Abstract
Objectives
Occupational exposure to aromatic solvents causes many serious health hazards to workers, especially if an ambient environment increases the exposure during routine working hours. This study was conducted on two related groups, i.e., automobile mechanics (MCs) and automobile spray painters (PNs), with an effort to analyze effects of chemical exposure on hematological parameters, keeping a focus on environmental parameters and workers’ personal behavioral characteristics that could be held responsible for increasing exposure risk.
Methods
A preliminary survey of various chemicals used in these places was done, and 78 blood samples were collected from three groups (control, n = 24; mechanics, n = 25; painters, n = 29). Demographic features of workers were recorded through a short questionnaire.
Results
Results showed that mean red blood cell (RBC) count was lower both in MCs [t(51) = 2.38, p < 0.021, r = 0.32] and in PNs [t(47) = 2.12, p < 0.03, r = 0.29], whereas mean hemoglobin (Hb) was significantly lower in MCs [t(51) = 2.5, p = 0.017, r = 0.33]. Combined data for exposed groups for smokers (SMs) versus nonsmokers (NSs) showed that SMs had a significantly lower number (RBC count: t(52) = 2.28, p < 0.027, r = 0.25; Hb count: t(52) = 2.71, p < 0.009, r = 0.30] of these parameters than NSs, even compared to the control group. Moreover, logistic regression results showed that smoking is a significant predictor of reduction in RBC and Hb counts, besides occupational exposure and work experience to a little extent among exposed workers. Mean white blood cell count [t(47) = 2.63, p < 0.01, r=0.35], mean corpuscle volume [t(47)= –2.82, p = 0.007, r = 0.29], and packed cell volume [t(47)= –2.28, p = 0.027, r = 31] were higher exclusively in painters, which could be related to exposure to benzene in addition to isocyanate.
Conclusion
It appeared that workplace exposure may be complex due to interaction of multiple factors and PNs face much more exposure to isocyanate and aromatic solvents than MCs, which had significant effects on their hematopoiesis. Smoking enhances exposure risk manifolds, and among MCs it showed combined effects along with occupational exposure. There is a need to create awareness among these workers to adopt self-safety measures during routine tasks and also of a separate study to elucidate actual occupational exposure among them, eliminating confounding factors.
Keywords: benzene, car mechanics, hematological parameters, hemoglobin, isocyanate, red blood cell, white blood cell
1. Introduction
In many occupational settings, the ambient environment is a sink of various contaminants that emerge from point and nonpoint sources and causes direct exposure to workers. Such exposures in petroleum-related occupations usually result from routine transportation, distribution, accidental spills, improper handling and use, and leaching of petroleum hydrocarbons products; there are also many other ways by which humans are exposed to these chemicals [1]. Many of the aromatic organic solvents, such as toluene, ethyl benzene, xylene, etc., are common components of petroleum products, most of which have already been confirmed as carcinogens, e.g., benzene [2-4]. Benzene is considered to be one of the possible causes of morbidities among automobile workshop mechanics as well as in automobile painters [5]. Among many other environmental sources, benzene mostly arises from fuel vapors and gasoline (range, 1.8–3.7%) and from solvents used for degreasing or as diluents at work areas of automobile mechanics [6]. Most exposures to organic solvents occur during the maintenance of various engine parts [7]. Such solvents, after being absorbed into the intercellular fluid, may enter main bloodstream and get distributed throughout the body [8]. Benzene affects blood production by affecting the bone marrow. In Korean industries, an excessive risk of hematopoietic diseases because of relatively high past exposure to benzene has been reported [9]. Apart from direct occupational exposure, nonoccupational population around chemical factories and other occupational sites may also undergo indirect exposure [10]. Thus, occupational exposure hematotoxicity [11] and other blood disorders such as blood cancer (leukemia), aplastic anemia, and dysplastic bone marrow conditions are common results of exposure to aromatics such as benzene [12], screening of which can be done easily by complete blood counts.
Thousands of workers in Pakistan are routinely exposed to such chemicals, but no such data are available due to lack of proper reporting [13]. Even local people who do not have any direct occupational exposure to chemicals may get exposed to varying levels of benzene from the ambient environment [14]. Exposure studies are the most important steps toward identification and prevention of multiple risks that vary with occupational categories and job responsibilities. Many studies [15] have used demographic features such as age, gender, body mass index (BMI), smoking status, and consumption of certain types of contaminated food in exposure assessments. It is necessary to keep these features in focus while setting rules and regulations for potential hazardous occupations, which can be helpful in minimizing health risks. In developing countries such as Pakistan, creating awareness among workers about workplace chemicals and other related hazards should also be given priority. There should be thorough hazard assessments at a large scale to review occupational safety conditions at the initial stage, and practical measures should be taken to minimize them in future. This study was planned to evaluate the effects of continuous exposure to solvents, chemical contaminants, and other confounding factors that may cause functional changes in blood parameters. It may be helpful in future for suggesting the most significant priorities in the light of research outcomes, to minimize workplace- and occupation-related health risks, and to ensure safety to workers’ health.
2. Materials and Methods
2.1. Sampling sites
Sampling was done at random at the visited study areas among car mechanics (MCs, n = 29), including diesel-engine mechanics, motor-truck mechanics, engine-repair mechanics, differential and brakes repairers, general automobile-service-station mechanics, workshop heads, and apprentices, and car spray painters (PNs, n = 25). Task reportedly performed by MCs included engine repair, oil changing, lubrication, basic maintenance of fuel systems, etc. and that by PNs were denting, abrading, cleaning, adjusting, aligning, assembling and disassembling, brushing, burning, cementing, chipping, fastening, filling, finishing, fitting, hammering, maintaining, pressing, repairing, sanding, scraping, soldering, and spraying, apart from painting task. Participants for an age-matched control group (CN, n = 24) were selected from nonchemical-related occupations of the same city. Selection criteria were age of >25 years and work experience of >2 years. Personal data of each participant were collected through short interviews using a questionnaire mainly based on multiple-choice questions. Major focus of the questionnaire was on demographic information of interviewees, such as height, age, BMI, education level, overall health, workplace environmental hygiene, socioeconomic status, smoking status, nature of job, work experience, and work hours, as well as on selfreported health and whether the interviewees suffer from any symptoms due to their occupation (Figures 1 and 2, Table 1).
Figure 1. Car mechanics at work.

Figure 2. Poor hygiene at a typical car mechanical workshop.

Table 1.
Personal characteristics of individuals in exposed groups (mechanics and painters) versus control group
| Parameters | Painters | Mechanics | Control | pa | pb |
|---|---|---|---|---|---|
| Age (y)c | 29.4 (27–31) | 31.34 (27.50–36.5) | 29.21 (27–31) | 0.88d | 0.38d |
| Height (cm)c | 175.7 (168–178.8) | 168 (164.4–178.2) | 171.6 (165.6–170.4) | 0.20d | 0.16d |
| Weight (kg)c | 60.76 (57–63.5) | 59.37 (54.5–63.5) | 59.50 (56–62.75) | 0.48e | 0.94e |
| BMI (kg/m2)c | 20.77 (17.8–25.8) | 21.78 (18.40–25.40) | 21.09 (14.60–29.60) | 0.88d | 0.92d |
| Work experiencec | 5.64 (4–7) | 6.34 (3–8) | 5.13 (3–6.7) | 0.45d | 0.37d |
| Daly work hours | 8.72 (8–8.0) | 8.44 (8.0–8.5) | 8.20 (8.0–8) | 0.25d | 0.52d |
| Smoking statusc | No 13 (52) | No 9 (31.5) | No 12 (50) | 0.20f | 0.50f |
| Yes 12 (48) | Yes 20 (68.5) | Yes 12 (50) | χ2 1.510 | χ2 .178 | |
| Headacheg | Never 3 (12) | Never 19 (65.5) | Never 21 (87.5) | ˂0.01f,* | 0.16f |
| Sometimes14 (56) | Sometimes 9 (31) | Sometimes 3 (12.5) | χ2 28.6 | χ2 3.66 | |
| Often 8 (32 ) | Often 1 (3.5) | Often 0 (0) | |||
| Nauseag | Never 15 (60) | Never 27 (93.1) | Never 23 (95.8) | ˂0.01f * | 0.57f |
| Sometimes 6 (24) | Sometimes 2 (6.9) | Sometimes 1 (4.2) | χ2 9.24 | χ2 0.67 | |
| Often 4 (16 ) | Often 0 (0 ) | Often 0 (0 ) | |||
| Education levelg | 0.01f,* | ˂0.01f,* | |||
| Under-primary | 12 (48) | 18 (62.07) | 4 (16.67) | χ2 9.13 | χ2 14.8 |
| Primary | 13 (52) | 11 (37.93) | 15 (62.5) | ||
| Secondary | 0 (0) | 0 (0) | 5 (20.83) | ||
aControl versus painters; bControl versus mechanics; cMean (25th–75th); dWilcoxon signed ranks test; eWelch test; fChi-square (χ2 ) test value; gFrequency(percent out of total).
*Significant at p ˂ 0.05. BMI = body mass index.
2.2. Sample collection and analysis
Samples were collected from workers willing to participate in this study during their routine work hours. About 3–4 mL venous blood from the antecubital vein of each participant was taken with the help of a 10-mL disposable plastic syringe and immediately transferred to a sterile vacutainer, containing potassium–EDTA anticoagulant. All samples were analyzed in the most immediate time. Analyses of selected parameters were performed using whole blood (approximately 50 μL automated) on digital Sysmex, an automated hematology analyzer (KX-21). Reagents used were diluents, a lytic reagent (500 mL), and an enzyme cleaner (2 × 50 mL). Systems were used to measure red blood cells (RBCs, in × 106/μL), white blood cells (WBCs, in × 106/μL), platelet counts (PCs, in × 106/μL), hemoglobin (Hb, in g/dL), packed cell volume (PCV, in %), and mean corpuscle volume (MCV, in ft).
2.3. Statistical analysis
The SPSS version 13 and Microsoft excel software were used for statistical analyses. The Student t test, Wilcoxon signed ranks test, and Welch tests were used for paired analysis to test the statistical significance difference of selected parameters among studied population, keeping in focus the assumption of parametric tests. The effect size (r) was calculated using t statistic values and (df) where applicable. The Chi-square test was used to compare the proportions of categorical variables. Stepwise regression analysis was used assuming blood parameters as dependent variables and personal features, behavioral characteristics, and jobrelated parameters as independent variables. A p value of <0.05 was considered statistically significant.
2.4. Ethics
The project was reviewed and approved by the ethical review committee of Quaid-i-Azam University, Islamabad, Pakistan. Only those individuals were recruited who were willing to participate and were clearly informed about the purpose of investigations and expected outcomes. All participants signed the written consent form. Sampling and logistic support for this research was granted by the ethical review committee of the university in collaboration with the Volunteer’s Social Welfare Organization (VSWO) (registered under Social Welfare Act 1961, Pakistan).
3. Results
3.1. Demographic characteristics of respondents
All male participants from exposed groups (MCs and PNs) and the unexposed (CN) group generally had a normal BMI level, and were of almost the same age, height, and weight (Table 1). Samples from occupationally exposed workers were collected during their routine hours, and none was found to be equipped with any type of self-protective equipment. Workers in the study groups (mechanics of automobile repair shops and painters) had poor socioeconomic backgrounds and very low levels of education. Most of them were not very aware of chemical-related hazards. Most of the painting workshops were situated amid or beside mechanical and spare-part workshops. Apart from petroleum products, materials used in a typical painting shop, e.g., diluents, binder, thinner, hardener, etc. contained chemicals such as isocyanate, and benzene and its derivatives such as toluene. However, in the mechanical workshops, the main contaminants included kerosene oil, petroleum products, and crude oil, and major contamination of workplaces and workers’ body parts was from the used gasoline engine oil. The smell of chemicals was unavoidable, and according to participants, despite wrapping clothing around the noses (self-made mask), it was a cause of severe headache and nausea, more specifically for spray-paint workers. Odor or smell from solvents may arise from volatile organic compounds (VOCs) used as tinting pigments and solvents that help stabilize the dispersion.
3.2. Laboratory data analysis
Laboratory data showed that RBC count was much lower in PNs (4.84 ± 0.5) than in CN group (5.12 ± 0.4), and this difference was significant [t(47) = 2.12, p = 0.03, r = 0.29]; similarly, difference was recorded for MCs [4.75 ± 0.7, t(51) = 2.38, p = 0.021, r = 0.32]. Mean WBC counts were slightly higher in both PNs and MCs, but for the difference in WBC counts between PNs and CN group was larger (5.73 ± 1.1) and significant [t(47)=–2.63, p = 0.01, r = 0.35] than that between MCs and CN group. Mean Hb values were lower in both PNs and MCs than in CN group, and the difference in Hb values between PNs and MCs (14.82 ± 0.5, 14.7 ± 0.6) was greater and significant as compared to CN group [t(47) = 2.09, p = 0.042, r = 29, and t(51)=2.5, p=0.01, r=0.33 for PNs and MCs, respectively]. Mean MCV and PCV recorded were higher only in PNs than in CN group, which was significant [t(47) = –2.82, p < 0.01, r = 0.29 and t(47) = –2.28, p = 0.027, r = 31, respectively]. Combined data of both exposed groups (PNs and MCs) showed significant differences for RBC count (lower as compared to CN group) [t(76) = 2.42, r = 0.27, p=0.018], Hb count [t(76)=2.73, r=0.30, p < 0.01], and PCV [t(76) = –2.31, r = 0.26, p = 0.028]. Differences in other parameters were nonsignificant (Table 2). When exposed individuals were divided into smokers (SMs) and nonsmokers (NSs), it appeared that RBC count was significantly lower among exposed SMs as compared to exposed NSs [t(52) = 2.28, p = 0.027, r = 0.25] and also mean Hb value was much lower among SMs than among NSs from exposed groups (combined data) [t(52) = 2.71, p < 0.01, r = 0.30] (Table 3).
Table 2.
Comparison of hematological parameters (exposed groups vs. control group)
| Parameters | Painters | Mechanics | All exposed | Control | pa | pb | pc |
|---|---|---|---|---|---|---|---|
| RBCd (×106/μL ) | 4.84 ± 0.5 | 4.75 ± 0.7 | 4.77 ± 0.61 | 5.12 ± 0.4 | 0.039* | 0.021* | 0.018* |
| 4.61–5.06 | 4.50–5.01 | 4.62–4.96 | 4.96–5.3 | ||||
| WBCd (×103/μL) | 5.73 ± 1.1 | 5.2 ± 1 | 5.47 ± 1.03 | 5.07 ± 0.7 | 0.011* | 0.51 | 0.09 |
| 5.30–6.17 | 4.9–5.6 | 5.18–5.7 | 4.80–5.3 | ||||
| PLT (103/μL) | 230.8 ± 30.9 | 219.2 ± 26.1 | 224.37 ± 29 | 220 ± 27 | 0.19 | 0.90 | 0.51 |
| 218–244 | 209.3–229.1 | 216.7–232.4 | 208.8–231.3 | ||||
| Hbd (g/dL) | 14.82 ± 0.5 | 14.7 ± 0.6 | 14. ± 0.6 | 15.21 ± 0.7 | 0.042* | 0.017* | <0.01* |
| 14.6–15.1 | 14.5–15 | 14.6–14.9 | 14.90–15.5 | ||||
| MCVd (fL) | 95.56 ± 3.8 | 93.6 ± 5.2 | 94.45 ± 4.7 | 92.2 ± 4.5 | <0.01* | 0.32 | 0.049 |
| 93.9–97.1 | 91.6–95.5 | 93.2–95.8 | 90.3–94.1 | ||||
| PCVd (%) | 47.01 ± 2.9 | 46.72 ± 3.1 | 46.86 ± 2.97 | 45.34 ± 4.2 | 0.027* | 0.073 | 0.028* |
| 45.83–48.2 | 45.5–47.9 | 46.1–47.7 | 44.41–46.3 | ||||
aControl versus painters; bControl versus mechanics; cControl versus all exposed; dResults are (mean ± standard deviation)/95% CI.
*Significant at p < 0.05. CI = confidence interval; Hb = hemoglobin; MCV = mean corpuscle volume; PCV = packed cell volume; PLT = platelet; RBC = red blood cell; WBC = white blood cell.
Table 3.
Comparison of hematological parameters among SMs and NSs
| Parameters | Exposed groups (n = 54) | All (n = 78) | ||||
|---|---|---|---|---|---|---|
| SMs | NSs | pa | SMs | NSs | pa | |
| RBCc (×106/μL ) | 4.65 ± 0.58 | 5.02 ± 0.60 | 0.027* | 4.76 ± 0.58 | 5.07 ± 0.49 | 0.01* |
| 4.43–4.85 | 4.74–5.28 | 4.58–4.94 | 4.89–5.24 | |||
| WBCc (×103/μL) | 5.51 ± 0.97 | 5.38 ± 1.13 | 0.65 | 5.43 ± 0.91 | 5.23 ± 0.97 | 0.36 |
| 5.16–5.86 | 4.88–5.89 | 5.15–5.71 | 4.89–5.57 | |||
| PLTc (103/μL) | 229.3 ± 27.8 | 217.7 ± 29.4 | 0.14 | 223.6 ± 27.3 | 218.7 ± 28.6 | 0.21 |
| 219.3–239.3 | 204.7–230.8 | 218.3–234.9 | 208.7–228.7 | |||
| Hbc (g/dL) | 14.61 ± 0.59 | 15.03 ± 0.51 | <0.01* | 14.71 ± 0.66 | 15.17 ± 0.56 | <0.01* |
| 14.39–14.8 | 14.80–15.26 | 14.5–14.9 | 14.97–15.36 | |||
| MCVc (fL) | 93.9 ± 5.04 | 95.31 ± 4.06 | 0.28 | 93.25 ± 5.07 | 94.47 ± 4.22 | 0.26 |
| 92.1–95.72 | 93.51–97.11 | 91.7–94.8 | 92.99–95.94 | |||
| PCVc (%) | 46.64 ± 2.85 | 47.18 ± 3.17 | 0.51 | 46.20 ± 2.6 | 46.63 ± 3.03 | 0.50 |
| 45.61–47.7 | 45.77–48.59 | 45.39–47.02 | 45.57–47.69 | |||
aSMs versus NSs, from exposed group; bSMs versus NSs, out of total data; cResults are (mean ± standard deviation)/95% CI.
*Significant at p < 0.05. CI = confidence interval; Hb = hemoglobin; MCV = mean corpuscle volume; NS = nonsmoker; PCV = packed cell volume; PLT = platelet; RBC = red blood cell; SM = smoker; WBC = white blood cell.
When all data were subjected to categorical analysis for SMs and NSs, more significant results were recorded, i.e. [t(76) = 2.44, r = 0.26, p < 0.01] and p < 0.002, [t(76) = 3.14, p < 0.01, r = 0.33], for RBC and Hb counts, among SMs and NSs respectively (Table 3).
3.3. Logistic regression analysis
All blood parameters of exposed workers (combined) were also subjected to logistic regression analyses; each blood parameter was considered as a dependent variable, while age, work hour, work experience, smoking status, etc. were entered in stepwise regression analyses as independent variables. Of all blood parameters, the most significant predictors of decrease in hemoglobin and RBC counts were found to be smoking [F(2, 75) = 9.49, p < 0.01, R2 = 0.20 and F(2, 75) = 5.91, R2 = 0.13, p = 0.019 for Hb and RBC, respectively] and work experience [F(2, 75) = 9.49, p < 0.01, R2 = 0.20 and F(2, 75) = 5.91, R2 = 0.13, p = 0.02 for Hb and RBC, respectively] (Table 4). Smoking was found to be the most significant predictor of decreased Hb and RBC counts, which shows that among SMs risks of decrease in the Hb and RBC counts amount to 0.43 and 0.29 units, respectively, per unit increase in smoking, after adjusting for each year of work experience (p = 0.04).
Table 4.
Logistic regression analysis for predictor variables (work experience, smoking, and work hours) and outcome variables (RBC, Hb, and PCs).
| B | Standard error (B) | β | Sig. | R2 | 95% confidence | interval of B | |
|---|---|---|---|---|---|---|---|
| Hb counta | |||||||
| Constant | 15.95 | 0.253 | 0.202* | Lower bound | Upper bound | ||
| Years spent in job | –0.063 | 0.022 | –0.295 | 0.006 | –0.108 | –0.019 | |
| Smoking | –0.430 | 0.137 | –0.324 | 0.002 | –0.704 | –0.157 | |
| RBC counta | |||||||
| Constant | 5.62 | 0.225 | 0.136* | ||||
| Years spent in job | –0.046 | 0.020 | –0.252 | 0.022 | –0.086 | –0.007 | |
| smoking | –0.292 | 0.122 | –0.257 | 0.019 | –0.535 | –0.049 | |
| PCa | |||||||
| Constant | 185.1 | 18.41 | 0.055 | ||||
| Work hours per day | 4.49 | 2.15 | 0.233 | 0.040 | 0.218 | 8.761 | |
aDependent variables.
*p <0.05. Hb = hemoglobin; PC = platelet count; RBC = red blood cell.
4. Discussion
In the present work, effects of complex aromatic mixture of solvents on blood parameters were studied for the first time in Pakistan; so far, no published data could be found on this subject. Influence of workplace environments on the extent of exposure and behavioral characteristics were also focused on among a selected occupational population. In Pakistan, workers’ safety and surveillance setup is a neglected subject. Despite a massive search, we could not find the guidelines for permissible exposure limits set by health authorities in Pakistan. People in such occupations are incapable of spending much for the betterment of self-health, neither does the government facilitate heath care; they bear poor socioeconomic status although they appeared physically healthy. In general, the poor do not seem to have a hazard-free future from a health perspective, especially in their workplaces. Almost all the participants in our study were found to be working without any proper personal protective equipment (Figures 1-3). In this study, the limited number of participants shows the difficulty in convincing people to participate and also in finding individuals who could meet the selection criteria. In our study, we found that most of the solvents used by both automobile MCs and PNs had benzene or its derivatives/by-products, and, apart from benzene constituents, participants reported the symptoms of isocyanate exposure, which was an important chemical in paint materials.
Figure 3. Mechanical workshops situated among congested residential areas.

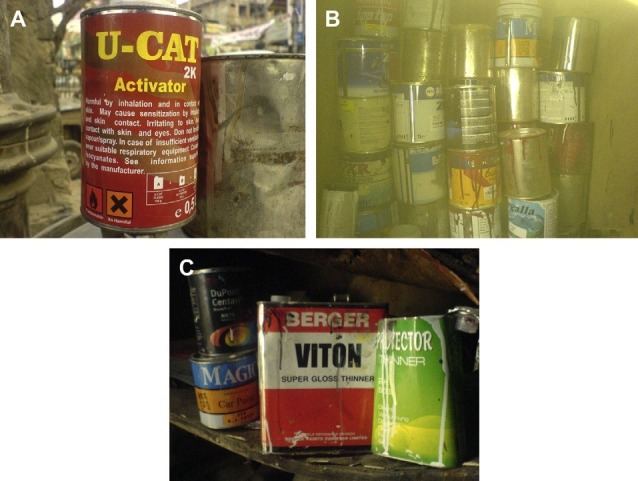
Our results showed some significant effects of occupational exposure, especially along with other confounding factors such as smoking- and job-related parameters. The present study also revealed that most of painting sites visited were adjacent to or near automobile repair shops, and painting occupations gave more exposure to inhalable chemicals such as isocyanate and aromatic aerosol. Our participants from painting occupation had significantly higher MCV [t(47) = –2.82, p = 0.007, r = 0.29]; mean Hb values were lower in both PNs and MCs, than in the CN group. Increased MCV may be an indication of the effects on liver and that of pernicious anemia [16]); in this case, it may be due to an aromatic exposure in this occupational group. Many studies have reported an association between benzene exposure and higher values of MCV [17-19], and our study results are in accordance with it. Many reports have shown that exposed populations had decreased hemoglobin levels [18-21]. In our study, we observed that most of the painting sites were amid or beside mechanical workstations, and workers reported episodes of headache during spray-painting tasks. Headache symptoms and nausea were more common among PNs because of inhalation of VOCs despite using self-made masks. Release of isocyanate vapors during spray painting is the most common cause of nausea, headache, and also respiratory tract irritation [22]. It is suggested in some studies that benzene concentration (and some other aromatics) is more likely to increase in blood of PNs and paint manufacturing workers, when concentrations of such chemicals in air exceed normal limits [23]. That is probably due to improper or poor displacement of indoor air with the influx of fresh air. Other studies have shown that benzene is absorbed mainly through skin and lungs; after being distributed into the tissues, benzene in the blood remains in equilibrium with that in expired air [24]. Data presented in this work suggest that, although automobile MCs do face exposure to several solvents during various maintenance tasks, they are relatively much less exposed to organic solvents than PNs. A scarce use of selfprotective equipment further enhances the risk of exposure to inhalable volatile chemicals (such as aromatic and isocyanate vapors) via both dermal and inhalatory routes of absorption. It seemed that PNs get more exposure to the solvents and VOCs as compared to MCs. Most common components of thinner hardeners and diluents include benzene, toluene, and isocyanate, which we also observed in our visited sites shown in Figures 4A–C. It is also suggested by Aksoy [25] that commonly used paint solvents and thinners may have a benzene content up to 70%; another study by Beving et al [7] had shown, in a comparison between MCs and PNs, that PNs were more exposed to organic solvents used in car spray-painting tasks. It inferred that PNs generally have to face more exposure to inhalable chemicals as compared with MCs, especially if air circulation is poor enough to minimize the burden of chemical vapors.
Figure 4. (A–C) Different chemical containers used in automobile spray painting.
Mean Hb values were lower in both PNs and MCs than in the CN group, and the difference between MCs and the CN group was greater and more significant than that between the PNs and the CN group (r = 0.33, p = 0.017 for MCs). RBC count was much lower in MCs than in CN group, and this difference was significant (p < 0.03, r = 0.29); similarly, more significant difference was recorded for MCs (p=0.021, r=0.32). This in our opinion is partly due to benzene exposure, because research in this field has shown an association between benzene exposure and lowering of RBC counts [20,26-28]. Some others, such as Marieb [29], showed an overall negative association of exposure of hydrocarbons, including benzene, to humans with adverse effects on spleen and lymph. Aromatic hydrocarbons such as benzene are common components of gasoline, which account for most of the occupational exposures; other components may be aliphatic and many unsaturated or saturated hydrocarbons [30-32]. Waste crankcase oil contains toxicants in which aromatic hydrocarbons may be 30%, among which toluene, benzene, xylene, and ethyl benzenes are common. The amount of organic and inorganic compounds present apart from other metallic additives is large [2-4]. Exposure to benzene is known to cause very harmful effects on human health [33,34].
It is obvious that exposure to aromatic solvents is more likely possible for MCs; petroleum products that they routinely encounter in their workplaces are reported, in many studies, to be toxic to various human organs, including vital organs, and are also responsible for carcinogenesis, toxicity to immune system, genotoxicity, etc. among many consequences [18,35-37].
We found smoking an important confounding factor as we divided all participants into SMs and NSs. Combined data of both exposed groups also showed decreased mean RBC and Hb counts, with effect sizes of 0.27 and 0.30, respectively, as the consequences of smoking; these outcomes were obtained from split data of control individuals (Tables 2 and 3).
Smoking and exposure to cigarette smoke are important causes of direct exposure to benzene [38]. It may be an indication that smoking not only enhances exposure in occupational environments but may also have exclusive effects on hematopoiesis. Our logistic regression results of combined data from exposed participants also highlighted that changes in Hb and RBC counts could significantly be predicted by smoking, which confirmed our previous assessment. Regression analysis also confirmed that Hb and RBC counts were significantly different in SMs, accounting for –0.430 and –0.292 units of decrease in Hb and RBC counts, respectively, per unit increase in smoking frequency after adjusting for work experience. It seems that workers with longer exposure have more adverse effects on blood chemistry, which are enhanced if they are SMs also. Risk from cigarette smoke remains almost equal for individuals with both active and passive smoking [39]. Smoking is a behavior that is commonly dependent on socioeconomic status of an individual, apart from their behavioral priorities. Smoking is the most common addition nowadays worldwide. In Pakistan, Ali et al [40] concluded that sociodemographic factors could be associated with tobacco smoking among adult males in 55% active SMs, with a good awareness regarding harmful effects of smoking habit, and they also found that smoking increased with increase in age and income. Although in the present work, the overall income status of workers in two occupations was low, it is suggested that smoking habits in the current study seem to have an association with poor socioeconomic status, which may be because people with lower education and selected occupations are commonly diverted to the most ubiquitous addiction of smoking.
Slightly increased PCs and WBC counts were observed in exposed individuals (more specifically in PNs), although it was not much substantial in case of PCs. However, such increase in platelet is unusual; previous studies [18,21]) showed a negative association of such exposure with platelets along with other parameters. This increase in PCs may possibly be an indication of certain type of anemia [16]. WBCs, like other blood parameters, change under abnormal conditions; in some diseases their number increases in the blood, mostly in acute infections and leukemia [16]. In our opinion, this unusual increase may also be due to certain inflammatory and infectious conditions because an essential function of WBCs is to provide primary defense. There are two reasonable and convincing possibilities for these increased parameters: exposure to isocyanate and outcome of smoking. WBC counts among SMs in both control and exposed individuals were more than among NSs. These results remain in accordance with previous research works that WBCs are found elevated among current participants; even the total WBC count in SMs in previous studies was 27% higher than in those who never smoked, in both genders [41-43]. According to Tell et al (1985) [43], this WBC count in SMs may also be due to chronic lung disease such as inflammation, more specifically in chronic SMs and that for PCs may be due to chemicals in cigarettes which might have induced increased production of WBCs and platelet cells. Considering the case of PNs in our study (Table 2), WBC counts were significantly different from the control group; the possible explanation is that such inflammation may be due to isocyanate that we found in high concentrations in painting materials. Isocyanate is known to have very harmful effects on the lungs and respiratory systems [44]. The routes for absorption of isocyanate are still the skin and lungs; isocyanate is a potential hazard in the form of released vapors, is inhalable during spray painting, and may cause eye irritation; other symptoms are nausea, headache, and respiratory tract irritation [22]. Some of these symptoms, such as headache, were significantly higher among our painting group individuals (Table 1). According to Glantz and William [42], even passive smoking may increase platelet activity, atherosclerotic lesions, and tissue damage, and it along with other confounding factors may lead to cardiac disorders. This explanation points out an important fact that individuals who may not be chronic SMs themselves but work at the same site where SMs work may be exposed to cigarette smoking as passive SMs, therefore they may also show an increase in their related blood parameters, as our results have shown.
Differences in blood parameters such as RBC and Hb counts show some levels of occupational exposure very clearly and that of work-related parameters. Because a decline in Hb and RBC counts was also predicted by work experience [F (2, 75) = 9.49, p = 0.05, R2 = 0.20 and F(2, 75) = 5.91, R2 = 0.13, p < 0.01, respectively] taking smoking constant (Table 3), these findings are in agreement with those of early exposure studies that have shown that morbidities such as hematotoxicity, genotoxicity and acute melogenous leukemia are enhanced due to long exposure [45-47] and also other effects were reported under long exposure [48,49]. Thus, routine work hours increase benzene uptake [38]. According to Foo [14], 8-hour time-weighted averages of automobile MCs’ exposure levels ranged from 0.014 to 1.7 ppm. Our findings also corroborate with that of Kirkeleit et al [50] that despite proper use of selfprotective equipment and low exposure to benzene, internal uptake of benzene by workers remains high over long working hours.
It is obviously difficult to separate actual occupational exposure, which is often disguised by many other behavioral and environmental factors, and as suggested by previous studies such as those of Brugnone et al [38], actual environmental exposures to benzene and the extent of true workplace exposure have always been a hindrance for researchers, and even difficult when exposure is at a very low level. These results also clearly show that factors that enhance or disguise the actual occupational exposure may be considered as potential hazard factors for the general population, especially those who dwell in the surroundings of such occupational sites (Figure 3). Therefore, our results showed that level of contaminants in blood due to occupational exposure is influenced by multiple factors, all or most of which show considerable associations.
5. Conclusions and Recommendations
Good ventilation at workplaces ensures lower concentrations of benzene and other vapor-phase chemicals than poor ventilation. Poor ventilation, as defined by Liu et al [51], may be due to a low level of exhaust system or no exhaust at all which relies merely on natural ventilation. It is conclusive to suppose that more inhalable particles emerge around painting sites, and PNs may have low levels of dermal contact when using protective equipment; therefore, it is opined that most of the aerosols are inhaled by PNs at worksites. EPA guidelines [52] suggest that chemicals such as benzene at painting booths should be monitored for keeping exposure level minimum; for example, at paint sites air flow may be 8000 m3/h with a paint application rate of 2 L/h or air flow exhaust may also be 10,000 m3/h with a paint application rate of 2 L/h, in which maximum pollutant content (benzene) of paint equals 2.5% v/v. In our study, we found no rules and regulations regarding worker’s safety being practiced at any visited site; it appears reasonable to conclude that poor ventilation status at work areas seems to increase risks of exposure many times, since the release of chemicals into congested work areas seems to exceed the its rate of removal from there. On the basis of its results, the most important conclusion that this study has drawn deals with the hazardous occupational environments in Pakistan; hygiene conditions in such setups are potential exposure factors and risks to workers’ health, and workers’ knowledge regarding safety of the workplace and chemicals is insufficient. Exposure to a complex mixture of solvents, especially aromatics such as benzene and others such as isocyanate, may lead to serious hematological disturbance when there is a low standard of hygiene and lack of personal protective equipment usage in the workplace. Further study is needed to investigate the exclusive impacts of occupational environment and smoking on workers’ health. However, MCs contact with body parts of automobile engines, and handling tools etc. smear most of the body parts with petrochemical fractions. There must be a regular use of coveralls and gloves. It can be suggested that if workplace hygiene is properly maintained and workers’ exposure time is reduced by minimizing the working hours, exposure risks can be minimized significantly.
References
- 1.Tang X, Eke PE, Scholz M, et al. Processes impacting on benzene removal in vertical-flow constructed wetlands. Bioresour Technol. 2008;100:227–34. doi: 10.1016/j.biortech.2008.05.038. [DOI] [PubMed] [Google Scholar]
- 2.Irwin RJ, Van-Mouwerik M, Stevens L, et al. Environmental contaminants encyclopedia. National Park Service, Water Resources Division; Fort Collins, CO: 1998. [Distributed within the Federal Government as an Electronic Document, 1997 (Projected public availability on the internet or NTIS).] [Google Scholar]
- 3.Canadian Environmental Protection Agency. Priority substances list assessment report: waste crankcase oils. NTIS; 1994. [Google Scholar]
- 4.Vermont Agency of Natural Resources Department of Environmental Conservation. Vermont Used Oil Analysis and Waste Oil Furnace Emissions Study. Environmental Protection Agency Control Technology Center RTP; North Carolina: 1994. p. 27711. [Google Scholar]
- 5.KOSHA; [Google Scholar]
- 6.Vitali M, Ensabella F, Stella D, Guidotti M. Exposure to organic solvents among handicraft car painters: A pilot study in Italy. Ind Health. 2006;44:310–7. doi: 10.2486/indhealth.44.310. [DOI] [PubMed] [Google Scholar]
- 7.Beving H, Ternling G, Olssen P. Increased erythrocyte volume in car repair painters and car mechanics. Br J Ind Med. 1991;48:499–501. doi: 10.1136/oem.48.7.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koz1owska K, Polkowska1 Z, Przyjazny A, et al. Analytical procedures used in examining human urine samples. Pol J Environ Stud. 2003;12(5):503–21. [Google Scholar]
- 9.Kang SK, Lee MY, Kim TK, et al. Occupational exposure to benzene in South Korea. Chem Biol Interact. 2005;153-4:65–74. doi: 10.1016/j.cbi.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Cerna M, Kratenova J, Zejglicova K, et al. Levels of PCDDs, PCDFs, and PCBs in the blood of the non-occupationally exposed residents living in the vicinity of a chemical plant in the Czech Republic. Chemosphere. 2007;67:238–46. doi: 10.1016/j.chemosphere.2006.05.104. [DOI] [PubMed] [Google Scholar]
- 11.IARC (International Agency for Research on Cancer). Benzene. In: IARC Monographs on the evaluation of carcinogenic risks to humans. Some industrial chemicals and dyestuffs, vol. 29. IARC Press; Lyon, France: 1982. pp. 93–148. [Google Scholar]
- 12.Snyder R. Issues in risk assessment of chemicals of concern to department of defense and agencies session. Drug Chem Toxicol. 2000;23(1):13–25. doi: 10.1081/dct-100100099. [DOI] [PubMed] [Google Scholar]
- 13.Kamal A. Comparison of blood benzene and naphthalene levels as indicator of occupational exposure among car-mechanics and car-spray painters in Rawalpindi. PMAS-AAUR; 2010. p. 78. Unpublished M. Phil thesis. [Google Scholar]
- 14.Foo SC. Benzene pollution from gasoline usage. Sci Total Environ. 1991;103(1):19–26. doi: 10.1016/0048-9697(91)90349-j. [DOI] [PubMed] [Google Scholar]
- 15.Lee CC, Lin WT, Liao PC, et al. High average daily intake of PCDD/Fs and serum levels in residents living near a deserted factory producing pentachlorophenol (PCP) in Taiwan: influence of contaminated fish consumption. Environ Pollut. 2006;141:381–6. doi: 10.1016/j.envpol.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 16.John W, Hole J. Essentials of human anatomy and physiology. 4th ed. Wm. C. Brown Publisher; USA: 1992. [Google Scholar]
- 17.Bogadi-Sare A, Turk R, Karacic V, et al. Red blood cell glycerol lysis and hematological effects in occupational benzene exposure. Toxicol Ind Health. 1997;13(4):485–94. doi: 10.1177/074823379701300402. [DOI] [PubMed] [Google Scholar]
- 18.Rothman N, Li GL, Dosemeci M. Hematotoxicity among Chinese workers heavily exposed to benzene. AmJ Ind Med. 1996;29:236–46. doi: 10.1002/(SICI)1097-0274(199603)29:3<236::AID-AJIM3>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 19.Fishbeck WA, Townsend JC, Swank MG. Effects of chronic occupational exposure to measured concentrations of benzene. J Occup Med. 1978;20(8):539–42. doi: 10.1097/00043764-197808000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Georgieva T, Lukanova A, Panev T, et al. Study of erythrocytes, hemoglobin levels, and menstrual cycle characteristics of women exposed to aromatic hydrocarbons. Int Arch Occup Environ Health. 1998;71:16–8. [PubMed] [Google Scholar]
- 21.Khuder SA, Youbgdale MC, Bisesi MS, et al. Assessment of complete blood count variations among workers exposed to low levels of benzene. J Occup Environ Med. 1999;41:821–6. doi: 10.1097/00043764-199909000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Department of Commerce. Guidance note controlling isocyanate hazards at work. Work Safe Level 5. West Perth, WA: 2008. [Google Scholar]
- 23.Xiao G, Pan C, Cai Y, Lin H, Fu Z. Effect of benzene, toluene, xylene on the semen quality and the function of accessory gonad of exposed workers. Ind. Ind Health. 2001;39:206–10. doi: 10.2486/indhealth.39.206. [DOI] [PubMed] [Google Scholar]
- 24.Godstein BD, Witz MD. Benzene. In: Lippmann M, editor. Environmental toxicants (Human exposure and their health effects). John Wiley & Sons,Inc.; 2000. pp. 121–49. [Google Scholar]
- 25.Aksoy M. Hematotoxicity and carcinogenicity of benzene. Environ Health Perspect. 1989;82:193–7. doi: 10.1289/ehp.8982193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cody RP, Strawderman WW, Kipen HM. Hematological effects of benzene. Job specific trends during the first year of employment among a cohort of benzene-exposed rubber workers. J Occup Med. 1993;35(8):776–82. [PubMed] [Google Scholar]
- 27.Qu Q, Shore R, Li G, et al. Hematological changes among Chinese workers with a broad range of benzene exposures. Am J Ind Med. 2002;42(4):275–85. doi: 10.1002/ajim.10121. [DOI] [PubMed] [Google Scholar]
- 28.Ward E, Hornung R, Morris J, et al. Risk of low red or white blood cell count related to estimated benzene exposure in a rubberworker cohort (1940–1975). Am J Ind Med. 1996;29:247–57. doi: 10.1002/(SICI)1097-0274(199603)29:3<247::AID-AJIM4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 29.Marieb EN. Human anatomy and physiology. 3rd ed. Benjamin and Cummings Publishing Company; CA: 1995. pp. 585–611. [Google Scholar]
- 30.Henderson RF, Sabourin PJ, Bechntold WE, et al. Isobutene (2-methylpropene). Toxicol Appl Pharmacol. 1993;123:50–61. doi: 10.1006/taap.1993.1220. [DOI] [PubMed] [Google Scholar]
- 31.Kato M, Rocha ML, Carvallio AB, et al. Occupational exposure to neutratoxicants–preliminary survey in five industries of Camacari petrochemical complex, Brazil. Environ Res. 1993;61:133–9. doi: 10.1006/enrs.1993.1057. [DOI] [PubMed] [Google Scholar]
- 32.Anderson D, Yu TW, Schmezer P. An investigation of the DNA damaging ability of benzene and its metabolites in human lymphocytes using the comet assay. Environ Mol Mutagen. 1995;26:305–14. doi: 10.1002/em.2850260406. [DOI] [PubMed] [Google Scholar]
- 33.Parke DV. Personal reflections on 50 years of study of benzene toxicology. Environ Health Perspect. 1996;104:1123–8. doi: 10.1289/ehp.961041123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith MT. The mechanism of benzene induced leukemia: a hypothesis and speculations on the causes of leukemia. Environ Health Perspect. 1996;104(6):1219–25. doi: 10.1289/ehp.961041219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klassen CD. Nonmetallic environmental toxicant: air pollutants, solvents, vapour and articles. In: Gilman AG, Rall TW, Niuo AS, Taylor P, editors. Goodman and Gillman’s textbook, the pharmacological basis of therapeutics. 8th ed. Pergamon Press; New York: 1990. pp. 1596–614. [Google Scholar]
- 36.Rabble GK, Wong O. Leukemia mortality by cell type in petroleum workers with potential exposure to benzene. Environ Health Perspect. 1996;104:1381–92. doi: 10.1289/ehp.961041381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ross D. Metabolic basis of benzene toxicity [review]. Eur J Haematol. 1996;60:111–8. doi: 10.1111/j.1600-0609.1996.tb01656.x. [DOI] [PubMed] [Google Scholar]
- 38.Brugnone F, Perbellini L, Romeo L, et al. Benzene in blood as biomarker of low level occupational exposure. Sci Tot Environ. 1999;235:247–52. doi: 10.1016/s0048-9697(99)00197-7. [DOI] [PubMed] [Google Scholar]
- 39.Taioli E, Sramb RJ, Binkova B, et al. Biomarkers of exposure to carcinogenic PAHs and their relationship with environmental factors. Mutat Res. 2007;620:16–21. doi: 10.1016/j.mrfmmm.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 40.Ali S, Sathiakumar N, Delzell E. Prevalence and sociodemographic factors associated with tobacco smoking among adult males in rural Sindh, Pakistan. Southeast Asian J Trop Med Public Health. 2006;37(5):1054–60. [PubMed] [Google Scholar]
- 41.Parry H, Cohen S, Schlarb J, et al. Smoking, alcohol consumption and leukocyte counts. Am J Clin Pathol. 1996;107(1):64–7. doi: 10.1093/ajcp/107.1.64. [DOI] [PubMed] [Google Scholar]
- 42.Glantz SA, William WP. Passive smoking and heart disease mechanisms and risk. J. JAMA. 1998;273(3):1047–53. [PubMed] [Google Scholar]
- 43.Tell GS, Grimm Jr RH, Vellar OD, Theodorsen L. The relationship of white cell count, platelet count, and hematocrit to cigarette smoking in adolescents: theOsloYouth Study. Circulation. 1985;72(5):971–4. doi: 10.1161/01.cir.72.5.971. [DOI] [PubMed] [Google Scholar]
- 44.Local 891 IATSE. Safe work procedures for isocyanate-containing products. Dillon Consulting Limited; Richmond, BC: 2000. [Google Scholar]
- 45.Davidson RD, Courage C, Rushton L. Benzene in the environment: an assessment of the potential risks to the health. Occup Environ Med. 2001 Jan;58(1):2–13. doi: 10.1136/oem.58.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yan C, Guilan L, Songnian Y. [Individuals susceptibility to hematotoxicity from benzene exposure and the genetic polymorphism of metabolic enzymes]. Wei Sheng Yan Jiu. 2002 Apr;31(2):130–2. [PubMed] [Google Scholar]
- 47.Yin SN, Hays RB, Linet MS, et al. A cohort study of cancer among benzene-exposed workers in China: overall results. Am J Ind Med. 1996;29:227–35. doi: 10.1002/(SICI)1097-0274(199603)29:3<227::AID-AJIM2>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 48.Snyder R, Witz G, Golstein BD. The toxicology of benzene. Environ Health Perspect. 1993;100:293–306. doi: 10.1289/ehp.93100293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Snyder R, Kalf GF. A perspective on benzene leukemogenesis. Crit Rev Toxicol. 1994;24:177–209. doi: 10.3109/10408449409021605. [DOI] [PubMed] [Google Scholar]
- 50.Kirkeleit J, Riise T, Bratveit M, et al. Biological monitoring of benzene exposure during maintenance work in crude oil cargo tanks. Chem Biol Interact. 2006;164:60–7. doi: 10.1016/j.cbi.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 51.Liu H, Bowes YS, Xu H, et al. Benzene exposure in industries using or manufacturing paint in China–a literature review, 1956–2005. J Occup Environ Hyg. 2009;6:659–70. doi: 10.1080/15459620903249646. [DOI] [PubMed] [Google Scholar]
- 52.EPA. EPA guidelines. 2007 Spray painting booths–control of air and noise emissions [EPA 100/07: Australian guideline replacement of earlier version (September 2003)]; June.


