Abstract
Objective
Although low parent health literacy (HL) has been linked to poor child health outcomes, it is not known whether differences in perceptions related to access to care and provider–parent partnership in care are potential contributing factors. We sought to assess whether parent HL is associated with differences in perceived barriers to care and attitudes regarding participatory decision-making with the provider.
Methods
This was a cross-sectional analysis of data collected from parents presenting with their child to an urban public hospital pediatric clinic in New York City. Dependent variables were caregiver-reported barriers to care (ability to reach provider at night/on weekends, difficult travel to clinic) and attitudes towards participatory decision-making (feeling like a partner, relying on doctor’s knowledge, leaving decisions up to the doctor, being given choices/asked opinion). The primary independent variable was caregiver HL (Short Test of Functional Health Literacy in Adults [S-TOHFLA]).
Results
A total of 823 parents were assessed; 1 in 4 (27.0%) categorized as having low HL. Parents with low HL were more likely to report barriers to care than those with adequate HL: trouble reaching provider nights/weekends, 64.9% vs. 49.6%, (p < 0.001, adjusted odds ratio [AOR] 1.7, 95% confidence interval [95% CI] 1.2–2.4); difficult travel, 15.3% vs. 8.0%, (p = 0.004, AOR 1.8, 95% CI 1.1–3.0). Low HL was also associated with not feeling like a partner (28.8% vs. 17.1%; AOR 2.0; 95% CI 1.4–3.0), preference for relying on the doctor’s knowledge (68.9% vs. 52.2%; AOR 1.7; 95% CI 1.2–2.4), and preference for leaving decisions up to the doctor (57.7% vs. 33.3%; AOR 2.2; 95% CI 1.6–3.1).
Conclusions
Addressing issues of parent HL may be helpful in ameliorating barriers to care and promoting provider-parent partnership in care.
Keywords: access, barriers to care, health literacy, participatory decision-making, pediatric primary care, provider–patient communication, shared decision-making
The presence of a “medical home” has been identified as a key indicator of high-quality primary care, serving as a mechanism to support the coordination of care between providers.1,2 A central feature of an adequate medical home is that it specifically addresses access barriers.1,3,4 A second core feature of the medical home, family-centered care, focuses on partnership between the primary care provider and the family, where they are considered to be jointly responsible for the decision-making process, including the development of a care plan.1,3
Adequate access to care has been linked to fewer unmet healthcare needs, improved health status, and better health outcomes.2,5,6 Strategies to ensure adequate access not only include providing access to health insurance but also involve addressing pragmatic barriers, such as ease of travel to the provider’s office and ease of access to providers after hours.7,8
Family-centered care, which includes participatory decision-making, has been shown to increase patient satisfaction with care and optimize health outcomes in adult primary and chronic disease care.9–11 Although there has been limited study of shared decision-making in pediatrics, greater parent participation in decision-making may also lead to improved care, such as less unnecessary antibiotic use.12
Accessing resources and functioning in partnership relationships with providers requires an ability to process and manage health-related information.13 Because such information is often complex, processing of this information may result in a high cognitive load for patients, a situation that can be especially difficult for those with low health literacy.14–16 For example, studies to date have found that adult patients with low health literacy report less accessibility of care, including less participation in medical decision-making related to their own care and lower levels of empowerment.13,17 It is not presently known, however, whether health literacy similarly contributes to differences in attitudes and perceptions related to access and participation in decision-making in the context of pediatric care. We sought to address this gap in knowledge through a study of families in a single primary care setting who would be expected to have equivalent access to providers and opportunities for shared decision-making but have varying levels of health literacy.
Methods
Study Sample
This was a cross-sectional analysis of data gathered as part of a large study examining provider–parent communication and medication counseling. Parents and caregivers presenting with their child for an acute care visit to the pediatric clinic at Bellevue Hospital, an urban public hospital in New York City, were enrolled from July 13, 2007, through October 7, 2008. During times when enrollment was taking place, research assistants consecutively assessed families to determine eligibility. Research assistants were present each day of the week, covering both morning and afternoon clinic sessions.
Inclusion criteria for the larger study were parent or legal guardian who was the primary caregiver of a child (1 day to 18 years of age) presenting for an acute care visit to the pediatric clinic. The exclusion criteria was caregiver’s language not English or Spanish. For this analysis of families within a single primary care setting, families were also excluded if they did not state that Bellevue Hospital was the primary site at which they sought care for their child. Written, informed consent was obtained. Institutional Review Board approval was obtained from the New York University School of Medicine and Bellevue Hospital Center.
Data Collection
Data were obtained by interview, conducted in English or Spanish, on the basis of the caregiver’s language of preference. Bilingual (English/Spanish) research assistants were present during all recruitment sessions. Research assistants who collected the data were trained by one of the authors (S.Y.) with periodic review and observation to ensure that data was collected reliably.
Dependent Variables
The primary dependent variables of interest encompassed 2 domains: barriers to care and participatory decision-making. Perceived barriers to care were assessed with the use of 2 questions from the Access subsection of the Parent Perceptions of Primary Care (P3C) survey instrument, a validated tool to examine pediatric primary care quality that has been found to be associated with poorer health-related quality of life and decreased adherence to treatment.7,8,18,19 Ability to reach a provider after hours was assessed with the question: “Are you able to reach someone in your child’s regular doctor’s office in the evenings and on the weekends?” Answer choices were yes, no, and don’t know. Answers were dichotomized in analyses, with caregivers who stated that they were able to reach someone compared with those who were not able to reach someone or were unsure.
Difficulty traveling to the child’s primary care site was assessed with the following question: “How easy is it to travel to your child’s regular doctor’s office?” Answer choices were very easy, somewhat easy, somewhat difficult, and very difficult. For the purposes of analyses, answers were dichotomized, with caregivers who stated that traveling to their child’s primary care site was very difficult compared to all others.
Perceptions and attitudes towards participatory decision-making were assessed with the use of 4 questions previously used to examine the provider–parent relationship and communication preferences in 2 large national surveys (1 question from the National Survey of Children with Special Health Care Needs; 3 questions from the General Social Survey, adapted to be child-focused).20,21 Parents’ perceptions of whether they felt like a partner in their child’s care were assessed with the question “How often did your child’s doctor or other health care providers help you feel like a partner in his/ her care?” Answer choices were always, usually, sometimes, never, or unsure.20 Answers were dichotomized for analyses, with parents who answered always/usually compared with those who answered sometimes/never/unsure. Parent preferences related to decision-making were assessed by asking parents the extent to which they agreed with the following statements: “I prefer to rely on my child’s doctor’s knowledge,” “I prefer to leave decisions about my child’s medical care up to my child’s doctor,” and “I prefer that my child’s doctor offers me choices and asks my opinion.”21 Answer choices were strongly agree, moderately agree, slightly agree, slightly disagree, moderately disagree, and strongly disagree. For purposes of analyses, answers were dichotomized with those who strongly agreed with the statement compared with all others.
Primary Independent Variable
The primary independent variable for this study was parent health literacy. Caregiver health literacy was assessed using the short Test of Functional Health Literacy in Adults (STOFHLA), which includes both reading comprehension and numeracy subsections.22 Health literacy was categorized as inadequate (score 0–53), marginal (score 54–66), or adequate (score 67–100). The STOFLHA is validated in English and Spanish and is one of the most commonly used assessments for health literacy.13,23 For 3 subjects, administration of the STOFHLA was interrupted when their children were called to be seen; for these subjects, the reading comprehension portion was able to be completed, allowing us to categorize the subjects into the 3 health literacy categories based on the reading comprehension sections only. This categorization schema has been previously validated and is highly correlated with the full STOFHLA.24 For purposes of analyses, health literacy was dichotomized as those with adequate literacycompared with those with low (inadequate/marginal) health literacy.
Additional Data Collected as Potential Confounders
Potential confounders, including sociodemographics and child health care-related experiences, were also collected. Sociodemographic data included child’s age, caregiver relationship to child, and caregiver’s age, country of origin, ethnicity, language, education, and socioeconomic status (SES). Caregiver country of origin was dichotomized as U.S. born or birthplace outside the United States. Ethnicity was categorized as Latino and non-Latino because Latinos comprise the majority of patients seen at Bellevue, and no other ethnic group in this sample comprised a large enough group to define a separate category. Caregiver language was categorized on the basis of caregiver preference of language of STOFHLA administration (English or Spanish).
Education was assessed as years of education received, as well as categorically on the basis of whether the caregiver had graduated high school. SES was assessed by the use of Hollingshead Four Factor Index of Social Status based upon education and occupation. SES was coded to a 5-point scale, with 1 representing the highest resource level and 5 representing the lowest resource level.25 For analyses, SES was dichotomized as Hollingshead Index of 4 or 5 versus all others. Because commute time to Bellevue Hospital is a potential confounder related to both difficulty traveling to the clinic site as well as health literacy level, we used caregiver address to estimate commute time using public transportation from the child’s home to the clinic site (Google Maps). The majority of families who seek care for their children at Bellevue use public transportation to travel to the pediatric clinic.
Child health care-related experiences were assessed by asking caregivers whether the child had a regular health care provider, as well as assessing child chronic disease status using the CSHCN (Children with Special Health Care Needs) Screener.26–28
Statistical Analyses
Data were analyzed with the use of SPSS 17.0 (SPSS Inc., Chicago, Ill). For all analyses, a 2-tailed P-value <.05 was considered to be statistically significant. We assessed associations between health literacy and the dependent variables of interest (parent reported barriers to care, parent attitudes toward provider–parent relationship), by using bivariate (χ2), and adjusted analyses (multiple logistic regression analyses). Adjusted analyses were performed with a priori inclusion of potential confounders, including caregiver age, language, country of birth, and ethnicity, as well as child age, child chronic disease status, and presence of child regular provider. Given ongoing controversy in the field about the relationship between education and health literacy, and inclusion of both as independent factors, we analyzed models with and without adjusting for years of education.29–31 For analyses related to difficulty traveling to child’s primary care site, we performed additional analyses controlling for commute time from the child’s home to the clinic site.
Results
During the enrollment period from July 2007 through October 2008, families presenting with their children to the pediatric clinic for acute care were consecutively assessed during times when research assistants were available. Of 1534 families assessed, 1236 (80.6%) were considered to be eligible (Fig. 1). A total of 298 (19.4%) were considered to be ineligible because of 1 or more of the following: caregiver not parent or legal guardian (n = 53), caregiver not able to communicate in English or Spanish (n = 181), primary caregiver not present (n = 111), or child uptriaged or brought to the physician to be seen quickly (n = 38). Of the 1236 eligible families, 876 (70.9%) were enrolled, whereas 360 (29.1%) refused. The primary reason for refusal was because of concern regarding the time constraints needed to complete the study.
Figure 1.
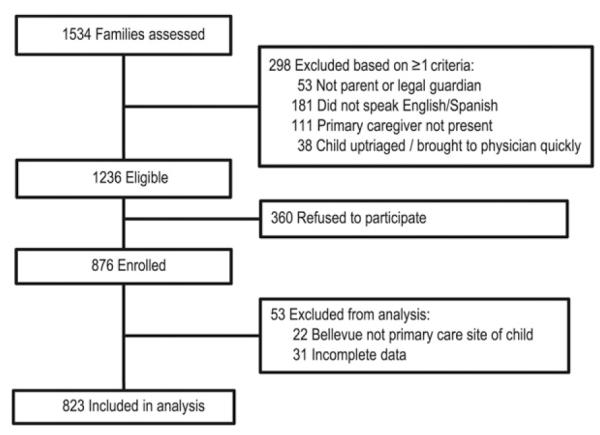
Study enrollment.
There was no statistically significant difference between those who were enrolled and those who refused with respect to age and gender. Although no data regarding country of birth or ethnicity were collected from those who refused to participate, these characteristics within the enrolled sample were consistent with known characteristics of our general clinic sample. For the purposes of this analysis, an additional 22 families were excluded because they did not state that Bellevue Hospital was the primary site at which they typically sought care for their child. In addition, 31 cases were excluded because of missing data. Therefore, 823 caregivers were included in analyses, with 775 mothers, 36 fathers, and 12 others interviewed. Caregivers were primarily Latino (81.9%) (23.1% Caribbean, 51.% Mexican, 3.6% Central American, 19.6% South American, 2.7% other). The majority of families had a low SES background (80.1%), with a large percent of parents being non-U.S. born (81.8%). Descriptive data are shown in Table 1.
Table 1.
Characteristics of Study Population*
| Child characteristics | |
| Child age, mean (SD), yr | 4.6 (4.3) |
| Child with chronic medical problem, n (%) | 175 (21.3) |
| Child with health insurance coverage | 793 (96.4) |
| Caregiver characteristics | |
| Caregiver age, mean (SD), yr | 32.3 (8.4) |
| Relationship to child, n (%) | |
| Mother | 775 (94.2) |
| Marital status single, n (%) | 229 (27.8) |
| Hollingshead SES† level 4 or 5, n (%)‡ | 659 (80.1) |
| Caregiver non-U.S. born, n (%) | 673 (81.8) |
| Caregiver race/ethnicity, n (%) | |
| Hispanic | 674 (81.9) |
| Non-Hispanic | |
| White, non-Hispanic | 20 (2.4) |
| Black, non-Hispanic | 57 (6.9) |
| Asian, non-Hispanic | 56 (6.8) |
| Other, non-Hispanic | 16 (1.9) |
| Caregiver language Spanish, n (%)§ | 507 (61.6) |
| Caregiver education, mean (SD), yr | 10.6 (3.7) |
| Caregiver education, n (%) | |
| Less than high school graduate | 249 (30.3) |
| High school graduate or equivalent | 148 (18.0) |
| More than high school | 426 (51.8) |
| Caregiver health literacy, n (%)∥ | |
| Inadequate literacy | 144 (17.5) |
| Marginal literacy | 78 (9.5) |
| Adequate literacy | 601 (73.0) |
| Commuting time, mean (SD), min | 40.9 (15.4) |
Data are mean (SD [standard deviation]) or n(%).
SES indicates socioeconomic status.
Lower number represents greater SES and greater family resources.
Language of survey administration.
Health literacy measured using STOFHLA (3 of whom completed only reading comprehension section).
Health Literacy
Mean (SD) caregiver STOFHLA score was 76.3 (23.9); range (0–100). Low health literacy was statistically significantly related to longer commute times (mean [SD] 42.6 [13.7] minutes vs 40.3 [16.0] minutes; P = .04). TOFHLA scores were lower for those who took the test in Spanish (20.5% inadequate, 11.2% marginal, 68.2% adequate) compared with those who took the test in English (12.7% inadequate, 6.6% marginal, 80.7% adequate; P < .001). Other sociodemographic factors associated with lower health literacy skills included birthplace outside the United States (P < .001), less than a high school education (P < .001) and being in a lower Hollingshead SES category (P < .001). No differences were found related to child health insurance and health literacy level (P = .8).
Perceived Barriers to Care
Almost one-half (45.8%) of parents reported that they were not able to reach someone after hours, with 7.9% unsure if they could do so. One in 10 reported that it was very difficult to travel to their child’s primary care site (Table 2). Difficulty traveling to the child’s primary care site was related to commute time (very difficult travel: mean (SD) 47.2 (15.1) minutes, not very difficult: 40.2 (15.3) minutes; P < .001).
Table 2.
Descriptive Data for Dependent Variables
| Dependent Variable | n (%) |
|---|---|
| Barriers to accessing care | |
| Able to reach provider during off hours* | |
| Yes | 381 (46.3) |
| No | 377 (45.8) |
| Not sure | 65 (7.9) |
| Travel to child’s primary care site† | |
| Very easy | 196 (23.8) |
| Somewhat easy | 298 (36.2) |
| Somewhat difficult | 247 (30.0) |
| Very difficult | 82 (10.0) |
| Provider–parent communication | |
| Child’s doctor helped them feel like a partner in care‡ |
|
| Always | 540 (65.6) |
| Usually | 116 (14.1) |
| Sometimes | 104 (12.6) |
| Never | 54 (6.6) |
| Unsure | 9 (1.1) |
| Prefer to rely on child’s doctor’s knowledge§ | |
| Strongly agree | 467 (56.7) |
| Moderately agree | 114 (13.9) |
| Slightly agree | 66 (8.0) |
| Slightly disagree | 53 (6.4) |
| Moderately disagree | 47 (5.7) |
| Strongly disagree | 76 (9.2) |
| Prefer to leave decisions about child’s medical care up to child’s doctor§ |
|
| Strongly agree | 328 (39.9) |
| Moderately agree | 207 (25.2) |
| Slightly agree | 92 (11.2) |
| Slightly disagree | 70 (8.5) |
| Moderately disagree | 59 (7.2) |
| Strongly disagree | 67 (8.1) |
| Prefer that child’s doctor offers choices and asks opinion§ |
|
| Strongly agree | 669 (81.3) |
| Moderately agree | 106 (12.9) |
| Slightly agree | 24 (2.9) |
| Slightly disagree | 4 (0.5) |
| Moderately disagree | 12 (1.5) |
| Strongly disagree | 8 (1.0) |
Dichotomized for analysis, with those answering “yes” compared with those who answered “no” or “unsure.”
Dichotomized for analysis, with those answering “very easy, ” “somewhat easy,” or “somewhat difficult” compared with those who answered “very difficult.”
Dichotomized for analysis, with those answering “always” or “usually,” compared with those who answered “sometimes” or “never” or “unsure.”
Dichotomized for analysis, with those answering “strongly agree” compared with those who answered “moderately agree,” “slightly agree,” “slightly disagree,” “moderately disagree,” or “strongly disagree.”
Perceptions and Attitudes Toward Participatory Decision-Making
One in 5 reported that their child’s doctor did not usually or always help make them feel like a partner. More than one-half strongly preferred to rely on their child’s doctor’s knowledge. Forty percent of parents strongly preferred to leave decisions about their child’s medical care up to their child’s doctor. Approximately 80% strongly agreed with the statement “I prefer that my child’s doctor offers me choices and asks my opinion” (Table 2).
Association between Low Parent Health Literacy and Perceived Barriers to Care
Unadjusted Analyses
In unadjusted analyses, parents with low (inadequate/marginal) health literacy were more likely to report an inability to reach a provider during off hours, compared with parents with adequate health literacy (64.9% vs 49.6%; P < .001). Similarly, parents with low health literacy were more likely to report that traveling to their child’s primary care site was very difficult compared with parents adequate health literacy (15.3% vs 8.0%; P = .004; Table 3).
Table 3.
Health Literacy, Parent-Reported Barriers To Care, and Attitudes Toward Provider–Parent Communication
| Health Literacy* |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Low |
Adequate |
Unadjusted Analyses |
Model 1, Adjusted Analyses† |
Model 2, Adjusted Analyses‡ |
|||||||
| n (%) | n (%) | Odds Ratio§ |
95% Confidence Interval |
P Value∥ | Adjusted Odds Ratio§ |
95% Confidence Interval |
P Value | Adjusted Odds Ratio§ |
95% Confidence Interval |
P Value | |
| Not able to reach provider during off hours |
144 (64.9) | 298 (49.6) | 1.9 | 1.4–2.6 | <.001 | 1.7 | 1.2–2.4 | .002 | 1.8 | 1.2–2.6 | .002 |
| Very difficult traveling to child’s primary care site |
34 (15.3) | 48 (8.0) | 2.1 | 1.3–3.3 | .004 | 1.8¶ | 1.1–3.0 | .03 | 1.7# | 0.95–3.0 | .08 |
| Does not usually feel like a partner in child’s care |
64 (28.8) | 103 (17.1) | 2.0 | 1.4–2.8 | <.001 | 2.0 | 1.4–3.0 | <.001 | 2.0 | 1.3–3.1 | .002 |
| Strongly prefers to rely on doctor’s knowledge |
153 (68.9) | 314 (52.2) | 2.0 | 1.5–2.8 | <.001 | 1.7 | 1.2–2.4 | .005 | 1.6 | 1.1–2.4 | .01 |
| Strongly prefers to leave decisions up to the doctor |
128 (57.7) | 200 (33.3) | 2.8 | 2.0–3.8 | <.001 | 2.2 | 1.6–3.1 | <.001 | 1.9 | 1.3–2.8 | .001 |
| Strongly prefers to be offered choices/asked opinion |
178 (80.2) | 491 (81.7) | 0.9 | 0.6–1.3 | 0.6 | 0.8 | 0.5–1.3 | 0.4 | 0.7 | 0.4–1.1 | 0.1 |
Health literacy measured using the Short Test of Functional Health Literacy in Adults (STOFHLA); low health literacy combination of inadequate and marginal health literacy categories.
Model 1: controlling for caregiver age, language, ethnicity, country of birth, socioeconomic status; child age, chronic disease status.
Model 2: controlling for variables in Model 1 and parent years of education.
Comparing low with adequate health literacy.
Chi-square.
With inclusion of commute time as part of Model 1, health literacy remains statistically significantly related (adjusted odds ratio 1.7; 95% confidence interval 1.04–2.9; P = .04).
With inclusion of commute time as part of Model 2, health literacy is not statistically significantly related (adjusted odds ratio 1.7; 95% confidence interval 0.95–3.0; P = .08).
Adjusted Analyses
Results of separate multiple logistic regression analyses assessing the association between parent health literacy and parent reported barriers to care are shown in Table 3. Low health literacy was significantly associated with inability to reach a provider during off hours (adjusted odds ratio [AOR] 1.7; 95% confidence interval [95% CI] 1.2–2.4). Low health literacy was also significantly associated with parent-reported difficulty traveling to the child’s primary care site (AOR 1.8; 95% CI 1.1–3.0). This relationship remained significant even after adjusting for commuting time (AOR 1.7; 95% CI 1.04–2.9). In adjusted analyses including education in the model, health literacy remained significantly associated with inability to reach a provider during off hours (P = .002) but was no longer statistically significantly associated with reported difficulty traveling to the child’s primary care site (P = .08).
Association between Low Parent Health Literacy and Perceptions and Attitudes Toward Participatory Decision-making
Unadjusted Analyses
In unadjusted analyses, parents with low health literacy were more likely to not feel like a partner in their child’s care and to strongly prefer to rely on their doctor’s knowledge and leave decisions up to the doctor (Table 3). There was no difference between parents with low and adequate literacy with respect to preference for being offered choices and asked for opinions (low health literacy: 80.2%, adequate health literacy: 81.7%; P = .8).
Adjusted Analyses
Low health literacy was statistically significantly associated with not feeling like a partner (AOR 2.0; 95% CI 1.4–3.0), and strong preference for relying on the doctor’s knowledge (AOR 1.7; 95% CI 1.2–2.4) and leaving decisions up to the doctor (AOR 2.2; 95% CI 1.6–3.1;Table 3). Even when education was included in the model, health literacy remained significantly associated with each of these outcome variables.
Discussion
Our study is one of the first to investigate health literacy and its relationship to parent perceptions of barriers to care and preferences for clinical decision-making. We found that within a single primary care site, considerable heterogeneity exists in perceived access to care and perceptions of provider–parent partnership in care, and that health literacy was found to be significantly associated with this heterogeneity. Parents with low health literacy were more likely to perceive difficulties with accessing care. Parents with low health literacy also reported lower levels of partnership in care and stated a preference for relying on the doctor to make decisions. These findings suggest a need to include a health literacy perspective in examining issues of perceived access and preferences regarding provider–parent participatory decision-making.
Despite the fact that the primary care site in our study emphasizes access to care, including providing 24-hour telephone access to providers, more than one-half of parents in our study reported difficulty reaching a provider during off hours or being unsure about whether it was possible to reach a provider at those times. In addition, almost 15% of parents with low health literacy reported significant difficulty traveling to the health care site, which may reflect lack of knowledge regarding how to access health care systems closer to their homes or how to navigate transportation options. Other studies in which authors have looked at health literacy as a factor in accessing care have linked low health literacy with more emergency room visits, suggesting barriers to accessing their regular provider,32 as well as increased likelihood of having an uninsured child in the household.”33 Our study findings suggest additional ways in which health literacy might impede access.
In addition, although this study took place within a single primary care site in which provider–parent partnership in care is valued, 1 in 5 parents did not feel like a partner in their child’s care. Few studies have examined the relationship between parent health literacy, provider–patient partnership, and communication preferences. Our findings support the need to further examine these communication preferences and are consistent with previous research in which authors have found that patients with low health literacy report poorer quality of empowerment in their treatment and less participation in medical decision-making.17
Although the majority of parents in our study preferred being offered choices in their child’s care, regardless of literacy level, parents with low health literacy reported a preference for lower levels of participatory decision-making. This finding is consistent with the characterization of low literacy patients as individuals who have difficulty with the complexities associated with obtaining, under-standing, and processing basic health information to make appropriate health decisions. With limitations in the ability to integrate reading, listening, analytical, and decision-making skills, parents with low health literacy may have a greater dependence on providers to make important management decisions.20
Addressing the provider–parent relationship using a health literacy approach may help empower families to more fully engage in their medical home. Physician use of clear communication strategies has been found to enhance communication across literacy levels,34 and may contribute to increased parent understanding of their child’s health issues as well as desire for increased partnership in their child’s health care. Reducing the complexity of information by using plain language, focusing on 2 to 3 key concepts, incorporating teachback, and providing pictorial-enhanced print materials to supplement written information, are among the evidence-based strategies that providers can incorporate into their daily routine.14,34,35 Use of these tools, in a universal precautions approach, is recommended because providers often are inaccurate in their estimation of patient health literacy levels,36 and patients are unlikely to express their inability to comprehend information provided, due to fear of embarrassment.37
It is well-recognized that variability in patient preferences regarding provider partnership and shared decision-making exists, and that cultural factors may play a role.38–41 Preconceived notions regarding patient preferences, however, may lead to physician behaviors that contribute to disparities in health outcomes.38 Physicians are therefore encouraged to engage all patients in clinical decision-making, and to assess the individual preferences of patients and families.38,42 A better understanding of how to effectively engage patients and their families across different cultures is needed to optimize health outcomes. Additional study is also indicated to examine other factors that may be related to the perceptions and preferences of those with limited health literacy, as health literacy may act through indirect pathways. For example, those with limited health literacy may be more likely to see providers who are less proficient in their ability to engage in shared decision-making.
This study has several limitations. This was a cross-sectional study; as such, only associations can be examined, and conclusions regarding causation cannot be drawn. In addition, we relied on self-report of barriers to care and preferences, which may have been subject to social desirability bias. Our data on commute time were obtained from geomapping rather than from parents themselves. Furthermore, these data were gathered as part of a larger study, where only patients presenting for acute care at their primary care setting were selected, which may have led to selection bias. It is possible that those who seek acute care in their primary care setting are different than those who seek acute care in the emergency department setting. Finally, as this study was conducted in one urban hospital with predominantly low SES Latina caregivers, these results may not be generalizable to other populations.
Our study findings reveal that low health literacy is associated with greater perceived barriers to care and decreased provider–parent partnership, which may directly affect access to care and health outcomes. These findings suggest that the communication of information regarding how to access primary care may need to be improved in order to enable low literacy patients to access services such as after-hours care. In addition, addressing provider-parent partnership and shared decision-making using a health literacy approach may be beneficial, in order to enable parents with low literacy to more fully engage in the management of their children’s health issues. Additional study is needed to examine how to best encourage partnership and shared decision-making using a health literacy perspective, while accounting for cultural variations in preferences.
What’s New.
Parents with low health literacy are more likely to perceive greater difficulties with accessing care and report lower levels of provider–parent partnership in care, which may place their children at risk for poor health outcomes.
Acknowledgments
Preliminary data from this study were presented at the 2009 Pediatric Academic Societies’ annual meeting (E-PAS2009:2350.4); May 2, 2009; Baltimore, MD. Research coordinators Isabel Bazan, BA, Maria Cerra, BA, Hannah Moreira, BA, and Dayana Sanchez, BA, and research assistants Brian Alvelo, BA, Cindy Encalada, BA, Alexandra Goodwin, BA, Brian Ahuja, BA, Bradley Collins, BS, Benjamin L. Kitchens, BA, Matthew Kline, MA, Jill Linnell, MPH, Nimesh Patel, BA, Tina Roa, BA, Mark Sechter, BA, Katherine Sticklor, BA, Alejandro Vanegas, BA, and the staff of the Bellevue Hospital Center pediatric outpatient clinic assisted in this study.
Dr. Yin’s work on this study was supported by the Pfizer Fellowship in Health Literacy/Clear Health Communication, NIH Loan Repayment Program (1L40 HD062191), and the APA Young Investigator Award Program. Funding for this study was also provided by the United Hospital Fund, as well as the New York University School of Medicine Department of Pediatrics through the Joseph Dancis Research Fund. Dr. Yin is currently supported in part by the Robert Wood Johnson Physician Faculty Scholars Program. The Robert Wood Johnson Foundation had no role in the design and conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Karina Vivar and Suzanne MacFarland assisted in this work as part of the New York University School of Medicine Department of Pediatrics Medical Student Summer Research Fellowship Program.
REFERENCES
- 1.Wegner SE, Antonelli RC, Turchi RM. The Medical Home-Improving Quality of Primary Care for Children. Pediatric Clinics of North America. 2009;56(4):953–964. doi: 10.1016/j.pcl.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 2.Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: Health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604–611. doi: 10.1542/peds.2009-3555. [DOI] [PubMed] [Google Scholar]
- 3.Trivedi HK, Pattison NA, Neto LB. Pediatric Medical Home: Foundations, Challenges, and Future Directions. Child and Adolescent Psychiatric Clinics of North America. 2010;19(2):183–197. doi: 10.1016/j.chc.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Starfield B, Shi L. The Medical Home, Access to Care, and Insurance: A Review of Evidence. Pediatrics. 2004;113(Supplement 4):1493–1498. [PubMed] [Google Scholar]
- 5.Litaker D, Koroukian SM, Love TE. Context and healthcare access: Looking beyond the individual. Medical Care. 2005;43(6):531–540. doi: 10.1097/01.mlr.0000163642.88413.58. [DOI] [PubMed] [Google Scholar]
- 6.Szilagyi PG, Dick AW, Klein JD, et al. Improved Asthma Care After Enrollment in the State Children’s Health Insurance Program in New York. Pediatrics. 2006;117(2):486–496. doi: 10.1542/peds.2005-0340. [DOI] [PubMed] [Google Scholar]
- 7.Seid M. Barriers to Care and Primary Care for Vulnerable Children with Asthma. Pediatrics. 2008;122(5):994–1002. doi: 10.1542/peds.2007-3114. [DOI] [PubMed] [Google Scholar]
- 8.Seid M, Varni JW, Bermudez LO, et al. Parents’ Perceptions of Primary Care. Pediatrics. 2001;108(2):264–270. doi: 10.1542/peds.108.2.264. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and Visit Characteristics Related to Physicians’ Participatory Decision-Making Style. Medical Care. 1995;33(12):1176–1187. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Greenfield S, Kaplan SH, Ware JE, et al. Patient Participation in Medical Care: Effects on blood sugar control and quality of life in diabetes. Journal of General Internal Medicine. 1988;3:448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 11.Rost KM, Flavin KS, Cole K, et al. Change in Metabolic Control and Functional Status after Hospitalization. Diabetes Care. 1991;14:881–889. doi: 10.2337/diacare.14.10.881. [DOI] [PubMed] [Google Scholar]
- 12.Merenstein D, Diener-West M, Krist A, et al. An Assessment of the Shared-Decision Model in Parents of Children with Acute Otitis Media. Pediatrics. 2005;118(8):1267–1275. doi: 10.1542/peds.2005-0486. [DOI] [PubMed] [Google Scholar]
- 13.Schwartzberg JG, Van Geest JB, Wang CC, editors. Understanding Health Literacy: Implications for Medicine and Public Health. AMA Press; 2005. [Google Scholar]
- 14.Doak CC, Doak LG, Root JH. Teaching patients with low literacy skills. Lippincott Williams & Wilkins; Philadelphia, PA: 1996. [Google Scholar]
- 15.Lavie N. Distracted and confused?: selective attention under load. Trends in Cognitive Science. 2005;9(2):75–82. doi: 10.1016/j.tics.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Lavie N, Hirst A, de Fockert J, Viding E. Load theory of selective attention and cognitive control. J Exp Psychol Gen. 2004;133(3):339–354. doi: 10.1037/0096-3445.133.3.339. [DOI] [PubMed] [Google Scholar]
- 17.Schillinger D, Bindman A, Wang F, et al. Functional Health Literacy and the Quality of Physician-Patient Communicaiton among Diabetes Patients. Patient Education and Counseling. 2004;52:315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 18.Seid M, Opipari-Arrigan L, Gelhard LR, et al. Barriers to Care Questionnaire: reliability, validity, responsiveness to change among parents with children with asthma. Academic Pediatrics. 2009;9(2):106–113. doi: 10.1016/j.acap.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Seid M, Stevens GD. Access to Care and Children’s Primary Care Experiences: Results from a Prospective Cohort Study. Health Services Research. 2005;40(6):1758–1780. doi: 10.1111/j.1475-6773.2005.00435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Survey of Children with Special Health Care Needs. Child and Adolescent Health Measurement Initiative; Portland, OR.: 2001. [Google Scholar]
- 21. [Accessed July 1, 2011];General Social Surveys, 1972-2008 Cumulative Codebook. National Data Program for the Social Sciences. 2009 Cumulative Data File. Available at: http://publicdata.norc.org:41000/gss/documents/BOOK/2008%20GSS%20Codebook.pdf.
- 22.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Education & Counseling. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 23.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes. a systematic review of the literature. Journal of General Internal Medicine. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nurss J, Parker R, Baker D. TOFHLA: Test of functional health literacy in adults. Peppercorn Books & Press; Snow Camp, NC: 1995. [Google Scholar]
- 25.Hollingshead A. Four factor index of social status. Yale University; New Haven, Conn: 1975. [Google Scholar]
- 26.Bethell CD, Read D, Neff J, et al. Comparison of the children with special health care needs screener to the questionnaire for identifying children with chronic conditions–revised. Ambulatory Pediatrics. 2002;2(1):49–57. doi: 10.1367/1539-4409(2002)002<0049:cotcws>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 27.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 28.van Dyck PC, McPherson M, Strickland BB, et al. The national survey of children with special health care needs. Ambulatory Pediatrics. 2002;2(1):29–37. doi: 10.1367/1539-4409(2002)002<0029:tnsocw>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 29.DeWalt DA, Dilling Marylee H, Rosenthal Marjorie S, Pignone Michael P. Low Parental Literacy Associated with Worse Asthma Care Measures in Children. Ambulatory Pediatrics. 2007;7(1):25–31. doi: 10.1016/j.ambp.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeWalt DA, Pignone MP. Reading Is Fundamental: The Relationship Between Literacy and Health. Arch Intern Med. 2005;165(17):1943–1944. doi: 10.1001/archinte.165.17.1943. [DOI] [PubMed] [Google Scholar]
- 31.Baker DW. The meaning and measure of health literacy. Journal of General Internal Medicine. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baker D, Gazmararian JA, William MV, et al. Health literacy and use of outpatient physician services by medicare managed care enrollees. J Gen Intern Med. 2004;19(3):215–220. doi: 10.1111/j.1525-1497.2004.21130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yin HS, Johnson M, Mendelsohn AL, et al. The health literacy of parents in the United States: A nationally representative study. Pediatrics. 2009;124:289–298. doi: 10.1542/peds.2009-1162E. [DOI] [PubMed] [Google Scholar]
- 34.Yin HS, Forbis S, Dreyer BP. Health literacy and pediatric health. Current Problems in Pediatric and Adolescent Health Care. 2007;37(7):253–286. doi: 10.1016/j.cppeds.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 35.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Archives of Internal Medicine. 2003 Jan 13;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 36.Wittich A, Mangan J, Grad R, et al. Pediatric asthma: Caregiver health literacy and the clinician’s perception. Journal of Asthma. 2007;44:51–55. doi: 10.1080/02770900601125672. [DOI] [PubMed] [Google Scholar]
- 37.Parikh NS. Shame and health literacy: The unspoken connection. Patient Education and Counseling. 1996;27:33–39. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- 38.Levinson W, Kao A, Kuby A, Thisted R. Not all patients want to participate in decision making. A national study of public preferences. Journal of General Internal Medicine. 2004;20(6):531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flores G, Vega L. Barriers to health care access for Latino children: A review. Family Medicine. 1998;30(3):196–205. [PubMed] [Google Scholar]
- 40.Peek M, Tang H, Cargill A, Chin M. Are there racial differences in patients’ shared decision-making preferences and behaviors among patients with diabetes? Medical Decision Making. 2011;31(3):422–431. doi: 10.1177/0272989X10384739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kon A. The shared decision-making continuum. JAMA. 2010;304(8):903–904. doi: 10.1001/jama.2010.1208. [DOI] [PubMed] [Google Scholar]
- 42.Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; Washington, DC: 2001. [PubMed] [Google Scholar]


