Abstract
OBJECTIVE
To study differences in glycemic control and HbA1c testing associated with use of secure electronic patient-provider messaging. We hypothesized that messaging use would be associated with better glycemic control and a higher rate of adherence to HbA1c testing recommendations.
RESEARCH DESIGN AND METHODS
Retrospective observational study of secure messaging at Group Health, a large nonprofit health care system. Our analysis included adults with diabetes who had registered for access to a shared electronic medical record (SMR) between 2003 and 2006. We fit log-linear regression models, using generalized estimating equations, to estimate the adjusted rate ratio of meeting three indicators of glycemic control (HbA1c <7%, HbA1c <8%, and HbA1c >9%) and HbA1c testing adherence by level of previous messaging use. Multiple imputation and inverse probability weights were used to account for missing data.
RESULTS
During the study period, 6,301 adults with diabetes registered for access to the SMR. Of these individuals, 74% used messaging at least once during that time. Frequent use of messaging during the previous calendar quarter was associated with a higher rate of good glycemic control (HbA1c <7%: rate ratio, 1.26 [95% CI, 1.15–1.37]) and a higher rate testing adherence (1.20 [1.15–1.25]).
CONCLUSIONS
Among SMR users, recent and frequent messaging use was associated with better glycemic control and a higher rate of HbA1c testing adherence. These results suggest that secure messaging may facilitate important processes of care and help some patients to achieve or maintain adequate glycemic control.
An increasing number of health care organizations are providing patients with access to their personal health data and care providers through the Internet. These sites, often termed “patient portals,” sometimes allow patients and providers to exchange secure electronic messages between office visits. Although most patients still do not have the option to communicate with their care providers electronically (1,2), more practices are transitioning to comprehensive clinical information systems with built-in messaging capabilities. The diffusion of new management paradigms such as the Chronic Care Model (3,4) and the Patient-Centered Medical Home (5) have also driven interest in electronic patient-provider messaging. Electronic messaging has potential to bridge the communication gap between home and clinic, to help patients to articulate their goals, to assist with team-based care, and to improve the timeliness and efficiency of care. How online care interacts with “traditional” outpatient care is still largely unknown. Several studies have found cross-sectional associations between secure messaging and higher diabetes care quality (6–9). A cross-sectional study at a large integrated delivery system found that patients who used the most messaging had higher levels of comorbidity and outpatient utilization (6), but there is also evidence from a longitudinal study that clinic visits decrease over time with increased participation in secure messaging (10). Given that secure messaging is a new care modality, most previous studies have been time-limited in scope.
The primary objective of this analysis was to determine the extent to which participation in secure messaging would be associated with subsequent changes in process and outcome measures related to diabetes care during a 3-year period after implementation. By using longitudinal as opposed to cross-sectional data, we were able to separate exposure from time and provide some evidence for a causal inference between secure messaging and our outcomes of interest. Specifically, we tested the hypothesis that secure messaging is associated with better glycemic control and a higher rate of adherence to HbA1c testing recommendations after exposure to secure messaging.
RESEARCH DESIGN AND METHODS
Setting
The study was conducted at Group Health, a mixed-model health care financing and delivery organization in Washington and North Idaho. Approximately 460,000 members receive care through Group Health’s Integrated Delivery System, which includes 25 Group Health–owned facilities and >550 Group Health physicians (11). Beginning in August 2003, all patients in the Integrated Delivery System were able to access patient Web services through the MyGroupHealth website. These services include prescription refills, appointment scheduling, medical record access, and secure messaging to contact primary care providers or specialists as previously described (12). The MyGroupHealth patient website has two levels of security. At the initial level, a patient creates a password-protected account that can be used to access health-related discussion groups. A second, higher level of security provides access to the medical record, secure messaging, and other advanced Web services. Access to this security level requires each patient to complete an additional step verifying their identity (ID verification). Initially, this entailed presenting a legal form of identification in person or by mail. Currently, new users are required to visit a website to obtain an ID verification code that is mailed to their home addresses.
Inclusion criteria
We included patients at least 18 years of age with a diagnosis of diabetes. For each study year, data were included from patients who had a primary care provider in Group Health’s Integrated Group Practice for 2 out of 3 months of each quarter, and for three out of four quarters. Because patients without a registered primary care provider do not have access to secure messaging, this requirement ensured that patients had access to secure messaging for a majority of each year. Short discontinuities in enrollment were allowed because they could reflect changes in employment or plan type rather than an actual lapse in coverage. Diabetes diagnoses were determined by enrollment in the Group Health diabetes registry. Prescription, diagnostic, and laboratory data were used to determine registry eligibility. Analyses were restricted to patients who obtained ID verification to use the shared medical record, all of whom had access to secure messaging and some of whom elected to use it. Once patients obtained access to the shared medical record, there was no additional sign-up process or log-in required to access secure messaging. We excluded HbA1c measurements taken within 6 months of a new diabetes diagnosis, during which time rapid changes in glycemic control would likely reflect the initiation of a treatment plan. Although secure messaging may have a role in the optimization of initial treatment plans, our primary aim was to look at the role of secure messaging in the long-term maintenance of glycemic control rather than its role at the time of diagnosis. Measurements were censored if end-stage renal disease developed.
Data source
All data were abstracted from clinical and administrative data warehouses maintained by Group Health Research Institute (Seattle, WA). Pharmacy data were used to identify enrollees using oral diabetes medications or insulin. To protect patient confidentiality, identifiers were excluded from the study dataset. Data were identified by a study-specific, person-level identifier. All study protocols were approved by Group Health’s Human Subjects Review Board.
Primary outcomes
We estimated the association between secure messaging use and three (binary) indicators of glycemic control as follows: HbA1c <7%; HbA1c <8%; and HbA1c >9%. These three indicators were analyzed as separate outcomes. To increase comparability to quality evaluations in other practice settings, we chose these HbA1c ranges based on American Diabetes Association and Healthcare Effectiveness Data and Information Set quality indicators (13,14). Because HbA1c reflects the average blood glucose over the previous 2 to 3 months, outcomes were assessed quarterly. The person-quarter was the primary unit of analysis for all models. In quarters in which a patient underwent multiple tests, the latest measurement was used. We also estimated the association between secure messaging use and adherence to HbA1c testing recommendations. Clinical practice recommendations from the American Diabetes Association were used to define testing adherence (14). A patient was classified as either adherent or nonadherent in every quarter depending on whether at least two HbA1c tests were recorded during the previous year as recommended under clinical guidelines (14).
Primary independent variable
Secure messaging was included in the models as a four-level, ordered, categorical variable based on the total number of threads in an exposure period. We categorized secure messaging to allow for nonlinearities and to increase the interpretability of our results. The placement of exposure cut-points was driven by conceptual considerations. Specifically, we felt that a single exposure represented a unique category. The exposure group of two or three threads per quarter was chosen to represent low-frequency use (i.e., one thread or less per month). Participation in four to seven threads was chosen to model high-frequency use (i.e., between one and two threads per month), and participation in at least 8 threads per quarter was chosen to model very high-frequency use (i.e., two or more threads per month). In our operationalization of long-term exposure, cut-points were chosen based on similar considerations.
A thread was defined as the set of messages related to an original message by successive replies. Previous analysis at Group Health has suggested that a message thread is most conceptually similar to a single episode of clinical care (15). Although primary and specialty care providers can initiate secure messaging threads, >90% of secure messaging threads at Group Health are initiated by patients and directed to their designated primary care providers (15).
Control variables
Models were adjusted for age, sex, plan type, overall medical comorbidity, baseline HbA1c, diabetes severity, diabetes treatment type, diabetes duration, history of treated depression, and calendar time. Twelve aggregated diagnostic groups were selected a priori to control for medical comorbidity (16,17). The Diabetes Complication Severity Index, a 13-point scale, was used to measure diabetes severity (18). Depression was included because it has been associated with poor glycemic control (19,20). A history of depression was defined by an antidepressant prescription associated with a visit diagnosis of a depressive disorder. To ensure a flexible specification and to minimize residual confounding, age, diabetes severity, and diabetes duration were modeled as continuous variables using linear splines. For each spline, the function being smoothed was visually assessed and knots were placed in regions of rapid variation.
Adherence models were adjusted for the same set of variables as the models for glycemic control with the addition of a categorical variable modeling the HbA1c testing frequency of the patient’s primary care provider. This variable was intended to control for provider-level variation in HbA1c testing frequency, as well as to minimize confounding from higher-level factors such as the clinical practice environment. To operationalize this construct, providers were divided into quartiles of testing frequency based on the mean HbA1c testing interval across their panel of patients with diabetes. Preliminary models for all outcome measures permitted effect modification by previous level of glycemic control.
Statistical analysis
The person-quarter was the unit of analysis for all models. Exposure periods were defined by secure messaging activity during the quarter (i.e., short-term exposure) or year (i.e., long-term exposure) before the time period in which the outcome was assessed. The reference group consisted of patients with no secure messaging in the given exposure period, irrespective of their use during other time periods. Given that it was impossible to predict when a patient might begin to use secure messaging, we chose not to divide this reference group into additional categories based on secure messaging use during quarters outside of the given exposure period.
Log-linear regression models were fit to estimate adjusted rate ratios for each binary outcome measure in each quarter over a 3-year period from the time of secure messaging implementation (2004–2006) (21–24). Generalized estimating equations (GEEs) were used to estimate population-averaged effects while accounting for correlation between multiple observations on the same individual over time (25). A log link was used instead of the usual logit link for logistic regression models to permit direct estimation of rate ratios; when the outcome is common, as was the case for our analyses, odds ratios do not approximate rate ratios well and the results from logistic regression models tend to be less interpretable. Throughout, a working exchangeable correlation structure was specified for the GEE, the robust Huber-White sandwich estimator used for SEs to account for potential overdispersion as well as correlation between multiple observations over time in the same individual (26). Trend tests were used to assess the statistical significance of secure messaging in each model. Stata version 11.1 and R version 2.14.0 were used for statistical analyses (27,28).
Although we chose a GEE framework for these analyses, the use of mixed models also was considered. Whereas mixed models produce conditional (i.e., subject-specific) estimates, GEEs result in marginal (i.e., population-averaged) estimates. We chose a GEE framework with Huber-White SE estimate because it would be robust to misspecification of the variance structure of the outcome. This includes misspecification of the mean–variance relationship (i.e., which may result in overdispersion) as well as misspecification of the correlation structure for repeated measures analyses. In contrast, mixed effects models require specification of a specific distribution for the random effects and are less robust to misspecification.
Missing data methods
For analyses of glycemic control, the outcome was considered to be missing in quarters in which no HbA1c measurement was recorded. Based on this definition, the proportion of missing outcome data was 54%. This reflects an average HbA1c testing frequency of approximately twice per year. All other model covariates were complete or had little missing data. Given the high amount of missing outcome data and the high likelihood that these data were not missing completely at random, we felt that a complete case analysis likely would have yielded biased results. We therefore used two approaches to address missing data: inverse probability weights (29) and multiple imputation (30). Two approaches were chosen because similar results from both methods would support the validity of our inferences.
Inverse probability weights were calculated from a logistic regression model that predicted HbA1c testing in a particular 3-month period for a particular person (a “person-quarter”) as a function of age, time since the last HbA1c test, the value of the last HbA1c test, diabetes treatment type, diabetes severity, diabetes duration, comorbidity, previous outpatient utilization rate, intensity of previous shared electronic medical record use, and the primary care provider’s HbA1c testing frequency. Comorbidity was modeled using three indicator variables: a history of cardiovascular complications and assignment to aggregated diagnostic group 11 or group 18 (chronic unstable medical or specialty/eye). Analyses using inverse probability weights were performed in R using the geeglm function from the geepack package.
Three variables contained the following missing values: hemoglobin HbA1c (54% missing); treatment type (2.1% missing); and plan type (<0.01% missing). Missing values were multiply-imputed using the “chained equations” method. Each variable was imputed with a prediction model containing the following variables (excluding the variable being predicted): HbA1c (values of previous, current, and future tests); diabetes treatment type (previous and current); diabetes duration; intensity of previous shared electronic medical record use; age; plan type; and inclusion in aggregated diagnostic group 11 (chronic unstable medical). Five imputations were performed. Imputations and analyses of imputed datasets were performed in Stata using user-written program ice for imputations and Stata mi and xtgee commands for primary analysis models.
RESULTS
Population characteristics
Fifteen-thousand four-hundred thirty-eight adults with diabetes were enrolled in the Integrated Group Practice during the study period. Of these, 6,638 (43%) were ID-verified; 296 (4%) of ID-verified patients were excluded because of a recent diabetes diagnosis. Forty-one patients (<1%) had observations that were censored because of end-stage renal disease; 6,301 patients met all eligibility criteria for inclusion. There was an average of eight quarterly observations per individual (range, 1–12).
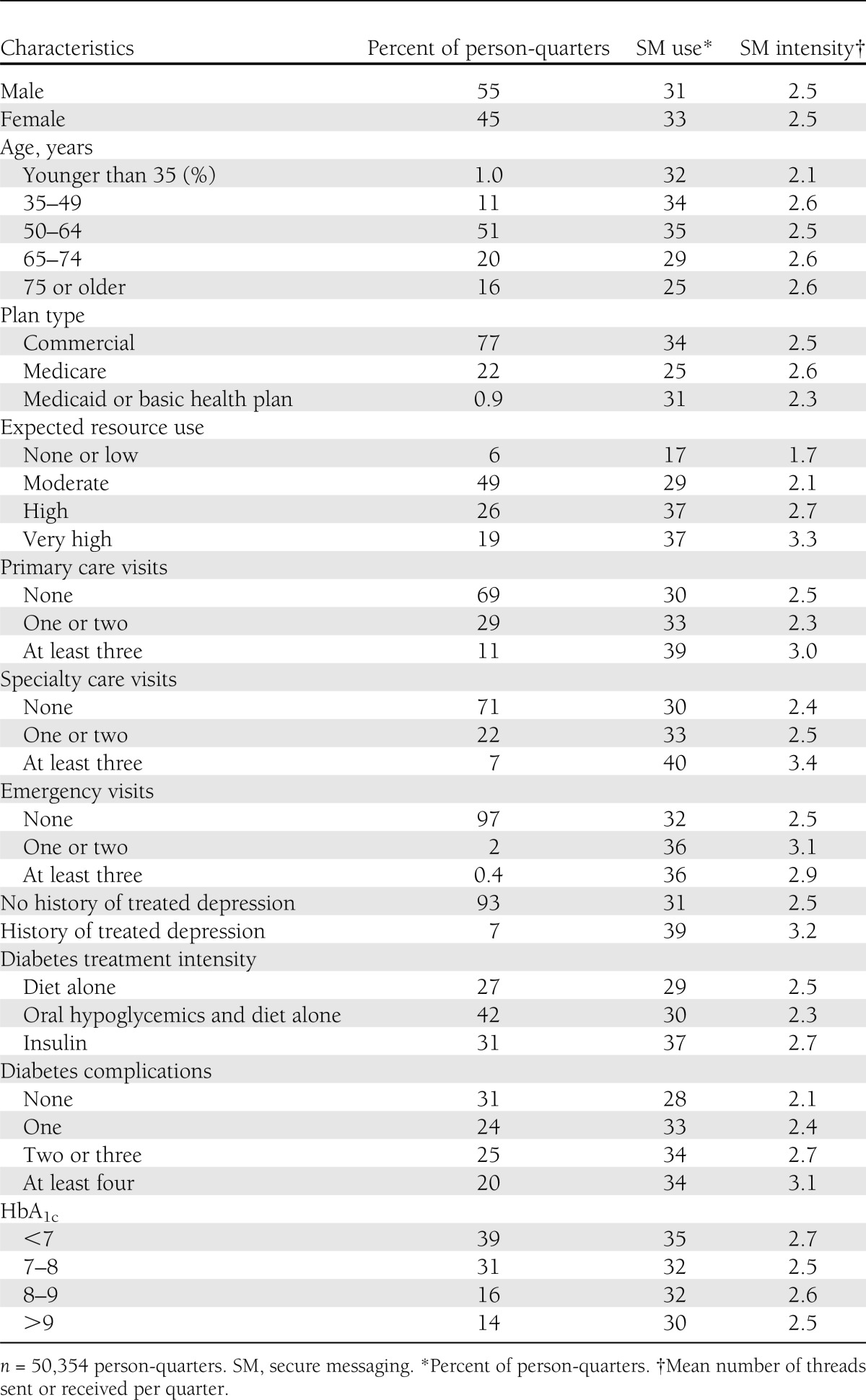
In unadjusted analyses, higher expected resource use and higher outpatient utilization were associated with greater secure messaging use (Table 1). In addition, use of insulin, a greater number of diabetes complications, and better glycemic control were associated with greater secure messaging use. Good control (HbA1c <7% vs. HbA1c >9%) was associated with a slightly higher rate of secure messaging use (35% vs. 30%) but a similar intensity of use (2.7 threads vs. 2.5 threads).
Table 1.
Demographic and health characteristics
Relationship between secure messaging and glycemic control
Relative risks estimated from inverse probability weighted models and multiply-imputed datasets differed by a mean absolute difference of 3%. Statistical significance was concordant in 11 of 12 trend tests. The adjusted rate of good glycemic control was monotonically higher in relation to higher levels of secure messaging in the previous quarter or previous year (HbA1c <7% and <8%: P < 0.05; Tables 2 and 3). The adjusted rate of poor control tended to be lower in relation to higher levels of secure messaging in the previous quarter (HbA1c >9%: P < 0.005). There was also a trend toward higher rates of poor control in relation to higher levels of secure messaging in the previous year (weighted observations: P = 0.006; imputed datasets: P = 0.205). A comparison of point estimates for all three outcomes suggested a larger effect when exposure to secure messaging was assessed during the previous quarter rather than the previous year.
Table 2.
Glycemic control in relation to secure messaging use (weighted observations)
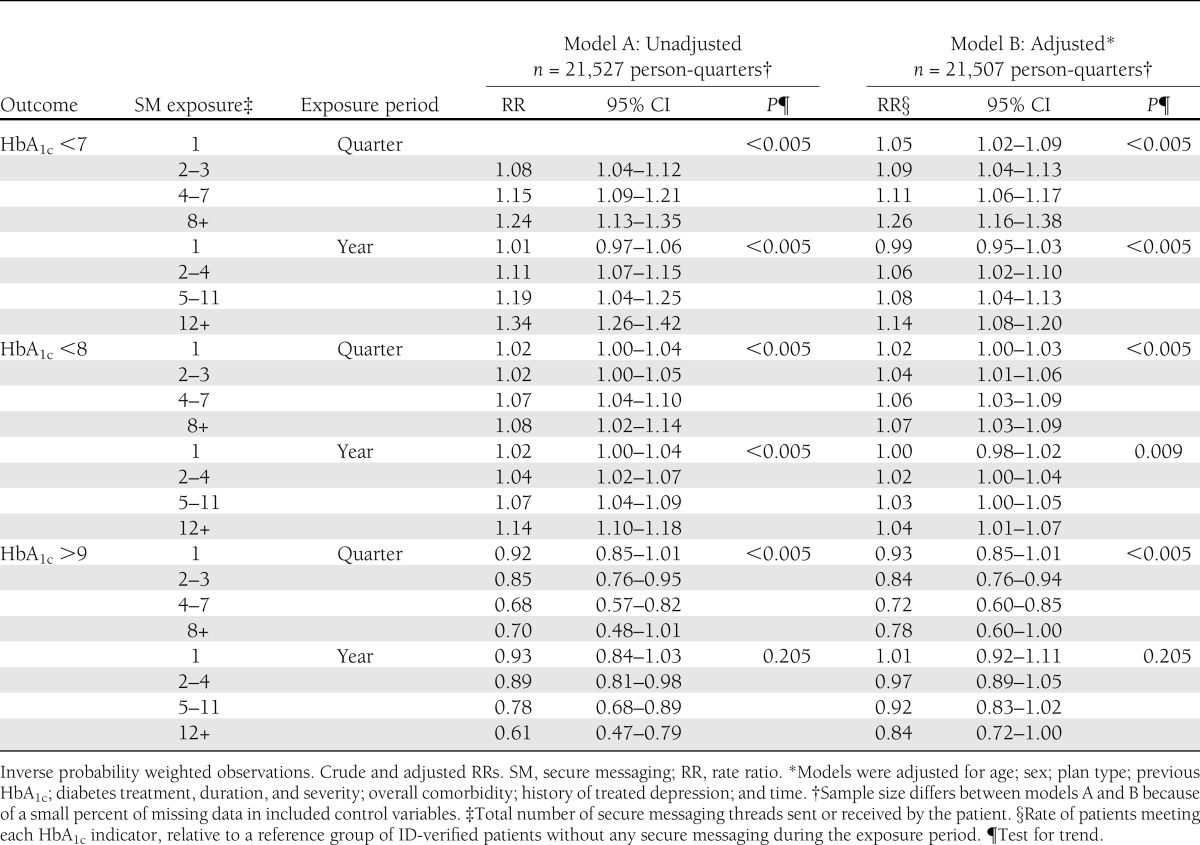
Table 3.
Glycemic control in relation to secure messaging use (imputed datasets)
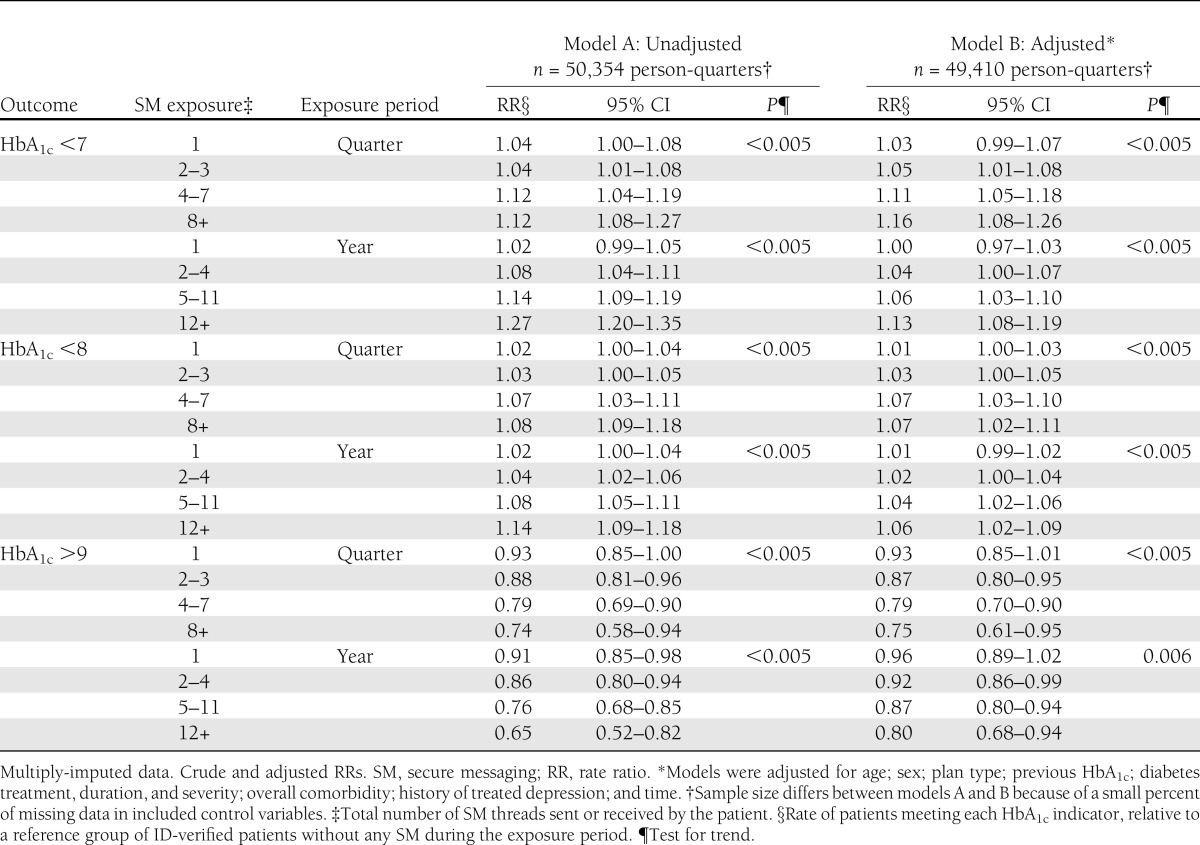
Final models were adjusted for age, sex, plan type, overall medical comorbidity, baseline HbA1c, diabetes severity, diabetes treatment type, diabetes duration, history of treated depression, and calendar time. We had initially hypothesized that secure messaging might have a greater effect in individuals with poor control. Accordingly, preliminary models included an interaction between previous secure messaging exposure and previous glycemic control. Interaction terms were nonsignificant, however, and therefore were excluded from final regression models. Results from completely unadjusted models were similar to results from adjusted models, with the estimated relative risks differing by a mean absolute difference of 6%.
Relationship between secure messaging and HbA1c testing
The adjusted rate of adherence to HbA1c testing twice yearly was monotonically higher in relation to higher levels of secure messaging (P < 0.005; Table 4). Adjusted relative rates were similar whether exposure to secure messaging was assessed during the previous quarter or the previous year.
Table 4.
HbA1c testing adherence in relation to secure messaging use
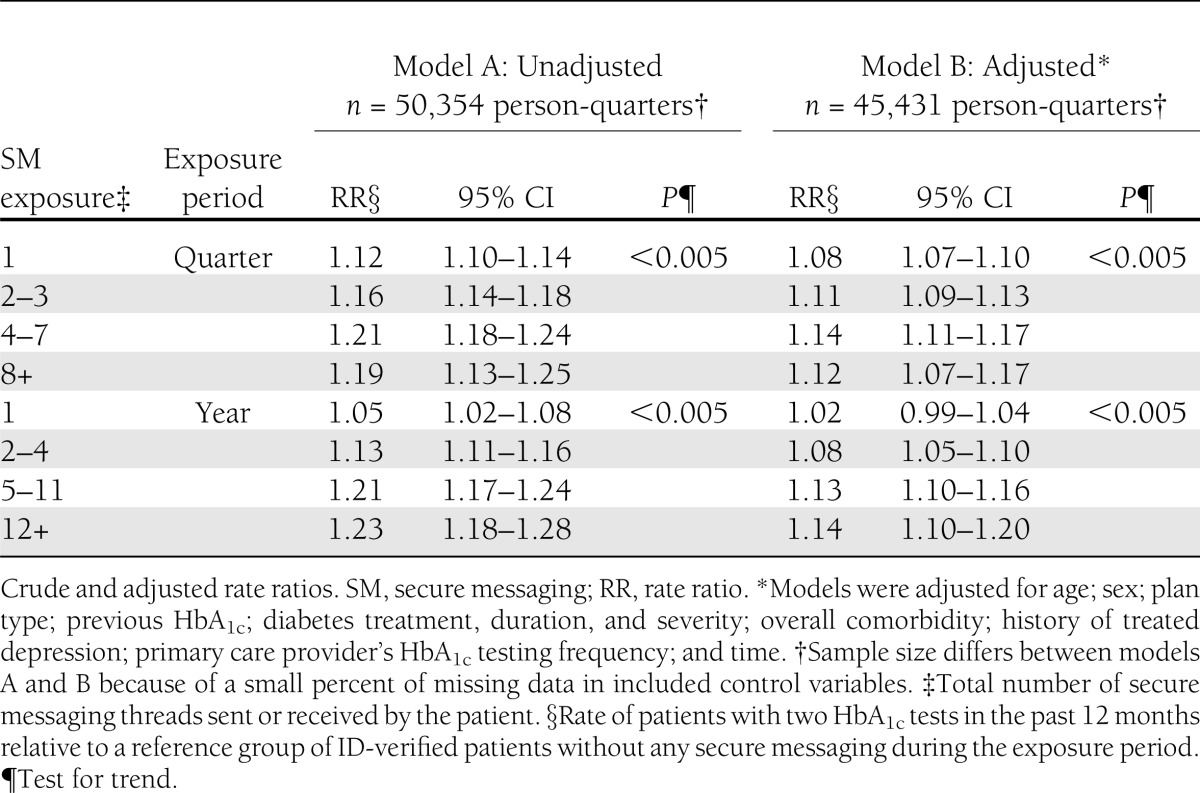
Final models included the same set of control variables as the models for glycemic control, with the addition of the HbA1c testing frequency of the patient’s primary care provider. Similar to models of glycemic control, preliminary models included an interaction between previous secure messaging exposure and previous glycemic control. Interaction terms were nonsignificant and excluded from final regression models. Results from completely unadjusted models were similar to results from adjusted models, with the estimated relative risks differing by a mean absolute difference of 12%.
CONCLUSIONS
In this analysis, patients with frequent use of secure messaging were more likely to achieve glycemic targets. In bivariate analyses, we observed relatively little difference in secure messaging (any use or intensity of use) by level of glycemic control. In multivariate models, rate ratios increased monotonically with increasing participation in secure messaging, suggesting a dose-dependent effect. Results from adjusted and unadjusted models differed, suggesting the association was partly moderated by the included control variables. For the lowest exposure category, one message thread, risk ratios were very close to 1 and suggestive of no effect. Similarly, risk ratios associated with moderately low exposure (two or three threads) were small and, although statistically significant in most cases, were not conclusive of a clinically relevant change.
The finding that more recent exposure was associated with a slightly larger effect would be compatible with a causal role of messaging. Overall, our results suggest that secure messaging may have a small positive effect on glycemic control, and that continued participation may be important for maximal benefit. Potential variables mediating the causal pathway between secure messaging and health outcomes are numerous, and may include changes to the treatment plan such as new prescriptions or dosage adjustments, health services use directly catalyzed by secure messaging, changes in patient attitudes (e.g., knowledge acquisition resulting in changes in self-management), or changes to the patient-provider relationship. Future work including content analyses of secure messaging threads or patient interviews could explore this issue in greater depth.
Frequent participation in secure messaging also was associated with increased adherence to testing recommendations, and the effects were similar when secure messaging exposure was assessed over the previous quarter or previous year. Secure messaging may modify testing frequency by increasing provider accessibility. For example, a patient may see a HbA1c test reminder in their online medical record and send a secure messaging to their primary care provider to follow-up and then ultimately schedule the test. Secure messaging also may help to promote testing adherence by strengthening the patient-provider relationship or increasing patient engagement. Alternatively, reverse causality may explain part of the observed association with testing frequency. Specifically, there was temporal overlap between the secure messaging exposure period (i.e., the previous quarter or previous year) and the period over which adherence was assessed (i.e., the previous year). For example, patients may have used secure messaging to follow-up on HbA1c results available in the electronic medical record. Likewise, providers may have used secure messaging to comment on recent HbA1c results, with or without any participation from the patient.
Strengths of our analysis include the large sample size, longitudinal design, heterogeneous population, and long duration of exposure to secure messaging. Our analysis has several limitations. Randomized assignment to secure messaging was not feasible, and observational analyses have a higher potential for bias. Our reference group of zero exposure to secure messaging was heterogeneous, including patients who may have used secure messaging during previous or subsequent quarters. There could be several important unmeasured potential confounders, including race, ethnicity, income, and education. In particular, nonwhite patients have been found to be less likely to use secure messaging, and also more likely to have poor glycemic control (31,32). Although we were able to use Medicaid enrollment as a proxy for low income, residual confounding attributable to income may be present. We sought to minimize, but may not have eliminated, the effects of self-selection by restricting our analysis to patients who signed-up for secure access to the shared electronic medical record. Patients who sign-up for the shared medical record but do not use secure messaging may be more similar to those who do use secure messaging in terms of unmeasured characteristics such as health-related self-efficacy and self-care behavior.
Furthermore, secure messaging is highly correlated with use of other services available from the shared medical record. Use of these services, independent of secure messaging, may explain part of the observed association. We chose not to control for this because use of online services may partly mediate our causal pathway of interest. For example, a secure messaging thread may catalyze use of the online portal to review medical records, schedule an appointment, or refill a prescription; any of these may ultimately impact glycemic control. Finally, we treated all secure message threads equally regardless of subject content or length.
Given that variables were collected at a quarterly frequency, we were unable to determine the temporal sequence of clinic visits and message threads within the same quarter. Clinic visits soon after engagement in messaging could mediate changes in glycemic control or HbA1c testing. In contrast, visits soon before secure messaging could represent a source of residual confounding. Patients with high levels of utilization may have systematically different outcomes than those with little or no utilization. Because we could not distinguish between mediation and confounding, we chose not to control for outpatient utilization.
We faced a significant missing data problem because of the fact that HbA1c was measured at irregular intervals and with a highly variable frequency across the diabetes population. A complex mix of patient and provider factors, including the underlying value of the measure itself, influences the measurement periodicity of HbA1c. We addressed this problem with two strategies: inverse probability weights and multiple imputation. The high concordance of results from these two approaches is reassuring.
Our findings are consistent with previous observational studies that have found an association between secure messaging and higher-quality diabetes care (6,7,9). Secure messaging also has been associated with better performance on process measures, including HbA1c, nephropathy, and retinopathy screening (7). Randomized controlled trials that have used secure messaging as part of diabetes case management have had mostly positive results (33–36). Our study adds to a growing body of evidence that secure messaging may have a small beneficial effect on process and outcome measures related to diabetes care. These findings may not generalize to settings with different payment models and plan types. Care providers in this study were salaried and received a small financial incentive for secure messages that were sent during the study period. Secure messaging was free to patients and widely advertised.
Our results cannot exclude the possibility that patients who participate in secure messaging achieve better outcomes simply because they are more engaged in their own self-care to begin with. In the absence of a randomized trial, it is impossible to completely eliminate this source of confounding and isolate the effect of secure messaging from the characteristics that may predispose a patient to use secure messaging. Further research is needed to disentangle these mechanisms and to determine how secure messaging interacts with the delivery of traditional outpatient services. As clinical information systems continue to evolve, it is likely that an increasing array of Web-based health care services will be available to patients in the coming years. Future studies also should carefully assess patient preferences for these new care modalities and rates of access, particularly in underserved populations. Previous work suggests that several higher-risk subgroups, including nonwhite, older, and low-income patients, have a significantly lower propensity to use Web-based patient resources (31,37,38). As online health care grows, it is important to remain cognizant of these differences in use so that existing disparities in diabetes outcomes do not widen.
Acknowledgments
Funding for this study was provided by grants R01 HS016759-01 (J.D.R.) and R21 HS017657-01 (David Grembowski) from the Agency for Healthcare Research and Quality.
No potential conflicts of interest relevant to this article were reported.
L.T.H. researched data and wrote the manuscript. T.D.K., S.J.H., D.P.M., and J.D.R. researched data and reviewed and edited the manuscript. L.T.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Beckjord EB, Finney Rutten LJ, Squiers L, et al. Use of the internet to communicate with health care providers in the United States: estimates from the 2003 and 2005 Health Information National Trends Surveys (HINTS). J Med Internet Res 2007;9:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sciamanna CN, Rogers ML, Shenassa ED, Houston TK. Patient access to U.S. physicians who conduct internet or e-mail consults. J Gen Intern Med 2007;22:378–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q 1996;74:511–544 [PubMed] [Google Scholar]
- 4.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78 [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, and American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home [Internet], March 2007. Available from http://www.acponline.org/advocacy/where_we_stand/medical_home/approve_jp.pdf Accessed 16 December 2011
- 6.Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: a cross-sectional analysis. Diabetes Care 2009;32:1182–1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou YY, Kanter MH, Wang JJ, Garrido T. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff (Millwood) 2010;29:1370–1375 [DOI] [PubMed] [Google Scholar]
- 8.Baer D. Patient-physician e-mail communication: the Kaiser Permanente experience. J Oncol Pract 2011;7:230–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bredfeldt CE, Compton-Phillips AL, Snyder MH. Effects of between visit physician-patient communication on Diabetes Recognition Program scores. Int J Qual Health Care 2011;23:664–673 [DOI] [PubMed] [Google Scholar]
- 10.Bergmo TS, Kummervold PE, Gammon D, Dahl LB. Electronic patient-provider communication: will it offset office visits and telephone consultations in primary care? Int J Med Inform 2005;74:705–710 [DOI] [PubMed] [Google Scholar]
- 11.Group Health Physicians. Quick Facts. Available from http://www.grouphealthphysicians.org/about/faqs.html
- 12.Ralston JD, Carrell D, Reid R, Anderson M, Moran M, Hereford J. Patient web services integrated with a shared medical record: patient use and satisfaction. J Am Med Inform Assoc 2007;14:798–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The National Committee for Quality Assurance. HEDIS 2012. Available from http://www.ncqa.org/tabid/78/Default.aspx#Vol_1 Accessed 1 September 2012
- 14.American Diabetes Association Executive summary: Standards of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl. 1):S4–S10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carrell D, Ralston J. Messages, strands and threads: measuring use of electronic patient provider messaging. In Proceedings of the 5th Annual Meeting of the American Medical Informatics Association, Washington, DC, 22–26 October 2005. Bethesda, MD, American Medical Informatics Association, p. 913. [PMC free article] [PubMed]
- 16.The Johns Hopkins ACG System, version 7.0 for Windows Baltimore, Johns Hopkins University, 1990–2006
- 17.Weiner JP, Starfield BH, Steinwachs DM, Mumford LM. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care 1991;29:452–472 [DOI] [PubMed] [Google Scholar]
- 18.Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care 2008;14:15–23 [PMC free article] [PubMed] [Google Scholar]
- 19.Dirmaier J, Watzke B, Koch U, et al. Diabetes in primary care: prospective associations between depression, nonadherence and glycemic control. Psychother Psychosom 2010;79:172–178 [DOI] [PubMed] [Google Scholar]
- 20.Papelbaum M, Moreira RO, Coutinho W, et al. Depression, glycemic control and type 2 diabetes. Diabetol Metab Syndr 2011;7;3:26 [DOI] [PMC free article] [PubMed]
- 21.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 2003;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petersen MR, Deddens JA. A comparison of two methods for estimating prevalence ratios. BMC Med Res Methodol 2008;8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–706 [DOI] [PubMed] [Google Scholar]
- 24.Yelland LN, Salter AB, Ryan P. Performance of the modified Poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol 2011;174:984–992 [DOI] [PubMed] [Google Scholar]
- 25.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1989;73:13–22 [Google Scholar]
- 26.White HA. Heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica 1980;48:817–830 [Google Scholar]
- 27.StataCorp Stata Statistical Software: Release 11. College Station, TX, StataCorp LP, 2009 [Google Scholar]
- 28.R Development Core Team R: A Language and Environment for Statistical Computing: Release 2.14.0. Vienna, Austria, R Foundation for Statistical Computing, 2011 [Google Scholar]
- 29.Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000;11:550–560 [DOI] [PubMed] [Google Scholar]
- 30.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, J. Wiley & Sons, 1987 [Google Scholar]
- 31.Lyles CR, Harris LT, Jordan L, et al. Patient race/ethnicity and shared medical record use among diabetes patients. Med Care 2012;50:434–440 [DOI] [PubMed] [Google Scholar]
- 32.Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care 2001;24:454–459 [DOI] [PubMed] [Google Scholar]
- 33.Goldberg HI, Ralston JD, Hirsch IB, Hoath JI, Ahmed KI. Using an Internet comanagement module to improve the quality of chronic disease care. Jt Comm J Qual Saf 2003;29:443–451 [DOI] [PubMed] [Google Scholar]
- 34.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care 2009;32:234–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCarrier KP, Ralston JD, Hirsch IB, et al. Web-based collaborative care for type 1 diabetes: a pilot randomized trial. Diabetes Technol Ther 2009;11:211–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lorig K, Ritter PL, Laurent DD, et al. Online diabetes self-management program: a randomized study. Diabetes Care 2010;33:1275–1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weppner WG, Ralston JD, Koepsell TD, et al. Use of a shared medical record with secure messaging by older patients with diabetes. Diabetes Care 2010;33:2314–2319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ralston JD, Rutter CM, Carrell D, Hecht J, Rubanowice D, Simon GE. Patient use of secure electronic messaging within a shared medical record: a cross-sectional study. J Gen Intern Med 2009;24:349–355 [DOI] [PMC free article] [PubMed] [Google Scholar]


