Abstract
Objectives
This study assessed HPV vaccination and its correlates among culturally diverse 18–26 year-old community college women in Los Angeles. Specific research questions were: (1) What proportion of respondents have initiated the HPV vaccine, and what proportion have completed the three-dose series? (2) What demographic (e.g., age, ethnicity), psychosocial (e.g., vaccine-related beliefs, perceived social norms), and health care-related variables (e.g., health insurance status, provider recommendation, health care trust and satisfaction) are associated with vaccine initiation for this sample?
Method
Participants were recruited from the campus of a community college in central Los Angeles. All female students between 18 and 26 were eligible to participate. An anonymous web-based survey assessed number of HPV vaccine doses received as well as demographic information, HPV- and HPV vaccine-related knowledge, attitudes, and behavior, perceived social norms, provider & health care system factors, sexual behavior, cervical health, and mother-daughter communication about sex. Analyses were conducted using 178 surveys. Multivariate logistic regression tested the relationships of statistically significant bivariate predictors to vaccine initiation.
Results
Those who initiated the vaccine were younger, more often had a health-related academic major, thought the vaccine to be safer, perceived HPV severity lower, and perceived higher social approval for HPV vaccination than those unvaccinated. All who had initiated the vaccine had a doctor’s recommendation.
Conclusion
To increase uptake among 18–26-year-old women, research should explore provider interventions to increase vaccine recommendation, and also identify individuals and groups who may have negative beliefs about vaccine safety and efficacy to provide support in vaccine decision-making.
Keywords: HPV vaccine, cervical cancer prevention, college women, community college, ethnic minority women
Two vaccines to prevent human papillomavirus (HPV) infection have been introduced in recent years. Both vaccines protect against the two strains of HPV that cause 70% of cervical cancers [1,2]. The Advisory Council on Immunization Practices (ACIP) recommends routine vaccination of girls 11–12 years old with either vaccine, and “catch-up” vaccination for females 13–26 years of age who were not previously vaccinated [3]. Wide use of HPV vaccines could drastically reduce morbidity and mortality associated with cervical cancer in the U.S. However, only a small proportion of eligible women have initiated the vaccine series, with women ages 18 to 26 lagging behind those 11 to 17 [4–6], and persistent ethnic disparities in rates of vaccine initiation and completion [4–7]. Understanding and increasing vaccine uptake for 18–26-year-olds is particularly important, as risk for acquiring HPV increases rapidly for many women during these years [8,9].
Existing research among 18–26-year-old women has identified HPV-vaccine-related knowledge, attitudes and beliefs [7,10,11], social approval and parent-daughter communication about sex [12], and healthcare-related factors like provider recommendation, provider practice specialty, recency of healthcare visits, and insurance type [6,11,13], in addition to age and ethnicity [5,10] as factors related to vaccine uptake.
However, much of the prior research among the 18–26-year-old age group has focused on young women in four-year universities and managed care plans [5,6,10,11], samples that may differ substantially from other segments of the population in health care access and socioeconomic status. Few studies have focused on ethnically diverse community samples, and no research to date on HPV vaccine uptake has focused specifically on community college women.
Objectives
This study assessed HPV vaccine initiation and its correlates in a sample of culturally diverse 18–26 year-old women recruited from a community college campus in Los Angeles. Specific research questions were:
What proportion of respondents have initiated the HPV vaccine, and what proportion have completed the three-dose series?
What demographic (e.g., age, ethnicity), psychosocial (e.g., vaccine-related beliefs, perceived social norms), and health care-related variables (e.g., health insurance status, provider recommendation, health care trust and satisfaction) are associated with vaccine initiation for this sample?
Method
Participants and Recruitment
Participants were recruited from the campus of a community college in central Los Angeles with total enrollment of 15,037. Enrolled students were 45% female, and approximately 45% were 26 years of age or younger. The ethnic composition of the school was 55% Hispanic/Latino, 30% African American, 7.5% Asian American, and 7% White students [14]. All female students between 18 and 26 years of age were eligible to participate in the study. The research team recruited participants in person and with posted fliers, class announcements, and word of mouth. Interested students self-selected to participate. Recruitment took place from September to November 2011. The UCLA Institutional Review Board approved the study protocol, and community college administrators granted necessary permissions.
Survey Procedures
An anonymous web-based survey was used to collect data. Surveys were administered in two ways:
In person: One day per week during the data collection period, the principal investigator collected data using laptop computers in a designated conference room on campus, and was present while participants completed the surveys.
Remote: Participants were also able to log on to the survey website to self-administer the survey from any computer, at their convenience, with no study staff present.
In both cases, participants entered the survey web address (printed on all recruitment materials), read the online consent form, and indicated consent by clicking a button at the bottom of the page. The survey used skip logic to administer only relevant questions based on participants’ responses, and took 20–30 minutes to complete. Participants received a $10 gift card and printed information from the CDC on HPV, cervical cancer screening, and the HPV vaccines. Women who completed the survey in person (n=160) received their incentives immediately; those who completed the survey remotely (n=91) entered their name and address in a separate online form to receive incentives by mail.
Survey Instrument
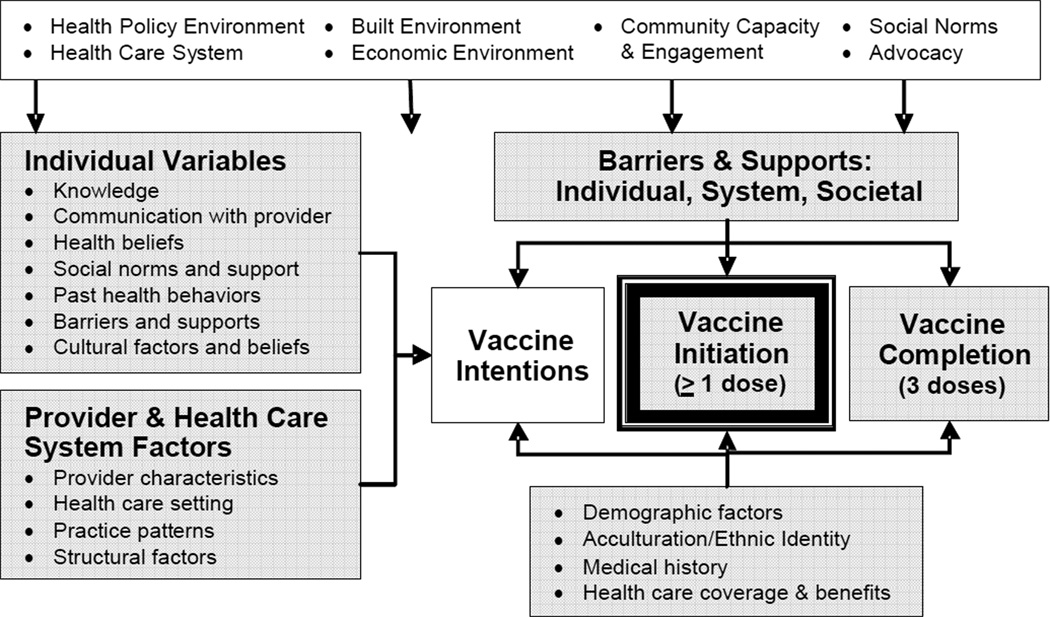
The Health Behavior Framework (HBF) [15] informed the constructs included in the survey (see Figure 1). The HBF is a theoretical framework for conceptualizing multiple influences on health behavior change, informed by social and cognitive theories of behavior and incorporating contextual factors (such as neighborhood resources or access to health insurance) in describing health behavior change [15].
Figure 1.
Health Behavior Framework
Survey items were drawn from measures used in prior studies of HPV vaccination [12,16,17], adolescent sexual behavior [18], and health care experiences and trust [19]. The main outcome of interest was HPV vaccine initiation. The survey included constructs in six main areas:
Demographic information: Age, gender, ethnicity, major in school, income, and relationship status.
- HPV- and HPV vaccine-related knowledge, attitudes, and behavior:
- HPV awareness and knowledge [7]: One question (yes/no) determined whether participants had heard of human papillomavirus or HPV ‘before today.’ Eleven true/false items measured participants’ knowledge of HPV, e.g., ‘HPV can cause cervical cancer.’ The number of items answered correctly was summed to create a scale score.
- Perceived vulnerability and severity of HPV [17]: One item, ‘I am likely to contract the HPV virus in my lifetime’ assessed perceived vulnerability to HPV infection, and a second item, ‘Getting the HPV virus would be a serious health problem for me’ evaluated perceived severity. Responses were on Likert-type scales from 1/strongly agree to 4/strongly disagree.
- HPV vaccine awareness and beliefs [17]: One item (yes/no) asked whether respondents had heard of a vaccine for HPV ‘before today.’ Perceived vaccine safety was measured with four items about perceptions of vaccine side effects, thoroughness of testing, potential to cause health problems, and overall safety. Responses were on Likert-type scales from 1/strongly disagree to 4/strongly agree. The items were reverse-scored as needed and averaged to create a mean score for perceived safety (current sample alpha=.65). Perceived vaccine effectiveness was measured with three items assessing perceptions of the vaccine’s effectiveness in preventing HPV, cervical cancer, and genital warts. Responses ranged from 3/very effective to 1/not at all effective.’ Scores were averaged (alpha=.65).
- HPV vaccine uptake [17]: One item assessed whether respondents had received any doses of the HPV vaccine; responses were coded 1=yes, 0=no/don’t know. A second item asked how many doses those who had initiated the vaccine had received (‘1/2/3/don’t know’).
Perceived social norms: Five items adapted from Roberts and colleagues [12] assessed perceptions of approval for getting the HPV vaccine among valued others (partner, parents, other family, friends, and medical provider). Responses ranged from 4/strongly approve to 1/strongly disapprove. Approval scores were averaged to create a mean approval score. Alpha was not calculated because many participants responded about only one or two valued others.
- Provider & health care system factors:
- Provider recommendation [17]: One item, ‘have you ever been offered the HPV vaccine by your doctor or nurse?’ assessed presence of a provider recommendation. Responses were coded 1 (yes) or 0 (no/don’t know).
- Health care satisfaction and trust: Six items adapted from the Primary Care Assessment Survey (PCAS) [19] asked whether respondents had a regular doctor and their frequency of doctor visits in recent years. Two additional subscales assessed respondents’ perceptions of interpersonal treatment at the doctor’s office (e.g., doctor’s caring and concern), and trust of their medical provider (e.g., doctor has respondent’s best interests in mind). The PCAS scales demonstrated internal consistency in the current sample of .82 for trust and .96 for satisfaction.
- Access to health care [17]: Two items assessed participants’ health insurance status (public/private/none), and whether they had a regular medical provider (yes/no).
- Sexual behavior, sexual health, and mother-daughter communication about sex:
- Sexual behavior: One item [18] asked whether respondents had ever had sexual intercourse (yes/no).
- Cervical health history: Two items created for this survey assessed timing of respondents’ most recent Pap test (<1 year/1–3 years/>3 years/never), and history of abnormal Pap tests (yes/no/don’t know).
- Mother-daughter communication about sex: Seven items adapted from Roberts and colleagues [12] asked how much the participant and her mother/mother figure had discussed sexual topics including puberty, sexual intercourse, when to start having sex, contraception/birth control, HIV/AIDS, other sexually transmitted diseases, and HPV. Reponses were on 4-point scales from 1/not at all to 4/sufficiently. Item scores were averaged to create a scale score, which had good reliability for this sample (alpha=.92).
Data Analysis
Data were screened for errors, improbable values, and duplicate submissions. Cases with multiple incentive requests to the same address were considered possible duplicates. The first of such cases were retained (i.e., the survey with the earliest date and time), and the rest were omitted from analyses. It is possible that this method omitted non-duplicate surveys from eligible participants in the same household, but we chose this strategy as a conservative approach to reducing the possibility of duplicate or fabricated responses. Cases with >20% incomplete responses, or which indicated male gender or age outside the 18–26 range, or reported attending a school other than a local community college were also omitted. This left a total of 178 surveys, 145 of which were completed in person and 33 completed remotely.
Bivariate analyses were used to compare participants using the two survey modes on demographic, predictor, and outcome variables. Those who completed the survey remotely perceived greater vaccine safety (t=2.63, p=.01) and effectiveness (trend; t=1.87, p=.06), and lower severity of HPV (t= −2.71, p=.01), than those who completed in person. Remote respondents were also more likely to have been born outside the U.S. (χ2=3.74, p=.05) and to attend a community college other than the primary site (χ2=21.06, p<.01). No other differences were observed by survey mode. This variable was added to final logistic regression models as a control.
Missing data (on average <5% among the usable surveys) were deleted listwise from analyses. Descriptive statistics were used to characterize the sample as a whole, and t-tests and chi-square analyses were used to compare means on predictor variables between women who had received ≥1 dose of HPV vaccine and those who had not. Predictor variables with statistically significant bivariate relationships (p<.10) with HPV vaccine initiation were included along with demographic control variables, in a multivariate logistic regression model to predict vaccine initiation.
Results
Analyses were conducted using 178 surveys. The sample was 21.6 years of age on average, and predominantly Latina (59%) and African American (32%). Full demographic information is displayed in Table 1. Most (80%) had heard of HPV and 70% had heard of a vaccine for HPV. Forty-five respondents (25%) had initiated the vaccine. Of these, 31% had received one dose, 26% had received two doses, and 43% had completed all 3 doses. Age at first dose ranged from 13 to 25, with a mean of 18 and a mode of 16. The most common reasons for getting the vaccine were having a doctor’s recommendation (n=37), wanting to prevent cervical cancer (n=20), and having a mother who recommended the vaccine (n=18). Among those who had heard of the vaccine but had not received any doses (n=77), 73% reported they had ‘never thought about’ or were ‘undecided about getting the HPV vaccine.’ Table 2 shows descriptive statistics for each predictor variable by vaccination status.
Table 1.
Demographic and descriptive statistics
| n | Mean (SD) | ||
| Age | 178 | 21.6 (2.64) | |
| Age at vaccinationa | 43 | 18.4 (3.10) | |
| n | % of sample | % of each sub-sample who initiated vaccine |
|
| Ethnicity | |||
| Hispanic/Latina | 105 | 59.0 | 24.8 |
| African American | 56 | 31.5 | 26.8 |
| Asian American | 4 | 2.2 | 50.0 |
| White | 2 | 1.1 | 50.0 |
| Other/prefer not to answer | 10 | 5.6 | 10.0 |
| Majorb | |||
| Health-related | 89 | 50.0 | 31.5 |
| Not health-related | 89 | 50.0 | 19.1 |
| Education | |||
| Not yet finished high school | 11 | 6.2 | 9.1 |
| Some college | 128 | 72.3 | 26.6 |
| 2-year degree | 21 | 11.9 | 38.1 |
| 4-year degree or more | 5 | 2.8 | 20.0 |
| Prefer not to answer | 12 | 6.8 | 8.3 |
| Annual income | |||
| $0 – $19,999 | 129 | 72.9 | 25.6 |
| $20,000 or more | 26 | 14.6 | 31.8 |
| Prefer not to answer | 22 | 12.4 | 18.2 |
| Relationship status | |||
| Married / in a committed relationship | 64 | 36.8 | 29.7 |
| Single, dating, separated, divorced, or widowed | 110 | 63.2 | 23.6 |
| Ever had intercourse | |||
| Yes | 139 | 79.4 | 25.2 |
| No | 29 | 16.6 | 27.6 |
| Prefer not to answer | 7 | 3.9 | 28.6 |
| Heard of HPV | |||
| Yes | 140 | 78.7 | 30.0 |
| No / don’t know | 36 | 20.2 | 8.3 |
| Heard of HPV vaccine | |||
| Yes | 123 | 69.9 | 36.9 |
| No / don’t know | 53 | 30.1 | n/a |
| Received any vaccine dosesa | |||
| Yes | 45 | 25.3 | |
| No / don’t know | 77 | 43.3 | n/a |
| How many dosesa | |||
| 1 | 13 | 31.0 | |
| 2 | 11 | 26.2 | |
| 3 | 18 | 42.9 | n/a |
These items were asked only of women who had heard of the HPV vaccine, so totals add to <178.
Health-related majors included biology, psychology, nursing/medicine, and related fields.
Table 2.
Bivariate comparisons between vaccinated and unvaccinated women
| Initiated Vaccine | No Vaccine | |||||||||||
| n | Mean | SD | Min | Max | n | Mean | SD | Min | Max | t | p | |
| Age | 45 | 21.0 | 2.60 | 18 | 26 | 77 | 21.9 | 2.63 | 18 | 26 | 1.95 | .05 |
| HPV knowledge (sum correct out of 11) | 42 | 6.5 | 2.35 | 1.0 | 11.0 | 65 | 6.4 | 1.85 | 3.0 | 10.0 | −.29 | .78 |
| Perceived vulnerability | 42 | 2.3 | .89 | 1.0 | 4.0 | 65 | 2.5 | .90 | 1.0 | 4.0 | 1.21 | .23 |
| Perceived severity | 42 | 3.3 | .72 | 1.0 | 4.0 | 65 | 3.6 | .59 | 2.0 | 4.0 | 1.86 | .07 |
| Perceived vaccine safety | 45 | 3.1 | .50 | 1.8 | 4.0 | 77 | 2.8 | .48 | 1.8 | 3.8 | −3.56 | <.01 |
| Perceived vaccine effectiveness | 45 | 2.3 | .49 | 1.7 | 3.0 | 77 | 2.2 | .47 | 1.0 | 3.0 | −1.60 | .11 |
| Perceived social approval | 38 | 3.7 | .42 | 2.5 | 4.0 | 72 | 3.4 | .57 | 2.0 | 4.0 | −2.98 | <.01 |
| Mother-daughter communication about sex | 44 | 2.8 | .92 | 1.0 | 4.0 | 77 | 2.8 | .89 | 1.0 | 4.0 | −.08 | .94 |
| Doctor satisfaction | 43 | 3.4 | .67 | 1.0 | 4.0 | 73 | 3.3 | .73 | 1.4 | 4.0 | −.50 | .62 |
| Doctor trust | 43 | 3.2 | .70 | 2.0 | 4.0 | 74 | 3.2 | .60 | 1.7 | 4.0 | −.41 | .68 |
| n | % | n | % | chi2 | p | |||||||
| Ethnicity | ||||||||||||
| Latina/Hispanic | 26 | 57.8 | 43 | 55.8 | .23 | .89 | ||||||
| African American | 15 | 33.3 | 25 | 32.5 | ||||||||
| Other / Pref not answer | 4 | 8.9 | 9 | 11.7 | ||||||||
| Have health insurance | ||||||||||||
| Yes | 31 | 68.9 | 50 | 64.9 | .20 | .66 | ||||||
| No | 14 | 31.1 | 27 | 35.1 | ||||||||
| Have a regular doctor | ||||||||||||
| Yes | 36 | 81.8 | 50 | 65.8 | 3.53 | .06 | ||||||
| No | 8 | 18.2 | 26 | 34.2 | ||||||||
| Offered vaccine by doctor | ||||||||||||
| Yes | 45 | 100.0 | 19 | 24.7 | 64.61 | <.01 | ||||||
| No / don’t know | 0 | 0.0 | 58 | 75.3 | ||||||||
| Ever had intercourse | ||||||||||||
| Yes | 35 | 78.0 | 62 | 80.5 | .28 | .87 | ||||||
| No | 8 | 17.8 | 11 | 14.3 | ||||||||
| Pref not answer | 2 | 4.4 | 4 | 5.2 | ||||||||
| Pap screening | ||||||||||||
| </= 1 year ago | 23 | 52.3 | 42 | 55.3 | 1.95 | .58 | ||||||
| > 1 year ago | 9 | 20.5 | 20 | 26.3 | ||||||||
| Never | 8 | 18.2 | 11 | 14.5 | ||||||||
Chi-square and t-test analyses were used to make bivariate comparisons between vaccinated and unvaccinated groups on all potential predictors (see Table 2). Vaccinated women were younger, perceived the vaccine to be safer, perceived HPV severity to be lower, reported more social approval, more often had a doctor’s recommendation for the vaccine, and more often had a regular doctor compared to women who had not received the vaccine (all, p<.10).
Finally, multivariate logistic regression was used to test the relationships of statistically significant bivariate predictors to vaccine initiation in a regression model. Demographic and control variables included in the model were age, ethnicity, relationship status, major in school, and survey mode (in person or remote). Predictors were perceived HPV severity, perceived HPV vaccine safety, perceived social approval for HPV vaccination, and having a regular doctor. Having a doctor’s recommendation was not included in the model because 100% of women who had gotten the vaccine reported having a doctor’s recommendation. The model correctly classified 78.7% of participants into groups by vaccination status, and Hosmer-Lemeshow fit statistics indicated no model misspecification (χ2=12.45, p=.13).
In the full logistic regression model (see Table 3), younger respondents and those with a health-related major were more likely to have initiated the vaccine. Those who thought the vaccine to be safer and perceived higher social approval for HPV vaccination were also more likely to have been vaccinated than those who perceived lower safety or less approval. Finally, those who rated HPV severity lower were more likely to have gotten the vaccine. No differences by ethnicity were observed in either bivariate or multivariate analyses.
Table 3.
| B | SE | df | p | OR | CI | |
|---|---|---|---|---|---|---|
| Age | −.24 | .12 | 1 | .04 | .79 | [.62, .99] |
| Ethnicity | ||||||
| African American (ref) | -- | -- | -- | -- | -- | -- |
| Latina | .27 | .97 | 1 | .78 | 1.31 | [.20, 8.67] |
| Other | −.14 | 1.04 | 1 | .89 | .87 | [.11, 6.68] |
| Relationship status | ||||||
| Single/dating/other (ref) | -- | -- | -- | -- | -- | -- |
| Married/committed | −.12 | .58 | 1 | .84 | .89 | [.29, 2.75] |
| Major | ||||||
| Health-related (ref) | -- | -- | -- | -- | -- | -- |
| Not health-related | −1.21 | .56 | 1 | .03 | .30 | [.10, .90] |
| Survey mode | ||||||
| In person (ref) | -- | -- | -- | -- | -- | -- |
| Remote | .50 | .67 | 1 | .45 | 1.66 | [.45, 6.11] |
| Perceived HPV severity | −.89 | .43 | 1 | .04 | .41 | [.18, .95] |
| Perceived HPV vaccine safety | 1.31 | .61 | 1 | .03 | 3.69 | [1.13, 12.09] |
| Perceived social approval | 1.36 | .67 | 1 | .04 | 3.90 | [1.05, 14.57] |
| Regular doctor | ||||||
| No (ref) | -- | -- | -- | -- | -- | -- |
| Yes | .57 | .68 | 1 | .40 | 1.77 | [.47, 6.69] |
Vaccine initiation was coded 1=yes, 0=no/don’t know.
Analyses were conducted with only those who had heard of the vaccine and who provided data on all variables in the model.
Discussion
The goal of this study was to improve understanding of factors that may influence HPV vaccine uptake among a diverse sample of community college women 18–26 years of age. About one quarter of the sample had initiated the vaccine, but less than half of those who initiated had received all three doses. These proportions are similar to recent national estimates that 21% of eligible 19–26-year-old women have initiated the vaccine in the U.S [4]. The proportion of women who initiated the vaccine in the current sample did not differ by ethnicity. In fact, the proportions of African American and Latina women who had been vaccinated were nearly identical. These findings again parallel national estimates, which recently showed no difference in vaccine initiation between African American and Latina young women. Nationally, Latina women were significantly less likely to have gotten the vaccine than their White counterparts [4]. The number of White women in the current sample (n=2) was too small to make comparisons to other ethnic groups. Further research may be needed to understand whether cultural factors, health care-related factors, or both, account for ethnic differences in vaccine uptake among 18–26-year-olds. In any case, both current findings and national vaccination coverage results indicate that many young adult women who could benefit from the vaccine have not received it.
In the current sample, most of the women who had received the vaccine had done so by the age of 18. Beyond this age, women may not know how to access the vaccine, particularly for low-income women who age out of eligibility for the Vaccines for Children program (a national program that provides free vaccines to low-income children and adolescents, 18 years and younger) and have no other insurance coverage. Expanding public and private insurance coverage for the HPV vaccines for 19–26-year-olds could enhance rates of catch-up vaccination. Another strategy could be to encourage health providers in low-income communities (for example, community college campus student health centers) who do not currently offer the HPV vaccines to stock them, and participate in cost assistance programs. Merck, for example, provides free vaccines including Gardasil for low-income adults through its Patient Vaccine Assistance Program (http://www.merck.com/merckhelps/vaccines/); GlaxoSmithKline has a similar program that covers Cervarix (http://www.gsk-vap.com/index.html). This strategy is only viable if clinics can afford to stock the vaccines, if enough demand exists for the vaccines, and if a sufficient number of patients can also pay for vaccines by other means (e.g., insurance or self-pay). However, for clinics like the student health center at the participating campus, this could help provide HPV vaccines to eligible women who might not get them elsewhere.
Similar to prior research [12], we found that having a provider’s recommendation – expressed here as having been “offered” the vaccine – was the factor most strongly associated with vaccination. The wording of the question in this survey, “Have you ever been offered the vaccine by your doctor or nurse?” suggests that the health care provider would have initiated discussion about the HPV vaccine. Since prior research shows that providers sometimes miss opportunities to recommend the HPV vaccine (e.g., [11,20] simple interventions could prompt health providers to make a vaccine recommendation when indicated (e.g., automatic computer reminders for age-eligible patients as mentioned by Chao and colleagues [5]. Interventions could also encourage eligible patients to broach the topic if health providers do not.
Younger age was another predictor of vaccine uptake, consistent with several prior surveys of college-aged women [5–7,11,13]. This may reflect a belief among women that they may not benefit from the vaccine as they get older, which is not necessarily true. The current study found that a sizeable proportion (17%) of respondents had never had sex, and the proportion of sexually naïve was larger for the younger participants. Since the vaccine is most effective when given before sexual initiation, there may be a significant proportion of younger college age women who could receive maximum benefit from vaccination. Moreover, even women who have initiated sexual activity may benefit from the HPV vaccines, if they have not yet been exposed to all the high-risk HPV types the vaccines protect against [9]. Efforts to improve vaccine coverage may need to specifically target the 18–26-year-old age group, and particularly emphasize the benefit of the vaccine for women who have not initiated sexual activity or who have limited sexual exposure.
Two other predictors hold particular promise for intervention. Perceptions that the HPV vaccines were safe, and that valued others approved (or would approve) of the HPV vaccine, were positively related to vaccine uptake. Given the cross-sectional nature of the data, it is possible that these perceptions were positively biased by having received the vaccine. Still, given the strong associations we observed among these variables, improving positive perceptions and social support for the vaccine could improve uptake. Given recent media attention to safety concerns, interventions to increase uptake should highlight the vaccine’s excellent safety record [21,22], teach where to find accurate safety information (e.g., the CDC website), and possibly encourage media literacy (i.e., critical thinking about media messages) when interpreting safety claims in the popular media. Interventions to encourage uptake might also include a component to improve social norms, such as encouraging women to ‘tell a friend’ if they get the vaccine.
Finally, having a health-related major was associated with greater odds of having received the vaccine. Perhaps this is an example of health education influencing health behavior, or it is also possible that an interest in health led to both HPV vaccination and to a health-related major and future career. If parents or other family were also in health careers, this may have influenced their decisions to get the HPV vaccine for their daughters. It may be important to attend to academic major as a stratification variable in future interventions among college women and HPV vaccination.
Limitations and Strengths
This study had some limitations. First, all data were self-reported, which may have introduced inaccuracy [23] or socially desirable responding, though the survey was anonymous in an effort to decrease social desirability bias. Second, the web-based nature of the study made it possible for some participants to complete the survey remotely, without the investigator present. This led to a higher rate of incomplete or improbable responses, which had to be removed, than would have been achieved with only in-person survey administration. Third, the participants were a convenience sample primarily from one community college campus in Los Angeles; therefore, these results may not generalize to other community college women, and more research is needed to understand larger patterns of HPV vaccination for this group. Finally, the cross-sectional nature of the data does not allow causal inferences to be made about relationships among predictor variables and HPV vaccination.
At the same time, this study had several strengths. The focus on community college women is a novel approach for HPV vaccine research. These women were more diverse in ethnicity and socioeconomic status than students at four-year universities in the same area. Conducting this research in partnership with a community college allowed us to reach women who have been left out of past research on HPV vaccination, and also provides infrastructure for future interventions to increase HPV vaccination and cervical cancer screening through the campus health center and other avenues. Another strength was assessment of a broad range of social and contextual constructs possibly influencing vaccination behavior, including social influences on vaccination.
In order to increase uptake among 18–26-year-old women, future research should identify individuals and groups who may have negative beliefs about the safety and efficacy of the HPV vaccines and provide accurate information to support vaccine decision-making. Developing provider interventions to increase vaccine recommendations may also be a viable way to improve catch-up vaccination rates among young women.
Acknowledgements
This research was supported by the UCLA Cancer Education and Career Development Program, NCI Grant R25 CA 87949. The authors also wish to thank the staff and students of the Los Angeles Community College District, who made this research possible.
Contributor Information
Erica Marchand, UCLA Center for Cancer Prevention & Control Research, School of Public Health, 650 Charles E. Young Drive South, A2-125 CHS, Box 956900, Los Angeles, CA 90095, p: (310) 206-8797, f: (310) 206-3566, erica.marchand@ucla.edu.
Beth A. Glenn, UCLA Center for Cancer Prevention & Control Research, School of Public Health, 650 Charles E. Young Drive South, A2-125 CHS, Box 956900, Los Angeles, CA 90095, p: (310) 206-9715, f: (310) 206-3566.
Roshan Bastani, UCLA Center for Cancer Prevention & Control Research, School of Public Health, 650 Charles E. Young Drive South, A2-125 CHS, Box 956900, Los Angeles, CA 90095, p: (310) 206-5197, f: (310) 206-3566.
References
- 1.Romanowski B, de Borba PC, Naud PS, et al. Sustained efficacy and immunogenicity of the human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine: Analysis of a randomized placebo-controlled trial up to 6.4 years. Lancet. 2009;374:1975–1985. doi: 10.1016/S0140-6736(09)61567-1. [DOI] [PubMed] [Google Scholar]
- 2.Villa LL, Costa RLR, Petta CA, et al. High sustained efficacy of a prophylactic quadrivalent human papillomavirus types 6/11/16/18 L1 virus-like particle vaccine through 5 years of follow-up. British Journal of Cancer. 2006;95:1459–1466. doi: 10.1038/sj.bjc.6603469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. Recommended adult immunization schedule – United States, 2011. MMWR. 2011;60(4):1–4. [PubMed] [Google Scholar]
- 4.CDC. Adult vaccination coverage – United States, 2010. MMWR. 2012;61(4):66–72. [PubMed] [Google Scholar]
- 5.Chao C, Velicer C, Slezak J, Jacobsen S. Correlates for human papillomavirus vaccination of adolescent girls and young women in a managed care organization. American Journal of Epidemiology. 2010;171:357–367. doi: 10.1093/aje/kwp365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dempsey A, Cohn L, Dalton V, Ruffin M. Worsening disparities in HPV vaccine utilization among 19–26 year old women. Vaccine. 2011;29(3):528–534. doi: 10.1016/j.vaccine.2010.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Licht AS, Murphy JM, Hyland AJ, Fix BV, Hawk LW, Mahoney MC. Is use of the human papillomavirus vaccine among female college students related to human papillomavirus knowledge and risk perception? Sexually Transmitted Infection. 2010;86:74–78. doi: 10.1136/sti.2009.037705. [DOI] [PubMed] [Google Scholar]
- 8.Chandra A, Mosher WD, Copen C, Sionean C. Sexual behavior, sexual attraction, and sexual identity in the United States: Data from the 2006–2008 National Survey of Family Growth. National Health Statistics Reports. 2011;36:1–28. [PubMed] [Google Scholar]
- 9.Paavonen J. At what age should we be vaccinating for human papillomavirus? Gynecologic and Obstetric Investigation. 2010;70:233–236. doi: 10.1159/000314011. [DOI] [PubMed] [Google Scholar]
- 10.Bynum SA, Brandt HM, Sharpe PA, Williams MS, Kerr JC. Working to close the gap: Identifying predictors of HPV vaccine uptake among young African American women. Journal of Health Care for the Poor and Underserved. 2011;22:549–561. doi: 10.1353/hpu.2011.0060. [DOI] [PubMed] [Google Scholar]
- 11.Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19–26: Importance of a physician’s recommendation. Vaccine. 2011;29:890–895. doi: 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]
- 12.Roberts M, Gerrard M, Reimer R, Gibbons F. Mother-daughter communication and human papillomavirus vaccine uptake by college students. Pediatrics. 2010;125(5):982–989. doi: 10.1542/peds.2009-2888. [DOI] [PubMed] [Google Scholar]
- 13.Tiro JA, Tsui J, Bauer HM, Yamada E, Kobrin S, Breen N. Uptake and correlates of the human papillomavirus vaccine among adolescent girls and young adult women: An analysis of the 2007 California Health Interview Survey. Journal of Women’s Health. 2012;21:1–10. doi: 10.1089/jwh.2011.3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Los Angeles Community College District. Research and statistics: Student characteristics. 2011 http://research.laccd.edu/student-characteristics/index.htm.
- 15.Bastani R, Glenn BA, Taylor VM, Chen MS, Nguyen TT, Stewart SL, Maxwell AE. Integrating theory into community interventions to reduce liver cancer disparities: The Health Behavior Framework. Preventive Medicine. 2010;50:63–67. doi: 10.1016/j.ypmed.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen J, Othus M, Shelton RC, Li Y, Norman N, Tom L, del Carmen MG. Parental decision making about the HPV vaccine. Cancer Epidemiology, Biomarkers & Prevention. 2010;19(9):2187–2198. doi: 10.1158/1055-9965.EPI-10-0217. [DOI] [PubMed] [Google Scholar]
- 17.Bastani R, Glenn B, Tsui J, Chang C, Marchand E, Taylor V, Singhal R. Understanding sub-optimal HPV vaccine uptake among ethnic minority girls. Cancer Epidemiology, Biomarkers, & Prevention. 2011;20:1463–1472. doi: 10.1158/1055-9965.EPI-11-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Metzler CW, Noell J, Biglan A. The validation of a construct of high-risk sexual behavior in heterosexual adolescents. Journal of Adolescent Research. 1992;7(2):233–249. [Google Scholar]
- 19.Safran DG, Kosinski M, Tarlov AR, Rogers WH, Taira DA, Lieberman N, et al. The Primary Care Assessment Survey: Tests of data quality and measurement performance. Medical Care. 1998;36(5):728–739. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Lau M, Lin H, Flores G. Factors associated with human papillomavirus vaccine-series initiation and healthcare provider recommendation in U.S. adolescent females: 2007 National Survey of Children’s Health. Vaccine. 2012 doi: 10.1016/j.vaccine.2012.02.034. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.Gee J, Naleway A, Shul I, et al. Monitoring the safety of quadrivalent human papillomavirus vaccine: Findings from the Vaccine Safety Datalink. Vaccine. 2011;29:8279–8284. doi: 10.1016/j.vaccine.2011.08.106. [DOI] [PubMed] [Google Scholar]
- 22.Haupt RM, Sings HL. The efficacy and safety of the quadrivalent human papillomavirus 6/11/16/18 vaccine Gardasil. Journal of Adolescent Health. 2011;49:467–475. doi: 10.1016/j.jadohealth.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Stupiansky NW, Zimet GD, Cummings T, Fortenberry JD, Shew M. Accuracy of self-reported human papillomavirus vaccine receipt among adolescent girls and their mothers. Journal of Adolescent Health. 2012;50:103–105. doi: 10.1016/j.jadohealth.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]