory complications) have been shown to be associated with DSWI [4–6].
Although the risk factors and treatment modalities were well explored and described in recent reports, the long-term influence of DSWI on postoperative life expectancy has seldom been addressed. In this report, we explore the influence of DSWI on postoperative survival over 10 years. Additionally, the natural history and evolution of history of patients with DSWI after discharge from the hospital is described with a focus on major cardiovascular events.
Material and Methods
Patient population and data collection
Included in these analyses were a total of 4732 consecutive patients who underwent open heart surgery at University Hospital Lausanne, CHUV, Switzerland, from January 1995 to December 2005. Patients having assist device implantation, heart transplantation, recent steroid treatment, and age younger than 18 years were excluded. Data from the institutional database were prospectively collected for variables such as age, sex, body mass index (BMI), type of surgical intervention, urgency of operation, prior cardiac surgery, congestive cardiomyopathy, history of myocardial infarction, smoking, diabetes mellitus, hypertension, family history, preoperative ejection fraction, cancer, COPD, and renal dysfunction. Procedural data were also collected on the use of cardiopulmonary bypass and the number of distal anastomoses. Postoperative parameters included emergency exploration due to hemodynamic instability, hospital mortality, length of stay, and major complications after surgery (e.g., transmural myocardial infarction, DSWI sepsis, renal failure, and respiratory failure).
Follow-up ended on April 15 2011 and was performed by phone calls to the patients and referred physicians.
Deep sternal wound infection patients were compared in a ratio of 1: 2 to the patients without infection; the matching criteria were: age, sex, surgical intervention, renal impairment, COPD, smoking, obesity, ejection fraction, and diabetes. Matching was performed in the institutional database, in which patients are routinely registered according to preoperative co-morbidities, intervention type, and in-hospital events.
Deep sternal wound infection was defined according to the guidelines of the Centers for Disease Control and Diagnosis, which requires fulfillment of at least 1 of the following criteria: (1) an organism isolated from culture of mediastinal tissue or fluid; (2) evidence of mediastinitis evident to the unaided eye; or (3) presence of either chest pain, sternal instability, or fever (38°C), and either purulent discharge from the mediastinum isolation of an organism isolated from blood culture or culture of drainage of the mediastinal area.
Data analysis
Statistical analyses were performed using SPSS software, version 17.0 (SPSS, Chicago, IL, USA). Data were tested for normality and equal distribution (Kolmogorov-Smirnov test and assessment of skewness and kurtosis). Risk factors of DSWI were identified using a binary logistic regression model applied to the entire population, after stepwise selection of the variables to be entered into the model. Adjusted odds ratios (OR) and 95% confidence intervals (CI95) were estimated.
To control for risk factors of DSWI, every patient with DSWI was matched with 2 control patients without DSWI, according to known risk factors of DSWI, and to those identified here. Balance between matched groups was checked using paired t tests for continuous variables, and McNemar’s test for categorical variables. In-hospital mortality rates were compared using McNemar’s test. Correlations between pre-, intra-, or postoperative variables and infection, or survival were evaluated by Pearson or Spearman correlation tests. Differences in postoperative survival between patients with DSWI and without DSWI were assessed by Kaplan-Meier analysis, the log-rank test, and a Cox regression model adjusted on parameters that were significantly correlated with survival or infection, as well as on the matching criteria mentioned above. Adjusted hazard ratios (HR) and CI95 were estimated.
Unless otherwise specified, numerical data are presented as mean and standard deviation (SD), and categorical data as group proportion (%) unless otherwise specified, and p < 0.05 was considered significant throughout.
Results
Out of 4792 patients who received open heart surgery during the period between December 1995 and January 2005, 74 patients (1.54%) developed deep sternal infection (DSWI). Matching of patients’ characteristics resulted in 2 groups: the DSWI group (n=74) compared to the control group (n=148) without infection (1:2 match). Significant independent predictors for the development of DSWI were: active smoking (OR 2.19, CI 1.35–3.53, p=0.001), obesity (OR 1.96, CI 1.20–3.21, p=0.007), and insulin-dependent diabetes mellitus (OR 2.09, CI 1.05–10.06, p=0.16).
The time to DSWI diagnosis ranged between 3 and 36 days, with a median of 13 days. The surgical treatment of DSWI was a 2-stage therapy. After diagnosis was established, the surgical revision was performed, including debridement of necrotic tissue and topical treatment with antiseptic solution. In the second part of the treatment, wound conditioning was performed by VAC. Secondary closure of the open chest wound was performed in all patients: as direct closure in 54 cases (72.3%), as reconstruction with rotated rectus abdominis flap in 11 patents (14.8%), and as pectoral muscle flap in 9 cases (12.2%). The preoperative characteristics of patients in both groups are presented in Table 1. Lengths of interventions (261±65 in DSWI vs. 208±55 min in controls; p=0.09), extracorporeal circulation time (111±61 in DSWI vs. 105±69 min in controls; p=0.74), and aortic cross-clamping time (76±42 min in DSWI vs. 67±35 min in controls; p=0.17) were not different between the 2 groups. In-hospital mortality was significantly higher in the DSWI group with 8% as compared to the control group with 2.7% (p=0.03). In the DSWI group, the hospital stay was longer as compared to the control group, 35 vs. 11 days, p<0.001). Incidence of acute postoperative renal impairment was also higher (25% vs. 8%, p=0.009). The frequencies of postoperative myocardial infarction, respiratory failure, and hemorrhage requiring re-intervention did not differ between patients with and without DSWI (Table 2). Cardiac cause of death during follow-up was not significantly different between groups (15% in the DSWI group vs. 11% in the control group, p=0.65)
Table 1.
Comparison of preoperative characteristic between groups after matching.
| DSWI group | Control group | p | |
|---|---|---|---|
| Age (years), mean, SD | 64±13 | 64±12 | 0.31 |
| Female | 19/74 (25.7%) | 40/148 (27.0%) | 1.00 |
| CABG | 49/74 (66.2%) | 98/148 (66.2%) | 1.00 |
| Valve operation | 24/74 (32.4%) | 48/148 (32.4%) | 1.00 |
| CABG + valve | 9/74 (12.1%) | 18/148 (12.2%) | 1.00 |
| Urgency operation | 14/74 (18.9%) | 18/148 (12.2%) | 0.36 |
| Ejection fraction categories | 0.23 | ||
| EF>50% | 23/74 (31.1%) | 55/148 (37.2%) | |
| EF 30–50% | 46/74 (62.2%) | 88/148 (59.4%) | |
| EF<30% | 5/74 (6.7%) | 5/148 (3.4%) | |
| Positive familiar anamnesis | 7/74 (9.4%) | 19/148 (12.8%) | 0.79 |
| Hypertension | 54/74 (74.0%) | 102/148 (68.9%) | 0.39 |
| COPD | 10/74 (13.5%) | 18/148 (12.2%) | 1.00 |
| Diabetes mellitus treated orally | 12/74 (16.2%) | 20/148 (13.5%) | 0.82 |
| Diabetes mellitus treated with insulin | 10/74 (13.5%) | 20/148 (13.5%) | 1.00 |
| Diabetes mellitus treated with diet | 3/74 (4.0%) | 4/148 (2.7%) | 1.00 |
| Impairement of renal function | 13/74 (17.6%) | 24/148 (16.2%) | 1.00 |
| Active smoking | 27/74 (36.5%) | 54/148 (36.5%) | 1.00 |
| Smoking history | 15/74 (20.3%) | 30/148 (20.3%) | 1.00 |
| Hypercholesterolemia | 34/74 (45.9%) | 76/148 (51.3%) | 0.62 |
| Hyper Triglyceridemia | 0/74 (0%) | 10/148 (6.7%) | 0.06 |
| Obesity (BMI >35) | 25/74 (33.8%) | 48/148 (32.4%) | 1.00 |
| Cancer | 8/74 (10.8%) | 4/148 (2.7%) | 0.10 |
Results are shown as numbers and percentages, unless stated otherwise. DSWI – deep sternal wound infection; CABG – coronary bypass graft; EF – ejection fraction; COPD – chronic obstructive pulmonary disease.
Table 2.
Postoperative complications in the matched set.
| DSWI group | Control group | p | |
|---|---|---|---|
| Reoperation because of hemorrhage | 7/74 (9.4%) | 16/148 (10.8%) | 1.00 |
| Length of hospital stay (days), median, IQR | 11, 10–15 | 35, 24–54 | <0.001 |
| Postoperative MI | 7/74 (9.4%) | 10/148 (6.7%) | 0.76 |
| Renal failure | 18/74 (24.3%) | 10/148 (6.7%) | 0.009 |
| Sepsis | 11/74 (14.9%) | 3/148 (2.0%) | 0.009 |
| Respiratory failure | 5/74 (6.7%) | 4/148 (2.7%) | 0.44 |
| In hospital mortality | 6/74 (8.1%) | 4/148 (2.7%) | 0.03 |
| Total mortality during follow up | 20/74 (27.0%) | 32/148 (21.6%) | 0.37 |
| Cardiac cause of mortality during follow up | 11/74 (14.9%) | 16/148 (10.8%) | 0.65 |
Results are shown as numbers and percentages, unless stated otherwise. DSWI – deep sternal wound infection; MI – myocardial infarction.
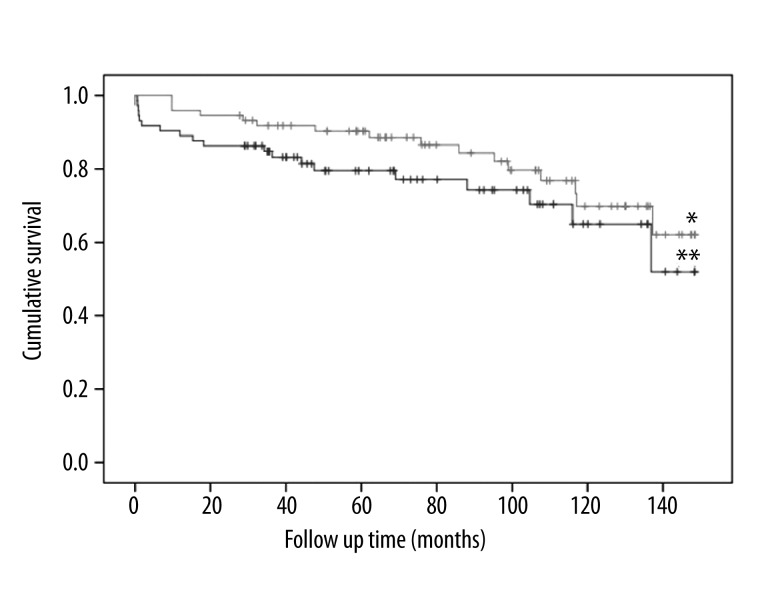
The median follow-up in the matched set was 125 months and the IQR ranged from 99 to 162 months. During follow-up, the mortality rate was 27.0% in the DSWI group and 21.6% in controls (log-rank test p value 0.57, Figure 1). After adjustment on the parameters that were significantly correlated with survival or infection, as well as on the matching criteria mentioned above, the risk of death during follow-up was not related to the occurrence of DSWI (HR 1.5, CI95 0.7–3.2, p=0.33). Independent predictors for long-term mortality were preoperative cancer (HR 12.1, CI95 3.9–37.2; p<0.001), surgery for heart valve in conjunction with aorto-coronary bypass (HR 3.8, CI95 1.6–9.1; p=0.003), and preoperative chronic lung disease (HR 2.6, CI95 1.1–6.2; p=0.03).
Figure 1.
Kaplan-Meier plot showing survival over a more than 10-year follow-up. Long-term survival was not significantly different between patients with DSWI (*) and controls without DSWI (**), 27.0% vs. 21.6% respectively, log-rank test p-value 0.57.
Discussion
Deep sternal wound infection is one of the most serious postoperative complications after median sternotomy and it has a relatively high mortality. This has motivated numerous research groups to evaluate in detail the clinical profiles of patients with DSWI as well as to explore the predictive factors that may presage this pathology. In this context, the influence of DSWI on in-hospital and short-term mortality was one of the most intensively discussed subjects in the past [1–6]. It seems that preoperative as well as intra-operative predictive factors were well identified. However, most risk factors for DSWI are not amenable to modification [7]. In order to reduce the incidence of DSWI, different preventive measures were undertaken. For example, in patients with diabetes mellitus, tight control of blood sugar level reduced the incidence of DSWI [8], and use of skeletonized mammary artery also significantly contributed to reduction of this complication [9]. Although the characteristics of DSWI were well explored, long-term survival and mortality profile of the patients having DSWI after hospital admission has not been sufficiently described and evaluated. To the best of our knowledge, few reports in the literature have discussed mid-term or long-term results following DSWI [10–12].
In the present study, a follow-up of more that 10 years was executed by phone calls to the patients and their personal physicians. Information regarding mortality and complications during this period were obtained. Incidence of DSWI was 1.56%, with perioperative mortality of 8.1%; both results are comparable to results published in the literature, in which the incidence of DSWI is reported to be between 1.5% and 3%, with a perioperative mortality ranging from 15% to 30% [10–12]. Out of 74 patients, a cardiac cause of death was presented in 5 patients and sepsis was presented in 4 cases. In 1 case with cardiac cause of death, laceration of the right ventricle was the cause of death. In the 3 remaining cases, cardiac failure was the reason for death.
In long-term survival, there was no difference between groups. The total mortality was 27% in the DSWI group and 21.6% in the controls (p=0.57), which actually corresponds to the long-term mortality after open heart surgery [14,15]. Mortality due to a cardiac event was not significantly different in the 2 groups investigated: 15% in DSWI and 11% in controls. This result corresponds to the reports published in which the impact of DSWI following cardiac surgery was evaluated over a period of 8 years [12,15]. Thirty-day mortality was also elevated in the DSWI group – 7.3% vs. 1.6% in the control group [15]. No further differences in 4-year and 8-year survival rate between the 2 groups were found (77.2% and 61.8%, respectively, in patients with DSWI, as compared with 78.0% and 67.5%, respectively, in patients without DSWI) [15]. Consistent with results reported by Cayci et al. [16], DSWI did not influence the long-term survival in the present population.
However, we have to be aware that this statement is only true after the perioperative period passed. This can also be seen in the Kaplan Meier curve, where the survival between the 2 groups is parallel after the perioperative period. This means that the in-hospital period for patients is critical, with elevated mortality. If this phase is successfully survived, their life expectancy does not differ from that of patients without DSWI. Reasons for in-hospital mortality in the DSWI group are multifactorial.
The in-hospital mortality was 7%, which is about 3 times higher than in the in-patient population without DSWI. In the majority of cases, it was a consequence of septicemia and/or multi-organ failure. In addition to the septic events, repeated surgical revision with change of VAC systems may contribute to elevated mortality. Repeated surgical revisions are earmarked by repeated surgical trauma, which clearly increases perioperative stress. Debridement and occasional sternal bone fractures due to infection, as well as debridement and repeated surgical manipulation with VAC system, may contribute to laceration and perforation of the right ventricle. This was also a case in our series.
Conclusions
DSWI is one of the most devastating complications in the postoperative period – patients suffer from a prolonged hospital stay coupled with repeated surgical interventions, which leads to increased hospital costs. Overall, the pathophysiological mechanism is unclear and difficult to prevent. The incidence has remained stable, and although different prevention measures have been proposed in the last decade, they have not lowered the prevalence of this complication. However, we believe that if prevention is impossible at this point of our knowledge, then treatment modalities may be changed to reduce the length of hospital stay, as well as reduce surgical trauma, mortality, and morbidity [16]. However, to prove this hypothesis, further clinical trials should be conducted.
Footnotes
Source of support: Departmental sources
References
- 1.Milano CA, Kesler K, Archibald N, et al. Mediastinitis after coronary artery bypass graft surgery. Circulation. 1995;92:2245–51. doi: 10.1161/01.cir.92.8.2245. [DOI] [PubMed] [Google Scholar]
- 2.Lu JCY, Grayson AD, Jha P, et al. Risk factors for sternal wound infection and mid-term survival following coronary artery bypass surgery. Eur J Cardiothorac Surg. 2003;23:943–49. doi: 10.1016/s1010-7940(03)00137-4. [DOI] [PubMed] [Google Scholar]
- 3.Gardlund B, Bitkover CY, Vaage J. Postoperative mediastinitis in cardiac surgery – microbiology and pathogenesis. Eur J Cardiothorac Surg. 2002;21:825–30. doi: 10.1016/s1010-7940(02)00084-2. [DOI] [PubMed] [Google Scholar]
- 4.Heilmann C, Stahl R, Schneider C, et al. Wound complications after median sternotomy: a single-centre study. Interact Cardiovasc Thorac Surg. 2013;16(5):643–48. doi: 10.1093/icvts/ivs554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Itagaki S, Cavallaro P, Adams DH, Chikwe J. Bilateral internal mammary artery grafts, mortality and morbidity: an analysis of 1 526 360 coronary bypass operations. Heart. 2013;99(12):849–53. doi: 10.1136/heartjnl-2013-303672. [DOI] [PubMed] [Google Scholar]
- 6.Parissis H, Al-Alao B, Soo A, et al. Risk analysis and outcome of mediastinal wound and deep mediastinal wound infections with specific emphasis to omental transposition. J Cardiothorac Surg. 2011;6:111. doi: 10.1186/1749-8090-6-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baskett RJ, MacDougall CE, Ross DB. Is mediastinitis a preventable complication? A 10-year review. Ann Thorac Surg. 1999;67:462–65. doi: 10.1016/s0003-4975(98)01195-3. [DOI] [PubMed] [Google Scholar]
- 8.Matros E, Aranki SF, Bayer LR, et al. Reduction in incidence of deep sternal wound infections: random or real? J Thorac Cardiovasc Surg. 2010;139(3):680–85. doi: 10.1016/j.jtcvs.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Peterson MD, Borger MA, Rao V, et al. Skeletonization of bilateral internal thoracic artery grafts lowers the risk of sternal infection in patients with diabetes. J Thorac Cardiovasc Surg. 2003;126:1314–19. doi: 10.1016/s0022-5223(03)00808-0. [DOI] [PubMed] [Google Scholar]
- 10.Braxton JH, Marrin CA, McGrath PD, et al. 10-year follow-up of patients with and without mediastinitis. Semin Thorac Cardiovasc Surg. 2004;16(1):70–76. doi: 10.1053/j.semtcvs.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Braxton JH, Marrin CA, McGrath PD, et al. Mediastinitis and long-term survival after coronary artery bypass graft surgery. Ann Thorac Surg. 2000;70:2004–7. doi: 10.1016/s0003-4975(00)01814-2. [DOI] [PubMed] [Google Scholar]
- 12.de Moraes AA, Abboud CS, Chammas AZ, et al. Long term mortality of deep sternal wound infection after coronary artery bypass surgery. Rev Bras Cir Cardiovasc. 2012;27(3):377–82. doi: 10.5935/1678-9741.20120065. [DOI] [PubMed] [Google Scholar]
- 13.Head SJ, Osnabrugge RL, Howell NJ, et al. A systematic review of risk prediction in adult cardiac surgery: considerations for future model development. Eur J Cardiothorac Surg. 2013;43(5):e121–29. doi: 10.1093/ejcts/ezt044. [DOI] [PubMed] [Google Scholar]
- 14.Wu C, Camacho FT, Wechsler AS, et al. Risk score for predicting long-term mortality after coronary artery bypass graft surgery. Circulation. 2012;125(20):2423–30. doi: 10.1161/CIRCULATIONAHA.111.055939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cayci C, Russo M, Cheema F, et al. Risk Analysis of Deep Sternal Wound Infections and Their Impact on Long-Term Survival: A Propensity Analysis. Ann Plast Surg. 2008;61:294–301. doi: 10.1097/SAP.0b013e31815acb6a. [DOI] [PubMed] [Google Scholar]
- 16.Berdajs DA, Trampuz A, Ferrari E, et al. Delayed primary versus late secondary wound closure in the treatment of postsurgical sternum osteomyelitis. Interact Cardiovasc Thorac Surg. 2011;12(6):914–18. doi: 10.1510/icvts.2010.263483. [DOI] [PubMed] [Google Scholar]