Abstract
Short-chain fatty acids, generated in colon by bacterial fermentation of dietary fiber, protect against colorectal cancer and inflammatory bowel disease. Among these bacterial metabolites, butyrate is biologically most relevant. GPR109A is a G-protein-coupled receptor for nicotinate, but recognizes butyrate with low affinity. Millimolar concentrations of butyrate are needed to activate the receptor. Although concentrations of butyrate in colonic lumen are sufficient to activate the receptor maximally, there have been no reports on the expression/function of GPR109A in this tissue. Here we show that GPR109A is expressed in the lumen-facing apical membrane of colonic and intestinal epithelial cells and that the receptor recognizes butyrate as a ligand. The expression of GPR109A is silenced in colon cancer in humans, in a mouse model of intestinal/colon cancer, and in colon cancer cell lines. The tumor-associated silencing of GPR109A involves DNA methylation directly or indirectly. Re-expression of GPR109A in colon cancer cells induces apoptosis, but only in the presence of its ligands butyrate and nicotinate. Butyrate is an inhibitor of histone deacetylases, but apoptosis induced by activation of GPR109A with its ligands in colon cancer cells does not involve inhibition of histone deacetylation. The primary changes in this apoptotic process include downregulation of Bcl-2, Bcl-xL, and cyclin D1, and upregulation of death receptor pathway. In addition, GPR109A/butyrate suppresses NF-κB activation in normal and cancer colon cell lines as well as in normal mouse colon. These studies show that GPR109A mediates the tumor-suppressive effects of the bacterial fermentation product butyrate in colon.
Introduction
The mammalian colon is the home for billions of bacteria, and these bacteria influence the biology of the host markedly, including energy balance, gene expression, immune function, and disease processes (1–3). Dietary fiber is fermented by bacteria in the colonic lumen to generate short-chain fatty acids, which are responsible for the beneficial effects of gut bacteria on intestinal/colonic health (4, 5). The presence of short-chain fatty acids in the colonic lumen is linked to decreased incidence of colorectal cancer and inflammatory bowel disease (6–9), but little is known on the molecular mechanisms involved in the maintenance of colonic health by these bacterial products. One of these short-chain fatty acids is butyrate, which functions as a tumor suppressor by inhibiting histone deacetylases (HDACs) (10, 11). Recently, we and others have identified a Na+-coupled transporter for short-chain fatty acids (12, 13). This transporter, known as SLC5A8, recognizes short-chain fatty acids and other monocarboxylates as substrates (12–17). SLC5A8 was originally identified as a tumor suppressor in colon (18) and its expression is silenced in colon cancer (18–20). The discovery that SLC5A8 is an active transporter for butyrate explains at least partly its tumor-suppressive function in colon (21–23). SLC5A8-mediated entry of butyrate from lumen into colonic epithelial cells leads to HDAC inhibition and tumor suppression. The expression of SLC5A8 in the lumen-facing apical membrane of colonocytes supports this mode of action (17, 19, 24).
Studies on the tumor-suppressive function of butyrate have focused so far mostly on its intracellular action as an HDAC inhibitor. Here we show that butyrate also elicits effects in colon cells extracellularly by serving as a ligand for GPR109A. GPR109A is a receptor for nicotinate (niacin) and mediates the lipid-lowering actions of the vitamin (25–27). Recently, Taggart et al (28) demonstrated that the ketone body β-D-hydroxybutyrate is a ligand for the receptor at physiologic concentrations. Butyrate was also able to activate the receptor with an EC50 (i.e., concentration necessary for half-maximal activation of the receptor) of ~1.6 mM. Even though the levels of butyrate in circulation are too low (~5 μM) to activate the receptor, butyrate is present at high levels (~20 mM) in colonic lumen (29). If GPR109A is expressed in the lumen-facing apical membrane of colonocytes, it might suggest that the ability of butyrate to prevent cancer and inflammation in colon may also be mediated extracellularly via the receptor without entering into cells. This rationale formed the basis of the current investigation.
Materials and Methods
Immunohistochemistry
Polyclonal antibodies against GPR109A and GPR109B were generated in rabbits. The antigenic peptides used were RKKTLGEPDNNRSTSVC and CHQEPASLEKQLG, respectively. There is only a single gene coding for nicotinate receptor (GPR109A) in mouse (30); therefore, mouse intestinal and colonic tissues were examined only for GPR109A. Human colonic biopsies were obtained during colonoscopy, after obtaining patients’ informed consent and approval from the institutional review board. Since there are two genes in humans coding for GPR109 (GPR109A and GPR109B) (30), human tissues were examined for both isoforms.
Nicotinate binding
Membranes prepared from CCD841 cells (a human colonic cell line) were used for [3H]nicotinate binding assays with a rapid filtration method (31). The interaction of butyrate with the receptor was evaluated by its ability to compete with nicotinate for binding.
Functional analysis of GPR109A
Activation of GPR109A with its ligands was examined using the activity of GIRK channels as the read-out. HEK 293 cells were transfected with a human GPR109A expression vector and used for experiments 48h later. Activation of GIRK channels by adenosine receptor A1R was used as a positive control. A cytosolic GFP expression vector (Invitrogen) was cotransfected with A1R or GPR109A expression vectors to identify transfected cells. When indicated, cells were pretreated overnight with pertussis toxin (100 ng/ml). GIRK channel activity was monitored as described previously (32).
Tissue collection
Paired normal colon and colon tumor specimens were collected from 18 adult patients with colorectal cancer, with patients’ informed consent and approval from the institutional review board (33). Wild type and ApcMin/+ mice were euthanized by CO2, and tissues from the intestinal tract were collected for RNA preparation.
RT-PCR
The PCR primers for specific genes were designed based on the nucleotide sequences available in GenBank. RT-PCR was repeated twice with each RNA sample. Hypoxanthine phosphoribosyltransferase (HPRT) was used as the internal standard. The intensities of the bands corresponding to specific gene transcripts were quantified by densitometry scanning and normalized to the intensities of corresponding HPRT bands.
Ectopic expression of human GPR109A
Cells (CCD841, a human normal colon cell line, and KM12L4, a human colon cancer cell line) were transfected with pcDNA or human GPR109A cDNA. pEGFP-N1 was used for co-transfection to determine transfection efficiency. After 24h, cells were treated with or without butyrate (1 mM) or nicotinate (1 mM) for 24h. Preparation of RNA and protein lysates was done as described previously (20). For FACS analysis, cells were fixed in 50% ethanol, treated with 0.1% sodium citrate, 1 mg/mL RNase, and 50 μg/mL propidium iodide, and subjected to fluorescence-activated cell sorting (FACS).
Western blot analysis
Fifty μg of protein was fractionated by SDS-PAGE, and the fractionated proteins were transferred onto a nitrocellulose membrane (Schleicher & Schull, Sacramento, CA). Membranes were blocked with bovine serum albumin and then exposed to respective primary antibody at 4°C overnight, followed by treatment with appropriate secondary antibody. Proteins were visualized by ECL Super Signal Western System (GE Healthcare).
HDAC activity
A commercially available kit (BioVision, Mountain View, CA) was used to determine HDAC activity in a cell-free system (34). The acetylation status of histone H3, histone H4, histone H4-Lys12, and histone H4-Lys16 was assessed by Western blot using specific antibodies as described previously (34). For normalization, the protein levels of histone H3 and histone H4 were determined with specific antibodies. The antibodies were obtained from the following sources: histone H3, acetylated histone H3, histone H4 and acetylated H4 (Upstate Biotechnology, Inc., Lake Placid, NY), acetylated H4-Lys12 (Santa Cruz Biotechnology, Inc., Santa Cruz, CA), and acetylated H4-Lys16 (Abcam, Inc., Cambridge, MA).
NF-κB-luciferase reporter assay
Cells were transfected with a NF-κB-luciferase reporter construct alone or with GPR109A cDNA. 24h later, cells were pretreated with GPR109A ligands for 4h and then treated with lipopolysaccharide (100 ng/mL) and GPR109A ligands for an additional 4h. Cells were then lysed, and the lysates used for luciferase activity. NF-κB-luciferase reporter assay was also done with colon tissue obtained from transgenic mice carrying the NF-κB-luciferase transgene under the control of β-actin promoter. Mice were euthanized by CO2, and colon was removed and everted. Tissue slices (~10 mg wet weight) were used for incubation with lipopolysaccharide with or without pretreatment with GPR109A ligands. Tissues were then homogenized and the lysates used for measurement of luciferase activity.
Results
Expression of GPR109 in mouse and human colon
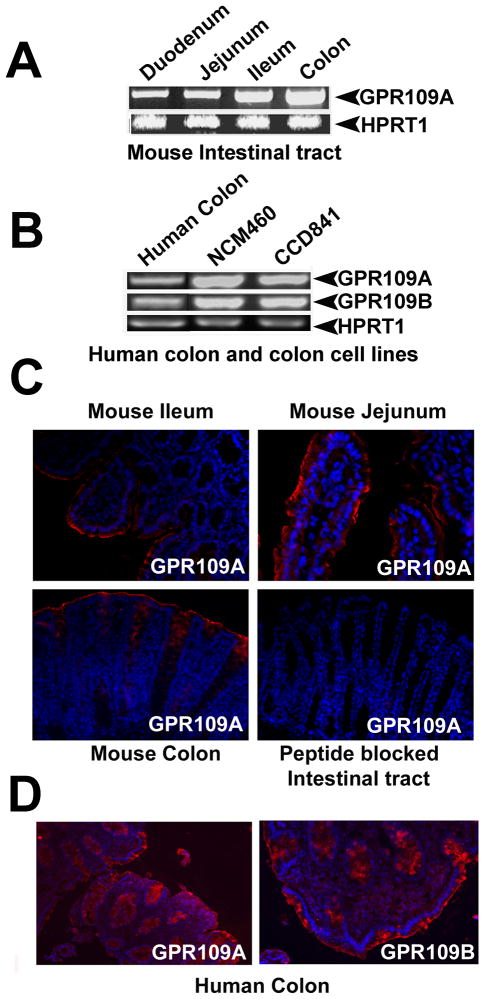
We first investigated the expression of GPR109A in mouse intestinal tract and human colon. GPR109A mRNA was detected all through the intestinal tract in mouse (Fig. 1A). The expression was lowest in the early parts of the intestinal tract and highest in the distal parts. Human colon expressed both isoforms, GPR109A and GPR109B. Two human normal colon cell lines, NCM460 and CCD841, also expressed GPR109A and GPR109B (Fig. 1B). Expression of GPR109A, analyzed by immunohistochemistry, was evident in small intestine (jejunum and ileum) as well as in large intestine in mouse (Fig. 1C). The expression was restricted to the lumen-facing apical membrane of intestinal/colonic epithelial cells. The immunopositive signals were not detected when antigen-neutralized primary antibody was used. Human colonic biopsies were examined for expression of GPR109A and GPR109B using respective antibodies (Fig. 1D). Human colon expressed both isoforms of GPR109. The expression of GPR109A as well as GPR109B in human colon was restricted to the apical membrane.
Figure 1.
Expression of GPR109A in colon. A, Expression of GPR109A mRNA in mouse intestinal tract. B, Expression of GPR109A and GPR109B mRNA in human colon and in human colon cell lines. C, Immunolocalization of GPR109A protein in mouse intestinal tract (GPR109A, red; nuclei, blue). D, Immunolocalization of GPR109A and GPR109B in human colonic biopsies (GPR109A & GPR109B, red; nuclei, blue).
Butyrate as a ligand for GPR109A
CCD841 cells were used to study nicotinate binding and interaction of butyrate with GPR109A. Specific binding of nicotinate was detected with membranes prepared from these cells; the binding was inhibited by butyrate (10 mM) (Supplementary Fig. S1A). The binding of nicotinate was of high-affinity (Kd, 245 ± 32 nM) (Supplementary Fig. S1B). The function of butyrate as a GPR109A agonist was investigated using a heterologous expression system in which the coupling of pertussis toxin-sensitive Gi proteins to the receptor was monitored with the activity of inwardly-rectifying potassium (GIRK) channels as the read-out. GIRK channels open in response to activation of pertussis toxin-sensitive G proteins (e.g., Gi and Go) (35). We used as a positive control the ability of ectopically expressed adenosine receptor A1R to activate GIRK channels in the presence of adenosine. Expression of GPR109A in HEK293 cells allowed activation of GIRK channels in the presence of nicotinate and butyrate (Supplementary Fig. S1C & D). In cells transfected with vector alone, nicotinate did not activate the channel. The involvement of GPR109A in the process was confirmed further by the effective blockade of nicotinate-induced activation of the channel by pertussis toxin. These results show that butyrate functions as an agonist for GPR109A.
Relevance of GPR109A to colon cancer
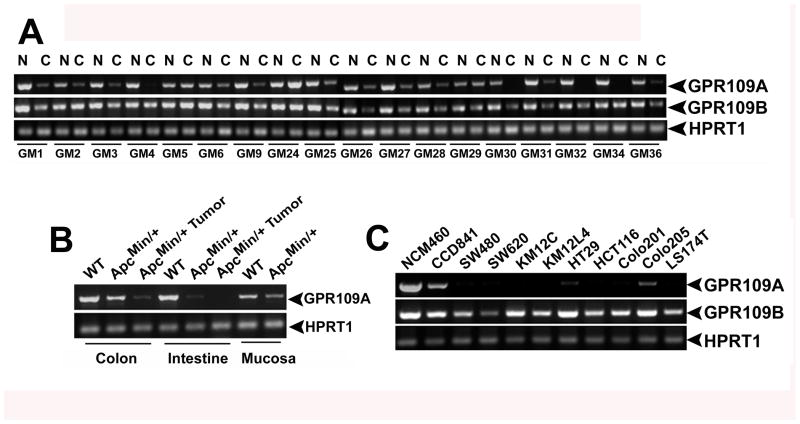
To determine the relevance of GPR109A to tumor-suppressive effects of butyrate in colon, we first examined the expression of GPR109A in normal colon and in colon cancer in humans. The receptor expression was decreased in a majority of primary colon cancer samples compared to corresponding normal colon samples (the decrease in mRNA levels was evident in 15 out of 18 paired samples) (Fig. 2A). A pair-wise comparison (cancer versus normal) with all 18 paired samples showed that the decrease in expression in cancer tissues was 83 ± 5%; p < 0.001). The levels of GPR109B mRNA were also reduced in colon cancer, but the decrease was much smaller (34 ± 8%, p < 0.05). We also examined the expression of GPR109A in a mouse model of intestinal/colon cancer (ApcMin/+ mouse) (Fig. 2B). The expression of the receptor mRNA was evident in colon, small intestine, and intestinal mucosal scrapings from wild type mouse. The expression levels decreased markedly in tumor-bearing regions of colon and intestine from ApcMin/+ mouse. Even in regions where there was no evidence of tumor, the expression was reduced significantly in ApcMin/+ mouse compared to wild type mouse. We then monitored the expression levels of GPR109A and GPR109B in normal and cancer colon cell lines of human origin (Fig. 2C). The normal cell lines CCD841 and NCM460 expressed the receptor; but the expression was reduced markedly in cancer cell lines (SW480, SW620, KM12C, KM12L4, HT29, HCT116, Colo201, Colo205, and LS174T). The expression of GPR109B was not significantly different in cancer cell lines compared to normal cell lines.
Figure 2.
Silencing of GPR109A in colon cancer. A, Expression of GPR109A and GPR109B in normal colon and paired colon cancer tissues from 18 patients as assessed by RT-PCR. B, Expression of GPR109A in the colon and intestine of wild type and ApcMin/+ mice. In ApcMin/+ mice, the tissues were collected from tumor sites and also from areas with no tumor. C, Comparison of expression of GPR109A and GPR109B by RT-PCR between normal colon cell lines (NCM460 and CCD841) and cancer colon cell lines.
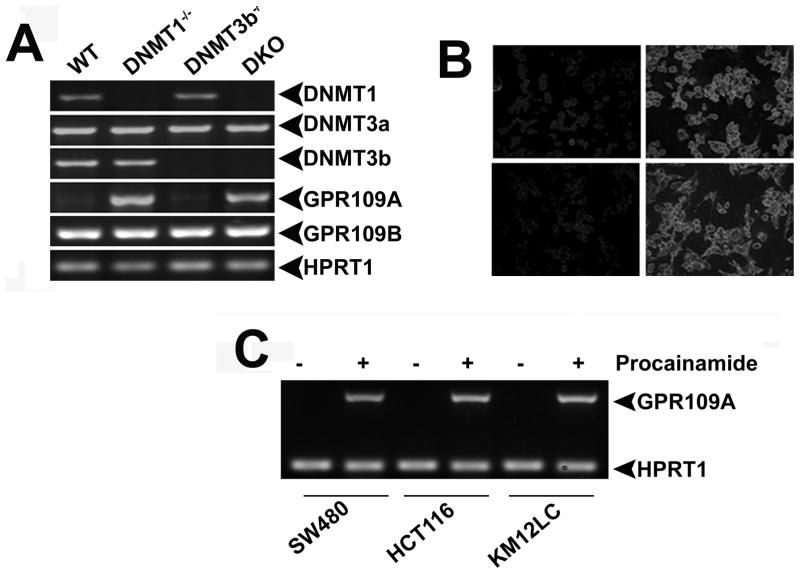
Role of DNA methylation in cancer-associated silencing of GPR109A in colon
To determine whether the decrease in the expression of GPR109A in colon cancer is due to DNA methylation, we treated normal and cancer colon cell lines with the DNA methylation inhibitor 5′-azacytidine and examined the expression of GPR109A. The treatment had no effect on GPR109A mRNA levels in normal cell lines. In contrast, the expression of the gene was induced in cancer cell lines in response to treatment (Supplementary Fig. S2A), indicating that DNA methylation is involved in the silencing of the gene in cancer cells. To determine which DNA methyltransferase (DNMT) is responsible for this process, we first evaluated the expression levels of different isoforms of DNMTs in normal and cancer cell lines and also in normal colon and in colon cancer (Supplementary Fig. 2B & C). We found the expression levels of DNMT1 and DNMT3b to be increased significantly in colon cancer cell lines and in primary colon cancer. DNMT1 mRNA levels increased 7.5 ± 0.6 fold (p < 0.001) in primary colon cancer compared to normal colon. The corresponding value for DNMT3b was 2.5 ± 0.3 (p < 0.01). There was no change in the levels of DNMT3a mRNA in primary colon cancer versus normal colon (p > 0.05). These data indicated that DNMT1, DNMT3b, or both might be involved in the silencing of GPR109A in colon cancer. We then examined the expression of GPR109A in HCT116 cells (a human colon cancer cell line positive for the expression of all three isoforms of DNMT) and in isogenic HCT116 cell lines with targeted deletion of DNMT1 (DNMT1−/−), DNMT3b (DNMT3b−/−), or both (DKO). We found very little expression of GPR109A in control HCT116 cells, but the expression was induced markedly in DNMT1−/− cells and in DKO cells but not in DNMT3b−/− cells. This was evident at the level of mRNA (Fig. 3A) and protein (Fig. 3B). This suggests that DNMT1 is most likely responsible for the silencing of GPR109A in cancer. In contrast to GPR109A, the levels of GPR109B mRNA remained the same in these cell lines, indicating that the expression of GPR109B is not regulated by DNMTs. To confirm the involvement of DNMT1 further in the cancer-associated silencing of GPR109A, we used procainamide, a specific inhibitor of DNMT1 (36). Treatment of colon cancer cell lines with this compound induced the expression of the receptor (Fig. 3C), supporting the conclusion that DNMT1 mediates the silencing of GPR109A in cancer cell lines.
Figure 3.
Involvement of DNMT1 in the silencing of GPR109A. A, Analysis of expression of GPR109A and GPR109B by RT-PCR in the human colon cancer cell line HCT116 which expresses all three isoforms of DNMT (WT), and in isogenic HCT116 cell lines with targeted deletion of DNMT1 (DNMT1−/−), DNMT3b (DNMT3b−/−) or both (DKO). B, Immunocytochemistry for GPR109A protein in WT, DNMT1−/−, DNMT3b−/−, and DKO cells. C, Effect of procainamide, a specific inhibitor of DNMT1, on GPR109A expression in colon cancer cell lines.
Role of GPR109A in tumor-suppressive effects of butyrate
To determine whether the butyrate receptor GPR109A has any role in the tumor-suppressive actions of butyrate, we selected CCD841 cells and KM12L4 cells as representatives of a normal colon cell line and a colon cancer cell line, respectively. CCD841 cells express the receptor constitutively. Exposure of these cells to GPR109A ligands butyrate or nicotinate did not have any effect on these cells (Fig. 4A). This was true even when the receptor was overexpressed by transfection with an expression vector. KM12L4 cells, being a cancer cell line, do not express the receptor. Accordingly, exposure of these cells to the receptor ligands butyrate or nicotinate did not have any effect (Fig. 4B). However, when the receptor was expressed ectopically, exposure of the cells to butyrate or nicotinate induced apoptosis (Fig. 4B). The GPR109A/nicotinate-induced apoptosis in KM12L4 cells was associated with activation of caspases (Fig. 4C). In addition, the expression of various anti-apoptotic genes (Bcl-2, Bcl-W, Bcl-xL, and Bfl-1) was decreased and that of various pro-apoptotic genes (FAS-L, FAS-R, FADD, and TNF-R1) was increased in association with GPR109A/nicotinate-induced apoptosis (Supplementary Fig. S3). Furthermore, the expression of cyclin D1 was decreased and the expression of PTEN, PPARγ, and Foxo3A was increased with GPR109A/nicotinate. Another interesting finding was the subunit switching for PI3-kinase in association with GPR109A/nicotinate-induced apoptosis. The expression of p55α was increased whereas the expression of p85α was decreased. Butyrate can diffuse into mammalian cells to some extent whereas nicotinate cannot. Therefore, to eliminate any potential confusion in the interpretation of the data, we used nicotinate rather than butyrate as the receptor ligand in these experiments.
Figure 4.

Induction of apoptosis in colon cancer cells by GPR109A ligands. A, The normal colon cell line CCD841 was transfected with vector or human GPR109A cDNA, and then treated with or without nicotinate (1 mM) or butyrate (1 mM) for 48h. Cells were then used for analysis of apoptosis by FACS. B, The colon cancer cell line KM12L4 was transfected with vector or human GPR109A cDNA, and then treated with or without nicotinate (1 mM) or butyrate (1 mM) for 48h. Cells were then used for analysis of apoptosis by FACS. C, The cell lysates from the experiments described in A and B were used to monitor caspase activation by Western blot using antibodies specific for cleaved fragments of caspases.
Non-involvement of histone deacetylase inhibition in cancer cell apoptosis induced by GPR109A activation
Butyrate is an inhibitor of histone deacetylases (HDACs). We have shown previously that butyrate induces apoptosis in colon cancer cell lines if SLC5A8, a butyrate transporter, is expressed in these cells and that the process is associated with inhibition of HDACs (20). In the present study, we showed that butyrate induces apoptosis in cancer cells by activation of GPR109A on the cell surface. To determine whether the apoptosis induced in colon cancer cells by GPR109A activation involved HDAC inhibition, we measured HDAC activity in CCD841 cells and KM12L4 cells under various experimental conditions (Supplementary Fig. S4). HDAC activity was significantly lower in CCD841 cells than in KM12L4 cells, showing that cancer cells have higher HDAC activity. The levels of HDAC activity did not change in CCD841 cells irrespective of whether or not GPR109A was expressed ectopically in these cells or whether or not these cells were exposed to nicotinate (Supplementary Fig. S4A). The same was true in KM12L4 cells. Importantly, there was no change in HDAC activity in these cells even after transfection with a GPR109A expression vector followed by treatment with nicotinate (Supplementary Fig. S4B). But, apoptosis was induced in these cells under these conditions. These HDAC activity data were confirmed by monitoring the acetylation status of histone H3, histone H4, histone H4-Lys12, and histone H4-Lys16 (Supplementary Fig. S4C).
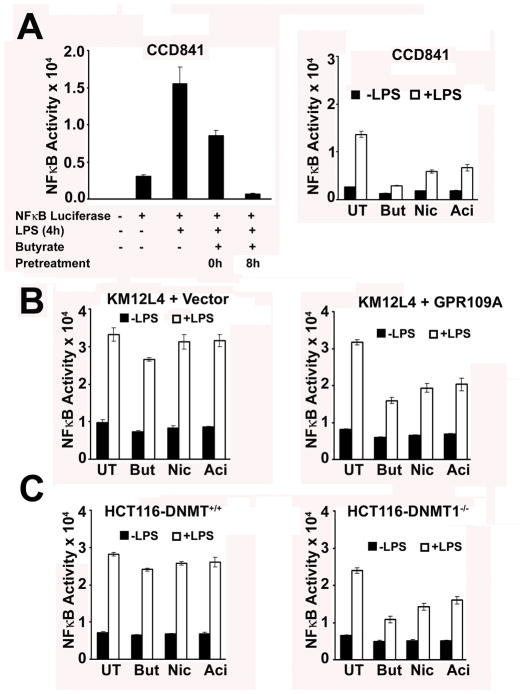
Blockade of NF-κB by GPR109A ligands in colon
Normal colonic epithelium expresses the toll-like receptor TLR4 which functions as a receptor for bacterial lipopolysaccharide (LPS) (37). Intriguingly, there is no undue inflammation of the colonic epithelium under normal conditions in the presence of bacteria in the colon. LPS is known to activate NF-κB signaling through TLR4. Since NF-κB is pro-inflammatory and pro-tumorigenic, we investigated the relevance of GPR109A and butyrate to LPS-induced NF-κB activation in colon cells. The normal colon cell line CCD841 cells expressed GPR109A and TLR4 constitutively (data not shown). When transfected with a NF-κB-luciferase reporter, the expression of luciferase in these cells was induced by LPS treatment; but pre-treatment with butyrate completely abolished this induction (Fig. 5A). This effect was reproduced with nicotinate and acifran, two other agonists of GPR109A. The colon cancer cell line KM12L4 expressed TLR4 but not GPR109A (data not shown). LPS induced luciferase expression in these cells after transfection with the reporter, but GPR109A ligands had no effect on this induction (Fig. 5B). This was expected because of the absence of GPR109A. However, with ectopic expression of GPR109A, the induction of luciferase by LPS in this cell line was significantly blocked by GPR109A ligands (p < 0.001). These results were corroborated by studies with HCT116 cells, which did not express GPR109A and the DNMT1−/− isogenic HCT116 cells, which expressed the receptor (Fig. 5C). To determine whether these findings are reproducible in normal colon, we used colon tissues from a transgenic mouse which carries NF-κB-luciferase reporter gene under the control of β-actin promoter. Since normal colon expresses GPR109A constitutively, we directly tested the effects of GPR109A ligands on LPS-induced activation of NF-κB reporter in these tissues. Butyrate and other GPR109A ligands were able to block LPS-induced activation of NF-κB in normal colon (Supplementary Fig. S5). Interestingly, activation of GPR109A in normal colon blocked not only LPS-induced activation of NF-κB but also the basal activity of NF-κB.
Figure 5.
Blockade of LPS-induced NF-κB activation by GPR109A in the normal colon cell line CCD841 and in the colon cancer cell lines KM12L4 and HCT116. A, CCD841 cells were first transfected with a NF-κB-luciferase reporter construct. 24h later, cells were treated with LPS (100 ng/mL) for 4h with or without pretreatment with butyrate (But, 1 mM), nicotinate (Nic, 1 mM), or acifran (Aci, 0.25 mM) for 4h. The ligands were present for an additional 4h during treatment with LPS. LPS-induced activation of NF-κB was monitored by measuring the activity of luciferase as a reporter. UT, no treatment with GPR109A ligands. B, KM12L4 cells were transfected with a NF-κB-luciferase reporter together with either vector or GPR109A cDNA. 24h later, cells were treated with LPS (100 ng/mL) for 4h with or without pretreatment with butyrate (But, mM), nicotinate (Nic, 1 mM), and acifran (Aci, 0.25 mM) for 4h. In addition to the pretreatment, the ligands were present also during LPS treatment. LPS-induced activation of NF-κB was monitored by measuring the activity of luciferase as a reporter. C, HCT116 cells (DNMT+/+ and DNMT1−/−) were transfected with a NF-κB-luciferase reporter construct. 24h later, cells were treated with LPS (100 ng/mL) for 4h with or without pretreatment with butyrate (1 mM), nicotinate (1 mM), or acifran (0.25 mM) for 4h. The ligands were present also during LPS treatment. LPS-induced activation of NF-κB was monitored by measuring the activity of luciferase. UT, no treatment with GPR109A ligands.
Discussion
Gut bacteria play a critical role in the prevention of colon cancer and inflammatory bowel disease, but the molecular mechanisms involved in the process are not well understood. The short-chain fatty acids generated by bacterial fermentation of dietary fiber and unabsorbed carbohydrates are believed to be responsible for these effects. Epidemiological studies indicate that increased intake of fiber in the diet is linked to decreased risk of colon cancer and inflammatory bowel disease (8). Among the short-chain fatty acids produced by the bacteria in colon, butyrate is unique in that it is an inhibitor of HDACs (10, 11). Butyrate induces differentiation in normal intestinal and colonic epithelial cells, but causes apoptosis in colon cancer cells (4–7). The ability of butyrate to inhibit HDACs inside the cells provides a molecular mechanism for these effects. This intracellular action of butyrate requires a mechanism for the entry of butyrate into cells. SLC5A8 was recently identified as a Na+-coupled high-affinity transporter for butyrate; the ability of the transporter to mediate concentrative entry of butyrate into colon cells offers a mechanism for the tumor-suppressive effect of this bacterial metabolite (21–23).
The present studies unravel a novel mode of action of butyrate in colon, involving the cell surface G-protein-coupled receptor GPR109A. This receptor is expressed in normal colon on the lumen-facing apical membrane of colonic epithelial cells where it has access to luminal contents. Butyrate serves as a ligand for the receptor. Our studies show that this receptor functions as a tumor suppressor in colon. GPR109A is expressed in normal colon, but silenced in colon cancer. This phenomenon is also seen in colon cell lines; normal cell lines express the receptor whereas cancer cell lines do not. Activation of the receptor in normal colon cells does not induce cell death. But, when the receptor is expressed ectopically in colon cancer cells, activation of the receptor with butyrate or other ligands leads to apoptosis. The cancer-associated silencing of GPR109A occurs via DNA methylation. DNMT1 is responsible for this process. It is not known at present whether GPR109A is the direct target for DNMT1 or whether the silencing of GPR109A occurs indirectly through some other intermediary gene products. The cell death in colon cancer cells induced by GPR109A activation does not involve inhibition of HDACs. Thus, the bacterial fermentation product butyrate causes cell death in colon cancer cells by two independent but complementary mechanisms, one through SLC5A8-mediated entry of butyrate into cells with subsequent inhibition of HDACs, and the second through GPR109A independent of HDACs. The signaling pathways responsible for GPR109A/butyrate-induced cell death in cancer cells remain to be identified. Inhibitors of DNA methylation are currently being evaluated for their utility in cancer chemotherapy (38); unfortunately, clinical trials have shown encouraging results against leukemia but not against solid tumors such as colon cancer. Since our studies show that inhibition of DNA methylation in colon cancer cells induces GPR109A expression and that activation of the receptor causes tumor cell-specific apoptosis, the efficacy of DNA methylation inhibitors in the treatment of colon cancer might be enhanced by co-treatment with GPR109A ligands such as nicotinate.
The present studies show that GPR109A functions not only as a tumor suppressor but also as a blocker of LPS-induced NF-κB activation. The NF-κB signaling pathway plays a critical role in colonic inflammation as well as in inflammation-induced cancer (39). Our present findings suggest that butyrate mediates the protective effects of gut bacteria against inflammatory bowel disease by serving as a ligand for GPR109A. This is supported by a recent study, which showed a significant decrease in the number of butyrate-producing bacteria in the colon of patients with ulcerative colitis compared to normal controls (40). Chronic inflammation of the colon as seen in ulcerative colitis is a risk factor for colon cancer; therefore, GPR109A ligands may have potential as therapeutic agents in the treatment of inflammatory bowel disease and colon cancer.
The expression of GPR109B is altered only slightly in colon cancer. Even though GPR109B has high homology to GPR109A in primary structure, the two isoforms have marked differences in ligand specificity. GPR109B exhibits drastically reduced affinity than GPR109A for nicotinate and butyrate (28). This suggests that, unlike GPR109A, GPR109B does not function as a butyrate receptor in colon. Since GPR109B is not likely to mediate the biologic effects of butyrate, this isoform is not targeted for silencing in colon cancer. Interestingly, medium-chain fatty acids such as heptanoate and octanoate activate GPR109B; however, these fatty acids are not generated at significant concentrations in colonic lumen by bacterial fermentation. As GPR109B is expressed almost at normal levels in colon cancer, it might be useful to evaluate in future studies the potential of this receptor as a drug target for treatment of colon cancer.
Supplementary Material
References
- 1.Hooper LV, Gordon JI. Commensal host-bacterial relationships in the gut. Science. 2001;292:1115–8. doi: 10.1126/science.1058709. [DOI] [PubMed] [Google Scholar]
- 2.Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005;307:1915–20. doi: 10.1126/science.1104816. [DOI] [PubMed] [Google Scholar]
- 3.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 4.Topping DL, Clifton PM. Short-chain fatty acids and human colonic function: Roles of resistant starch and nonstarch polysaccharides. Physiol Rev. 2001;81:1031–64. doi: 10.1152/physrev.2001.81.3.1031. [DOI] [PubMed] [Google Scholar]
- 5.Mortensen PB, Clausen MR. Short-chain fatty acids in the human colon: relation to gastrointestinal health and disease. Scand J Gastroenterol. 1996;216:132–48. doi: 10.3109/00365529609094568. [DOI] [PubMed] [Google Scholar]
- 6.Manning TS, Gibson GR. Microbial-gut interactions in health and disease. Prebiotics Best Pract Res Clin Gastroenterol. 2004;18:287–98. doi: 10.1016/j.bpg.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Wong JM, de Souza R, Kendall CW, Emam A, Jenkins DJ. Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol. 2006;40:235–43. doi: 10.1097/00004836-200603000-00015. [DOI] [PubMed] [Google Scholar]
- 8.World Cancer Research Fund and American Institute for Cancer Research. Patterns of diet and cancer. In: Potter JD, editor. Food, Nutrition and Prevention of Cancer: a Global Perspective. Washington, DC: American Institute for Cancer Research; 1997. pp. 20–52. [Google Scholar]
- 9.Scheppach W, Weiler F. The butyrate story: old wine in new bottles? Curr Opin Clin Nutr Metab Care. 2004;7:563–7. doi: 10.1097/00075197-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Marks P, Rifkind RA, Richon VM, et al. Histone deacetylases and cancer: causes and therapies. Nat Rev Cancer. 2001;1:194–202. doi: 10.1038/35106079. [DOI] [PubMed] [Google Scholar]
- 11.Drummond DC, Noble CO, Kirpotin DB, et al. Clinical development of histone deacetylase inhibitors as anticancer agents. Annu Rev Pharmacol Toxicol. 2005;45:495–528. doi: 10.1146/annurev.pharmtox.45.120403.095825. [DOI] [PubMed] [Google Scholar]
- 12.Miyauchi S, Gopal E, Fei YJ, Ganapathy V. Functional identification of SLC5A8, a tumor suppressor down-regulated in colon cancer, as a Na+-coupled transporter for short-chain fatty acids. J Biol Chem. 2004;279:13293–6. doi: 10.1074/jbc.C400059200. [DOI] [PubMed] [Google Scholar]
- 13.Coady MJ, Chang MH, Charron FM, et al. The tumor suppressor gene SLC5A8 expresses a Na+-monocarboxylate cotransporter. J Physiol (Lond) 2004;557:719–31. doi: 10.1113/jphysiol.2004.063859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gopal E, Fei YJ, Sugawara M, et al. Expression of slc5a8 in kidney and its role in Na+-coupled transport of lactate. J Biol Chem. 2004;279:44522–32. doi: 10.1074/jbc.M405365200. [DOI] [PubMed] [Google Scholar]
- 15.Gopal E, Fei YJ, Miyauchi S, et al. Sodium-coupled and electrogenic transport of B-complex vitamin nicotinic acid by slc5a8, a member of the Na/glucose co-transporter gene family. Biochem J. 2005;388:309–16. doi: 10.1042/BJ20041916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin PM, Gopal E, Ananth S, et al. Identity of SMCT1 (SLC5A8) as a neuron-specific Na+-coupled transporter for active uptake of L-lactate and ketone bodies in the brain. J Neurochem. 2006;98:279–88. doi: 10.1111/j.1471-4159.2006.03878.x. [DOI] [PubMed] [Google Scholar]
- 17.Gopal E, Miyauchi S, Martin PM, et al. Transport of nicotinate and structurally related compounds by human SMCT1 (SLC5A8) and its relevance to drug transport in the mammalian intestinal tract. Pharm Res. 2007;24:575–84. doi: 10.1007/s11095-006-9176-1. [DOI] [PubMed] [Google Scholar]
- 18.Li H, Myeroff L, Smiraglia D, et al. SLC5A8, a sodium transporter, is a tumor suppressor gene silenced by methylation in human colon aberrant crypt foci and cancers. Proc Natl Acad Sci USA. 2003;100:8412–7. doi: 10.1073/pnas.1430846100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paroder V, Spencer SR, Paroder M, et al. Na+/monocarboxylate transport (SMCT) protein expression correlates with survival in colon cancer: Molecular characterization of SMCT. Proc Natl Acad Sci USA. 2006;103:7270–5. doi: 10.1073/pnas.0602365103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thangaraju M, Cresci G, Itagaki S, et al. Sodium-coupled transport of the short-chain fatty acid butyrate by SLC5A8 and its relevance to colon cancer. J Gastrointest Surg. 2008;12:1773–82. doi: 10.1007/s11605-008-0573-0. [DOI] [PubMed] [Google Scholar]
- 21.Ganapathy V, Gopal E, Miyauchi S, Prasad PD. Biological functions of SLC5A8, a candidate tumour suppressor. Biochem Soc Trans. 2005;33:237–40. doi: 10.1042/BST0330237. [DOI] [PubMed] [Google Scholar]
- 22.Gupta N, Martin PM, Prasad PD, Ganapathy V. SLC5A8 (SMCT1)-mediated transport of butyrate forms the basis for the tumor suppressive function of the transporter. Life Sci. 2006;78:2419–25. doi: 10.1016/j.lfs.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 23.Ganapathy V, Thangaraju M, Gopal E, et al. Sodium-coupled monocarboxylate transporters in normal tissues and in cancer. AAPS J. 2008;10:193–9. doi: 10.1208/s12248-008-9022-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takebe K, Nio J, Morimatsu M, et al. Histochemical demonstration of a Na+-coupled transporter for short-chain fatty acids (slc5a8) in the intestine and kidney of the mouse. Biomed Res. 2005;26:213–21. doi: 10.2220/biomedres.26.213. [DOI] [PubMed] [Google Scholar]
- 25.Soga T, Kamohara M, Takasaki J, et al. Molecular identification of nicotinic acid receptor. Biochem Biophys Res Commun. 2003;303:364–9. doi: 10.1016/s0006-291x(03)00342-5. [DOI] [PubMed] [Google Scholar]
- 26.Wise A, Foord SM, Fraser NJ, et al. Molecular identification of high and low affinity receptors for nicotinic acid. J Biol Chem. 2003;278:9869–74. doi: 10.1074/jbc.M210695200. [DOI] [PubMed] [Google Scholar]
- 27.Tunaru S, Kero J, Schaub A, et al. PUMA-G and HM74 are receptors for nicotinic acid and mediate its anti-lipolytic effect. Nat Med. 2003;9:352–5. doi: 10.1038/nm824. [DOI] [PubMed] [Google Scholar]
- 28.Taggart AK, Kero J, Gan X, et al. (D)-beta-Hydroxybutyrate inhibits adipocyte lipolysis via the nicotinic acid receptor PUMA-G. J Biol Chem. 2005;280:26649–52. doi: 10.1074/jbc.C500213200. [DOI] [PubMed] [Google Scholar]
- 29.Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer RJ. Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther. 2008;27:104–19. doi: 10.1111/j.1365-2036.2007.03562.x. [DOI] [PubMed] [Google Scholar]
- 30.Gille A, Bodor ET, Ahmed K, Offermanns S. Nicotinic acid: pharmacological effects and mechanisms of action. Annu Rev Pharmacol Toxicol. 2008;48:79–106. doi: 10.1146/annurev.pharmtox.48.113006.094746. [DOI] [PubMed] [Google Scholar]
- 31.Ganapathy ME, Prasad PD, Huang W, Seth P, Leibach FH, Ganapathy V. Molecular and ligand-binding characterization of the sigma-receptor in the Jurkat human T lymphocyte cell line. J Pharmacol Exp Ther. 1999;289:251–60. [PubMed] [Google Scholar]
- 32.Digby GJ, Sethi PR, Lambert NA. Differential dissociation of G protein heterotrimers. J Physiol (Lond) 2008;586:3325–35. doi: 10.1113/jphysiol.2008.153965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta N, Miyauchi S, Martindale RG, et al. Upregulation of the amino acid transporter ATB0,+ (SLC6A14) in colorectal cancer and metastasis in humans. Biochim Biophys Acta. 2005;1741:215–23. doi: 10.1016/j.bbadis.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 34.Thangaraju M, Carswell KN, Prasad PD, Ganapathy V. Colon cancer cells maintain low levels of pyruvate to avoid cell death caused by inhibition of HDAC1/HDAC3. Biochem J. 2009;417:379–89. doi: 10.1042/BJ20081132. [DOI] [PubMed] [Google Scholar]
- 35.Logothetis DE, Kurachi Y, Galper J, Neer EJ, Clapham DE. The beta gamma subunits of GTP-binding proteins activate the muscarinic K+ channel in heart. Nature. 1987;325:321–6. doi: 10.1038/325321a0. [DOI] [PubMed] [Google Scholar]
- 36.Lee BH, Yegnasubramanian S, Lin X, Nelson WG. Procainamide is a specific inhibitor of DNA methyltransferase 1. J Biol Chem. 2005;280:40749–56. doi: 10.1074/jbc.M505593200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gay NJ, Gangloff M. Structure and function of Toll receptors and their ligands. Annu Rev Biochem. 2007;76:141–65. doi: 10.1146/annurev.biochem.76.060305.151318. [DOI] [PubMed] [Google Scholar]
- 38.Goffin J, Eisenhauer E. DNA methyltransferase inhibitors - state of the art. Ann Oncol. 2002;13:1699–716. doi: 10.1093/annonc/mdf314. [DOI] [PubMed] [Google Scholar]
- 39.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441:431–6. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 40.Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA. 2007;104:13780–5. doi: 10.1073/pnas.0706625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.