Patients with diabetes mellitus (DM) are at higher risk of tuberculosis (TB) (1), especially in China, where there is a high burden of both diseases (2). Comorbidity of DM and TB (DM + TB) results in higher probabilities of treatment failure, multidrug resistance, and death (3). In China, epidemiologic information for DM + TB is limited, and effective tools to identify cases of DM + TB are not available. Therefore, this cross-sectional, observational pilot study aimed to identify the prevalence, risk factors, and clinical symptoms of TB in patients with DM.
A stratified-cluster random sampling method was used to enroll patients with diagnosed type 2 DM who were ≥25 years of age in randomly selected villages in two sampling sites/counties (Ningyang and Yishui in the Shandong Province) from May to July 2012. Diagnostic criteria of DM followed the guidelines of World Health Organization (4). TB screening guidelines were recommended by a consensus of experts. Diagnostic criteria of active TB followed the International Standards for TB Care (5). The study was approved by the ethics committee of Shandong University. After providing written informed consent, each patient was interviewed about their demographics and medical history, and then chest radiography was performed. Patients with abnormal chest radiographs provided three sputum specimens for sputum smear and culture. Patients in our study were diagnosed as having active TB if they met one of three criteria: positive smear, positive culture, or positive chest radiograph, as determined by a clinical diagnosis team. A Poisson regression model was used to evaluate the associations between TB and risk factors in patients with DM.
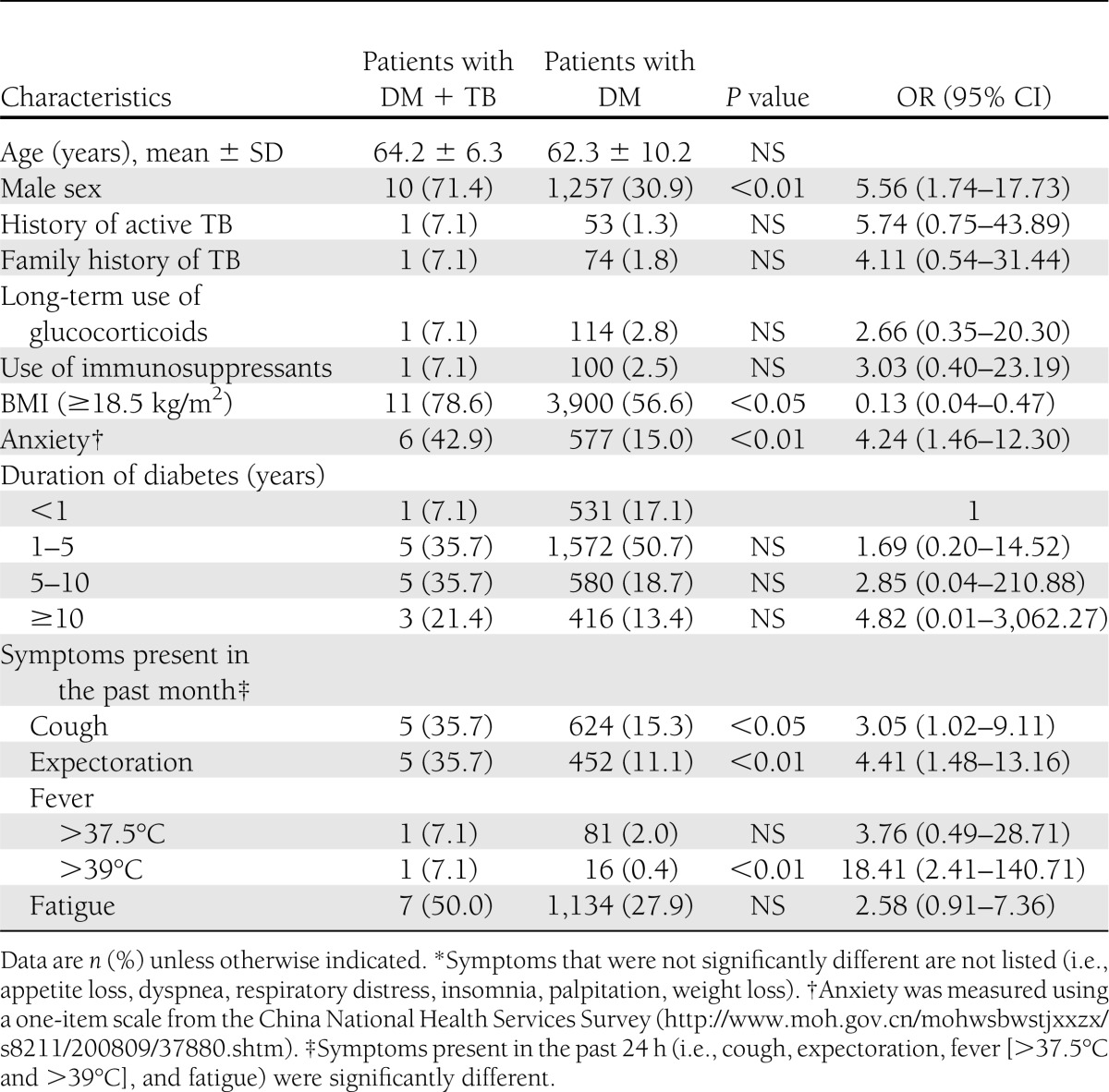
The overall enrollment rate of patients with DM was 68.7% at both sites. TB was diagnosed in 14 of 4,085 patients with DM. Thirteen new TB cases (8 in Ningyang, 5 in Yishui) included one with a positive culture, and 12 with a positive radiograph (none of the new cases had a positive smear). One case in Yishui was re-treated and had a positive smear. The prevalence of TB in patients with DM at the two sampling sites was 342.7 per 100,000 persons, compared with 42.8 per 100,000 persons in the local general population (i.e., approximately 8 times in relative risk). Table 1 presents the demographics and symptoms of the groups with DM + TB and DM only. The Poisson regression further identified the risk factors in adjusted odds ratio (OR) and 95% CI. Male patients (adjusted OR 5.50 [95% CI 1.70–17.85]) were more likely to have TB. Normal and overweight patients (adjusted OR 0.15 [95% CI 0.04–0.56]) were less likely to have TB than those who were underweight. Patients with DM + TB were more likely to have symptoms of cough, expectoration, fever, and fatigue. Compared with patients with only DM, patients with DM + TB were more like to report anxiety symptoms such as feeling nervous and worrisome (adjusted OR 4.92 [95% CI 1.66–14.60]) on an one-item scale.
Table 1.
Demographic characteristics and reported symptoms of patients with diabetes*
This pilot DM + TB screening study in China’s community sample of patients with DM found a high relative risk, suggesting that patients with type 2 DM are a population at high risk for TB. More efforts need to be made to coordinate screening, prevention, and treatment for patients with DM + TB in the context of cross-cutting health systems of TB and chronic diseases in China.
Acknowledgments
The study was supported by a World Health Organization Western Pacific Regional Office (WHO WPRO) TB Operational Research Grant (WPPDCC1002661).
No potential conflicts of interest relevant to this article were reported.
W.Z., Q.C., and A.Y. collected, analyzed, and interpreted the data. L.S., V.A.F., J.H., and A.Y. designed the study. J.H. provided epidemiological consultation. D.S. and J.Z. monitored, trained, and coordinated the participants. All authors coordinated the study and critically revised the article. A.Y. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Nobuyuki Nishikiori, WHO WPRO; Shiwen Jiang, Dongmei Hu, and Jun Li, China National TB Control Program; Fang Li, Shandong Provincial TB Control Program; Junyan Ning, Ningyang TB Control Center; and Min Zhao and Tong Liu, Yishui TB Control Center, for their support and contributions.
References
- 1.Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med 2008;5:e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. New Engl J Med 2010;362:1090–1101 [DOI] [PubMed] [Google Scholar]
- 3.Dooley KE, Tang T, Golub JE, Dorman SE, Cronin W. Impact of diabetes mellitus on treatment outcomes of patients with active tuberculosis. Am J Trop Med Hyg 2009;80:634–639 [PMC free article] [PubMed] [Google Scholar]
- 4.Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia [report online], c2006Geneva: World Health Organization; Available from http://whqlibdoc.who.int/publications/2006/9241594934_eng.pdf Accessed 10 June 2013 [Google Scholar]
- 5.International standards for tuberculosis care [report online], 2006Geneva: World Health Organization; Available from http://www.who.int/tb/publications/2006/istc_report_shortversion.pdf Accessed 10 June 2013 [Google Scholar]


