Abstract
Aims
To describe temporal trends in methamphetamine use among young injection drug users (IDU) in San Francisco.
Design and Methods
Secondary analysis of cross-sectional baseline data collected for a longitudinal study of young IDU from 1998 to 2004. Participants were 1445 young IDU (< 30 years old) who reported injection in the previous month, English-speaking, and recruited by street outreach methods. We examined trends for: lifetime (ever) and recent (30-day) methamphetamine use, including injected and non-injected, and by age group and sexual risk behaviour [men who have sex with men injecting drug users (MSM-IDU), male IDU (non-MSM) and female IDU].
Results
In 1998, 1999, 2000, 2001, 2003 and 2004 we interviewed 237, 276, 431, 310, 147 and 44 participants, respectively. Overall, median age was 22 years [interquartile range (IQR) 20 – 25], 30.3% were women and median duration of injecting was 4.4 years (IQR 2 – 7). Prevalence of methamphetamine use was high, with 50.1% reporting recent injection, but overall there were no temporal increases in reported ‘ever’ injected use. Recent methamphetamine injection (past 30 days) increased significantly, and peaked at 60% in 2003. MSM-IDU had higher methamphetamine injection ever (92.3%) and recently (59.5%) compared to heterosexual male (non-MSM) IDU (81.6% and 47.3%, respectively) and to female IDU (78.4% and 46.1%, respectively).
Conclusions
Despite reports of ubiquitous increases in methamphetamine use, there were no significant increases in 6 years in ever injecting methamphetamine overall among young IDU. MSM-IDU who reported the highest methamphetamine use overall reported some increases in recent injected use. The methamphetamine ‘epidemic’ was probably under way among young IDU earlier than other populations.
Keywords: injection drug use, methamphetamine, MSM-IDU, prevalence, trends, young injectors
Introduction
In the United States, methamphetamine use grew rapidly in the 1990s and became a significant public health concern nationally. Chronic use is associated with significant negative acute and chronic health, psychiatric and social consequences [1 – 9], and methamphetamine users are among the most difficult drug treatment patients [10]. In certain populations, including men who have sex with men (MSM), methamphetamine is associated with high-risk sexual and injection behaviors and elevated human immunodeficiency virus (HIV) rates [4,11 – 14]. In the United States, the spotlight on methamphetamine use has been especially intense as it has become more widespread, particularly among white, middle-class youth and young adults [15 – 17]. Groups experiencing increases, however, appear to be heterogeneous, including Hispanic and Asian populations, male and female sex workers, transgendered people, high-school and college students and farm workers [15,18,19]. Nationally, indicators of escalating methamphetamine use in the last decade include increases in: admissions to publicly funded drug treatment programmes [20]; emergency department reports involving methamphetamine [21]; and the percentage and numbers of arrestees testing positive for methamphetamine [22]. In California, methamphetamine-related admissions to drug treatment programmes increased 363% from 1992 to 2005 [20].
In San Francisco, street-based youth and young adults have historically had high exposure to methamphetamine [23 – 26]. In some of the only trend data available in San Francisco, methamphetamine use among marginally housed and homeless adults tripled overall between 1996 and 2003, but quadrupled in the younger groups (< 35 years) [27]. From 1989 to 2004 methamphetamine use (past 30-day recall) increased from 24% to 37% among older injection drug users (IDU) [28]. As the public health literature and lay press have published widely on increases in methamphetamine use in the United States, in particular among youth, we hypothesised that methamphetamine use increased among young IDU. Here we examine longitudinal trends in reported methamphetamine use from cross-sectional data collected serially from ongoing study of young IDU in San Francisco, California.
Methods
Population
Young IDU were recruited from 1998 to 2001 and 2003 to 2004 to participate in the UFO Study (at the study's inception, the acronym represented ‘U Find Out’ (serostatus); details and recruitment procedures are described in detail in [29]) in San Francisco, California, using targeted street outreach methods. In brief, young IDU were recruited by peer outreach workers to screen for participation in prospective epidemiological studies of HIV, hepatitis B and C virus (HBV and HCV) infections. In 1999 only, snowball sampling methods were added, wherein participants were asked to refer other known young IDU. In all years, eligible participants were under age 30, reported injection in the previous month and were English-speaking. A baseline structured interview assessing self-reported behavioural risk and drug exposures was administered, followed by counselling and testing for HIV, HBV and HCV. Participants were reimbursed for interview time and returning for test results. We examined temporal trends in self-reported injected and non-injected methamphetamine at baseline interview.
Methamphetamine use variables
For all years, data were examined regarding recent (past 30 days) or ‘ever’ self-reported injected methamphetamine. Regarding non-injection use of methamphetamine, in addition to ‘ever’ use, participants were asked about use in the past year (in 1998 and 1999) and use in the past 3 months (2000, 2001, 2003 and 2004).
Analyses
Summary statistics were calculated for selected sociodemographic and risk exposures. Yearly trends in methamphetamine use were examined overall, as well as by age group [≤22 compared to > 22 (cut-offs were based on median age of the sample)] and sexual risk group (MSM-IDU, male non-MSM-IDU and female IDU), using χ2 tests for trend. All analyses were conducted using stata 9.0 (STATA Corporation, College Station, TX, USA).
Results
Participants were interviewed in 1998 (n = 237), 1999 (n = 276), 2000 (n = 431), 2001 (n = 310), 2003 (n= 147) and 2004 (n = 44) (Table 1). Overall, median age of participants was 22 years [interquartile range (IQR) 20, 25], the majority reported injecting daily (64.5%), was male (69.7%) and most (83.5%) reported not being housed the previous night. The median number of reported years of injecting was four (IQR, 2, 7). Prevalence of HIV, HBV and HCV infections were 3.5%, 20.9% and 38.8%, respectively.
Table 1. Characteristics and prevalence of selected risk exposures among of young IDU in San Francisco (1998 – 2004).
| Characteristics | Total (n = 1445) n (%) |
|---|---|
| Median age (IQR) | 22.0 (20 – 25) |
| Gender | |
| Male | 1007 (69.7) |
| Female | 438 (30.3) |
| Race/ethnicity | |
| Caucasian | 1132 (79.0) |
| Non-Caucasian | 301 (21.0) |
| Sexual risk group | |
| MSM | 359 (25.0) |
| Male (non-MSM) | 640 (44.5) |
| Female | 438 (30.5) |
| Housing last night | |
| No | 1044 (72.7) |
| Yes | 392 (27.3) |
| Education | |
| <High school | 721 (50.2) |
| High school | 443 (30.9) |
| >High school | 272 (18.9) |
| Median number of years injecting (IQR) | 4.4 (2 – 7) |
| Injected every day last 30 days | |
| No | 934 (64.8) |
| Yes | 507 (35.2) |
IQR: interquartile range; MSM: men who have sex with men.
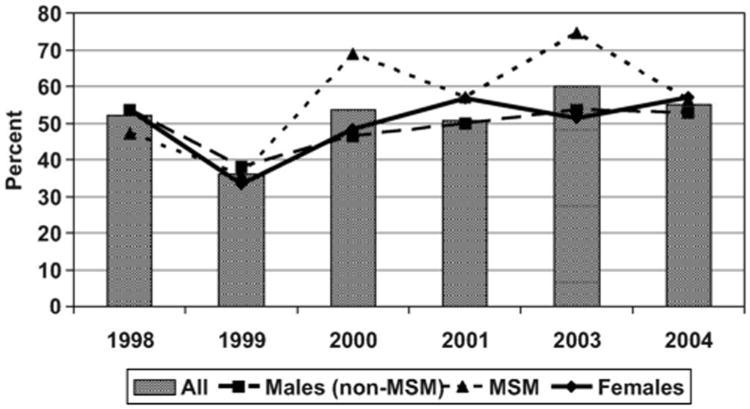
Table 2 shows the proportion of respondents reporting ever and recent injection and non-injection methamphetamine use: overall, by year and stratified by gender/risk and age groups. A majority (83.7% overall) of participants reported having ever injected methamphetamine; no significant changes were observed over time for ever injecting methamphetamine in any subgroup. Overall, a higher proportion of MSM-IDU reported having ever injected methamphetamine (92.3%) compared to male (non-MSM) IDU (81.6%) and female IDU (78.4%), and over most years (Figure 1). Injected methamphetamine in the past 3 months showed similar patterns. Statistically significant temporal differences (p ≤ 0.01) were seen with respect to recent methamphetamine injection (past 30 days) among MSM-IDU and older (>22 years) participants, with a nadir in 1999 and a peak in reported use in 2003, which was consistent across all groups.
Table 2. Trends in injection and non-injection methamphetamine use from 1998 to 2004 by sexual risk and age group in young injectors in San Francisco (n = 1445).
| Total n (%) | 1998 N = 237 | 1999 N = 276 n (%) | 2000 N = 431 n (%) | 2001 N = 310 n (%) | 2003 N = 147 n (%) | 2004 N = 44 n (%) | p-value for trend | |
|---|---|---|---|---|---|---|---|---|
| Injected methamphetamine ever (yes) | ||||||||
| All | 775 (83.7) | 364 (84.7) | 253 (81.9) | 122 (84.7) | 36 (83.7) | 0.94 | ||
| Female | 214 (78.4) | 102 (81.6) | 78 (74.3) | 28 (77.8) | 6 (85.7) | 0.77 | ||
| Male (non-MSM) | 315 (81.6) | 143 (80.8) | 110 (82.1) | 46 (83.6) | 16 (80.0) | 0.66 | ||
| Male MSM | 241 (92.3) | 119 (93.0) | 65 (92.9) | 43 (91.5) | 14 (87.5) | 0.49 | ||
| ≤22 | 375 (81.5) | 181 (84.2) | 142 (78.9) | 37 (77.1) | 15 (88.2) | 0.48 | ||
| >22 | 400 (85.8) | 183 (85.1) | 111 (86.1) | 85 (88.5) | 21 (80.8) | 0.78 | ||
| Injected methamphetamine in last 3 months (yes) | ||||||||
| All | 539 (58.2) | 251 (58.2) | 165 (53.6) | 99 (68.3) | 24 (57.1) | 0.12 | ||
| Female | 143 (52.0) | 67 (53.2) | 51 (48.6) | 21 (56.8) | 4 (57.1) | 0.33 | ||
| Male (non-MSM) | 209 (54.3) | 93 (52.5) | 72 (53.7) | 33 (60.0) | 11 (57.9) | 0.72 | ||
| Male MSM | 182 (70.0) | 91 (71.1) | 42 (60.9) | 40 (85.1) | 9 (56.3) | 0.54 | ||
| ≤22 | 260 (56.4) | 120 (55.6) | 98 (54.4) | 32 (66.7) | 10 (58.8) | 0.27 | ||
| >22 | 279 (60.0) | 131 (60.9) | 67 (52.3) | 67 (69.1) | 14 (56.0) | 0.38 | ||
| Injected methamphetamine last 30 days (yes) | ||||||||
| All | 719 (50.1) | 123 (52.1) | 99 (36.1) | 231 (53.6) | 156 (50.5) | 87 (60.0) | 23 (56.1) | <0.01 |
| Female | 200 (46.1) | 37 (53.6) | 30 (33.3) | 61 (48.4) | 49 (46.7) | 19 (51.4) | 4 (57.1) | 0.36 |
| Male (non-MSM) | 302 (47.3) | 60 (53.6) | 54 (38.0) | 82 (46.3) | 67 (50.0) | 29 (52.7) | 10 (55.6) | 0.48 |
| Male MSM | 213 (59.5) | 26 (47.3) | 15 (35.7) | 88 (68.8) | 40 (57.1) | 35 (74.5) | 9 (56.3) | <0.01 |
| ≤22 | 372 (49.3) | 71 (56.4) | 61 (36.3) | 111 (51.4) | 91 (50.6) | 29 (60.4) | 9 (56.3) | 0.17 |
| >22 | 347 (50.9) | 52 (47.3) | 38 (35.9) | 120 (55.8) | 65 (50.4) | 58 (59.8) | 14 (56.0) | 0.01 |
| Non-injection methamphetamine ever (yes) | ||||||||
| All | 851 (91.8) | 407 (94.4) | 283 (91.3) | 125 (87.4) | 36 (83.7) | <0.01 | ||
| Female | 251 (91.6) | 120 (95.2) | 95 (89.6) | 31 (88.6) | 5 (71.4) | 0.06 | ||
| Male (non-MSM) | 352 (91.2) | 165 (93.2) | 122 (91.0) | 49 (89.1) | 16 (80.0) | 0.03 | ||
| Male MSM | 243 (93.1) | 122 (95.3) | 66 (94.3) | 40 (85.1) | 15 (93.8) | 0.06 | ||
| ≤22 | 424 (91.8) | 206 (95.4) | 163 (90.1) | 40 (83.3) | 15 (88.2) | <0.01 | ||
| >22 | 427 (91.8) | 201 (93.5) | 120 (93.0) | 85 (89.5) | 21 (80.8) | 0.03 | ||
| Non-injection methamphetamine use last year* (yes) | ||||||||
| All | 209 (40.7) | 98 (41.4) | 111 (40.2) | – | – | – | – | 0.79 |
| Female | 65 (40.4) | 32 (45.7) | 33 (36.3) | 0.07 | ||||
| Male (non-MSM) | 98 (38.6) | 37 (33.0) | 61 (43.0) | 0.09 | ||||
| Male MSM | 46 (46.9) | 29 (52.7) | 17 (39.5) | 0.12 | ||||
| ≤22 | 138 (46.5) | 65 (51.2) | 73 (42.9) | 0.04 | ||||
| >22 | 71 (32.9) | 33 (30.0) | 38 (35.9) | 0.47 | ||||
| Non-injection methamphetamine last 3 months† (yes) | ||||||||
| All | 478 (51.4) | 211 (49.0) | 152 (49.0) | 91 (62.3) | 24 (55.8) | 0.01 | ||
| Female | 147 (53.3) | 63 (50.0) | 58 (54.7) | 23 (62.2) | 3 (42.9) | 0.03 | ||
| Male (non-MSM) | 172 (44.6) | 75 (42.4) | 54 (40.3) | 31 (56.4) | 12 (60.0) | 0.39 | ||
| Male MSM | 154 (59.0) | 73 (57.0) | 40 (57.1) | 32 (68.1) | 9 (56.3) | 0.35 | ||
| ≤22 | 243 (52.5) | 110 (50.9) | 91 (50.3) | 31 (63.3) | 11 (64.7) | 0.09 | ||
| >22 | 235 (50.3) | 101 (47.0) | 61 (47.3) | 60 (61.9) | 13 (50.0) | 0.04 | ||
In 1998 and 1999, participants were asked about non-injection use in the past year;
in 2000 – 04, participants were asked about non-injection use in the past 3 months. IQR: interquartile range; MSM: men who have sex with men.
Figure 1.
Trends in self-reported injected methamphetamine use in the last 30 days among young IDU in San Francisco by year and by sexual risk group.
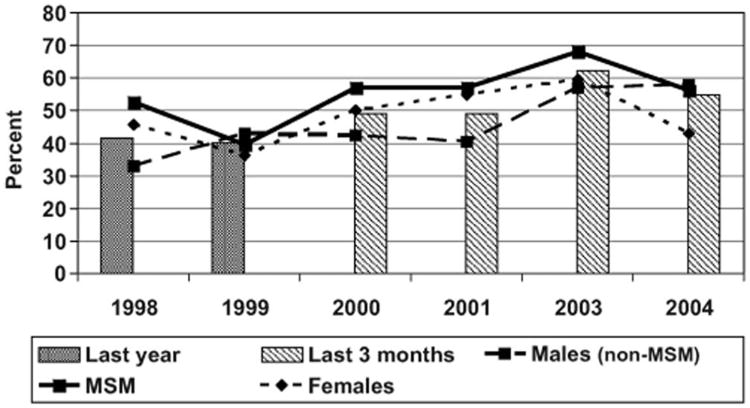
Non-injection methamphetamine use ‘ever’, which could include smoking and snorting, was reported by almost all participants (91.8%). Significant declines are seen over time in the overall sample (p < 0.01), consistent across all subgroups, except from 2003 to 2004, when those aged 22 and older reported a slight increase. Reported non-injection use in the previous 3 months varied significantly overall, with the highest proportion (62.3%) in 2003 (p = 0.01); the same trends were seen in all subgroups, but were significant only among females (0.03) and those 22 years and older (0.04). Declines seen in non-injection use of methamphetamine were not associated with any observed increases in injection use. As with injected methamphetamine, a higher proportion of MSM compared to males (non-MSM) and females reported recent non-injection use, but differences were not significant (Figure 2).
Figure 2.
Trends in self-reported non-injected methamphetamine use among young IDU in San Francisco by year and by sexual risk group.
Discussion
Among young IDU in San Francisco, methamphetamine use has been very high since 1998 and continuing through 2004. In general, no temporal increases were observed in reported methamphetamine injection with respect to lifetime (ever) use; however, very recent (past 30 days) use increased significantly, corresponding to a nadir in 1999 and peak in 2003. Reported recent use in all other years varied little, between 50% and 60%. The declines observed in 1999 may be associated with the modified sampling methods (resulting in fewer methamphetamine users). Significant declines were noted in non-injection use for lifetime ‘ever’ recall, but not for shorter recall periods. The results suggest that the ‘methamphetamine epidemic’ was under way among young IDU earlier than among other populations. The proportion of young San Francisco IDU reporting methamphetamine use was radically higher than that reported by young IDU in Vancouver, where methamphetamine injection prevalence was 6.7% in 2004 [30].
The higher reported use of methamphetamine among the MSM subgroup in this sample of young IDU compared to male (non-MSM) and female IDU corroborates other reports of increased methamphetamine use among MSM, especially younger ones, in San Francisco [12]. These increases corresponded to elevated rates of HIV, which are attributed largely to higher-risk sexual exposures [31 – 33], including trading sex for drugs [34], which may be practised to obtain methamphetamine [35] in this high-risk group.
Findings from this study have the following potential limitations. First of all, these are secondary data analyses; the UFO studies were designed principally to examine disease outcomes associated with injection-related exposures. The consistency of the data suggest that, over time, few if any differential reporting occurred, even with respect to sexual risk and age groups. Even in 1999, when reported recent injected methamphetamine was lowest, the results did not vary by group. These factors suggest that the data are not highly compromised.
This study contributes to the literature of drug use among young high-risk IDU, which lacks population-based documentation on temporal trends in types, frequency and methods of administration. Methamphetamine among young IDU in San Francisco is higher than other locales and other groups; it is likely to contribute to the high morbidity and mortality of young IDU, as well as increased risk for HIV in association with both elevated sexual and injection related risks [30,36 – 39]. These data show the continued urgent need for methamphetamine prevention and intervention programmes targeted toward young IDU.
Acknowledgments
The authors would like to acknowledge the ongoing participation of all the UFO Study participants whose involvement continues to help provide important information to public health practice and research. We also wish to recognise the contributions the UFO Study receives from the San Francisco Department of Public Health, Tenderloin AIDS Resource Center (TARC), SOS, and Homeless Youth Alliance (HIYA). This study and the authors were supported by US National Institutes for Health 2 R01 DA016017-03A1 and K01 DA023365. Ms Inglez-Dias was supported to participate in the CAPS International Training Program in AIDS Prevention Studies Scientific Writing Program by NIH awards R25 MH64712 and 1 D43 TW05799-04.
References
- 1.Williams N, Covington JS., III Methamphetamine and meth mouth: an overview. J Tenn Dent Assoc. 2006;86:32–5. [PubMed] [Google Scholar]
- 2.Meredith CW, Jaffe C, Ang-Lee K, Saxon AJ. Implications of chronic methamphetamine use: a literature review. Harv Rev Psychiatry. 2005;13:141–54. doi: 10.1080/10673220591003605. [DOI] [PubMed] [Google Scholar]
- 3.McKetin R, McLaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction. 2006;101:1473–8. doi: 10.1111/j.1360-0443.2006.01496.x. [DOI] [PubMed] [Google Scholar]
- 4.Shoptaw S, Peck J, Reback CJ, Rotheram-Fuller E. Psychiatric and substance dependence comorbidities, sexually transmitted diseases, and risk behaviors among methamphetamine-dependent gay and bisexual men seeking outpatient drug abuse treatment. J Psychoact Drugs. 2003;35(Suppl. 1):161–8. doi: 10.1080/02791072.2003.10400511. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Hayashi T, Chang CF, et al. Methamphetamine potentiates ischemia/reperfusion insults after transient middle cerebral artery ligation. Stroke. 2001;32:775–82. doi: 10.1161/01.str.32.3.775. [DOI] [PubMed] [Google Scholar]
- 6.Smith L, Yonekura ML, Wallace T, Berman N, Kuo J, Berkowitz C. Effects of prenatal methamphetamine exposure on fetal growth and drug withdrawal symptoms in infants born at term. J Dev Behav Pediatr. 2003;24:17–23. doi: 10.1097/00004703-200302000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Hong R, Matsuyama E, Nur K. Cardiomyopathy associated with the smoking of crystal methamphetamine. JAMA. 1991;265:1152–4. [PubMed] [Google Scholar]
- 8.Lan KC, Lin YF, Yu FC, Lin CS, Chu P. Clinical manifestations and prognostic features of acute methamphetamine intoxication. J Formos Med Assoc. 1998;97:528–33. [PubMed] [Google Scholar]
- 9.Sheridan J, Bennett S, Coggan C, Wheeler A, McMillan K. Injury associated with methamphetamine use: a review of the literature. Harm Reduct J. 2006;3:14. doi: 10.1186/1477-7517-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rawson RA, Gonzales R, Brethen P. Treatment of methamphetamine use disorders: an update. J Subst Abuse Treat. 2002;23:145–50. doi: 10.1016/s0740-5472(02)00256-8. [DOI] [PubMed] [Google Scholar]
- 11.Mansergh G, Purcell DW, Stall R, et al. CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection: summary and suggestions. Public Health Rep. 2006;121:127–32. doi: 10.1177/003335490612100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colfax G, Coates TJ, Husnik MJ, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82:i62–70. doi: 10.1093/jurban/jti025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Page-Shafer K, Veugelers PJ, Moss AR, Strathdee S, Kaldor JM, van Griensven GJ. Sexual risk behavior and risk factors for HIV-1 seroconversion in homosexual men participating in the Tricontinental Seroconverter Study, 1982 – 1994. Am J Epidemiol. 1997;146:531–42. doi: 10.1093/oxfordjournals.aje.a009311. [DOI] [PubMed] [Google Scholar]
- 14.Chesney MA, Barrett DC, Stall R. Histories of substance use and risk behavior: precursors to HIV seroconversion in homosexual men. Am J Public Health. 1998;88:113–16. doi: 10.2105/ajph.88.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunt D, Kuck S, Truitt L. Methamphetamine use: lessons learned. [accessed 27 March 2007];Report to the US Department of Justice no 209730. 2006 Jan 31; Available at: http://www.ncjrs.gov/pdffiles1/nij/grants/209730.pdf.
- 16.Anglin MD, Perrochet B. Drug use and crime: a historical review of research conducted by the UCLA Drug Abuse Research Center. Subst Use Misuse. 1998;33:1871–914. doi: 10.3109/10826089809059325. [DOI] [PubMed] [Google Scholar]
- 17.Gibson DR, Leamon MH, Flynn N. Epidemiology and public health consequences of methamphetamine use in California's Central Valley. J Psychoact Drugs. 2002;34:313–19. doi: 10.1080/02791072.2002.10399969. [DOI] [PubMed] [Google Scholar]
- 18.Rutkowski BA. California Substance Abuse Research Consortium, September 2005: update on recent methamphetamine trends in four California regions. J Psychoact Drugs. 2006;(Suppl. 3):369–75. doi: 10.1080/02791072.2006.10400600. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control. Methamphetamine use and HIV risk behaviors among heterosexual men—preliminary results from five northern California counties, December 2001 – November 2003. MMWR. 2006;55:273–7. [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services Substance Abuse and Mental Health Services Administration Office of Applied Studies. Treatment episode data set (TEDS) Rockville, MD: National Admissions to Substance Abuse Treatment Services; 2005. [accessed 27 March 2007]. Available at: http://www.oas.samhsa.gov. [Google Scholar]
- 21.US Department of Health and Human Services Substance Abuse (UHDHHS) and Mental Health Services Administration Office of Applied Studies (MHSAOAS) DAWN Series. Rockville, MD: UHDHHS/MHSAOAS; [accessed 27 March 2007]. Drug Abuse Warning Network, 2005: national estimates of drug related emergency department visits. Available at: http://DAWNinfo.samhsa.gov/ [Google Scholar]
- 22.US Department of Justice. National Institute of Justice Arrestee drug abuse monitoring program. Washington, DC: US Department of Justice, National Institute of Justice; [accessed 27 March 2007]. Available at: http://www.ojp.usdoj.gov/nij/adam/welcome.html. [Google Scholar]
- 23.Clements K, Gleghorn A, Garcia D, Katz M, Marx R. A risk profile of street youth in northern California: implications for gender-specific human immunodeficiency virus prevention. J Adolesc Health. 1997;20:343–53. doi: 10.1016/S1054-139X(97)00033-5. [DOI] [PubMed] [Google Scholar]
- 24.Gleghorn AA, Marx R, Vittinghoff E, Katz MH. Association between drug use patterns and HIV risks among homeless, runaway, and street youth in northern California. Drug Alcohol Depend. 1998;51:219–27. doi: 10.1016/s0376-8716(98)00042-8. [DOI] [PubMed] [Google Scholar]
- 25.Moon MW, Binson D, Page-Shafer K, Diaz R. Correlates of HIV risk in a random sample of street youths in San Francisco. J Assoc Nurses AIDS Care. 2001;12:18–27. doi: 10.1016/S1055-3290(06)60182-9. [DOI] [PubMed] [Google Scholar]
- 26.Kral AH, Lorvick J, Edlin BR. Sex- and drug-related risk among populations of younger and older injection drug users in adjacent neighborhoods in San Francisco. J Acquir Immune Def Syndr. 2000;24:162–7. doi: 10.1097/00126334-200006010-00011. [DOI] [PubMed] [Google Scholar]
- 27.Das-Douglas M, Colfax G, Moss AR, Bangsberg DR, Hahn JA. Tripling of methamphetamine/amphetamine use among homeless and marginally housed persons, 1996 – 2003. J Urban Health. 2007 doi: 10.1007/s11524-007-9249-4. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.San Francisco Department of Public Health. Synthesis of data on methamphetamine use in San Francisco. [accessed 9 January 2008];HIV/AIDS statistics and epidemiology section. 2007 Mar; Available at: www.dph.sf.ca.us/sfcityclinic/providers/MethRaymondReport2006.pdf.
- 29.Hahn J, Page-Shafer K, Lum P, Ochoa K, Moss A. Hepatitis C virus infection and needle exchange use among young injection drug users in San Francisco. Hepatology. 2001;34:180–7. doi: 10.1053/jhep.2001.25759. [DOI] [PubMed] [Google Scholar]
- 30.Fairbairn N, Kerr T, Buxton JA, Li K, Montaner JS, Wood E. Increasing use and associated harms of crystal methamphetamine injection in a Canadian setting. Drug Alcohol Depend. 2006;8:313–16. doi: 10.1016/j.drugalcdep.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Colfax G, Shoptaw S. The methamphetamine epidemic: implications for HIV prevention and treatment. Curr HIV/AIDS Rep. 2005;2:194–9. doi: 10.1007/s11904-005-0016-4. [DOI] [PubMed] [Google Scholar]
- 32.Page-Shafer K, Hahn JA, Lum PJ, Ochoa K, Graves A, Moss A. Prevalence and correlates of HIV infection among young injection drug users in San Francisco. J Acquir Immune Defic Syndr. 2002;31:422–31. doi: 10.1097/00126334-200212010-00009. [DOI] [PubMed] [Google Scholar]
- 33.Kral AH, Lorvick J, Ciccarone D, et al. HIV prevalence and risk behaviors among men who have sex with men and inject drugs in San Francisco. J Urban Health. 2005;82:i43–50. doi: 10.1093/jurban/jti023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bacon O, Lum P, Hahn J, et al. Commercial sex work and risk of HIV infection among young drug-injecting men who have sex with men in San Francisco. Sex Transm Dis. 2006;33:228–34. doi: 10.1097/01.olq.0000204914.91923.ad. [DOI] [PubMed] [Google Scholar]
- 35.Brecht ML, O'Brien A, von Mayrhauser C, Anglin MD. Methamphetamine use behaviors and gender differences. Addict Behav. 2004;29:89–106. doi: 10.1016/s0306-4603(03)00082-0. [DOI] [PubMed] [Google Scholar]
- 36.Davidson PJ, McLean RL, Kral AH, Gleghorn AA, Edlin BR, Moss AR. Fatal heroin-related overdose in San Francisco, 1997 – 2000: a case for targeted intervention. J Urban Health. 2003;80:261–73. doi: 10.1093/jurban/jtg029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tyndall MW, Craib KJ, Currie S, Li K, O'Shaughnessy MV, Schechter MT. Impact of HIV infection on mortality in a cohort of injection drug users. J Acquir Immune Defic Syndr. 2001;28:351–7. doi: 10.1097/00126334-200112010-00008. [DOI] [PubMed] [Google Scholar]
- 38.Bogart LM, Kral AH, Scott A, et al. Sexual risk among injection drug users recruited from syringe exchange programs in California. Sex Transm Dis. 2005;32:27–34. doi: 10.1097/01.olq.0000148294.83012.d0. [DOI] [PubMed] [Google Scholar]
- 39.Lorvick J, Martinez A, Gee L, Kral AH. Sexual and injection risk among women who inject methamphetamine in San Francisco. J Urban Health. 2006;83:497–505. doi: 10.1007/s11524-006-9039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]