Abstract
Background
Neisseria meningitidis is a leading etiologic agent of severe invasive disease. The objective of the study was to characterise invasive meningococcal disease (IMD) epidemiology in Poland during the last decade, based on laboratory confirmed cases.
Methods
The study encompassed all invasive meningococci collected between 2002 and 2011 in the National Reference Centre for Bacterial Meningitis. The isolates were re-identified and characterised by susceptibility testing, MLST analysis, porA and fetA sequencing. A PCR technique was used for meningococcal identification directly from clinical materials.
Results
In the period studied, 1936 cases of IMD were confirmed, including 75.6% identified by culture. Seven IMD outbreaks, affecting mostly adolescents, were reported; all were caused by serogroup C meningococci of ST-11. The highest incidence was observed among children under one year of age (15.71/100,000 in 2011). The general case fatality rate in the years 2010–2011 was 10.0%. Meningococci of serogroup B, C, Y and W-135 were responsible for 48.8%, 36.6%, 1.2% and 1.2% of cases, respectively. All isolates were susceptible to third generation cephalosporins, chloramphenicol, ciprofloxacin, and 84.2% were susceptible to penicillin. MLST analysis (2009–2011) revealed that among serogroup B isolates the most represented were clonal complexes (CC) ST-32CC, ST-18CC, ST-41/44CC, ST-213CC and ST-269CC, and among serogroup C: ST-103CC, ST-41/44CC and ST-11CC.
Conclusions
The detection of IMD in Poland has changed over time, but observed increase in the incidence of the disease was mostly attributed to changes in the surveillance system including an expanded case definition and inclusion of data from non-culture diagnostics.
Introduction
Neisseria meningitidis is a leading etiologic agent of severe invasive disease characterized by rapid onset, of which meningitis and septicaemia are the most common and important manifestations [1], [2]. Meningococcal disease has a general case-fatality rate around 10%, however it is lower for meningitis (approximately 5%), and higher for septicaemia (from 5 to 40%, but even up to 70% in some studies) [1], [3]–[6]. Additionally, 11–19% of survivors may develop long-term sequelae [7], [8]. Although meningococcal infections may appear in every age group, infants and young children are at the highest risk of invasive meningococcal disease (IMD). A second peak of IMD incidence is observed in adolescence [9]. The disease may occur sporadically, as outbreaks or large epidemics; this last is characteristic for meningococci of serogroup A in Africa, and there are periodic fluctuations in IMD incidence and the occurrence of outbreaks and epidemics [1], [8]. In addition to the continuously changing epidemiology, IMD incidence and serogroup/clonal complex distribution are highly regional. Therefore, there is a necessity for comprehensive IMD monitoring to assess the local epidemiology and disease burden which may influence vaccine choice and prevention strategies, especially in light of serogroup- or protein-specific prophylaxis available [10].
The objective of the study was to characterise invasive meningococcal disease epidemiology in Poland during the last decade (2002–2011), based on laboratory confirmed cases and in particular to assess the IMD incidence, serogroup distribution, antimicrobial resistance patterns and molecular characteristics of isolates. This is the first such wide scale study on meningococcal isolates responsible for invasive infections in Poland.
Materials and Methods
Ethical Statement
Isolates were obtained as part of routine activity of the National Reference Centre for Bacterial Meningitis (NRCBM) and were analyzed anonymously. All data were collected in accordance with the European Parliament and Council decision for the epidemiological surveillance and control of communicable disease in the European Community [11], [12]. Ethical approval and informed consent were thus not required.
Country Background
In Poland, IMD is a notifiable disease. Every suspected case has to be reported by physicians to the local Sanitary Inspectorate within 24 hours of hospital admission. IMD cases are registered through two independent surveillance systems, a written documentation-based surveillance system run by the National Institute of Public Health-National Institute of Hygiene (NIPH-NIH) and a laboratory-confirmed surveillance system run by the NRCBM. The registration system of meningococcal disease has changed over the study period (2002–2011). Until 2005, both Polish surveillance systems collected data on meningococcal meningitis only, although the NRCBM was receiving sporadically isolates responsible for other invasive infections. Since 2005, a mandatory notification of all IMD cases has been introduced [5]. Additionally, the NRCBM started using a routine non-culture PCR method for IMD laboratory identification from 2005 onwards. Finally, the NRCBM system was reinforced by building a voluntary-based network (BINet) of hospital laboratories more deeply engaged in the surveillance of community-acquired invasive bacterial infections including IMD, in Poland in 2008. For laboratories involved in BINet, both the shipment and diagnostics of isolates or clinical materials are offered free of charge. The NRCBM receives meningococcal isolates, as well as data on demographic characteristics, antibiotic therapy, vaccination status, clinical diagnosis, and disease outcome if already available. In the majority of cases the outcome is unknown at time of isolate/material shipment. Therefore, from 2010 the NRCBM has started to actively obtain information concerning outcome by phone calls to reffering microbiologists or physicians.
At the beginning of the study the total Polish population was 38,242,197, of whom 1,919,827 (5.0%) were children younger than 5 years of age (data for 31st December 2001), while at the end of 2011, the population was 38,538,447, including 2,072,768 (5.4%) children under five years of age [http://demografia.stat.gov.pl/bazademografia/CustomSelect.aspx]. Estimates of the national census for 31st December of every year were used as the denominator for the calculation of annual incidence rates [http://www.stat.gov.pl/gus/5840_655_PLK_HTML.htm?action=show_archive].
Case Definition
A case of IMD was defined as the recovery of an isolate of N. meningitidis or meningococcal DNA from a normally sterile body site, such as blood, cerebrospinal fluid (CSF), joint aspirates, or tissues samples. In addition, isolates from the nose or nasopharynx were included in the analysis only if both, clinical symptoms of IMD were observed and positive PCR results were obtained from sterile body sites material. Only one isolate from each IMD case was included in the analysis.
Identification and Serogrouping
All isolates were identified based on typical morphology of colonies, Gram stain, oxidase test and API NH test (bioMerieux, Marcy l’Etoile, France) or Rapid NH System (Remel) according to the manufacturer’s instructions. Serogroups A, B, C, W-135 and Y were determined by slide agglutination tests using commercial antisera (Remel).
The NRCBM has also been receiving clinical materials (blood, cerebrospinal fluid or tissues samples) from patients with suspected IMD. The DNA isolated from these samples was used for polymerase chain reactions to identify N. meningitidis to the species and capsular group level [13], [14].
Susceptibility Testing
Minimal inhibitory concentrations (MICs) for penicillin, cefotaxime, chloramphenicol, rifampicin, and ciprofloxacin were determined by the broth microdilution method according to the Clinical and Laboratory Standards Institute (CLSI) guidelines up to June 2007, and subsequently by the E-test (AB Biodisk, Solna, Sweden) or MICEvaluators (Oxoid) methods according to manufacturers’ instructions [15] and interpreted according to the latest EUCAST guidelines [16]. Streptococcus pneumoniae ATCC 49619 strain was used as the quality control strain.
Multilocus Sequence Typing and Sequencing of porA and fetA Genes
The meningococci were also characterised by multilocus sequence typing and DNA sequencing of the porA and fetA genes, which encode outer membrane proteins [17], [18]. Sequence types (ST) and PorA and FetA types were determined via the meningococcal typing website [http://pubmlst.org/neisseria/].
Chi square test or Fisher’s exact test were used to analyse the differences in frequencies (Programme STATISTICA 10 trial); p-values ≤0.05 were considered to be significant.
Results
Descriptive Epidemiology of Invasive Meningococcal Disease Cases
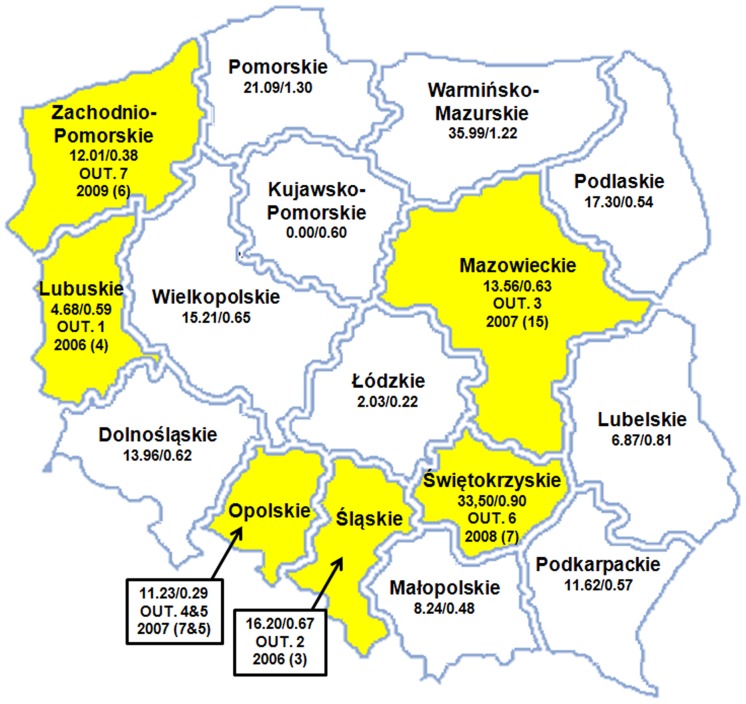
Between 2002 and 2011, the NRCBM confirmed 1936 cases of IMD, including 1463 (75.6%) identified by culture and 473 (24.4%) by PCR. The number of laboratory confirmed cases per year increased over the study period from 35 in 2002 to 337 in 2007, but subsequently decreased to 293 in 2011. Data on age were available for 1903 cases (98.3%). The incidence rates of IMD by age group in specific years are shown in Table 1. The highest incidence was observed among children under one year of age (15.71/100,000 in 2011), amongst whom 21.2% of all IMD cases occurred, and was also high in children under 5 years of age (in total 7.04/100,000 in 2011). There was also a second incidence peak in patients aged 15–19 years old (Table 1). Meningococci were isolated in hospitals located in all 16 voivodeships (regions) of Poland, but isolate submissions to the NRCBM and consequently incidence rates of IMD differed significantly among voivodeships as is shown for years 2010–2011 in Figure 1.
Table 1. The total annual incidence rates (/100,000) of invasive meningococcal disease (IMD)/meningitis rates in age groups in Poland based on laboratory-confirmed cases, including culture- and PCR-positive samples, 2002–2011 (only cases with known age were included when calculating the incidence) and total annual incidence rates of IMD registered by the compulsory notification system (NIPH-NIH).
| Age | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | %Casesa |
| in months | |||||||||||
| 0–11 | 3.97/3.40 | 3.15/1.72 | 7.91/5.08 | 5.24/3.86 | 8.32/4.56 | 15.02/9.32 | 16.94/11.86 | 15.59/8.40 | 11.14/7.02 | 15.71/9.27 | 21.2 |
| 12–23 | 0.83/0.83 | 2.27/0.85 | 4.30/2.58 | 2.54/1.69 | 5.24/3.31 | 6.98/3.22 | 10.09/6.73 | 6.28/4.59 | 7.17/4.78 | 8.21/4.83 | 11.0 |
| 24–35 | 0.53/0.53 | 1.38/1.10 | 1.14/0.85 | 3.44/2.29 | 2.26/1.70 | 3.31/1.38 | 3.76/1.88 | 6.72/3.36 | 3.62/1.93 | 4.84/3.00 | 6.3 |
| 36–47 | 0 | 0.53/0.53 | 1.10/0.55 | 1.42/1.42 | 1.72/1.72 | 5.37/2.54 | 3.04/1.38 | 5.10/3.49 | 3.62/2.58 | 4.17/3.24 | 5.1 |
| 48–59 | 0.26/0.26 | 0.26/0.26 | 0.80/0.53 | 1.93/1.66 | 0.85/0.57 | 2.58/0.86 | 2.55/1.41 | 2.21/1.66 | 2.15/1.07 | 2.97/1.98 | 3.2 |
| in years | |||||||||||
| 0–4 | 1.07/0.97 | 1.48/0.88 | 3.01/1.89 | 2.92/2.19 | 3.74/2.40 | 6.80/3.56 | 7.57/4.87 | 7.37/4.40 | 5.64/3.54 | 7.04/4.39 | 46.8 |
| 5–9 | 0.18/0.18 | 0.09/0.05 | 0.39/0.24 | 0.40/0.20 | 0.89/0.57 | 1.40/0.91 | 1.65/0.94 | 1.12/0.78 | 0.90/0.51 | 0.88/0.60 | 7.7 |
| 10–14 | 0.11/0.07 | 0.30/0.23 | 0.28/0.16 | 0.37/0.25 | 0.35/0.13 | 1.26/0.86 | 0.85/0.47 | 1.03/0.93 | 0.35/0.30 | 0.78/0.57 | 6.5 |
| 15–19 | 0.12/0.09 | 0.13/0.13 | 0.70/0.27 | 0.31/0.28 | 0.97/0.79 | 1.81/1.26 | 1.91/1.22 | 1.46/1.07 | 0.79/0.54 | 1.90/1.60 | 13.9 |
| 20–24 | 0.03/0.03 | 0.03/0.03 | 0.09/0.06 | 0.24/0.15 | 0.43/0.33 | 1.13/0.66 | 0.75/0.52 | 0.64/0.57 | 0.46/0.28 | 0.61/0.50 | 7.1 |
| 25–44 | 0.02/0.02 | 0.03/0.02 | 0.06/0.02 | 0.05/0.03 | 0.09/0.07 | 0.29/0.16 | 0.29/0.22 | 0.24/0.19 | 0.17/0.14 | 0.20/0.15 | 8.4 |
| 45–64 | 0 | 0.03/0.02 | 0.04/0.03 | 0.07/0.05 | 0.10/0.08 | 0.33/0.22 | 0.21/0.14 | 0.16/0.11 | 0.14/0.13 | 0.21/0.17 | 7.0 |
| 65+ | 0.02/0.02 | 0.06/0.02 | 0.06/0.02 | 0.02/0.02 | 0.02/0 | 0.16/0.04 | 0.17/0.12 | 0.17/0.10 | 0.10/0.06 | 0.19/0.11 | 2.6 |
| All ages | 0.09/0.08 | 0.13/0.09 | 0.28/0.15 | 0.26/0.19 | 0.40/0.28 | 0.88/0.52 | 0.86/0.56 | 0.77/0.53 | 0.54/0.37 | 0.76/0.53 | 100 |
| No cases b | 35 | 51 | 106 | 99 | 154 | 337 | 327 | 294 | 207 | 293 | 1903 |
| % PCR+ c | 0 | 0 | 0 | 7.1 | 11.7 | 27.6 | 34.3 | 34.4 | 23.7 | 27.6 | 24.2 |
| Men-cult. d | 0.08 | 0.09 | 0.15 | 0.17 | 0.25 | 0.39 | 0.37 | 0.33 | 0.28 | 0.38 | 0.08 |
| NIPH-NIH e | 0.22 | 0.17 | 0.29 | 0.55 | 0.61 | 1.04 | 0.97 | 0.81 | 0.60 | 0.77 |
%Cases - percentage of IMD cases in age group among all cases;
No cases - total number of cases in a particular year;
percentage of cases identified by PCR in a particular year;
Men-cult. - incidence rates of meningitis confirmed by culture only;
NIPH-NIH – total incidence of invasive meningococcal disease for all age groups registered by compulsory notification system run by the National Institute of Public Health – National Institute of Hygiene (Available: http://www.pzh.gov.pl/oldpage/epimeld/index_p.html. Accessed 2013 May 24).
Figure 1. Map of Poland with the incidence rates (per 100,000) of invasive meningococcal disease in children under 1 year of age/all age groups, in 16 voivodeships, in years 2010–2011.
The voivodeships with notified outbreaks during study period are marked in yellow (OUT. – outbreak, numbered like in the text, the year of the outbreak, in bracket there is number of outbreak cases).
Of 1936 N. meningitidis isolates, 1002 (51.8%) were recovered from CSF, 901 (46.5%) from blood, 25 (1.3%) from post mortem tissue samples, 7 (0.4%) from the nasopharynx, and 1 from joint fluid. Among all the patients, 42.4% were diagnosed as having meningitis, 22.3% with sepsis, 23.9% with meningitis and sepsis, and the remaining 11.5% with other manifestations or undetermined IMD. The patients’ age ranged from 1 day to 87 years (median, 6 years). Among 1920 patients with reported gender, 55.7% were male.
The case fatality rate (CFR) was assessed for IMD between 2010 and 2011, as the outcome was known for 91.6% of cases during this period, whereas in the years from 2002 to 2009 such information was available for 25.1% of cases only. CFR data are shown in Table 2. The general CFR was 10.0% for cases with known outcome only, and was highest in patients aged ≥65 years (46.2%, p = 0.001), although the incidence of IMD was lowest in that age group. The highest CFR was found in patients with sepsis (22.4%), as compared to patients with meningitis and sepsis (7.0%, p = 0.0007) and to meningitis alone (3.1%, p<0.0001).
Table 2. Incidence of invasive meningococcal disease (/100,000) case fatality rate (CFR) and percentage of cases with sequelae in age groups in Poland, 2010–2011 (only cases with known outcome were included when calculating the CFR, n = 458).
| Age | Incidence | Total CFR (%) | MenBCFRa | MenCCFRb | Sequelae (%) |
| in months | |||||
| 0–11 | 13.36 | 10.9 | 9.3 | 14.3 | 3.0 |
| 12–23 | 7.69 | 8.6 | 9.8 | 5.9 | 3.4 |
| 24–35 | 4.24 | 17.6 | 26.7 | 11.1 | 0.0 |
| 36–47 | 3.91 | 6.9 | 7.1 | 6.7 | 3.4 |
| 48–59 | 2.57 | 5.0 | 10.0 | 0.0 | 5.0 |
| in years | |||||
| 0–5 | 6.35 | 10.3 | 11.0 | 9.0 | 2.9 |
| 5–9 | 0.89 | 12.5 | 9.5 | 10.0 | 3.1 |
| 10–14 | 0.56 | 5.6 | 12.5 | 0.0 | 5.6 |
| 15–19 | 1.33 | 3.7 | 3.7 | 6.5 | 1.9 |
| 20–24 | 0.53 | 15.4 | 23.5 | 0.0 | 3.8 |
| 25–44 | 0.18 | 7.9 | 0.0 | 9.5 | 2.6 |
| 45–64 | 0.17 | 2.9 | 0.0 | 6.7 | 5.7 |
| 65+ | 0.14 | 46.2 | 37.5 | 50.0 | 7.7 |
| All ages | 0.65 | 10.0 | 10.3 | 8.8 | 3.3 |
MenB CFR - case fatality rate associated with infections caused by serogroup B meningococci;
MenC CFR - case fatality rate associated with infections caused by serogroup C meningococci.
Establishment of BINet contributed to a slight increase of IMD detection by laboratories involved in the network, from 60.8% before 2008 to 61.8% since 2008 and increase of IMD detected by PCR, from 59.1% before 2008 to 63.4% since 2008. However, these values were not statistically significant.
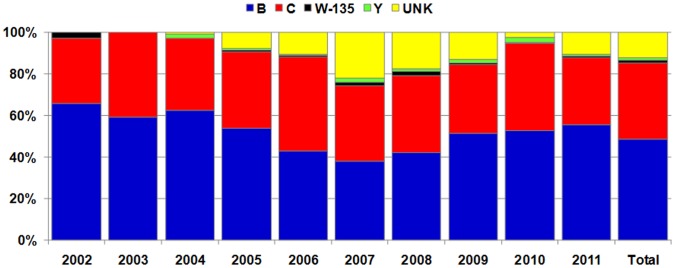
Serogroup Distribution among N. meningitidis
The serogroup was identified for 1700 (87.8%) cases, including 1445 IMD cases confirmed by culture and 255 by PCR. Out of all meningococcal cases, 944 (48.8%) were caused by serogroup B (MenB), 709 (36.6%) by serogroup C (MenC), 24 (1.2%) by serogroup Y (MenY) and 23 (1.2%) by serogroup W-135 (MenW-135). The serogroup was not identified or causative isolates were nongroupable in 236 (12.2%) cases, of which 92.4% were identified by PCR. Serogroup distribution of meningococci responsible for invasive infections in Poland between 2002 and 2011 is presented in Figure 2. The data on the incidence of IMD caused by isolates of particular serogroups and serogroup distribution by age groups over the years 2002–2006 and 2007–2011 is shown in Table 3. The results were separated because the incidence rates were significantly different for the two periods.
Figure 2. Serogroup distribution of meningococci responsible for invasive infections in Poland, 2002–2011.
(n = 1936; UNK - cases with unknown serogroup).
Table 3. Incidence rates (/100,000) of invasive meningococcal disease caused by isolates of particular serogroups and serogroup distribution in age groups in Poland, 2002–2006 and 2007–2011.
| Incidence per100,000/serogroup distribution in age group, % | ||||||||||
| 2002–2006 | 2007–2011 | |||||||||
| Age | B | C | W-135 | Y | UNKa | B | C | W-135 | Y | UNKa |
| in months | ||||||||||
| 0–11 m | 4.30/74.8 | 1.12/19.4 | 0.11/1.9 | 0/0 | 0.22/3.9 | 9.72/65.3 | 3.17/21.3 | 0.10/0.7 | 0.10/0.7 | 1.78/12.0 |
| 12–23 m | 1.91/63.0 | 0.90/29.6 | 0/0.0 | 0.06/1.9 | 0.17/5.6 | 4.99/64.5 | 1.84/23.9 | 0.05/0.6 | 0/0 | 0.85/11.0 |
| 24–35 m | 0.84/48.4 | 0.72/41.9 | 0.06/3.2 | 0/0 | 0.11/6.5 | 2.18/48.9 | 1.78/39.8 | 0.10/2.3 | 0/0 | 0.41/9.1 |
| 36–47 | 0.49/52.9 | 0.33/35.3 | 0/0 | 0.05/5.9 | 0.05/5.9 | 1.83/43.2 | 1.83/43.2 | 0/0 | 0.05/1.2 | 0.52/12.3 |
| 48–59 m | 0.38/46.7 | 0.43/53.3 | 0/0 | 0/0 | 0/0 | 1.30/52.2 | 0.71/28.3 | 0/0 | 0/0 | 0.49/19.6 |
| in years | ||||||||||
| 0–4 | 1.57/64.5 | 0.70/28.6 | 0.03/1.4 | 0.02/0.9 | 0.11/4.5 | 4.09/59.4 | 1.89/27.5 | 0.05/0.7 | 0.03/0.4 | 0.82/11.9 |
| 5–9 | 0.20/53.8 | 0.16/41.0 | 0/0 | 0/0 | 0.02/5.1 | 0.46/38.9 | 0.47/39.8 | 0/0 | 0/0 | 0.25/21.3 |
| 10–14 | 0.08/28.6 | 0.20/71.4 | 0/0 | 0/0 | 0/0 | 0.23/27.0 | 0.48/55.1 | 0.01/1.1 | 0.02/2.2 | 0.13/14.6 |
| 15–19 | 0.13/30.8 | 0.24/55.4 | 0/0 | 0.01/1.5 | 0.05/12.3 | 0.48/30.2 | 0.84/53.3 | 0.02/1.5 | 0.04/2.5 | 0.20/12.6 |
| 20–24 | 0.07/40.7 | 0.09/55.6 | 0/0 | 0/0 | 0.01/3.7 | 0.29/39.8 | 0.22/29.6 | 0.03/4.6 | 0.02/2.8 | 0.17/23.1 |
| 25–44 | 0.03/53.8 | 0.02/46.2 | 0/0 | 0.0 | 0/0 | 0.08/34.6 | 0.11/48.1 | 0.00/0.8 | 0/0 | 0.04/16.5 |
| 45–64 | 0.03/58.3 | 0.01/25.0 | 0/0 | 0.00/4.2 | 0.01/12.5 | 0.11/51.4 | 0.07/30.6 | 0.00/1.8 | 0.01/4.5 | 0.02/11.7 |
| 65+ | 0.02/55.6 | 0.02/44.4 | 0/0 | 0/0 | 0/0 | 0.09/57.5 | 0.05/30.0 | 0.00/2.5 | 0.01/5.0 | 0.01/5.0 |
| All ages | 0.12/53.3 | 0.09/39.8 | 0.00/0.7 | 0.00/0.9 | 0.01/5.4 | 0.36/47.5 | 0.27/35.9 | 0.01/1.2 | 0.01/1.4 | 0.11/13.9 |
UNK – cases with unknown serogroup.
The case fatality rate associated with MenB infections was slightly higher (10.3%) than with MenC (8.8%, p = 0.73) but this finding was not statistically significant (Table 2).
Antimicrobial Susceptibility
Antimicrobial susceptibility testing was performed for 1373 meningococcal isolates. Most of them (n = 1156, 84.2%) were highly susceptible to penicillin, however, 197 (14.3%) showed intermediate susceptibility, and 20 (1.5%) resistance. In general MenB were more often non-susceptible to penicillin (19.0%) than those of MenC (11.3%, p = 0.0002). Although not statistically significant, non-susceptibility to penicillin was the most common in children under one year of age, in whom MenB infections were the most frequent in comparison to the whole population (36.6% vs 28.9%, p = 0.24) All isolates tested were susceptible to third generation cephalosporins, chloramphenicol and ciprofloxacin. Only 4 isolates (0.3%) were resistant to rifampicin, including 2 of MenB with MICs of 0.5 and 0.75 mg/l, respectively, one of MenC with an MIC of 0.5 mg/l and one of MenW-135 with an MIC of >32 mg/l.
MIC, MIC50 and MIC90 ranges (in mg/l) were as follows: for penicillin < = 0.0075–1.0, 0.03–0.06 and 0.06–0.012, respectively; for third generation cephalosporins < = 0.0008–0.12, 0.0016–0.004 and 0.003–0075, respectively; for chloramphenicol, 0.25–2.0, 0.5–2 and 1–2, respectively: for ciprofloxacin < = 0.002–0.015, 0.002–0.015 and 0.004–0.015, respectively; for rifampicin 0.002->32, 0.008–0.06 and 0.047–0.25, respectively. Analysis of meningococcal susceptibility did not reveal any significant differences in their percentages, values of MIC50 and MIC90, and MICs ranges, through the whole period studied.
Based on data between 2010 and 2011, infections caused by isolates non-susceptible to penicillin were not associated with higher CFR in comparison to susceptible ones (9.8% vs 8.5%, p = 0.89).
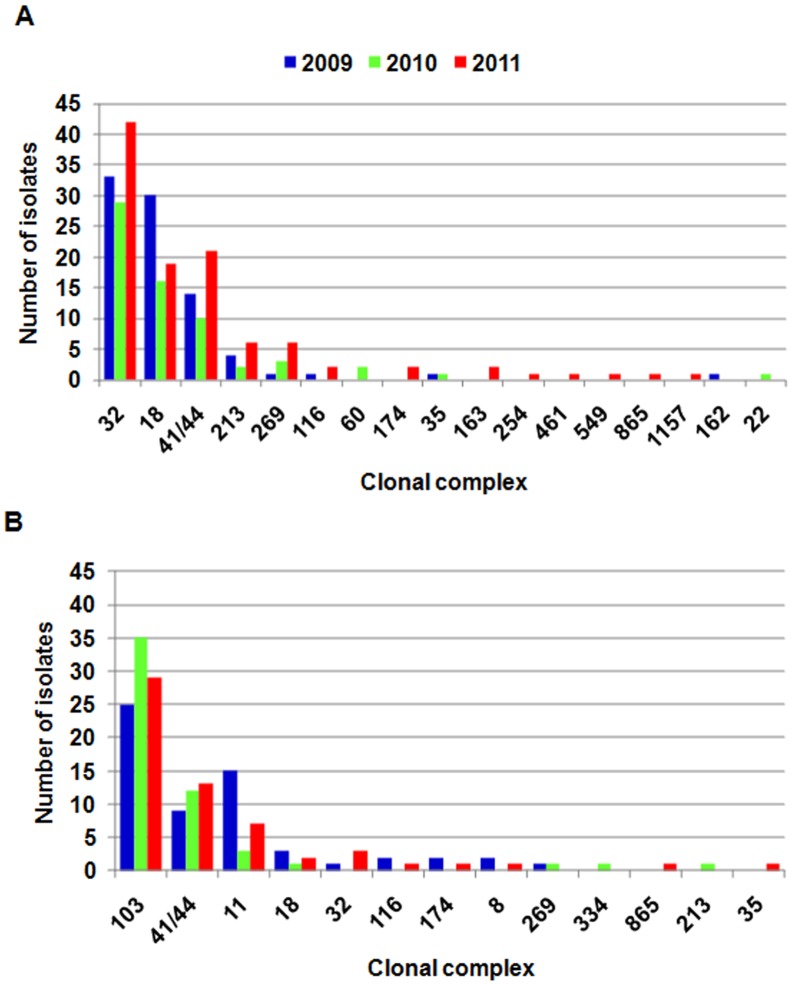
Molecular Characteristics
MLST analysis, porA and fetA sequencing started to be routinely performed in the NRCBM since 2009 and therefore molecular analysis included isolates collected between 2009 and 2011. MLST analysis revealed 164 STs among MenB isolates, of which 79.1% belonged to eighteen international clonal complexes (CC). Despite the diversity, five major CCs (ST-32CC, ST-18CC, ST-41/44CC, ST-213CC and ST-269CC) grouped 73.5% of all MenB isolates studied.
Among MenC isolates 58 STs were identified. Although 81.6% of MenC meningococci belonged to thirteen international clonal complexes (CC), 69.8% were grouped in three of the most predominant CCs (ST-103CC, ST-41/44CC and ST-11CC). Meningococci of ST-11CC and ST-103CC belonged exclusively to serogroup C and of ST-32CC, ST-18CC, ST-213CC and ST-269CC mostly to serogroup B, whereas ST-41/44CC meningococci belonged to both serogroups. Molecular characterization of the most represented clonal complexes (with at least 10 isolates) of MenB and MenC is summarized in Table 4. The distribution of CCs among Polish meningococci of MenB and MenC between 2009 and 2011 is shown in Figure 3.
Table 4. Molecular characterization of meningococcal isolates of serogroup B and C belonging to the most dominant clonal complexes (CC) represented at least by 10 isolates, 2009–2011.
| Serogroup B (n = 321) | Serogroup C (n = 212) | |||||||
| Clonal complex (CC) | ST-32CC | ST-18CC | ST-41/44CC | ST-213CC | ST-269CC | ST-103CC | ST-41/44CC | ST-11CC |
| Number of isolates in CC | 104 | 65 | 45 | 12 | 10 | 89 | 34 | 25 |
| % B or C | 32.4% | 20.2% | 14.0% | 3.7% | 3.1% | 42.0% | 16.0% | 11.8% |
| STa (n) | 15 | 42 | 19 | 4 | 9 | 4 | 14 | 3 |
| Most common ST | ST-32 (71) | ST-145 (17) | ST-1194 (13) | ST-213 (7) | ST-479 (2) | ST-5133 (85) | ST-3346 (8). ST-5323 (8) | ST-11 (23) |
| PorA VR1,VR2 variants (n) | 12 | 22 | 21 | 2 | 7 | 5 | 11 | 6 |
| Most common PorA VR1,VR2 | ||||||||
| combination (n) | 7, 16 (57) | 22, 14 (17) | 7-2, 4 (12) | 22, 14 (11) | 19-1,15-11 (3) | 18-1, 3 (65) | 17, 16-4 (17) | 5, 2 (14) |
| FetA variants (n) | 8 | 25 | 11 | 3 | 7 | 2 | 6 | 2 |
| Most common FetA variant (n) | F3-3 (85) | F1-17 (10) | F1-5 (29) | F5-5 (10) | F5-1 (3) | F3-9 (86) | F3-9 (18) | F3-3 (14) |
ST – sequence type.
Figure 3. Distribution of clonal complexes between 2009 and 2011 among Polish meningococci of serogroup B (A) and C (B).
Between 2009 and 2011, four isolates of MenW-135 were identified which belonged to four different STs. Only one of these belonged to a recognized international CC, ST-22CC. Sequencing of porA and fetA genes also confirmed the heterogeneity of the isolates. All five MenY belonged to international CCs: ST-22CC, ST-23CC, ST-92CC and ST-167CC (n = 2). Three MenY isolates shared the same PorA VR1 (5-1) and FetA (F4-1), and two the same VR2 (10-1).
Geographic analysis of clonal complex prevalence revealed that isolates of ST-11CC were more often responsible for infections in the West of Poland than in the East (7.1% vs 1.6%, p = 0.006), especially in Wielkopolskie and Zachodnio-Pomorskie voivodeships (in which the last documented outbreak took place) [19]. Representatives of this clone were also more often identified among isolates from 2009 in comparison to 2010 (8.1% vs 1.9%, p = 0.03).
Meningococci of ST-11CC were more frequently isolated from persons over 5 years of age (8.2%, p = 0.0004) and in particular from individuals 15–24 years old (13.7%, p<0.0001) in comparison to children under 5 years of age (1.1%). In contrast, meningococci of ST-18CC more often affected children under 5 years of age than persons over 5 years old (18.2% vs 7.8%, p = 0.003). This last CC was associated with the highest CFR (26.3%) in comparison with the whole Polish meningococcal population (8.7%, p = 0.002); however, this high CFR was not associated with any particular ST within ST-18CC. Although not statistically significant, the CFR was slightly higher for infections caused by isolates belonging to any of the recognised CCs (9.2%) compared to those not associated with any CCs (6.3%). Interestingly, non-susceptibility to penicillin was most prevalent among the isolates not belonging to any international CC (47.8% vs 28.8%, p = 0.003) and least prevalent among meningococci of ST-103CC, in comparison to the whole meningococcal population (4.9% vs 28.8%, p = 0.003).
For other CCs there were no significant differences in respect to CFR, geographical, temporal and age group distribution.
IMD Outbreaks
Between 2002 and 2011, seven outbreaks were notified in Poland, affecting mostly adolescents [19]–[22]. All of them were caused by MenC of ST-11.
The ST-11 isolates have been notified in Poland since 1998 but until 2006 were responsible for 0–2 cases annually. In March 2006, the first outbreak (OUT.1 in the Figure 1) with 4 cases in army recruits took place at a military base in Lubuskie voivodeship in the West of Poland [22]. In June 2006 IMD was diagnosed in three teenage friends in Bytom (Śląskie voivodeship, OUT.2) based on characteristic clinical symptoms. The cases were not laboratory confirmed due to sampling being delayed until the commencement of antibacterial therapy, however ST-11 meningococci were isolated from the nasopharynx from four of their close contacts. Consequently, it was assumed that isolates of that clone were responsible for the outbreak [20]. In January 2007, 15 cases of IMD, including 2 fatal at a Warsaw military base (Mazowieckie voivodeship, OUT.3) were laboratory confirmed primarily using PCR or an antigen test. MLST analysis of five cases confirmed ST-11 meningococci [20]. In 2007, outbreaks of IMD were notified in two counties, Brzeg (7 cases, OUT.4) and Kluczbork (4 cases, OUT.5), in Opolskie voivodeship. Molecular analysis of available isolates revealed meningococci of ST-11 [21]. At the beginning of 2008, an outbreak (OUT.6) of 7 IMD cases, also caused by ST-11, was reported in Świętokrzyskie voivodeship. All of the above outbreaks were caused by ST-11 meningococci with a PorA variant P1.5-1,10-1, while those identified in Poland between 1997 and 2005 had PorA variant P1.5,2 [19].
Finally, in an outbreak (OUT.7) in Goleniów county of Zachodnio-Pomorskie voivodeship in March 2009, 6 IMD cases in individuals aged from 7 to 25 years of age were caused by ST-11. Interestingly, the Goleniów county isolates had an FetA variant (F3-3) that differed from all sequenced ST-11 isolates responsible for IMD cases before 2009 in Poland (generally, these were F3-6, with only two isolates having F3-9). Additionally, the isolates responsible for the Goleniów county outbreak had the same PorA variant as that of ST-11 meningococci isolated before 2006 (P1.5,2) [19]. Geographical sites of outbreaks are presented in Figure 1.
At two military bases and four other locations – two each in Opolskie, Świętokrzyskie and Zachodnio-Pomorskie voivodeships - vaccination campaigns against MenC were organized resulting in a high vaccine coverage [19]–[22].
Discussion
The epidemiology of IMD is very dynamic and characterised by significant variation in the incidence, serogroup and sequence type/clonal complex distribution [23]. It is influenced by the patients’ age, geographic region, season, period studied and vaccination policy. Consequently, continuous laboratory-based surveillance of meningococcal isolates is needed in order to ensure appropriate IMD management and control. IMD laboratory-based surveillance in Poland has revealed a remarkable increase in IMD cases over the last decade. However, despite possible changes in the epidemiology, the rise in IMD has mainly been influenced by changes to the Polish surveillance system. Up to 2005, only meningococcal meningitis cases were notified in Poland; however, mandatory notification of all invasive cases has been required since then [5], [24]. Additionally, the NRCBM introduced a routine PCR-based diagnostic test (i.e. not culture-based) for identification of IMD in 2005. PCR is more sensitive and provides a more-accurate estimation of the incidence as shown by the fact that during the last five years 24–34% of all IMD cases in Poland were confirmed by this technique alone. Such increases in IMD detection following PCR introduction were also observed in other countries [10], [25], [26]. Finally, the laboratory-based system was reinforced by BINet activity in 2008 [27], [28]. The reinforcement due to the establishment of BINet did not result in a major increase in laboratory notifications of IMD. It could be explained by the fact that the medical community and general public were already very much alerted following six high-profile IMD outbreaks between 2006 and 2008, and the associated educational campaigns, that occurred immediately prior to the start of BINet activity [20]–[22]. All of the above mentioned formal changes in the Polish notification system resulted in an expected increase in overall IMD incidence rates. However, the simultaneous increase in culture-confirmed meningitis incidence rates may have been due to better surveillance and/or possible changes in IMD epidemiology in Poland (Table 1).
Between 2005 and 2011 Poland ranked among countries with an overall low IMD incidence rates ranging from 0.26 to 0.88 per 100,000 inhabitants. In 2009, IMD incidence rates in Europe varied widely between countries based on an ECDC assessment, ranging from 0.13 to 3.01 per 100,000 inhabitants, giving an average of 0.98 per 100,000 inhabitants [29]. As expected, the highest incidence of IMD was observed in children. The results of our study showed that 46.8% of all cases affected children under five years of age, including 21.2% of children aged less than one year. The general laboratory-confirmed incidence rate of IMD, 6.88/100,000 in Polish children under five years of age in the years from 2007 to 2011 was similar to that observed in Europe in 2009 (7.37/100,000) [29]. However, the average IMD incidence rate 14.87/100,000 between 2007 and 2011 in children aged under one year was lower in comparison to the average data for 27 European countries from 2006 (approximately 20/100,000) [10]. It is worthy emphasizing that geographic analysis revealed high variations in IMD incidence rates in children under one year of age between Polish regions (0.0 vs 35.99/100,000). This may be due to a diverse epidemiological situation, but more probably results from differences in the effectiveness of the monitoring system in place, which is strongly affected by insufficient/low frequency of blood culturing and blood samples submission to the NRCBM for PCR diagnostic [27], [30].
Universal vaccination against IMD has so far not been implemented in Poland, although the anti-meningococcal conjugated vaccines are registered and highly recommended. Until 2002, more than 85% of IMD cases in Poland were caused by MenB but from that year onwards a country-wide increase of IMD due to MenC was observed reflecting the rapidly changing epidemiology of this disease [31]. Our results also revealed that most cases of meningococcal disease are caused by MenB, although in some years of the study the proportions of serogroup B and C isolates were comparable. Similarly, MenB and MenC disease dominated in Europe at the end of the 20th Century; however, MenB are currently responsible for more than 85% of infections in countries with mass vaccination against MenC [32]–[34]. In our study, MenB infections predominated in children less than 1 year of age, but despite this the incidence of MenC disease was also highest in that age group in comparison to the other age groups. Such observations were also characteristic for other European countries [34], [35]. Unexpectedly, a rapid rise in the number of MenY infections was noticed in some countries, in both recent and previous studies, although our results did not demonstrate such an increase in Poland [36]–[38].
Even with limited data on disease outcome, our study showed that fatality differs by patient age and the manifestation of infection, but is independent of non-susceptibility to antibiotics as previously described [39]. The overall CFR found during our study (10.0%) was higher than the mean CFR of 7.8% found in other European countries. The CFR associated with MenB infections was higher (10.3% vs 6.5%), whereas that related to MenC was lower (8.8% vs 12.3%) in our study in comparison to the European average [35]. Surprisingly, in our study a low percentage of sequelae was notified in comparison to other authors, which is difficult to explain but it may be associated with poor reporting of sequelae or with reporting of very severe sequelae only [7], [8].
Most of the Polish meningococcal isolates were highly susceptible to penicillin; however, 15.8% of them showed some degree of decreased susceptibility to this antibiotic and the proportion of these strains has been gradually increasing [40]. The proportion of such isolates varies widely from country to country [41]. During our study we found four isolates that were resistant to rifampicin according to the latest EUCAST criteria [16]. However, according the latest CLSI criteria, as well as criteria proposed by the authors of a multi-centre study to establish the breakpoint for rifampicin resistance in meningococci by rpoB sequencing, rifampicin susceptible isolates should be defined as those with MICs of <1 mg/l. Using this breakpoint, only one of the isolates had an MIC of >32 mg/l, which would make it resistant to rifampicin [15], [42].
As shown in other countries, the population of MenB analysed during our study was much more diverse than the population of MenC meningococci [10]. Despite that, the majority of Polish MenB belonged to well known and widely distributed clonal complexes, namely ST-32CC, ST-18CC and ST-41/44CC [33,34; http://pubmlst.org/neisseria/]. Meningococci of the ST-32 complex, have been responsible for many epidemic and sporadic IMD cases worldwide, for example in Norway, Spain, Cuba, Brazil, Oregon in the USA and Normandy in France [43]–[45]. Isolates of ST-32 with PorA VR1,VR2 combination 7, 16 and FetA F3-3 of our study were similar to an epidemic clone found in Norway and Oregon (B:15:P1.7,16), which was confirmed by serotyping some of the Polish ST-32 MenB isolates using an ELISA (data not shown).
ST-18CC was very diverse given that 42 STs, 22 PorA VR1,VR2 combinations and 25 FetA variants were found amongst 65 isolates. Meningococci of this clonal complex were responsible for more than 3 times higher CFR in comparison to the whole Polish meningococcal population.
As previously mentioned, an increase in the proportion of MenC among all IMD cases has been observed since 2002. This was related to the rise of cases caused by meningococci of two clonal complexes ST-8CC and ST-103CC, which were not previously identified in Poland, apart from one case due to ST-8CC meningococci in 2001. Interestingly, the emergence of ST-8CC in some countries resulted in mass immunization campaigns, but also in a significant increase in the level of penicillin non-susceptibility [46]–[48]. ST-8CC isolates, which predominated among Polish MenC between 2003 and 2004, were almost universally susceptible to penicillin and in later years were responsible for no more than one or two cases annually ([49], unpublished NRCBM data). Such a decline, following its previous predominance, was also noted in Italy [50]. On the other hand, isolates of ST-103CC were the most common amongst MenC in Poland in 2005 and then from 2008 onwards (unpublished NRCBM data). In our study these isolates constituted 42% of all MenC. To begin with, the ST-103CC group was very homogenous and was composed exclusively of ST-5133 isolates with the same PorA and FetA profile. However, this group has diversified over time, with single and double locus variants of ST-5133 isolates not belonging to ST-103CC subsequently occurring. Interestingly, representatives of this clonal complex, although of different sequence types, were often responsible for infections and occasionally for IMD outbreaks in Brazil [51], [52].
In our study, the third most common clonal complex of MenC was the hyper-virulent ST-11 CC, which between 2006 and 2007 predominated among MenC in Poland and additionally in the years from 2006 to 2009 were responsible for numerous outbreaks. Infections with ST-11 meningococci, as also described by others, most commonly present as sepsis, affect mostly adolescents and young adults, are generally associated with a high CFR and have been responsible for numerous epidemics and outbreaks in different parts of the world [39], [53]–[57]. Similar to ST-103CC, ST-11CC in this study was also very homogenous by MLST analysis and was composed mainly of ST-11 isolates. However, during the study period, both PorA and FetA variants of ST-11 isolates appeared, which may partially explain the increase in sporadic cases as well as the occurrence of outbreaks in Poland. It has been suggested that even very small alterations in antigenic characteristics, which can be the result of a single point mutation, may result in an increase in the number of IMD cases in particular geographic areas [19], [55], [58].
The results of our study showed that the detection of IMD in Poland has changed over time, but observed increase in the incidence of the disease was mostly attributed to changes in the surveillance system, including an expanded case definition and the inclusion of data from non-culture diagnostics. Even though IMD is a rare disease in our country, the severity of the disease itself and the occurrence of outbreaks have resulted in a certain fear among the general public. To control IMD in Poland, where mass vaccination against the disease has yet to be introduced, inclusion of vaccines against MenC and MenB into the childhood immunization schedule should be considered.
Acknowledgments
We thank all BINet participants and all other physicians and microbiologists who participated in the national surveillance programme of invasive meningococcal diseases in Poland, providing isolates and data. Participants of a laboratory-based surveillance of community acquired invasive bacterial infections (BINet) who positively responded for a co-authorship proposition: Anna Bucka, Central Laboratory, County Hospital in Wadowice, Wadowice, Poland; Anna Budzyńska, Laboratory Diagnostics Department, Independent Public Medical Establishment in Lębork, Lębork, Poland; Krzysztof Burdynowski, Department of Microbiology, Regional Medical Centre in Opole, Opole, Poland; Mariola Cichoń, Bacteriological Laboratory, Voivodeship Hospital in Bielsko-Biała, Bielsko-Biała, Poland; Ewa Czekalska-Lachowicz, Molecular Diagnostics Laboratory, Hospital of Infectious Diseases, Warsaw, Poland; Małgorzata Dorycka, Department of Microbiology, DIAGNOSTYKA Sp. z o.o., Cracow, Poland; Małgorzata Drozdowska, Laboratory of Microbiology I, Voivodeship Polyclinic Hospital of L. Rydygier in Toruń, Toruń, Poland; Maria Drzewicka, Microbiological Laboratory of Central Laboratory, Pediatric Hospital, Bielsko-Biała, Poland; Urszula Gajda, Analytical Laboratory of the Laboratory of Bacteriology, Independent Public Health Care in Puławy, Puławy, Poland; Sylwia Gotlibowska, Medical Laboratory Synevo Zielona Góra, Zielona Góra, Poland; Marzena Grab, Department of Microbiology, Polish Mother’s Memorial Hospital Research Institute, Łódź, Poland; Elżbieta Grodecka, Medical Microbiology Laboratory, Specialized Hospital of H. Klimontowicz in Gorlice, Gorlice, Poland; Aneta Guzek, Departament of Medicial Diagnostics, Military Institute of Medicine, Warsaw, Poland; Jadwiga Heffner, Clinical Laboratory, Opole Province Epidemical and Sanitary Center, Opole, Poland; Zofia Hetkowska-Abramczyk, Microbiology Laboratory, The John Paul’s II Western Hospital, Grodzisk Mazowiecki, Poland; Ewa Hołownia-Puczel, Department of Laboratory Diagnostics, Independent Public Health Care Centre of the Ministry of the Internal Affairs of Warmia and Mazury with Centre of Oncology in Olsztyn, Olsztyn, Poland; Joanna Humanowska, Laboratory of Microbiology, Maritime Hospital in Gdynia, Gdynia, Poland; Jadwiga Jaworowska, Department of Microbiological Diagnostics and Infectious Immunology, Medical University of Białystok Clinical Hospital, Białystok, Poland; Anna Jędrzejewska, Department of Bacteriology, Marcin Kacprzak Regional Hospital, Płock, Poland; Bożena Jeż, Department of Laboratory, Holy Spirit Specialist Hospital in Sandomierz, Sandomierz, Poland; Małgorzata Juszczyk-Grudzińska, Laboratory of Microbiology, Public Hospital “Latawiec” in Świdnica, Świdnica, Poland; Joanna Kaczyńska, Laboratory of Microbiological Diagnostic, Specialised Hospital with Outpatient Clinic in Elbląg, Elbląg, Poland; Jolanta Kędzierska, Department of Microbiology, University Hospital in Cracow, Cracow, Poland; Beata Klonowska, Microbiological Laboratory, Voivodeship Hospital Center of Kotlina Jeleniogórska, Jelenia Góra, Poland; Hanna Kołakowska, Laboratory Bacteriology, Independent Public Health Care Team, Wyszków, Poland; Ewelina Konefal, Department of Microbiological Diagnostics, L. Rydygier Regional Hospital of in Toruń, Toruń, Poland; Anna Koperska, Department of Bacteriology, Regional Hospital of Nicholas Copernicus, Koszalin, Poland; Jolanta Kostuń, Laboratory of Microbiology II, Voivodeship Polyclinic Hospital of L. Rydygier in Toruń, Toruń, Poland; Małgorzata Kozak, Department of Clinical Microbiology, Multidisciplinary Hospital of Ludwik Błażek in Inowrocław, Inowrocław, Poland; Paweł Kozak, Laboratory of Microbiology, Independent Public Regional Hospital of Jan Boży Memorial, Lublin, Poland; Anna Kozieł, Department of Laboratory Diagnostics, Fryderyk Chopin Provincial Specialist Hospital, Rzeszów, Poland; Dorota Kozłowska, Brest Medical Center, Independent Public Health Care in Brzeg, Brzeg, Poland; Dorota Krawiecka, Department of Microbiology, Regional Centre of Pulmonology in Bydgoszcz, Bydgoszcz, Poland; Grażyna Kwarciak, Microbiological Laboratory, John Paul II Hospital, Cracow, Poland; Elżbieta Maćkowiak, Department of Clinical Microbiology, Regional Specialist Hospital, Częstochowa, Poland; Anita Mądroszyk, Department of Clinical Microbiology, Voivodeship Hospital in Konin, Konin, Poland; Elżbieta Majda, Bacteriological Laboratory, NZOZ hospital, Kutno, Poland; Helena Majewska, Institute of Bacteriology, Hospital of St. John, Starogard Gdański, Poland; Urszula Mamorska, Department of Laboratory Diagnostics, Regional Hospital, Leszno, Poland; Anna Mazur, Laboratory of Bacteriology, ZOZ in Szczytno, Szczytno, Poland; Anna Meller, Microbiology Laboratory, Central Hospital of the Ministry of Internal Affairs, Warsaw, Poland; Grzegorz Michalak, Emergency Department, Bielański Hospital, Warsaw, Poland; Danuta Michałek-Aniko, Microbiological Diagnostics Department, The Independent Public Group of Health Departments in Gryfice, Gryfice, Poland; Zofia Mikołajczyk, Microbiological Laboratory, District Hospital in Mielec, Mielec, Poland; Agnieszka Mikucka, Department of Microbiology, Ludwik Rydygier Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University, Bydgoszcz, Poland; Katarzyna Ochmanek, NZOZ Diaklin Laboratory, Hospital in Cieszyn, Cieszyn, Poland; Anna Ochmańska, Microbiological Laboratory, Department of Health Care in Oświęcim, Oświęcim, Poland; Hanna Ogrodniczuk, Medical Laboratory Synevo, Lublin, Poland; Justyna Pałuba, Laboratory of Bacteriology, CMKP Independent Public Central Clinical Hospital of Prof. W. Orłowski, Warsaw, Poland; Marzena Paprzycka, Microbiological Diagnostics Hospital Laboratory, University Hospital No. 2 in Bydgoszcz, Bydgoszcz, Poland; Danuta Pawlik, Microbiology Laboratory, Independent Public Healthcare Centre, Maków Mazowiecki, Poland; Małgorzata Pilarska, Medical Diagnostic Laboratory and Microbiology, Dr Ludwik Rydygier Voivodeship Hospital in Suwałki, Suwałki, Poland; Mirosława Piotrowska, Molecular Diagnostics Laboratory, Wł. Buszkowski Kielce Province Children’s Hospital, Kielce, Poland; Jaroslaw Piszczyk, Laboratory, Nikolaus Copernicus Autonomous Voivodeship Hospital in Piotrków Trybunalski, Piotrków Trybunalski, Poland; Monika Pomorska-Wesołowska, Analytical and Microbiological Laboratory of Ruda Śląska, KORLAB NZOZ, Ruda Śląska, Poland; Magdalena Popielarz, Microbiological Laboratory, Hospital in Radziejów, Radziejów, Poland; Ryszard Prosiecki, Department of Microbiology, SP ZOZ, Sanok, Poland; Ewa Rapacz, Laboratory of Microbiology, Independent Public Medical Care Team in Kościan, Kościan, Poland; Tomasz Romanowski, Laboratory of Bacteriology, Provincial Integrated Hospital in Elbląg, Elbląg, Poland; Paweł Sacha, Department of Microbiological Diagnostics, Medical University of Białystok, Białystok, Poland; Anna Schneider, Department of Microbiology, University Hospital of Lord’s Transfiguration in Poznań, University of Medical Sciences, Poznań, Poland; Maria Skok, Laboratory of Microbiology, Specialized Hospital in Jasło, Jasło, Poland; Wioletta Stawska-Drzymała, Microbiology Laboratory, Voivodeship Hospital, Bełchatów, Poland; Beata Stempkowska-Podkowińska, Medical Diagnostic Laboratory, 111st Military Hospital in Poznań, Poznań, Poland; Marta Sudak, Department of Laboratory Diagnostics, Medical Center in Łańcut, Łańcut, Poland; Barbara Symula, Laboratory of Bacteriology, Independent Public Health Care in Oława, Oława, Poland; Anna Szkarłat, Department of Clinical Microbiology, University Children’s Hospital of Cracow, Cracow, Poland; Hanna Szwajkert Sobiecka, Department of Microbiology, Nicolaus Copernicus Specialist Municipal Hospital in Toruń, Toruń, Poland; Maria Szymankiewicz, Department of Microbiology, Oncology Centre of Prof. Franciszek Łukaszczyk memorial, Bydgoszcz, Poland; Elżbieta Szymańska, Microbiology Laboratory, Independent Public Health Care Institution in Krotoszyn, Krotoszyn, Poland; Grażyna Śliwa, Microbiological Laboratory, Provincial Hospital in Tarnobrzeg, Tarnobrzeg, Poland; Ewa Śpiewak, Department of Microbiology, Polish Mother’s Memorial Hospital Research Institute, Łódź, Poland; Izabela Trendota-Horniak, Department of Microbiology, The St. Lukas District Hospital in Tarnów, Tarnów, Poland; Agnieszka Urbanowicz, Microbiological Laboratory, “ASPER” Diagnostic Center, Tychy, Poland; Beata Walaszkowska, Microbiological Laboratory, Public Hospital SPS ZOZ “ZDROJE”, Szczecin, Poland; Grażyna Woch, Department of Laboratory Diagnostics, Military Teaching Hospital-Veterans Central Hospital in Łódź, Łódź, Poland; Ilona Wojak, Microbiology Laboratory, Voivodeship Children’s Hospital in Bydgoszcz, Bydgoszcz, Poland; Lidia Wójcik, Microbiological Laboratory, Regional Hospital in Opole, Opole, Poland; Małgorzata Wróblewska, Microbiological Laboratory, Dr Władyslaw Biegański Regional Hospital in Grudziądz, Grudziądz, Poland; Zofia Żak-Puławska, Bacteriology, Hospital in Wołomin, Wołomin, Poland; Jolanta Zawiasa, Laboratory of Bacteriology, Voivodeship Hospital, Skierniewice, Poland; Grzegorz Ziółkowski, Department of Clinical Microbiology, Voivodeship Specialist Hospital in Sosnowiec, Sosnowiec, Poland; Wojciech Żulikowski, Department of Microbiology Diagnostics, Regional Hospital in Łomża, Łomża, Poland.
The authors would like to thank Stephen Murchan for critical reading of the manuscript and English language editing, and Anna Klarowicz for her excellent technical assistance. This publication made use of the Neisseria Multi-Locus Sequence Typing website (http://pubmlst.org/neisseria/) developed by Keith Jolley and sited at the University of Oxford (Jolley & Maiden 2010, BMC Bioinformatics, 11∶595). The development of this site has been funded by the Wellcome Trust and European Union.
Funding Statement
The study was partially supported by the Ministry of Health within the framework of the Modul I of the National Programme of Antibiotic Protection (NPOA), by the Ministry of Science and Higher Education (Mikrobank 2 Programme), and by an unrestricted grant from Glaxo SmithKline (114538). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Stephens DS (2007) Conquering the meningococcus. FEMS Microbiol Rev 31: 3–14. [DOI] [PubMed] [Google Scholar]
- 2. Khatami A, Pollard AJ (2010) The epidemiology of meningococcal disease and the impact of vaccines. Expert Rev Vaccines 9: 285–298. [DOI] [PubMed] [Google Scholar]
- 3. Cohn AC, MacNeil JR, Harrison LH, Hatcher C, Theodore J, et al. (2010) Changes in Neisseria meningitidis disease epidemiology in the United States, 1998–2007: implications for prevention of meningococcal disease. Clin Infect Dis 50: 184–191. [DOI] [PubMed] [Google Scholar]
- 4. Healy CM, Butler KM, Smith EO, Hensey OP, Bate T, et al. (2002) Influence of serogroup on the presentation, course, and outcome of invasive meningococcal disease in children in the Republic of Ireland, 1995–2000. Clin Infect Dis 34: 1323–1330. [DOI] [PubMed] [Google Scholar]
- 5. Skoczynska A, Kadlubowski M, Knap J, Szulc M, Janusz-Jurczyk M, et al. (2006) Invasive meningococcal disease associated with very high case fatality rate in the North-West of Poland. FEMS Immunol Med Microbiol 46: 230–235. [DOI] [PubMed] [Google Scholar]
- 6.Pollard AJ, Nadel S. (2006) Course of disease and clinical management. In: Frosh M, Maiden MCJ, editors. Handbook of Meningococcal Disease. Weinheim: Wiley-VCH. Pp. 481–517.
- 7. Edwards MS, Baker CJ (1981) Complications and sequelae of meningococcal infections in children. Journal Pediatr 99: 540–545. [DOI] [PubMed] [Google Scholar]
- 8. Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM (2001) Meningococcal disease. New Engl J Med 344: 1378–1388. [DOI] [PubMed] [Google Scholar]
- 9. Harrison LH, Pass MA, Mendelsohn AB, Egri M, Rosenstein NE, et al. (2001) Invasive meningococcal disease in adolescents and young adults. JAMA 286: 694–699. [DOI] [PubMed] [Google Scholar]
- 10. Harrison LH, Trotter CL, Ramsay ME (2009) Global epidemiology of meningococcal disease. Vaccine 27 supp. 2B51–B63. [DOI] [PubMed] [Google Scholar]
- 11.The European Commission of the European Communities, European Union website (2000) Commission decision of 22 December 1999 on the communicable diseases to be progressively covered by the community network under decision number 2119/98/EC of the Parliament and of the Council. Official J Eur Communities L28/50. Available: http://europa.eu.int/eur-lex/pri/en/oj/d?at/2000/l_028/l_02820000203en00500053.pdf. Accessed 2013 May 24.
- 12.The European Parliament, the Council of the EU, European Union website (1998) Decision number 2119/98/EC of the European Parliament and of the Council of 24 September 1998: setting up a network for the epidemiological surveillance and control of communicable diseases in the community: Official J Eur Communities L268/1. Available: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:31998D2119:EN:NOT. Accessed 2013 May 24.
- 13. Guiver M, Borrow R, Marsh J, Gray SJ, Kaczmarski EB, et al. (2000) Evaluation of the Applied Biosystems automated Taqman polymerase chain reaction system for the detection of meningococcal DNA. FEMS Immunol Med Microbiol 28: 173–179. [DOI] [PubMed] [Google Scholar]
- 14. Taha MK (2000) Simultaneous approach for nonculture PCR-based identification and serogroup prediction of Neisseria meningitidis . J Clin Microbiol 38: 855–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clinical and Laboratory Standards Institute (2011) Performance standards for antimicrobial susceptibility testing; Twenty-first informational supplement; Wayne, PA M100-S21.
- 16.The European Committee on Antimicrobial Susceptibility Testing (2013) Breakpoint tables for interpretation of MICs and zone diameters. Version 3.1, 2013. http://www.eucast.org.
- 17. Maiden MC, Bygraves JA, Feil E, Morelli G, Russell JE, et al. (1998) Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci U S A 95: 3140–3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jolley KA, Brehony C, Maiden MC (2007) Molecular typing of meningococci: recommendations for target choice and nomenclature. FEMS Microbiol Rev 31: 89–96. [DOI] [PubMed] [Google Scholar]
- 19.Skoczyńska A, Wasko I, Kuch A, Gołębiewska A, Foryś M, et al. (2010) Outbreak of invasive meningococcal disease in Goleniów County, north-west Poland, March 2009. Euro Surveill 15(34): pii = 19646. Available: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19646. Accessed 2013 May 24. [PubMed]
- 20.Kadłubowski M, Waśko I, Klarowicz A, Hryniewicz W (2007) Invasive meningococcal disease at a military base in Warsaw, January 2007. Euro Surveill 12: pii = 3147. Available: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3147. Accessed 2013 April 24. [DOI] [PubMed]
- 21. Posmyk U, Hryniewicz W, Skoczyńska A, Kumala R (2012) Invasive meningococcal disease in Opolskie Voivodeship between 2005–2010. Polski Merkuriusz Lekarski 32: 287–292. [PubMed] [Google Scholar]
- 22.Grecki M, Bienias M (2006) Outbreak of invasive meningococcal disease among soldiers in Skwierzyna, Poland, March 2006. Euro Surveill 2006;11(7): E060706.4. Available from: http://www.eurosurveillance.org/ew/2006/060706.asp#4. Accessed 2013 April 24. [DOI] [PubMed]
- 23. Vogel U, Claus H (2003) Molecular epidemiology of Neisseria meningitidis . Front Biosci 8: 14–22. [DOI] [PubMed] [Google Scholar]
- 24.Gryniewicz O, Kolbusz J, Rosinska M, Zielinski A, Stefanoff P (2007) Epidemiology of meningococcal meningitis and changes in the surveillance system in Poland, 1970–2006. Euro Surveill 12(5). Available: http://www. eurosurveillance.org/em/v12n05/1205–224.asp. Accessed 2013 April 24. [DOI] [PubMed]
- 25. Kaczmarski EB, Ragunathan PL, Marsh J, Gray SJ, Guiver M (1998) Creating a national service for the diagnosis of meningococcal disease by polymerase chain reaction. Commun Dis Public Health 1: 54–56. [PubMed] [Google Scholar]
- 26. Papavasileiou K, Papavasileiou E, Tzanakaki G, Voyatzi A, Kremastinou J, et al. (2011) Acute bacterial meningitis cases diagnosed by culture and PCR in a children’s hospital throughout a 9-Year period (2000–2008) in Athens, Greece. Mol Diagn Ther 15: 109–13. [DOI] [PubMed] [Google Scholar]
- 27. Skoczyńska A, Sadowy E, Bojarska K, Strzelecki J, Kuch A, et al. (2011) The current status of invasive pneumococcal disease in Poland. Vaccine 29: 2199–2205. [DOI] [PubMed] [Google Scholar]
- 28. Skoczyńska A, Hryniewicz W, Ronkiewicz P, Kuch A (2012) BINet – surveillance network for community-acquired invasive bacterial infections (in Polish). Standardy Medyczne/Pediatria 9: 389–395. [Google Scholar]
- 29.European Centre for Disease Prevention and Control (2011) Annual Epidemiological Report 2011. Reporting on 2009 surveillance data and 2010 epidemic intelligence data. Stockholm: ECDC: 155–157.
- 30. Skoczyńska A, Kuch A, Waśko I, Gołębiewska A, Ronkiewicz P, et al. (2012) Invasive meningococcal disease in patients under 20 years of age in Poland, 2009–2011. Pediatria Polska 87: 438–443. [Google Scholar]
- 31. Konior R, Jackowska T, Skoczyńska A, Hryniewicz W, Kajfasz P, et al. (2012) Vaccination against meningococci – current recommendations and suggestions (in Polish). Pediatria Polska 87: 489–497. [Google Scholar]
- 32. Kriz P, Wieffer H, Holl K, Rosenlund M, Budhia S, et al. (2011) Changing epidemiology of meningococcal disease in Europe from the mid-20th to the early 21st Century. Expert Rev Vaccines 10: 1477–1486. [DOI] [PubMed] [Google Scholar]
- 33.Racloz VN, Luiz SJD (2010) The elusive meningococcal meningitis serogroup: a systematic review of serogroup B epidemiology. BMC Infect Dis 10: 175. Available: http://www.biomedcentral.com/1471-2334/10/175. Accessed 2013 April 24. [DOI] [PMC free article] [PubMed]
- 34. Trotter CL, Chandra M, Cano R, Larrauri A, Ramsay ME, et al. (2007) A surveillance network for meningococcal disease in Europe. FEMS Microbiol Rev 31: 27–36. [DOI] [PubMed] [Google Scholar]
- 35.EU-IBIS Network (2006) Invasive Neisseria meningitidis in Europe 2006. Health Protection Agency, London. Available: http://www.hpa-bioinformatics.org.uk/euibis/documents/2006_meningo.pdf. Accessed 2013 April 24.
- 36. Rosenstein NE, Perkins BA, Stephens DS, Lefkowitz L, Cartter ML, et al. (1999) The changing epidemiology of meningococcal disease in the United States, 1992–1996. J Infect Dis 180: 1894–1901. [DOI] [PubMed] [Google Scholar]
- 37. Ladhani SN, Lucidarme J, Newbold LS, Gray SJ, Carr AD, et al. (2012) Invasive meningococcal capsular group Y disease, England and Wales, 2007–2009. Emerg Infect Dis 18: 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bröker M, Jacobsson S, Kuusi M, Pace D, Simões MJ, et al. (2012) Meningococcal serogroup Y emergence in Europe: Update 2011. Hum Vaccin Immunother 8: 1907–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Trotter CL, Fox AJ, Ramsay ME, Sadler F, Gray SJ, et al. (2002) Fatal outcome from meningococcal disease - an association with meningococcal phenotype but not with reduced susceptibility to benzylpenicillin. J Med Microbiol 51: 855–860. [DOI] [PubMed] [Google Scholar]
- 40. Skoczyńska A, Kriz P, Konradsen H, Hryniewicz W (2000) Characteristics of the major etiologic agents of bacterial meningitis isolated in Poland in 1997–98. Microb Drug Resist 2: 147–153. [DOI] [PubMed] [Google Scholar]
- 41. Taha MK, Vazquez JA, Hong E, Bennett DE, Bertrand S, et al. (2007) Target gene sequencing to characterize penicillin G susceptibility of Neisseria meningitidis . Antimicrob Agents Chemother 51: 2784–2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Taha MK, Thulin Hedberg S, Szatanik M, Hong E, Ruckly C, et al. (2010) Multicenter study for defining the breakpoint for rifampin resistance in Neisseria meningitidis by rpoB sequencing. Antimicrob Agents Chemother 54: 3651–3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Caugant DA, Froholm LO, Bovre K, Holten E, Frasch CE, et al. (1986) Intercontinental spread of a genetically distinctive complex of clones of Neisseria meningitidis causing epidemic disease. Proc Natl Acad Sci USA 83: 4927–4931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Diermayer M, Hedberg K, Hoesly F, Fischer M, Perkins B, et al. (1999) Epidemic serogroup B meningococcal disease in Oregon: the evolving epidemiology of the ET-5 strain. JAMA 281: 1493–1497. [DOI] [PubMed] [Google Scholar]
- 45.Rouaud P, Perrocheau A, Taha MK, Sesboué C, Forgues AM, et al. (2006) Prolonged outbreak of B meningococcal disease in the Seine-Maritime department, France, January 2003 to June 2005. Euro Surveill 11: 178–181. Available: http://www.eurosurveillance.org/images/dynamic/EQ/v06n03/v06n03.pdf. Accessed 2013 April 24. [PubMed]
- 46. Alcalá B, Arreaza L, Salcedo C, Uría MJ, De La Fuente L, et al. (2002) Capsule switching among C:2b:P1.2,5 meningococcal epidemic strains after mass immunization campaign, Spain. Emerg Infect Dis 8: 1512–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Caniça M, Dias R, Ferreira E (2004) Meningococci Study Group (2004) Neisseria meningitidis C:2b:P1.2,5 with intermediate resistance to penicillin, Portugal. Emerg Infect Dis 10: 526–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Stefanelli P, Fazio C, Neri A, Tonino S, Mastrantonio P (2004) Emergence in Italy of a Neisseria meningitidis clone with decreased susceptibility to penicillin. Antimicrob Agents Chemother 48: 3103–3106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Skoczyńska A, Kadłubowski M, Wasko I, Hryniewicz W (2006) Characterisation of Neisseria meningitidis C:2b:P1.2,5 isolates in Poland. Clin Microbiol Infect 12: 1027–1030. [DOI] [PubMed] [Google Scholar]
- 50. Neri A, Fazio C, Carannante A, Mastrantonio P, Stefanelli P (2012) Diversity of Neisseria meningitidis invasive isolates in Italy in the period 2008–2010. J Prev Med Hyg 53: 109–112. [PubMed] [Google Scholar]
- 51. Iser BP, Lima HC, de Moraes C, de Almeida RP, Watanabe LT, et al. (2012) Outbreak of Neisseria meningitidis C in workers at a large food-processing plant in Brazil: challenges of controlling disease spread to the larger community. Epidemiol Infect 140: 906–915. [DOI] [PubMed] [Google Scholar]
- 52. de Lemos AP, Yara TY, Gorla MC, de Paiva MV, de Souza AL, et al. (2007) Clonal distribution of invasive Neisseria meningitidis serogroup C strains circulating from 1976 to 2005 in greater Sao Paulo, Brazil. J Clin Microbiol 45: 1266–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Whalen CM, Hockin JC, Ryan A, Ashton F (1995) The changing epidemiology of invasive meningococcal disease in Canada, 1985 through 1992. Emergence of a virulent clone of Neisseria meningitidis . JAMA 273: 390–394. [PubMed] [Google Scholar]
- 54. Jelfs J, Munro R, Ashton FE, Caugant DA (2000) Genetic characterization of a new variant within the ET-37 complex of Neisseria meningitidis associated with outbreaks in various parts of the world. Epidemiol Infect 125: 285–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Harrison LH, Jolley KA, Shutt KA, Marsh JW, O’Leary M, et al. (2006) Antigenic shift and increased incidence of meningococcal disease. J Infect Dis 193: 1266–1274. [DOI] [PubMed] [Google Scholar]
- 56. Krizova P, Musilek M (1995) Changing epidemiology of meningococcal invasive disease in the Czech republic caused by new clone Neisseria meningitidis C:2a:P1.2(P1.5), ET-15/37. Cent Eur J Public Health 3: 189–194. [PubMed] [Google Scholar]
- 57. Tyrrell GJ, Chui L, Johnson M, Chang N, Rennie RP, et al. (2002) Outbreak of Neisseria meningitidis, Edmonton, Alberta, Canada. Emerg Infect Dis 8: 519–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. McGuinness BT, Clarke IN, Lambden PR, Barlow AK, Poolman JT, et al. (1991) Point mutation in meningococcal por A gene associated with increased endemic disease. Lancet 337: 514–517. [DOI] [PubMed] [Google Scholar]