Abstract
Gain-of-function mutations of KCNJ11 can cause permanent neonatal diabetes mellitus, but only rarely after 6 months of age. Specific uncommon mutations KCNJ11 give rise to a syndrome defined as developmental delay, epilepsy, and neonatal diabetes (DEND), or – more frequently – to a milder sub-type lacking epilepsy, denoted as intermediate-DEND (iDEND). Our aim was to consider a possible monogenic etiology in a 12-yr-old boy with early onset diabetes and mild neurological features. We studied a subject diagnosed with diabetes at 21 months of age, and negative to type 1 diabetes autoantibodies testing. He had learning difficulties during primary school, and a single episode of seizures at the age of 10 yr. We performed direct DNA sequencing of the KCNJ11 gene with subsequent functional study of mutated channels in COSm6 cells. The patient's clinical response to oral glyburide (Glyb) was assessed. Motor coordination was evaluated before and after 6 and 12 months of Glyb therapy. Sequencing of the KCNJ11 gene detected the novel, spontaneous mutation S225T, combined with deletion of amino acids 226–232. In vitro studies revealed that the mutation results in a KATP channel with reduced sensitivity to the inhibitory action of ATP. Glyb improved diabetes control (hemoglobin A1c on insulin: 52 mmol/mol/6.9%; on Glyb: 36 mmol/mol/5.4%) and also performance on motor coordination tests that were impaired before the switch of therapy. We conclude that KCNJ11/S225T, del226-232 mutation caused a mild iDEND form in our patient. KCNJ11 should be considered as the etiology of diabetes even beyond the neonatal period if present in combination with negative autoantibody testing and even mild neurological symptoms.
Keywords: developmental delay, glyburide, infancy onset diabetes, KCNJ11, mutation
Heterozygous, activating mutations of KCNJ11 encoding the pore-forming subunit (Kir 6.2) of the ATP-sensitive potassium channel (KATP) are the most prevalent cause of diabetes with onset in the first 6 months of life [1]. Rarely, KCNJ11 mutations are associated with diabetes that presents later in childhood or adulthood [2]. Kir6.2 is expressed not only in the pancreatic beta cell, but also in skeletal muscle, peripheral nerves, and especially brain [3], likely the explanation for a more severe condition termed developmental delay, epilepsy, and neonatal diabetes (DEND syndrome) that can result from rare KCNJ11 missense mutations [3, 4]. Patients with DEND syndrome have motor and speech delay and are often unable to talk and walk without aid. In addition, they suffer from epilepsy that generally occurs before 1 yr of age [3, 4]. In contrast, an intermediate form of the syndrome (iDEND), i.e.. with no epilepsy. is more frequent and less severe [1, 3, 5-8]. Identification of KCNJ11 mutations has important therapeutic consequences, as most patients respond to oral treatment with the sulfonylurea (SU) class of anti-diabetic drugs and can be totally weaned from insulin injections, reaching an excellent, long-lasting metabolic control [9-11]. In addition, motor function and other neurological consequences may be improved by SU treatment [3, 7, 12-14], although some patients with DEND may fail to favorably respond even to very high doses of SU [4, 9].
Patient and methods
The patient is the second child of healthy, non-consanguineous Italian parents. Family history was positive for type 2 diabetes (maternal grandfather) and for headache (mother), but negative for epilepsy. The proband was born at 37 wk with a birth weight of 2400 g (25th centile) after an uneventful pregnancy. The mother reported that motor development in the first years of life was normal, although no medical record describing developmental milestones was available. At the age of 21 months, the child was diagnosed with diabetes without ketosis [plasma glucose: 321 mg/dL, hemoglobin A1c (HbA1c): 101 mmol/mol or 11.4%] and insulin therapy was started. Markers of autoimmune diabetes (i.e., anti-glutamic acid decarboxylase, anti-islet antigen-2 autoantibodies) were negative. At the age of 4 yr, the patient underwent polysomnography because of episodes of nocturnal apneas reported by his mother; the exam did not show any obvious signs of central or peripheral apnea or any other electroencephalogram (EEG) abnormality. At about the same age, the patient showed speech delays necessitating therapy. In addition, the patients had learning difficulties, especially concerning reading–writing and drawing-specific geometric symbols that required teaching assistant at school. From the age of 9 yr. the child presented episodic headache, classified as migraine. A year later, he was admitted to the Child Neurology Unit of Catholic University in Rome because of an occipital epileptic seizure with secondary generalization consisting of dizziness, visual hallucinations (flashing stars), loss of consciousness, and generalized tonic-clonic jerks. The duration of the seizure was of 2–3 min with spontaneous recovery. Glycemic values were in the normal range at the time of the crisis (i.e., no hypoglycemia). EEG showed focal spikes on the posterior regions and diffuses paroxysmal activities (brief, irregular spikes-waves discharges) with activation during intermittent photic stimulation and in the first stage of sleep. However, neurological and ophthalmological examinations were normal immediately after the seizure episode. Brain magnetic resonance imaging performed a week after the crisis was also normal and single photon emission computed tomography showed normal perfusion. No antiepileptic drug was prescribed, but EEG examination was scheduled every 6 months.
The combination of diabetes with neurological symptoms prompted investigation of the KCNJ11 gene [3], by DNA direct sequencing as described [1, 5]; the mutation was then confirmed on individual clones after TA-TOPO cloning. Functional assessment of recombinant KATP channel was performed in COSm6 cells to simulate the heterozygous condition of the patient by coexpression of wild-type and mutant Kir6.2 subunits together with SUR1 subunits, as described previously [4, 7]. Because patients in whom the switch from insulin to SU is attempted during childhood or adulthood and/or with neurological symptoms may require high doses of glyburide (Glyb) [7, 9-12]. drug plasma levels during administration were monitored by mass spectroscopy (with modifications [15]).
The Wechsler Intelligence Scale for Children-Revised (WISC-R) was used to perform neuropsychological development. Performance subtests of the (WISC-R) consisted in matrix reasoning, picture completion, block design, and coding [16]. A discrepancy more than 15 points between Verbal IQ and Performance IQ is considered statistically significant. Visuomotor and visuoperceptual functions were assessed by using The Developmental Test of Visual-Motor Integration (VMI) including both supplementary tests (Visual Perception and Motor Coordination). These tests assess fine motor development, perceptual discrimination skills, and the ability to integrate perceptual and motor processes. The VMI consists of 27 basic geometric figures, in increasing order of difficulty, which have to be copied. The number of correct performances was judged and scored according to the manual. Poor performance was defined as mild perceptual impairment if the results were between 1 and 2 SDs (corresponding to 15th and 5th centile) from the mean of the control group, and as severe perceptual impairment if the results were below 2 SD (corresponding to a score below 5th centile) [17].
Results
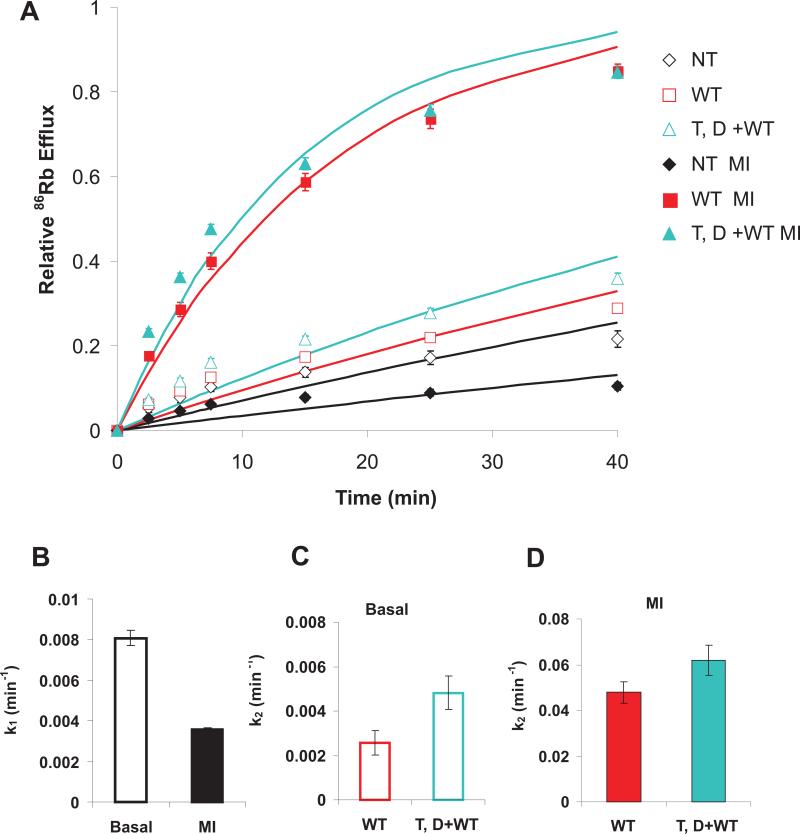
We identified the novel heterozygous mutation c. 674G->C + 676_696del (DNA level), p. Ser225Thr + Pro226_Pro232del (protein level), that appeared to have arisen de novo (Fig. S1), since no mutation was identified in either parent. In vitro studies revealed a gain-of-function for the mutant channels: wild-type channels were half inhibited at 14 μM ATP, whereas mutant channels were only half inhibited at 44 μM (Fig. 1). This result predicts that in vivo, there will be enhanced KATP channel activity under normal metabolic conditions.
Figure 1.
Sensitivity of wild-type (WT) and mutant KATP channels to ATP inhibition. Dose-response curves were obtained by exposing channels to different concentrations of ATP in Kint solutions and are fit by the Hill equation: relative current = 1/(1+{[ATP]/IC50}H) with IC50 = 14 μM (WT), and 44 μM ([S225T, del]+WT) and H = 1.6 (WT) and 1.2 ([S225T, del]+ WT).
At the time of the identification of the genetic defect, the patient was 12 yr, 10 months old, at Tanner stage 3, and his weight and height were 54.3 kg and 162.3 cm, respectively. Immediately prior to the Glyb trial, the daily insulin dose was 0.92 U/kg and HbA1c 52 mmol/mol (or 6.9%). Treatment with Glyb was initiated and the patient fully weaned from insulin in 13 d at a Glyb dose of 0.37 mg/kg/d. Glyb dosage was then tapered to a final dose of 0.09 mg/kg/d over 11 months, reaching an excellent metabolic control (HbA1c: 36 mmol/mol, or 5.4%). In addition, continuous glucose monitoring obtained every 6 months revealed greatly reduced glycemic excursions on SU as compared to insulin treatment (not shown). Glyb plasma concentration measured immediately after switch (0.37 mg/kg/d) and after 6 months (0.17 mg/kg/d) was 82 and 41.7 ng/ml, respectively. These values were comparable to those of other patients of the Italian data set with isolated diabetes or iDEND due to KCNJ11 mutations (not shown).
As shown in Table 1, overall IQ (TIQ) was found to be normal before commencement of SU treatment, but with a statistically significant discrepancy between verbal (VIQ) and performance (PIQ) subscores (112 vs. 95). In addition, before Glyb therapy the child showed both VMI total and motor coordination scores in the poor performance range (12th centile and 10th centile), showing impaired ability to integrate perceptual and motor processes and difficulties in fine motor coordination. After 1 yr of Glyb treatment, there was an improvement in PIQ that closed the gap between VIQ and PIQ scores (115 vs. 110). Furthermore, improvements in total VMI score (37th centile) and in motor coordination subtest (65th centile) were recorded, with both scores falling within the normal range.
Table 1.
Results of neurological assessment
| Before Glyb | After a year of Glyb | |
|---|---|---|
| TIQ | 105 | 114 |
| VIQ | 112 | 115 |
| PIQ | 95 | 110 |
| VMI | 12° | 37° |
| Visual perception | 42° | 30° |
| Motor coordination | 10° | 65° |
Glyb, glyburide; PIQ, performance intelligence quotient; TIQ, total intelligence quotient; VIQ, verbal intelligence quotient; VMI, visuomotor integration.VMI results are expressed as centiles.
Discussion
We described here a boy with an activating KCNJ11 mutation with an unusual combination of clinical findings, i.e.. diabetes presentation during infancy [2, 6, 18] associated with mild learning impairment and a single, major epileptic seizure at 10 yr of age. This novel mutation is different from the KCNJ11 in-frame deletion (removing Kir6.2 residues from 28 to 32) described in a patient diagnosed with isolated diabetes at the age of 3 months [19], and unusual in including both an amino acid change (S225T) and a deletion within the channel. Previously, genotype-phenotype correlations firmly established that iDEND, which combines neonatal diabetes and various degrees of developmental delay is associated with recurrent missense mutations KCNJ11/G53D, V59M. and R201C, with well established effects on KATP channel activity [1, 3, 7, 8]. Our functional studies showed a gain-of-function resulting from the combined mutation and deletion in this case. Although not particularly severe, it is important to note that the functional assessment is carried out in recombinant cells and that alterations in trafficking or in interactions with other proteins or signaling molecules that could be important in native cells may not be detected and conceivably the gain-of-function could be further enhanced in vivo. Our patient had a history of speech delay and of learning difficulties at primary school, and when examined after the seizure a significant difference between VIQ and PIQ (>17 points) and low VMI scores, mainly in the motor coordination subtest, were recorded. After 1 yr of Glyb therapy, there was an improvement in both PIQ and VMI, with the motor coordination subtest score increasing from the 10th to the 65th centile. Previously, an amelioration of motor abilities has been described in children with iDEND due to mutations KCNJ11/H46L and V59M transferred to SUs [12, 13], suggesting that a better motor coordination also contributes to improve visuoperceptual abilities and performance on cognitive tests. Interestingly, the Glyb dose employed in this case was similar to that used in patients with iDEND associated with mutation KCNJ11/V59M [9-11, 14]. Thus, considering the positive response of both diabetes and neurocognitive function to Glyb therapy, we favor the interpretation that this novel KCNJ11 mutation is responsible for both conditions, and that our patient is likely affected by a very mild form of iDEND. However, we recognize that the description of additional patients with similar clinical features is needed to substantiate our hypothesis.
As for the epileptic episode that brought the patient to our attention, clinical and EEG semiology were suggestive of occipital seizures, resembling those observed in Gastaut childhood occipital epilepsv [20, 21], which generally occur in the same age range of our subject, and are also associated with photoparoxysmal responses and headaches. Thus, in consideration of the major differences observed between our patient and those with DEND [4, 12] in terms of time of onset of epilepsy, clinical features, and EEG findings, we believe that patient's seizure was likely coincidental.
We conclude that the combination of non-autoimmune diabetes in childhood with even mild neurological symptoms warrants the analysis of genes encoding KATP.
Acknowledgements
Part of this work was supported by the grant Fondazione Roma ‘Molecular mechanisms in the pathogenesis of type 2 diabetes mellitus and its cardiovascular complications’ to Fabrizio Barbetti and by Transnational European research grant on Rare Diseases (ERANET 09 RARE 005).
Funded by
Fondazione Roma
Transnational European research grant
Footnotes
How to Cite
Battaglia D Lin Y-W Brogna C Crinò A Grasso V Mozzi AF Russo L Spera S Colombo C Ricci S Nichols CG Mercuri E Barbetti F. Glyburide ameliorates motor coordination and glucose homeostasis in a child with diabetes associated with the KCNJ11/S225T, del226-232 mutation
Supporting Information
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
References
- 1.Gloyn AL, Pearson ER, Anteliff JF, et al. Activating mutations in the gene encoding the ATP-sensitive potassium-channel subunit Kir6.2 and permanent neonatal diabetes. N Engl J Med. 2004;350:1838–1849. doi: 10.1056/NEJMoa032922. [DOI] [PubMed] [Google Scholar]
- 2.Yorifuji T, Nagashima K, Kurokawa K, et al. The C42R mutation in the Kir6.2 (KCNJ11) gene as a cause of transient neonatal diabetes, childhood diabetes or later-onset, apparently type 2 diabetes. J Clin Endocrinol Metab. 2005;90:3174–3178. doi: 10.1210/jc.2005-0096. [DOI] [PubMed] [Google Scholar]
- 3.Hattersley AT, Ashcroft FM. Activating mutations in Kir6.2 and neonatal diabetes: new clinical syndromes, new scientific insights, and new therapy. Diabetes. 2005;54:2503–2513. doi: 10.2337/diabetes.54.9.2503. [DOI] [PubMed] [Google Scholar]
- 4.Masia R, Koster JC, Tumini S, et al. An ATP-binding mutation (G334D) in KCNJ11 is associated with a sulfonylurea-insensitive form of DEND (Developmental Delay, Epilepsy, and Neonatal Diabetes). Diabetes. 2007;56:328–336. doi: 10.2337/db06-1275. [DOI] [PubMed] [Google Scholar]
- 5.Massa O, Iafusco D, D'Amato E, et al. KCNJ11 mutations in Italian patients with permanent neonatal diabetes. Hum Mutat. 2005;25:2–27. doi: 10.1002/humu.20124. [DOI] [PubMed] [Google Scholar]
- 6.Russo L, Iafusco D, Brescianini S, et al. Permanent diabetes during the first year of life: multiple gene screening in 54 patients. Diabetologia. 2011;54:1693–1701. doi: 10.1007/s00125-011-2094-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koster JC, Cadario F, Peruzzi C, Colombo C, Nichols CG, Barbetti F. The G53D mutation in Kir6.2 (KCNJ11) is associated with neonatal diabetes and motor dysfunction in adulthood that is improved with sulfonylurea therapy. J Clin Endocrinol Metab. 2008;93:1054–1061. doi: 10.1210/jc.2007-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clark RH, McTaggart JS, Webster R, et al. Muscle dysfunction caused by a KATP channel mutation in neonatal diabetes is neuronal in origin. Science. 2010;329:458–461. doi: 10.1126/science.1186146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pearson ER, Flechtner I, Njolstad PR, et al. Switching from insulin to oral sulfonylureas in patients with diabetes due to Kir6.2 mutations. N Engl J Med. 2006;355:467–77. doi: 10.1056/NEJMoa061759. [DOI] [PubMed] [Google Scholar]
- 10.Tonini G, Bizzarri C, Bonfanti R, et al. Sulphonylurea treatment outweighs insulin therapy in short-term metabolic control of patients with permanent neonatal diabetes mellitus due to activating mutations of the KCNJ11 gene. Diabetologia. 2006;49:2210–2213. doi: 10.1007/s00125-006-0329-x. [DOI] [PubMed] [Google Scholar]
- 11.Iafusco D, Bizzarri C, Cadario F, et al. No beta cell desensitisation after a median of 68 months on glyburide therapy in patients with KCNJll-associated permanent neonatal diabetes. Diabetologia. 2011;54:2736–2738. doi: 10.1007/s00125-011-2273-7. [DOI] [PubMed] [Google Scholar]
- 12.Shimomura K, Horster F, de Wet H, et al. A novel mutation causing DEND syndrome: a treatable channelopathy of pancreas and brain. Neurology. 2007;69:1342–1349. doi: 10.1212/01.wnl.0000268488.51776.53. [DOI] [PubMed] [Google Scholar]
- 13.Mlynarski W, Tarasov AI, Gach A, et al. Sulfonylurea improves CNS function in a case of intermediate DEND syndrome caused by a mutation in KCNJ11. Nat Clin Pract Neurol. 2007;3:640–645. doi: 10.1038/ncpneuro0640. [DOI] [PubMed] [Google Scholar]
- 14.Slingerland AS, Nuboer R, Hadders-Algra M, Hattersley AT, Bruining GJ. Improved motor development and good long-term glycaemic control with sulfonylurea treatment in a patient with the syndrome of intermediate developmental delay, early-onset generalised epilepsy and neonatal diabetes associated with the V59M mutation in the KCNJ11 gene. Diabetologia. 2006;49:2559–2563. doi: 10.1007/s00125-006-0407-0. [DOI] [PubMed] [Google Scholar]
- 15.Mistri HN, Jangid AG, Shrivastav PS. Liquid chromatography tandem mass spectrometry method for simultaneous determination of antidiabetic drugs metformin and glyburide in human plasma. J Pharm Biomed Anal. 2007;45:97–106. doi: 10.1016/j.jpba.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Wechsler D. Wechsler Intelligence Scale for Children. 3rd edn. Psychological Corporation; San Antonio: 1992. [Google Scholar]
- 17.Beery KE. Developmental Test of Visual-Motor Integration. Modern Curriculum Press; Cleveland: 1989. [Google Scholar]
- 18.Rubio-Cabezas O, Flanagan SE, Damhuis A, Hattersley AT, Ellard S. K(ATP) channel mutation in infants with permanent diabetes diagnosed after 6 months of life. Pediatr Diabetes. 2012:XIII. doi: 10.1111/j.1399-5448.2011.00824.x. [DOI] [PubMed] [Google Scholar]
- 19.Crai TJ, Shimomura K, Holl RW, Flanagan SE, Ellard S, Ashcroft FM. An in-frame deletion in Kir6.2 (KCNJ11) causing neonatal diabetes reveals a site of interaction between Kir6.2 and SUR1. J Clin Endocrinol Metab. 2010;94:2551–2557. doi: 10.1210/jc.2009-0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caraballo RH, Cersósimo RO, Fejerman N. Childhood occipital epilepsy of Gastaut: a study of 33 patients. Epilepsia. 2008;49:288–297. doi: 10.1111/j.1528-1167.2007.01322.x. [DOI] [PubMed] [Google Scholar]
- 21.Andermann F. Migraine and the benign partial epilepsies of childhood: evidence for an association. Epileptic Disord. 2000;1:S37–S39. [PubMed] [Google Scholar]