Abstract
OBJECTIVE
It is unknown whether any association between neighborhood food environment and obesity varies according to individual income and/or race/ethnicity. The objectives of this study were to test whether there was an association between food environments and obesity among adults with diabetes and whether this relationship differed according to individual income or race/ethnicity.
RESEARCH DESIGN AND METHODS
Subjects (n = 16,057) were participants in the Diabetes Study of Northern California survey. Kernel density estimation was used to create a food environment score for each individual’s residence address that reflected the mix of healthful and unhealthful food vendors nearby. Logistic regression models estimated the association between the modeled food environment and obesity, controlling for confounders, and testing for interactions between food environment and race/ethnicity and income.
RESULTS
The authors found that more healthful food environments were associated with lower obesity in the highest income groups (incomes 301–600% and >600% of U.S. poverty line) among whites, Latinos, and Asians. The association was negative, but smaller and not statistically significant, among high-income blacks. On the contrary, a more healthful food environment was associated with higher obesity among participants in the lowest-income group (<100% poverty threshold), which was statistically significant for black participants in this income category.
CONCLUSIONS
These findings suggest that the availability of healthful food environments may have different health implications when financial resources are severely constrained.
Access to healthful food is distributed inequitably by area-level socioeconomic status (SES) and racial/ethnic composition (1). Improving access to healthful food environments can improve the disparity in access to healthful foods, but less is known about whether better access to healthful foods will influence obesity risk. Specifically, studies of the associations between healthful and unhealthful food vendors and obesity prevalence show mixed results (2,3). A recent review (2) suggested that the most consistent association has been between supermarkets and weight status. However, supermarkets have been associated with both lower (4–7) and higher (8) BMI or prevalence of obesity, in addition to null findings (9,10). Similarly, the relationships between obesity and fast food and convenience stores have also had inconsistent results across studies (3,6,11). These inconsistencies might be explained by heterogeneity in operationalization of food environments, in contexts studied, or in population composition.
Specifically, few studies have investigated whether any association between food environments and obesity among adults varies across demographic characteristics, such as income or race/ethnicity. This is relevant not only as a possible explanation for inconsistent associations, but also because obesity-related policies regarding the food environment are often targeted at populations with low income and/or racial/ethnic minority populations. The association between food environments and obesity might be different for populations with high income compared with low because having a low income may render healthful foods unaffordable, even when they are available in one’s neighborhood. In a similar line of reasoning, it has been previously shown that black American populations do not experience the same level of health benefits from increasing socioeconomic resources as compared with white Americans (12,13). In the realm of environmental resources, walkable neighborhoods have been associated with lower BMI for white Americans, but not for black Americans or Latinos (14). The mechanisms for these observed relations are not completely elucidated, but it has been hypothesized that the multiple additional barriers to health faced by racial/ethnic minorities in the U.S., including discrimination, may make potential health assets less effective for promoting health (12). In contrast, among adolescents, it has been reported that supermarkets have a greater protective association for black American adolescents compared with whites or Latinos (7). For these reasons, we hypothesized that the association among adults between food environments and obesity might vary by race, but we did not have a strong hypothesis about the direction of this variation.
The objectives of this study were to test the association between food environments and obesity among adults with diabetes and determine whether any association differed by income or race/ethnicity. Few studies of neighborhood food environments have specifically investigated associations among adults living with chronic diseases (for exception, see Ref. 15). Yet, neighborhood food environments may be quite important facilitators or barriers to healthful weight status for populations living with a chronic disease, such as diabetes, which requires lifestyle modification for optimal management.
RESEARCH DESIGN AND METHODS
Study population
Participants were selected from the 20,188 members of Kaiser Permanente Northern California, an integrated health care delivery system, who responded to a survey conducted by the Diabetes Study of Northern California (DISTANCE) during 2005–2006 (16). The survey was administered to a race/ethnicity–stratified random sample of adults with diabetes from the Kaiser Permanente Diabetes Registry, had a 62% response rate, and queried demographic, health, and behavioral information. Participants’ clinical measures were gathered from Kaiser Permanente Northern California electronic medical records. Exclusion criteria for the current analyses were type 1 diabetes (n = 962), pregnancy within 9 months before the survey (n = 25), cancer within 1 year prior to the survey (n = 189), and history of lower extremity amputation (n = 210). Participants with missing data were also excluded from the analytic sample (BMI [n = 478], residential location [n = 1,115], education [n = 338], neighborhood deprivation [n = 151], comorbidity index [n = 47], marital status [n = 602], and nativity [n = 14]), leaving 16,057 subjects for our analysis.
Dependent variable
Our outcome of interest was obesity, defined according to World Health Organization classifications as BMI ≥30 (17). Height and weight measured at the last clinic visit prior to the survey completion date were used to calculate BMI (weight [kg]/height [m2]). If measured BMI was unavailable, self-reported values were used (n = 704). Self-reported and measured BMI were highly correlated (r = 0.89) with an average difference of 0.59 BMI units.
Independent variable
Food environment score: net difference in the kernel density of healthful and unhealthful food vendors.
Our main independent variable was a composite measure of the food environment calculated as the difference between the kernel densities of healthful and unhealthful retail food vendors at the census block centroid of each individual’s residence. This measure aimed to quantify the mix of healthful and unhealthful food vendors nearby an individual’s residence. The multistep process to create this measure is described in detail below. To briefly summarize, we identified supermarkets, produce markets, convenience stores, and fast-food restaurants in the 19 counties in which study participants lived. We classified supermarkets and produce markets as healthful food vendors and convenience stores and fast-food vendors as unhealthful. We used a 1-mile radius buffer around each store to transform the geocoded point locations into a smooth kernel density surface. Finally, we subtracted the density surface of the unhealthful food surface from the density surface of the healthful food surface to create a composite food environment score measure for each participant.
Identification and classification of food vendors.
We used 2006 commercial food store data from the National Establishment Time Series to geocode vendor addresses and to identify four categories of food vendors in our measure of the food environment: supermarkets, produce vendors, convenience stores, and fast-food restaurants, based on Standardized Industrial Codes. A total of 9,623 vendors was identified; however, many were classified as “grocery stores” or “eating places” instead of supermarket, produce vendor, convenience store, or fast-food restaurant. Consequently, we used keyword searches and chain-name identification to reclassify vendors labeled as “grocery stores” or “eating places” into the four categories above. Vendors labeled as “grocery stores” but with ≥$1 million in sales and >30 employees were reclassified as supermarkets (18). In preliminary work, we found that grocery stores with a sales volume <$1 million tended to carry fewer nutritious food items (19) and were a heterogeneous mix of healthful and unhealthful food vendors; we therefore excluded these grocery stores from our measure (n = 1,698; 17%). We also excluded vendors classified still as “eating places” after the reclassifying procedure (n = 2,295; 23%). Certified farmers’ markets were classified as produce vendors.
A total of 5,630 stores within 19 counties in northern California were used for the kernel density measure. Following previous work (20,21), we classified supermarkets and produce vendors as healthful food vendors and convenience stores and fast-food restaurants as unhealthful food vendors.
Creating the kernel density surface.
Next, we transformed the discrete point locations for each food vendor type into continuous kernel density surfaces using a 1-mile radius and a quadratic function for inverse distance weighting so that the density was greatest at the geocoded point for each vendor and decreased to zero at the edge of the radius. Overlapping density values were summed in the kernel density surface. Because supermarkets are physically larger, have a larger service area, and tend to have longer hours (22,23), we double weighted the supermarket density surface.
Composite measure of healthful and unhealthful kernel density surfaces.
Finally, we subtracted the kernel density surface of the unhealthful food vendors from the kernel density surface of the healthful food vendors to create a composite kernel density surface. A positive net kernel density score indicates the presence of more healthful than unhealthful food vendors.
We used the net score for the kernel density of each participant’s census block centroid as a measure of the participant’s food environment (hereafter “net kernel density food environment score” or “food environment score”). Individuals who had neither a healthful nor an unhealthful food vendor within a one-mile radius of their block centroid had a food environment value of zero (n = 1,224). All spatial analyses used the spatial analyst extension of ArcGIS v.10.0 (ESRI, Inc., Redlands, CA).
Advantages of kernel density method.
The kernel density method has previously been used in neighborhood-health literature (24) and is advantageous because it can account for distance, density, and diversity. For example, stores that are closer to a residential location are weighted greater than those further away. Density values for stores of the same type that exist within 1 mile of each other are added together to capture the presence of food retail clusters. Lastly, kernel density surfaces can be easily combined to represent composite measures of the food environment. Previous composite measures have relied on ratios of unhealthful to healthful food stores (25), but doing so creates a problem when there are zero food stores in the denominator. We avoided this by subtracting rather than dividing.
Covariates and effect measure modifiers
Confounders were factors hypothesized to affect selection into neighborhoods and obesity status (26) and chosen based on prior knowledge that informed a directed acyclic graph for the relation between food environment and obesity. Confounders included race/ethnicity (self-reported: white, black, Latino, or Asian), family income as a percent of federal poverty line according to family size (≤100, 101–300, 301–600, and >600%), neighborhood deprivation [a principal components index based on eight census tract variables (27), by quartiles], nativity (born in U.S. or elsewhere), age (continuous and quadratic terms), sex, education (did not graduate high school, graduated high school but not college, or graduated college), marital status (married, cohabitating, divorced/separated, widowed, or never married), and baseline comorbidity score [based on DxCG (Verisk Health), a validated comorbidity index that predicts future health care costs based on a patient’s current health conditions; modeled as a continuous score (28)]. Although neighborhood walkability and/or physical activity may be correlated with neighborhood food environment through a common cause, such as neighborhood deprivation, we did not find a compelling reason to think that walkability or physical activity caused the neighborhood food environment, so these were not included as confounders. All categorical variables entered the models as indicator variables. A substantial number of participants did not report income and were not in the four largest race/ethnicity categories, so we included indicator variables for missing groups in these categories to avoid excluding observations.
We hypothesized that the association between the food environment and obesity would vary by income and race/ethnicity, so we tested interactions between these variables and food environment (i.e., income × food environment; race/ethnicity × food environment) as well as a quadratic term for food environment (i.e., income × food environment2; race/ethnicity × food environment2). We also tested a number of interactions as part of our model-building and assumption-checking process: whether the association between obesity and the food environment varied by sex; whether the association between obesity and education, income, neighborhood deprivation, or race/ethnicity varied by sex; and whether the association between obesity and neighborhood deprivation varied by race/ethnicity.
Statistical analyses
Means or frequency distributions of key variables for the total sample and within each food environment quartile were calculated. We performed several analyses to briefly assess the reliability and validity of our food environment score. First, we found the Pearson correlation between the food environment score from 2 different years to assess test-retest reliability. Next, to assess construct validity [whether the score is correlated with factors known or suspected to reflect the construct it seeks to measure (29)], we found the correlation between neighborhood deprivation and the food environment score, and we assessed the counts of each food vendor category according to quartile of our food environment score. To assess possible structural confounding (i.e., systematically missing observations for certain combinations of exposures and covariates), we examined the distribution of family incomes within food environment quartiles for the total sample and within race/ethnic group (30).
Statistical model building
We used logistic regression with Huber-White SEs to model the relationship between the net kernel density food environment score and prevalence of obesity. We built our model according to the following steps. First, we first established the fullest model with all hypothesized interactions and confounders included; this model included quadratic terms for food environment score and age to allow for curvilinearity. We then tested the significance of each interaction in the full model using a Wald test of joint significance. We deleted the interaction terms that were not statistically significant in the fullest model [all at once, as opposed to backward selection (31)]. In this reduced model, we retested the previously significant interactions and the interactions of substantive interest (race/ethnicity × food environment and income × food environment). We deleted any nonsignificant interactions from this model, and the resulting model was our final model.
Based on this process, the final model included independent variables and confounders (food environment score, food environment score squared, income, race/ethnicity, sex, age, age squared, comorbidity index, marital status, attained education, neighborhood deprivation) plus the statistically significant interaction terms: income × food environment (P = 0.046), income squared × food environment (P = 0.027), race × food environment (P = 0.037), and sex × race (P = 0.0006). Our tests of interactions indicated that the association between obesity and the food environment score did not vary by sex, nor did the association between obesity and sex vary by education, income, or neighborhood deprivation. These interactions were therefore not included in the final model. We predicted the probability of obesity using the coefficient estimates from the final reduced model (Supplementary Table 2), converted from odds to probabilities, across the observed range of food environment scores and graphed the results.
Sensitivity analyses
In sensitivity analyses, we assessed whether results would change had we: 1) used a complete case analysis (i.e., excluding participants missing race/ethnicity and income information); 2) included an indicator for self-reported BMI; 3) modeled BMI as a continuous rather than a dichotomous outcome; and 4) not double weighted the supermarkets in our kernel density measure.
We performed three sensitivity tests related to the modeling of the difference in unhealthful and healthful food densities as a curvilinear relation. First, having zero healthful food vendors and zero unhealthful food options may not be equivalent to having an equal number of each. To test this, we excluded all observations with zero healthful and unhealthful vendors and reran the final model. Second, to test if the curvilinear specification was accurately capturing the slope directions from negative to zero and zero to positive, we replaced the continuous and quadratic food environment terms with a piecewise linear spline with a knot at the kernel density value of zero. Third, we probed whether having any healthful food options was associated with lower obesity compared with having no healthful food options. For this test, instead of net kernel density food environment score, we modeled an indicator variable for no healthful food (kernel density of healthful food: 0–0.5 (inclusive) versus some healthful food (kernel density of healthful food >0.5–10), while controlling for the kernel density of unhealthful food.
Statistical analyses were conducted in Stata version 10.1. The α value was set at 0.05 for main effects and 0.10 for interactions. Sampling weights for race/ethnicity were used in the descriptive analyses presented in Tables 1 and 2 to represent the full DISTANCE sampling frame. We did not use sampling weights in tabular examinations of individual SES distribution across neighborhood quartiles or in regression analyses as all analyses include race/ethnicity interactions (32).
Table 1.
Selected health and sociodemographic characteristics† according to quartiles of food environment score,‡ DISTANCE, 2005–2006
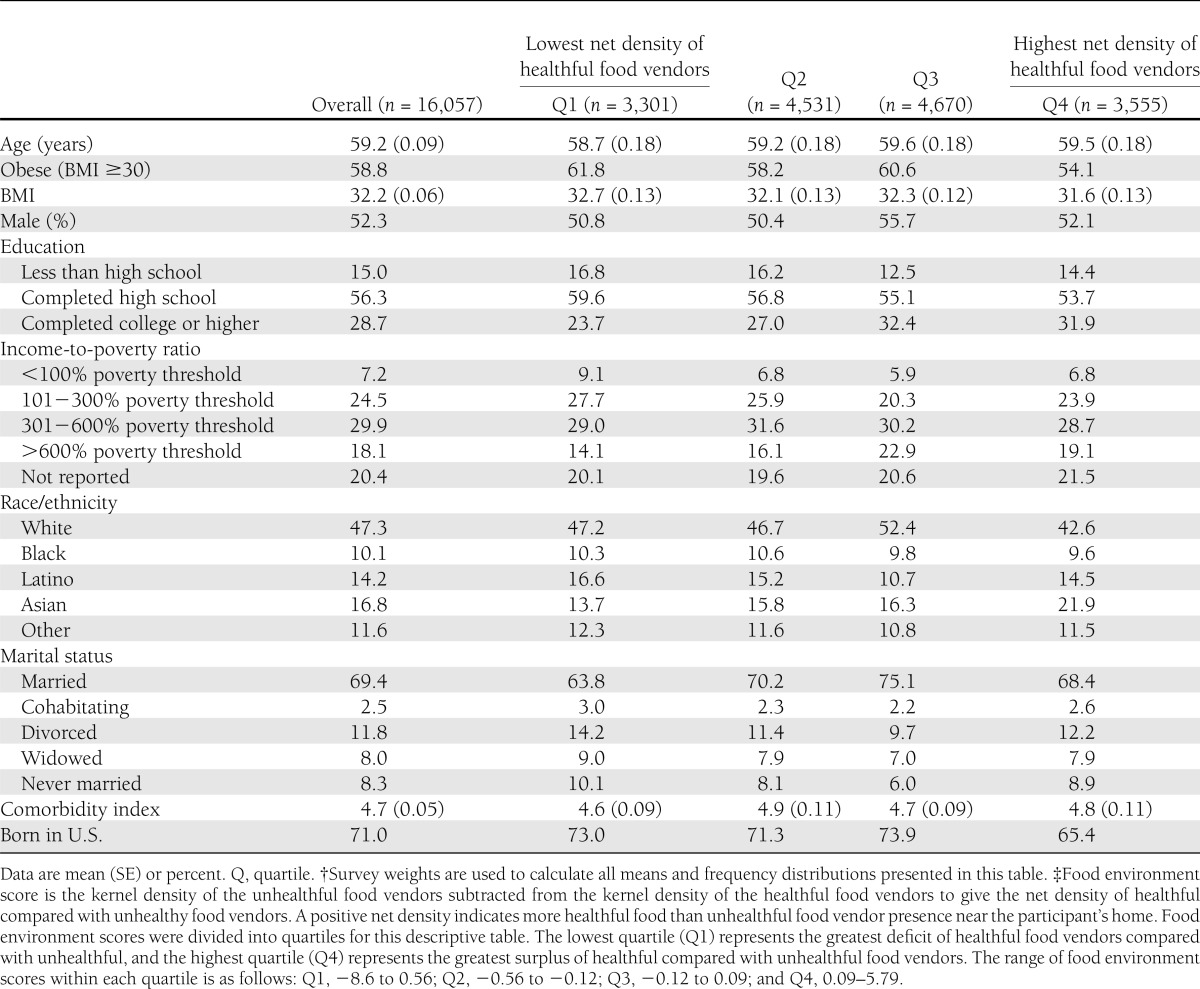
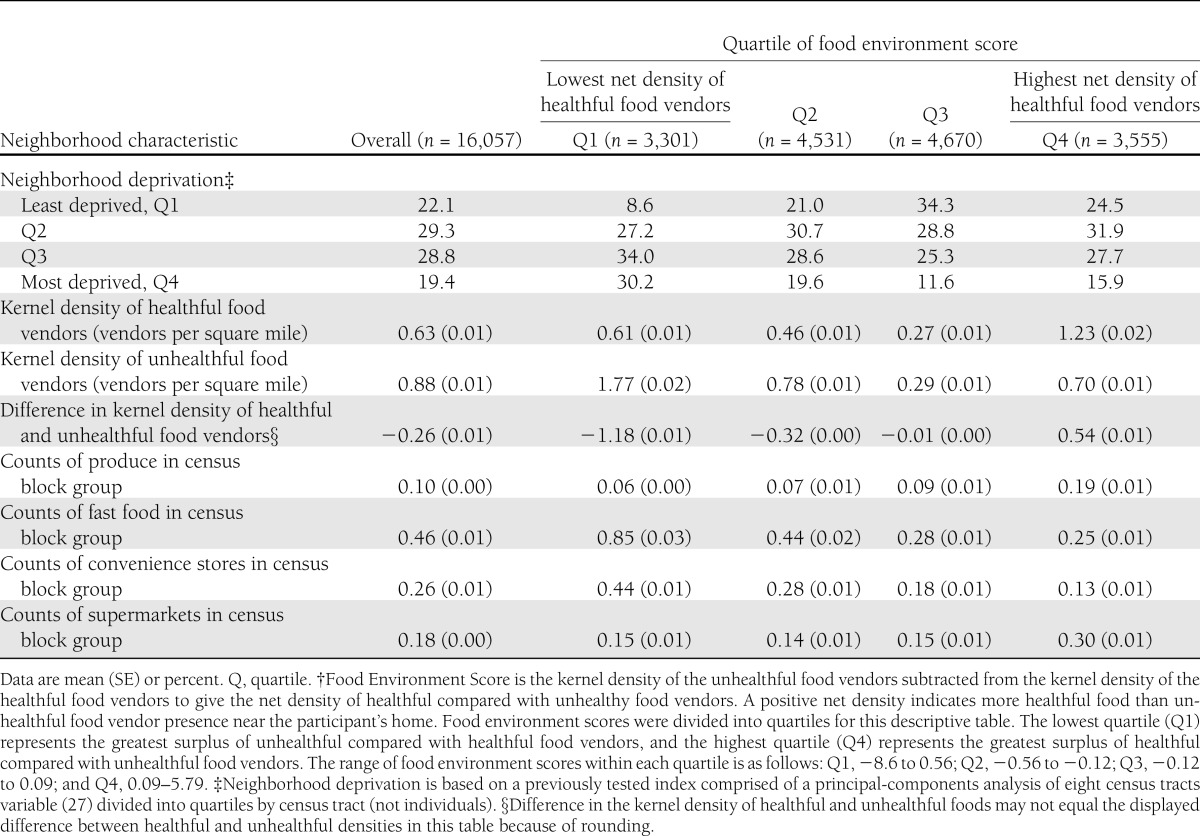
Table 2.
Neighborhood characteristics according to quartile of food environment score,† DISTANCE, 2005–2006
This study was approved by the Institutional Review Boards of the University of California, Berkeley, and the Kaiser Permanente Division of Research.
RESULTS
Fifty-nine percent of the subjects in our sample were obese. Higher obesity prevalence was observed among participants in the least healthful food environments (quartile 1) compared with the most healthful (quartile 4) (61.8 vs. 54.1%) before adjustment (Table 1). People in the most healthful food environments (compared with least healthful) were more likely to be college graduates, Asian, married, and in the highest income category.
The mean net kernel density food environment score was negative (−0.26; range: −8.7 to 5.8; interquartile range: −0.5 to 0.10; see Supplementary Fig. 1 for distribution), meaning that, on average, the kernel density of unhealthful stores exceeded that of healthful stores (Table 2). The correlation of the food environment score in years 2006 and 2007 (test-retest reliability) was 0.87. Our tests of construct validity revealed that our food environment score was significantly negatively correlated with neighborhood deprivation (r = −0.18; P < 0.001); the counts of food vendors across quartiles of the food environment score suggested that our net kernel density measure was appropriately reflecting the food vendor mix. We found no evidence of structural confounding by individual income and neighborhood food environment in the data (Supplementary Table 1).
Unadjusted results were similar in direction but generally further away from the null relative to adjusted results. The adjusted association between the net kernel density food environment score and odds of obesity varied significantly by income and race/ethnicity. Due to the complexity introduced by these interactions, the main results are presented graphically (Fig. 1; model coefficients used to produce this figure can be found in Supplementary Table 2).
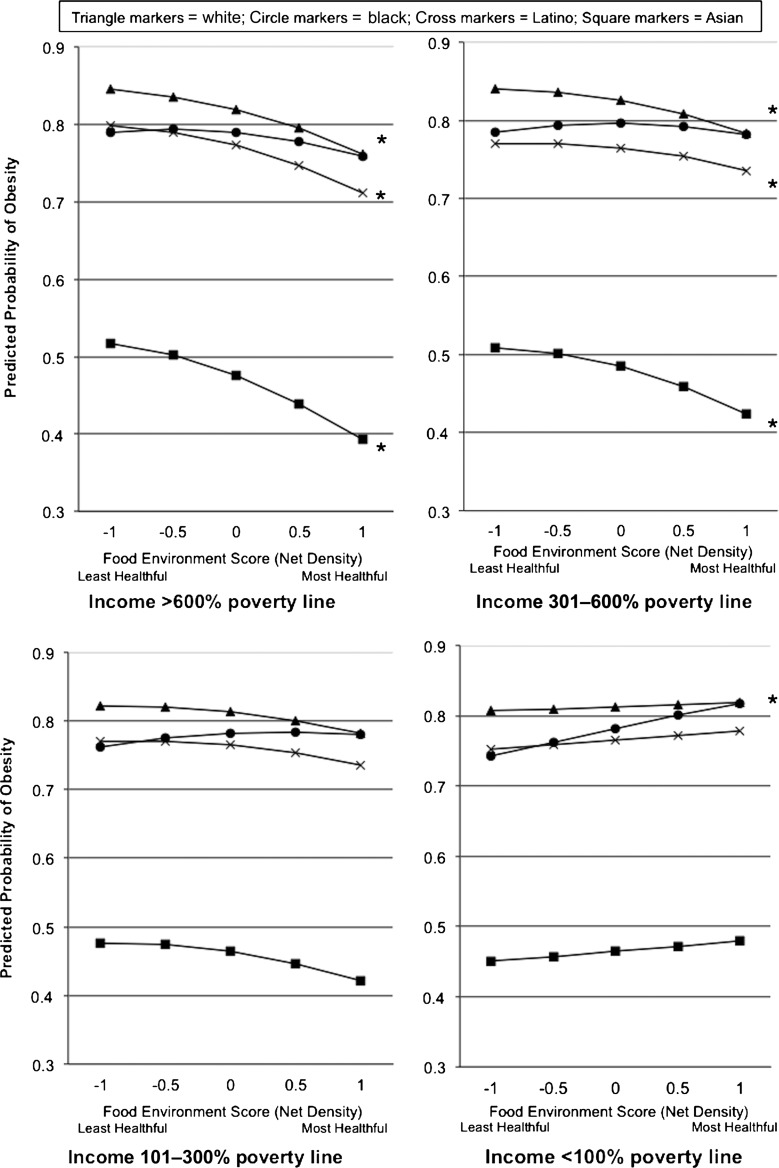
Figure 1.
Associations between food environment score and obesity according to income level and race/ethnicity, DISTANCE. *P < 0.05 within each demographic subgroup for the difference in predicted probability when comparing a net kernel density food environment score difference of −1 to +1 (significant differences are seen among whites, Latinos, and Asians with incomes >600% poverty line and incomes 301–600% poverty line and among blacks with incomes <100% poverty line). Food environment score is the kernel density of the unhealthful food vendors subtracted from the kernel density of the healthful food vendors to give the net density of healthful compared with unhealthy food vendors. A positive net density indicates more healthful food than unhealthful food vendor presence near the participant’s home. Predicted probabilities of obesity are calculated from converted coefficients (from odds to probabilities) from the logistic regression of obesity prevalence and food environment score. Models are adjusted for neighborhood deprivation, age, sex, comorbidities, nativity, marital status, and education and include a squared term for age and the food environment variable, main effects and interaction terms between food environment and income, main effects and interaction terms between food environment squared term and income, main effects and interaction terms between food environment and race/ethnicity, and main effects and interaction terms between race/ethnicity and sex. Predicted probabilities display the shape of the relationship between food environments and obesity according to income and race/ethnicity for the entire sample. However, the intercepts will differ based on other variables in the model. The intercepts shown reflect the following characteristics: women with the sample average age and comorbidity levels, with a high school or some college education level, living in the second least-deprived quartile of neighborhood, born in the U.S., and married. Slopes are the same for men, but intercepts are different.
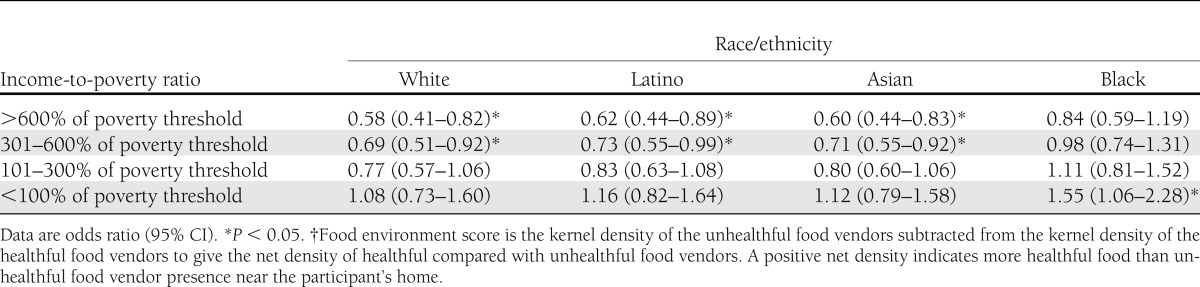
For each subgroup, we also assessed odds of obesity when comparing a net kernel density food environment score difference of −1 (predominately unhealthful food vendors) to +1 (predominately healthful food vendors). Odd ratios and 95% CIs are shown in Table 3. In the highest two income categories (income >600% of the poverty threshold and 301–600% of the poverty threshold), more healthful food environments were associated with lower odds of obesity. Inverse associations were significant for whites, Latinos, and Asians, but smaller and not statistically significant for blacks. Fig. 1 shows flatter slopes between −1 and 0 compared with 0 and +1, indicating that most of the difference occurred when comparing predominately healthful environments to either predominantly unhealthful or equal levels of healthful and unhealthful. For whites, Latinos, and Asians in the second lowest income group (101–300% of the poverty threshold), the relationship was still negative, but slopes were flatter and nonsignificant, while for blacks, the relationship was positive. For all race/ethnic groups in the lowest income category (<100% of the poverty threshold), the lines were flat to positively sloped, revealing a tendency for higher obesity in the more healthful food environments. The greater odds of obesity reached statistical significance for blacks.
Table 3.
Odds ratio and 95% CIs for obesity for participants with food environment score† of +1 (predominantly healthful food vendors) compared with food environment score of −1 (predominantly unhealthful food vendors; referent group), according to income-to-poverty ratio and race/ethnicity
Sensitivity analyses
Results were substantively unchanged for the complete case analysis, using an indicator for self-reported BMI, and when not doubly weighting the supermarkets. The model specifying continuous BMI as the outcome generated results similar in direction to our main findings for obesity with the exception that, among whites in the lowest income group, the association between relatively more healthful compared with unhealthful food environment was negative instead of positive. Results were virtually unchanged when we excluded people from the analysis with zero unhealthful and zero healthful food vendors as were results from the model with a piecewise linear spline with a knot at the value zero. We tested whether having any healthful food compared with having no healthful foods, while controlling for the level of unhealthful food, was associated with lower prevalence of obesity. In all of the subgroup comparisons, having no healthful food compared with having some healthful food was not significantly associated with obesity prevalence (all P > 0.20).
CONCLUSIONS
This is one of the first studies in the U.S. to examine how the food environment is associated with obesity in a large sample of adults with diabetes, an increasingly prevalent chronic condition. It is also the first study to our knowledge to investigate whether associations between food environments and obesity vary by individual income or race/ethnicity among adults. Among all race/ethnic groups in the highest income category, having a greater net density of healthful food vendors compared with unhealthful food vendors was associated with lower odds of obesity. On the contrary, among low-income participants of all racial/ethnic groups, having a higher density of healthful compared with unhealthful food vendors was associated with higher odds of obesity, although only statistically significantly so for black participants.
These findings build on recent work that specifically investigates whether sociodemographic characteristics are modifiers of neighborhood-health associations. Similar to our findings, Lovasi et al. (14) found inverse associations between neighborhood walkability and obesity were strongest and most consistent for higher income, higher education groups, and among non-Hispanic whites. It has been hypothesized that such findings could be due to the multiple barriers faced by disadvantaged populations. A positive neighborhood environment may not adequately compensate for multiple other disadvantages (14). However, our results are less consistent with this hypothesis. Even if multiple barriers reduced the effect of a more healthful food environment to promote improved weight status, having an additional barrier of a predominantly unhealthful food environment should be expected to be associated with even higher risk for obesity. Conversely, we found that among participants with lower incomes, those living in more unhealthful food environments actually had lower odds of obesity compared with those with higher net density of healthful food. This was strongest for black participants.
Assuming these associations are not due to chance, reverse causation, or unmeasured confounding, one explanation for these counterintuitive findings among low-income groups may be that supermarkets and produce vendors have different meanings and implications for populations with very constrained resources. While supermarkets provide a wide variety of lower-priced fresh foods, they also have lower prices on a wide range of less healthful foods (33). Furthermore, healthful foods in supermarkets may be less affordable than the unhealthful foods, particularly on a per-calorie basis (34). Thus, residents with access to a supermarket may not be able to afford healthy foods, but may be able to buy unhealthful foods more cheaply than those living in neighborhoods where convenience stores and fast-food establishments predominate. This is consistent with the notion that supermarkets alone may not be adequate to affect obesity in the most resource-constrained populations (35). This also underscores the potential for ecological fallacy (36) if we assume that populations with a more healthful food environment choose predominately healthful food options inside those environments.
Our findings among black participants at all income levels also deserve further discussion. Among high-income participants, for whom more healthful food environments were associated with lower odds of obesity, this relationship was weakest among black participants. Among low-income participants, for whom more healthful food environments were associated with higher odds of obesity, this association was strongest among black participants. Previous literature has suggested that the health returns for higher levels of SES are lower for blacks compared with whites (12,13). Whether this finding is specific to our study population should be further explored in other geographic areas and in adults without diabetes.
We cannot rule out the possibility that the observed relationship between neighborhood food environment and obesity is noncausal. Unmeasured personal preferences might dominate both the selection into neighborhoods with a certain type of food environment and the food choices within that environment (37). This might account for the expected relationship between healthful food environments and lower odds of obesity among populations with high income and non-black populations. Having a higher income and facing less racial residential discrimination likely increases the probability that one can choose a neighborhood that reflects personal preferences. In contrast, having a lower income or being a person of color may decrease the likelihood that one can live in a neighborhood that matches personal preferences due to financial limitations or discrimination. Recent work using fixed effects regression to control for unobserved time-invariant preferences found that supermarket availability was not associated with improved fruit and vegetable intake (35), as did a quasi-experimental study (38). Conversely, in the experimental Moving to Opportunity demonstration program (39), moving to a less deprived neighborhood resulted in lower risk of obesity among healthy mothers, lending evidence toward causality, but in this case focused on neighborhood deprivation rather than food environments specifically. Future work using longitudinal data or quasi-experimental designs can address these limitations and will be particularly informative.
In addition to the limitations inherent in our cross-sectional design described above, other limitations should be noted. We were limited in our ability to classify all food vendors as either healthful or unhealthful. Many establishments that sell food, such as non–fast-food restaurants, specialty food stores, mobile vendors, and small grocery stores were not included in our kernel density food environment scores. Also, this measure is not immediately translatable into a policy recommendation, such as banning fast food or promoting supermarkets. Although these are limitations, we felt that our composite measure, using four types of food vendors that have been previously studied, reflects the mix of food vendors around an individual’s home and offers perspective that cannot be gained from examining each individual type of food vendor type separately. Additionally, our sensitivity testing indicated that our findings were not primarily driven by the existence of any healthful food (compared with no healthful food). This is consistent with the notion that our composite measure of the food environment “mix” is getting a different construct than simply the availability of any healthful food. Next, we relied on the National Establishment Time Series business data; however, this limitation is common to most studies of a sizeable area. Our survey had a response rate of 62%; we previously reported that participation was somewhat lower among race/ethnic minorities and those with less education; however, the respondents and nonrespondents were otherwise similar (16). Due to missing data on covariates, our analytic sample included 80% of the total survey participants. No significant differences were seen in obesity prevalence or net difference in kernel density between the survey sample and the analytic sample among those that had information on both. Finally, we studied odds of obesity among a sample of adults with diabetes who have a very high prevalence of obesity; our findings are likely not generalizable to nondiabetic populations.
Our findings indicate that in these adults with diabetes, the association between the food environment and obesity differed across income and race/ethnicity and suggest that availability of healthful food vendors may have different implications when financial resources are severely constrained. Future studies should not assume that the association between food environments and obesity is the same for all demographic groups. Whether these same findings persist in future studies with experimental or longitudinal designs and among different populations will be informative.
Acknowledgments
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (grants DK-080744, DK-065664, and HD-46113) to the Kaiser Permanente Division of Research, University of California, San Francisco, and the University of California, Berkeley, to conduct this research, which was ancillary to DISTANCE. Kaiser Permanente and the University of California, San Francisco, were also supported by the Center for Diabetes Translation Research (Grant P30-DK-092924).
No potential conflicts of interest relevant to this article were reported.
J.C.J.-S. conceptualized the research question, conducted the analyses, and led the drafting and revising of the manuscript. A.J.K. was the principal investigator for the DISTANCE study, oversaw the survey data collection and compilation, and provided critical feedback on study design, analysis, and manuscript revisions. E.M.W. contributed to the analyses and interpretation, provided critical feedback on the manuscript, and contributed in the drafting and revising of the manuscript. M.K. supervised the collection of neighborhood food environment data and creation of neighborhood contextual variables, assisted in the interpretation of results, and provided critical feedback on the manuscript. E.K. designed the neighborhood food environment score and contributed to the analyses and the drafting and revising of the manuscript. H.H.M. managed the DISTANCE survey design and data collection, provided critical feedback on study design, analyses, and data interpretation, and contributed to manuscript revisions. N.A. was co-principal investigator for the DISTANCE study and provided critical feedback on study design, analysis, and manuscript revisions. D.S. was co-principal investigator for the DISTANCE study and provided critical feedback on study design and manuscript revisions. B.A.L. supervised the collection of food environment measures and creation of the neighborhood contextual variables, supervised the study design and analyses, and provided critical feedback on analyses, interpretation, and manuscript. J.C.J.-S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Preliminary findings from this study were previously presented in abstract form at the 3rd North American Congress of Epidemiology, Montreal, Canada, 21–24 June 2011.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-2190/-/DC1.
The sponsors played no role in the design or interpretation of the study, and none of the funders had input into the content of this article.
References
- 1.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7–20 [DOI] [PubMed] [Google Scholar]
- 2.Giskes K, van Lenthe F, Avendano-Pabon M, Brug J. A systematic review of environmental factors and obesogenic dietary intakes among adults: are we getting closer to understanding obesogenic environments? Obes Rev 2011;12:e95–e106 [DOI] [PubMed] [Google Scholar]
- 3.Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place 2010;16:175–190 [DOI] [PubMed] [Google Scholar]
- 4.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place 2009;15:491–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med 2006;30:333–339 [DOI] [PubMed] [Google Scholar]
- 6.Black JL, Macinko J, Dixon LB, Fryer GE., Jr Neighborhoods and obesity in New York City. Health Place 2010;16:489–499 [DOI] [PubMed] [Google Scholar]
- 7.Powell LM, Auld MC, Chaloupka FJ, O’Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. Am J Prev Med 2007;33(Suppl.):S301–S307 [DOI] [PubMed] [Google Scholar]
- 8.Wang MC, Kim S, Gonzalez AA, MacLeod KE, Winkleby MA. Socioeconomic and food-related physical characteristics of the neighbourhood environment are associated with body mass index. J Epidemiol Community Health 2007;61:491–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mobley LR, Root ED, Finkelstein EA, Khavjou O, Farris RP, Will JC. Environment, obesity, and cardiovascular disease risk in low-income women. Am J Prev Med 2006;30:327–332 [DOI] [PubMed] [Google Scholar]
- 10.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health 2005;119:1059–1068 [DOI] [PubMed] [Google Scholar]
- 11.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Philadelphia, PA, Lippincott, Williams & Wilkins, 2008 [Google Scholar]
- 12.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci 1999;896:173–188 [DOI] [PubMed] [Google Scholar]
- 13.Hajat A, Kaufman JS, Rose KM, Siddiqi A, Thomas JC. Long-term effects of wealth on mortality and self-rated health status. Am J Epidemiol 2011;173:192–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lovasi GS, Neckerman KM, Quinn JW, Weiss CC, Rundle A. Effect of individual or neighborhood disadvantage on the association between neighborhood walkability and body mass index. Am J Public Health 2009;99:279–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gary-Webb TL, Baptiste-Roberts K, Pham L, et al. Look AHEAD Research Group Neighborhood and weight-related health behaviors in the Look AHEAD (Action for Health in Diabetes) study. BMC Public Health 2010;10:312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moffet HH, Adler N, Schillinger D, et al. Cohort Profile: The Diabetes Study of Northern California (DISTANCE)—objectives and design of a survey follow-up study of social health disparities in a managed care population. Int J Epidemiol 2009;38:38–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization/Food and Agriculture Organization Expert Consultation on Diet, Nutrition and the Prevention of Chronic Diseases: Report of the Joint WHO/FAO Expert Consultation. Geneva, World Health Organization, 2003 [Google Scholar]
- 18.Truong K, Fernandes M, An R, Shier V, Sturm R. Measuring the physical food environment and its relationship with obesity: evidence from California. Public Health 2010;124:115–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kersten E, Laraia B, Kelly M, Adler N, Yen IH. Small food stores and availability of nutritious foods: a comparison of database and in-store measures, Northern California, 2009. Prev Chronic Dis 2012;9:E127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rundle A, Neckerman KM, Freeman L, et al. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect 2009;117:442–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spence JC, Cutumisu N, Edwards J, Raine KD, Smoyer-Tomic K. Relation between local food environments and obesity among adults. BMC Public Health 2009;9:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McClelland WG. Economics of the supermarket. Econ J 1962;72:154–170 [Google Scholar]
- 23.Bonanno A, Lopez RA. Competition effects of supermarket services. Am J Agr Econ 2009;91:555–568 [Google Scholar]
- 24.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med 2008;34:16–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Babey SH, Diamant AL, Hastert TA, Harvey S. Designed for disease: the link between local food environments and obesity and diabetes [article online], 2008. Available at http://www.policylink.org/atf/cf/%7B97c6d565-bb43-406d-a6d5-eca3bbf35af0%7D/designedfordisease_final.pdf Accessed 26 March 2013
- 26.Fleischer NL, Diez Roux AV. Using directed acyclic graphs to guide analyses of neighbourhood health effects: an introduction. J Epidemiol Community Health 2008;62:842–846 [DOI] [PubMed] [Google Scholar]
- 27.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health 2006;83:1041–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao Y, Ellis RP, Ash AS, et al. Measuring population health risks using inpatient diagnoses and outpatient pharmacy data. Health Serv Res 2001;36:180–193 [PMC free article] [PubMed] [Google Scholar]
- 29.DeVellis RF. Scale Development: Theory and Applications. Los Angeles, CA, Sage Publications, Inc; 2011 [Google Scholar]
- 30.Oakes JM. Commentary: advancing neighbourhood-effects research—selection, inferential support, and structural confounding. Int J Epidemiol 2006;35:643–647 [DOI] [PubMed] [Google Scholar]
- 31.Jewell NP. Statistics for Epidemiology. Boca Raton, Chapman & Hall/CRC, 2004 [Google Scholar]
- 32.Winship C, Radbill L. Sampling weights and regression analysis. Sociol Methods Res 1994;23:230–257 [Google Scholar]
- 33.Ford PB, Dzewaltowski DA. Disparities in obesity prevalence due to variation in the retail food environment: three testable hypotheses. Nutr Rev 2008;66:216–228 [DOI] [PubMed] [Google Scholar]
- 34.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6–16 [DOI] [PubMed] [Google Scholar]
- 35.Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, Shikany JM, Lewis CE, Popkin BM. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med 2011;171:1162–1170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robinson WS. Ecological correlations and the behavior of individuals. Int J Epidemiol 2009;38:337–341 [DOI] [PubMed] [Google Scholar]
- 37.Chaix B, Leal C, Evans D. Neighborhood-level confounding in epidemiologic studies: unavoidable challenges, uncertain solutions. Epidemiology 2010;21:124–127 [DOI] [PubMed] [Google Scholar]
- 38.Cummins S, Petticrew M, Higgins C, Findlay A, Sparks L. Large scale food retailing as an intervention for diet and health: quasi-experimental evaluation of a natural experiment. J Epidemiol Community Health 2005;59:1035–1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes—a randomized social experiment. N Engl J Med 2011;365:1509–1519 [DOI] [PMC free article] [PubMed] [Google Scholar]