Abstract
Pharmacy education programs in Vietnam are complex and offer various career pathways. All include theory and laboratory modules in general, foundation, and pharmaceutical knowledge; placements in health facilities; and a final examination. The various pharmacy degree programs allow specialization in 1 or more of 5 main fields: (1) drug management and supply, (2) drug development and production, (3) pharmacology and clinical pharmacy, (4) traditional medicine and pharmacognosy, and (5) drug quality control, which are offered as main specialization options during the reformed undergraduate and postgraduate programs. However, pharmacy education in Vietnam in general remains product oriented and clinical pharmacy training has not received adequate attention. Only students who have obtained the bachelor of pharmacy degree, which requires a minimum of 5 years of study, are considered as fully qualified pharmacists. In contrast, an elementary diploma in pharmacy awarded after 1 year of pharmacy study permits entry into more junior pharmacy positions. Since the 2000s, there has been a surge in the number and types of schools offering pharmacy qualifications at various levels.
Keywords: pharmacy education, pharmacy practice, Vietnam
INTRODUCTION
While pharmacy education in Vietnam, a country in Southeast Asia with a population of 88 million,1 has undergone many changes since the first faculty of pharmacy was established in 1914,2 it has witnessed the most profound developments during the last 3 decades. Since the mid-1980s, because of rapid industrialization in the pharmaceutical sector, privatization in the retail sector, and economic growth, there has been an increase in demand for qualified pharmacy personnel. Newly established pharmacy schools and degree programs have provided more opportunities for students wishing to pursue a career in pharmacy. There are a variety of pharmacy qualifications offered. This article describes Vietnamese pharmacy education programs, including criteria for admission, the type and length of training, and an overview of the curricula; and outlines the system of pharmacy schools. The career opportunities for pharmacy graduates, educational barriers, and recent and future directions in pharmacy education are also discussed.
PHARMACY EDUCATION PROGRAMS
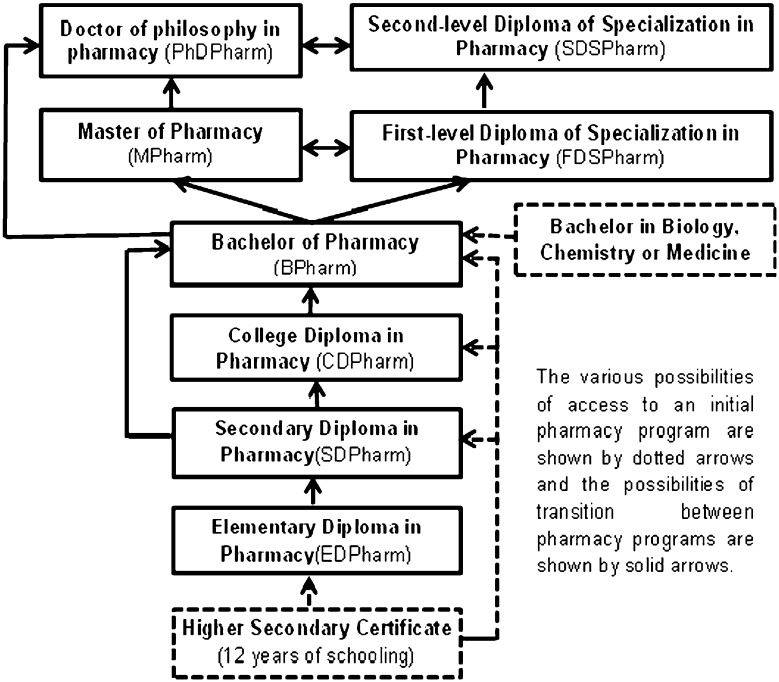
Compared to France,3 the United Kingdom,4 and the United States, the variety of pharmacy qualifications in Vietnam is more heterogeneous. Various flexible training programs have been developed to meet the diverse learning needs of prospective students. A range of pharmacy qualifications are offered (Figure 1) including: elementary diploma in pharmacy (EDPharm), secondary diploma in pharmacy (SDPharm), college diploma in pharmacy (CDPharm), bachelor of pharmacy (BPharm), master of pharmacy (MPharm), doctor of philosophy in pharmacy (PhDPharm), first-level diploma of specialization in pharmacy (FDSPharm), and the second-level diploma of specialization in pharmacy (SDSPharm).
Figure 1.
System of Vietnamese pharmacy degrees.
After 12 years of formal education, high school graduates wishing to pursue a career in pharmacy can choose between courses leading to 1 of the 4 first-level qualifications: EDPharm (1 year), SDPharm (2 years), CDPharm (3 years), or BPharm (5 years), depending on their academic achievement, references, and motivation. After completing a first-level pharmacy program, students can enter the workforce or follow a higher-level course (Figure 1). Pharmacy programs vary in length depending on the preexisting pharmacy training of the candidate (Table 1). For example, a high school graduate can choose to enroll directly in the 5-year BPharm program or complete a 2-year SDPharm program followed by the 4-year BPharm program. Students holding a bachelor’s degree in biology, chemistry, or medicine can apply for the 3-year BPharm program.
Table 1.
Characteristics of Vietnamese Pharmacy Education Programs
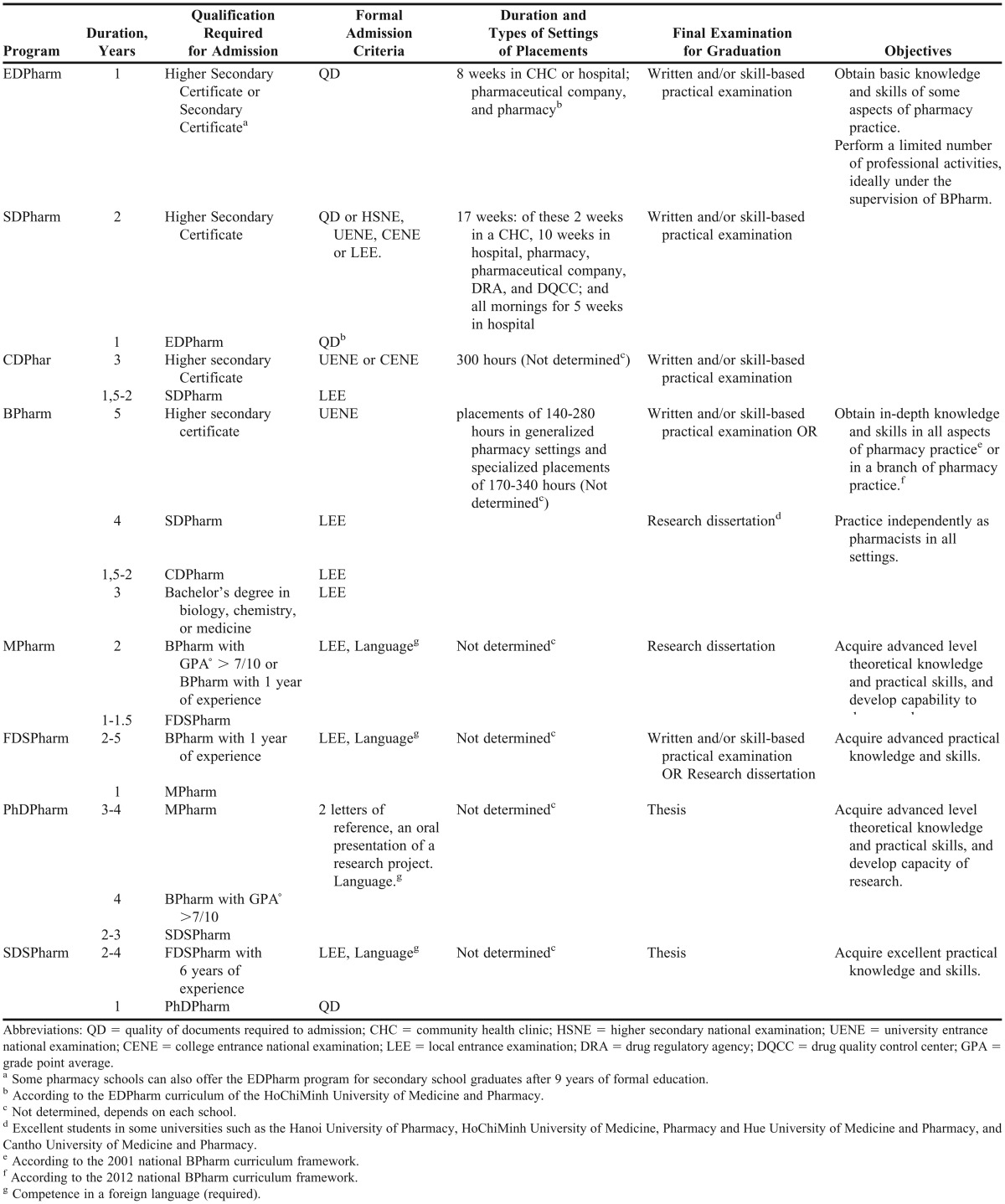
There are 2 parallel postgraduate programs: the new master’s-doctorate system, similar to that in Europe, and the traditional Vietnamese diploma of specialization. The most significant difference between them is that the master’s-doctorate degree program aims to enhance academic knowledge and research competence, while the specialization programs focus on practical knowledge and skills. Therefore, there is a trend for pharmacists in research institutions and universities to follow the former option. In 2002 the Ministry of Health issued rules regarding transferable accreditation between the 2 degree systems.5 Thus, a MPharm or a PhDPharm graduate can transfer to the FDSPharm or SDSPharm program, respectively, and vice versa. If a student wants to transfer, they have to apply for the desired program; if accepted, the committee of each school considers the previous courses followed by the candidate so as to exempt him/her from some modules. However, few students have pursued these pathways because of the complexity of the transfer process.6,7 In practice, there is not much distinction in requirements between the 2 postgraduate diplomas except in universities and research institutes where the MPharm and PhD Pharm are preferred.
Admission Criteria
In Vietnam, there are many mechanisms for admission to pharmacy school. The dominant one is a formal application, based on an entrance examination and sometimes the academic achievement of the student. Table 1 summarizes the formal admission criteria for entry into pharmacy programs. Other mechanisms include (1) the direct recruitment of candidates from ethnic groups after they have followed a preparatory course, or of high school students who have obtained a national or international award in chemistry, etc; and (2) lower admission criteria (extra points added to the candidate’s entrance score) for specific groups, eg, applicants contracted by local autorities (after graduation students are then obliged to work in the locality in which they were recruited), students from remote areas, etc. Nevertheless, the candidate’s entrance score must be above a cut-off point established annually by the Ministry of Education and Training.8 In general, admission criteria differ between programs and between candidates from different backgrounds, and depend essentially on the individual pharmacy school.
After 12 years of formal education, high school students must pass the National Higher Secondary Examination and obtain a Higher Secondary Certificate. After that, depending on the pharmacy school for which they want to apply, there are 3 alternative examinations: the National University-Entrance Examination, the National College-Entrance Examination administered by the Ministry of Education and Training; or a Local Entrance Examination organized by some individual schools. Admission to a first-level pharmacy program depends on the candidate’s scores on these examinations or grades on high school continuous assessments. After graduating from a first-level pharmacy program, students wishing to pursue a higher-level pharmacy program have to sit for/complete a competitive entrance examination organized by the individual pharmacy schools. However, admission to the SDPharm program depends on grades obtained in the EDPharm program and entry to the PhDPharm program is based on the candidate’s research project, 2 references, and an oral presentation in front of a scientific committee.9 In general, competence in a foreign language is required for access to all postgraduate programs.
The pharmacy schools determine quotas for student admissions depending on the need for healthcare manpower, the capacity of the school, and the criteria of education quality assurance. The 2 main criteria include the teacher/student ratio and the space/student ratio (eg, the teacher/student ratio is 20 for the SDPharm, 15 for CDPharm, and 10 for BPharm, and the space/student is 2m2/student).10 The quota and the numbers of students applying vary across universities. For instance in 2011, 2,500 students applied for 550 BPharm places (ratio 5:1) at Hanoi University of Pharmacy (HUP), while 6,488 students competed for 300 places (ratio 22:1) at HoChiMinh University of Medicine and Pharmacy (HCMUMP).
Curriculum
Pharmacy programs in Vietnamese pharmacy schools are based on national curriculum frameworks outlined by the Ministry of Education and Training and/or Ministry of Health in terms of main contents, the proportion of theoretical and practical sessions, and the number of credits per module. All national curricula are designed by a national committee of experts in the field of medical and pharmaceutical education, practice, and management.
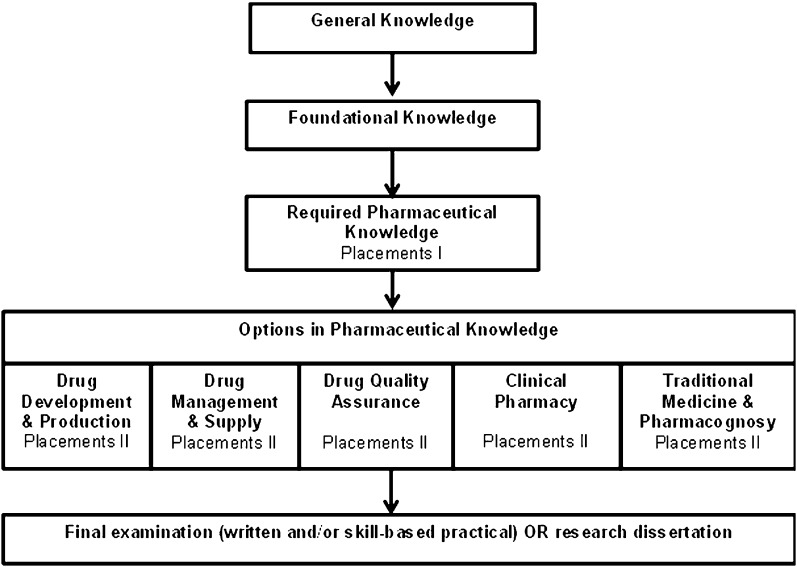
The structure of pharmacy programs includes modules (theory and laboratory), a series of placements in a variety of health facilities, and a final examination for graduation (Figure 2). There are 3 types of modules: general knowledge, which includes philosophy, language and informatics, etc, which are common to all Vietnamese undergraduate programs; foundation knowledge, which includes modules such as botany, analytical chemistry, and basic medicine, etc, providing sufficient background knowledge for students to understand the pharmaceutical module; and pharmaceutical knowledge, which is composed of modules such as pharmacology, pharmaceutics and pharmaceutical management, etc.
Figure 2.
General structure of the 2012 National BPharm Curriculum.
For placements, undergraduate students generally spend 1-2 weeks in each of several different health settings (eg, community health center, hospital, pharmacy, pharmaceutical company, drug regulatory agency, drug quality control center, etc) with which the pharmacy school has established a partnership. Commonly, a school assigns a group of students to each setting and then rotates them every 1-2 weeks to another setting. The aim of placements is to enable students to become familiar with different professional environments, to get insight into their subsequent professional activities, and to perform some simple tasks in each setting. All students follow the same placements; except for students following the 2012 BPharm curriculum (see BPharm in Figure 2). Students are evaluated by report-based, oral, and/or skill-based assessments at the end of each placement, and/or at the end of a series of placements.
Finally, all students are required to (1) pass a final examination (written and/or skill-based practical), or (2) do a research project, write a dissertation, and present their work to a scientific committee in order to graduate. The duration and types of health settings for placements and the type of final examination for each program are summarized in Table 1.
The 1-year EDPharm program emphasizes basic knowledge and skills required to enable students to perform the simple tasks encountered in pharmacy practice such as drug dispensing, providing drug information, preparing simple solutions, and counseling patients regarding local herbal remedies. Most modules are highly pertinent to everyday pharmacy practice. For example, the typical EDPharm curriculum of the HCMUMP includes philosophy, basic medicine, writing and reading drug names, management of drug and medical devices, drug use, pharmacognosy, pharmaceutical management, pharmaceutics, and pharmaceutical law. Students have 32 weeks of classroom teaching and 8 weeks of placements.11
The national SDPharm curriculum framework was issued in 2003.12 In this 2-year course, pharmaceutical knowledge makes up about 60% of the total number of credits. Students spend 2 weeks in a community health clinic at the end of the first year and 1-2 weeks each in a pharmacy department of a hospital, a drug regulatory agency, a pharmaceutical company, and a drug quality control center over a 10-week period at the end of the second year. Also, for 5 weeks at the beginning of the second year, students spend the mornings in hospital clinical departments to observe the day-to-day therapeutic approach to treating major diseases.
The first national CDPharm curriculum framework was set up in 2010.13 Compared to the SDPharm, the CDPharm curriculum offers more modules in foundation knowledge and a selection of optional modules in pharmaceutical knowledge. The introduction of optional modules (23% of the total number of credits) in the CDPharm curriculum is aimed at giving the students an opportunity to explore their own professional interests. Pharmacy schools are free to design optional modules depending on their capacity; however, the 2 “optional” specialized fields suggested by the Ministry of Education and Training are (1) drug management and supply and (2) drug quality assurance.
In the last decade, all pharmacy faculties have been required to develop their own specific BPharm curriculum based on the 2001 National BPharm Curriculum Framework.14 This curriculum was designed with the aim of providing students with a broad education in all fields of pharmacy practice that would enable them to enter a diverse range of jobs. Therefore, all students followed virtually the same curriculum. However, this model proved ineffective and the demand for more specialized pharmacy training within the BPharm program was recognized by Vietnamese academic leaders. In 2012 a new national BPharm curriculum was issued in order to meet this demand (Table 2).15
Table 2.
Overview of the 2012 National BPharm Curriculum in Vietnam
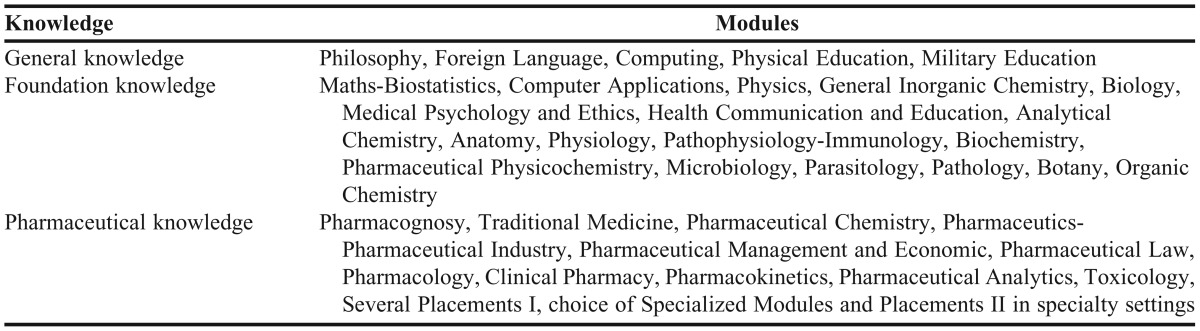
After finishing the general knowledge, foundation knowledge, and obligatory pharmaceutical knowledge modules, and following initial placements (140 to 280 hours) in several general pharmaceutical settings; students study 1 of 5 optional modules and complete longer, more specialized placements (170-340 hours) according to their professional interests. The 5 optional specialized fields suggested by the Ministry of Education and Training are (1) drug management and supply, (2) drug development and production, (3) clinical pharmacy, (4) traditional medicine – pharmacognosy, (5) drug quality assurance. Finally, while a few students with high academic performance in some universities have an opportunity to carry out a research project, write a dissertation, and present their work to a scientific committee, most students have to pass a final examination for graduation (Figure 2). The number of selected students, level of required academic performance, and kinds of research projects vary among pharmacy schools depending on the capacity of pharmacy educators, competence of students, etc. In general, a grade point average above 7-8/10 is required, and students can conduct a research project in any of the 5 core fields of pharmacy in the 2 largest pharmacy schools, the HUP and HCMUMP, while those in the Hue University of Medicine and Pharmacy have a more limited choice.
The modification of the BPharm curriculum is considered as a major breakthrough in pharmacy education. However, it will take time to see how pharmacy departments implement the new BPharm curriculum. The HUP is the only university that has initiated (in a pilot phase) the more specialized BPharm program. In the academic year 2011-2012, between 120 and 240 out of over 400 fourth-year students were offered more specialized pharmacy courses in pharmaceutics, clinical pharmacy, or pharmacy economics, while the other students followed the old BPharm program.
The MPharm program requires an additional 2 years of study after obtaining a BPharm. In the first year, students study common fundamental modules (eg, research methods or biostatistics at the HUP16; or medical and pharmaceutical sociology, or pharmaceutical law at the HCMUMP17) In the second year, students follow specialized modules and conduct a research project in either: (1) the pharmaceutical industry and pharmaceutics, (2) pharmaceutical economics and management, (3) pharmacognosy and traditional medicine, (4) pharmacology and clinical pharmacy, (5) pharmaceutical analytics and toxicology, or (6) pharmaceutical and biological chemistry.16
The courses and opportunities for specialization of the FDSPharm program are similar to those of MPharm programs, but the purpose is more vocational. As a result, the training is predominately practical, with laboratory or fieldwork accounting for at least 50% of the whole program (in term of teaching method) and predominately specialized courses (in term of teaching content) accounting for at least 60% of the whole program.18
The minimum duration of PhDPharm study is 3 academic years after a MPharm degree (a total of 10 years of pharmacy study), which includes some time spent completing additional courses, but most time spent carrying out a research project. Those BPharm students transferring directly to PhDPharm programs are required to study supplementary courses from MPharm programs.9
Like the FDSPharm program, the SDSPharm program has a more practical focus. The structure of the programs, the number of credits, the distribution between theoretical and practical training, and the time allotted to optional specialized studies is similar to that of the FDSPharm program. Students pursuing the SDSPharm program have to undertake a research project before graduation.19
CLINICAL PHARMACY EDUCATION
The basic concepts of clinical pharmacy were introduced in Vietnam in 1990 through the project “The Rational Use of Drugs and Drug Information” organized by Curtin University in Australia and HUP.20 The pharmacy faculties began adapting their curricula to focus on the patient and on clinical practice. Many of these changes were introduced by faculty members returning from France, Australia, and The Netherlands, etc. The master’s and doctoral degree programs in pharmacology and clinical pharmacy that were started in 1998 and 2006, respectively, need to be expanded and improved. Government authorities, academics, and pharmacy professionals recognize that the development of clinical pharmacy is essential to improve the safety, effectiveness, and efficiency of drug therapy for patients. The 2011 National Survey on Clinical Pharmacy Services in Vietnamese Central and Provincial Hospitals, conducted by HUP and the World Health Organization, aiming to help the government authorities to issue policies and academics to improve the initial and continuing pharmacy programs of clinical pharmacy, found that nearly half of hospitals assigned pharmacists to work in clinical wards (47.4%), but often for only a limited amount of time. The number of pharmacy department staff members and pharmacists per 100 beds was 5.3 ± 1.9 and 1.4 ± 1.0, respectively. Of 137 clinical pharmacists responding, nearly 40% were not trained in clinical aspects of pharmacy at university and only 58% of them participated in continuing education courses.21 Entities promoting clinical pharmacy education include (1) the 2007-2012 project “Strengthening the training quality of clinical pharmacists in Vietnam” in which 6 Vietnamese schools of pharmacy collaborated with Dutch, Thai, and Indonesian institutions to introduce clinical pharmacy as a specialization into existing pharmacy programs22; (2) the Ministry of Education and Training issued the 2012 BPharm curriculum reform which will require the pharmacy school to increase the proportion of clinical components and offer the a specialization in clinical pharmacy 15; and (3) Ministry of Health issued regulations defining the role and duties of clinical pharmacists in 201123 and guidelines for clinical pharmacy practice in health care facilities (drafting) which create the demand of well-trained clinical pharmacists.24 These driving forces aim to bring the benefits of clinical pharmacy practice to a large part of Vietnamese society.
SYSTEM OF PHARMACY SCHOOLS
Vietnamese pharmacy schools include technical high schools, colleges, and universities. The technical high schools can train EDPharm and SDPharm, and colleges can offer the CDPharm and lower-level programs, but only universities can award the BPharm and postgraduate degrees.
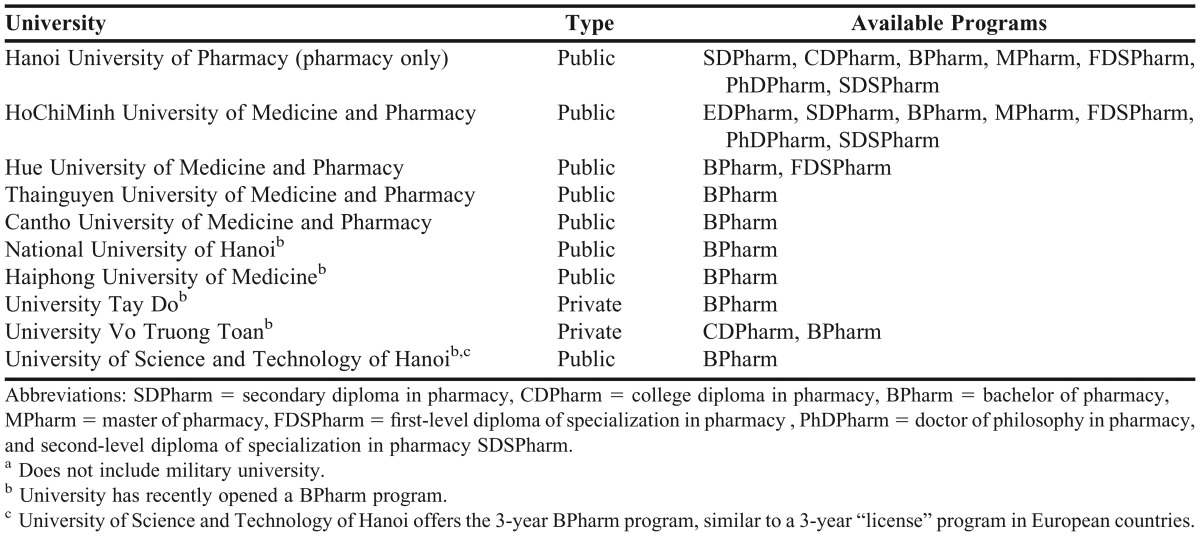
According to the 2012 Global Pharmacy Workforce Report, the number of pharmacists per 10,000 people in Vietnam is lower than in 50 of 82 countries.25 In 2006, the Ministry of Health set a target to double the number of pharmacists by 2020 (from 1.2 pharmacists per 10,000 people in 2006 to 2 to 2.5 in 2020).26 In the last 5 years, 5 universities have opened a BPharm program, bringing the total number of BPharm programs to 11 in 2012.2,8 Table 3 lists all Vietnamese universities offering the BPharm program in 2012. Only the HUP is solely dedicated to pharmacy training. Established in 1902, HUP is the oldest and largest pharmacy school in the country and where virtually half of all new pharmacy personnel graduate each year.27 Pharmacy schools are regulated by the Ministry of Health and/or Ministry of Education and Training. Most pharmacy schools are public-funded; however, the number that is privately funded has significantly increased.
Table 3.
Pharmacy Programs Offered by Vietnamese Universities in 2012a
In 2008, there were about 32,700 pharmacist’s assistants with an EDPharm degree and 29,800 with an SDPharm degree, 28 and as of 2010, there were approximately 13,900 pharmacists, of whom about 1,400 held a postgraduate degree.29 (These figures do not include people working in pharmacy schools, research centers, and some central hospitals). According to 2009 data, the expected annual number of graduates was about 5,200 with an EDPharm degree, 2,000 with an SDPharm degree, and 1,300 with a BPharm degree.26 Only 3 universities offer postgraduate pharmacy programs. In 2010, about 300 positions were available in the MPharm and FDSPharm programs, and about 20 positions were available in the PhDPharm and SDSPharm programs. Because of the limited numbers admitted to postgraduate pharmacy programs, as well as concerns about the quality of education, some prospective pharmacists seek opportunities overseas to pursue a masters or PhD degree.
Education Quality Assurance
In Vietnam, the quality of education has been given much attention in the last 10 years. There is a general system for the accreditation of establishments and quality assurance, but no specific system exists for pharmacy education. The General Department for Educational Quality Assurance, Accreditation, and Testing under the Ministry of Education and Training was established in 2004 and has developed many innovative policies of quality assessment at the national level. Since 2007, each pharmacy school is obliged to set up a Unit for Quality Assurance, Accreditation, and Testing that is responsible for quality assurance at the institutional level.30 The pharmacy schools are assessed according to a set of 10 criteria (mission, management, programs, education activities, research, staff, students, international cooperation, materials, and financial management). The process of quality assessment must include 3 steps: (1) internal assessment by the school, (2) external assessment by the Ministry of Education and Training, and (3) an accreditation decision.31 The internal assessment began as a voluntary exercise but became mandatory in 2007. The pharmacy school is required to report the results of internal assessment to the public and the Ministry of Education and Training, annually.30 Schools have started to conduct surveys about opinions of students in order to improve the education programs.27,32 The accreditation requirement is a first step in improving the quality of pharmacy education in Vietnam.
CAREER OPPORTUNITIES
With a degree from pharmacy school, graduates are able to be employed immediately in most public or private settings. While the lowest entry-to-practice qualification is the EDPharm, only those who have obtained the BPharm are considered to be fully qualified pharmacy practitioners.33 For example, a BPharm is required to be a head of a pharmacy department, a clinical pharmacist, or compounding pharmacist for pediatric, cancer, and addictive drug users in a hospital, except for small hospitals in which a SDPharm is obligatory.23 However, pharmacy staff members must apply for a Private Pharmacy Practice License to become the chief or a professionally responsible person in a private pharmaceutical company. The BPharm with a minimum of 5 years of practical experience is generally required to be a chief of a private pharmacy in an urban area (or 2 years of practical experience for rural areas), or required with a minimum of 3 to 5 years of practical experience to be a professionally responsible person for a private pharmaceutical company (eg, company providing pharmaceutical quality control services, a pharmaceutical manufacturing company, a wholesale drug distributor, or a company providing pharmaceutical storage services). EDPharm holders with at least 2 years of experience can work as the person in charge of a community health center or as a distributor-owned wholesale dealer.33
Career opportunities in pharmacy are quite abundant because of the large shortage of pharmacists in all sectors. In 2010 all BPharm graduates of the 2 largest pharmacy faculties had a job 1 year after graduation.27,32 According to the Vietnamese Drug Administration, there were 15,150 pharmacists in 2010 (not including pharmacists working in pharmacy schools, research institutions, and some central hospitals), 59% of whom worked in community pharmacies, 23% in the drug industry, 12% in hospitals and health care facilities, 3% in government agencies, and 3% in other settings.29 Because of the lack of pharmacists, many register to work in community pharmacies but also have jobs in a pharmaceutical company. In fact, for most pharmacists, the pharmaceutical industry was their first career choice. There is a highly unbalanced distribution of the pharmacy workforce between urban and rural regions, with 82% of pharmacists working in urban areas where only 27% of the population lives.1,26 In particular, nearly half the pharmacy workforce is concentrated in the 2 largest cities, Ha Noi and Ho Chi Minh.29
In 2012, the total number of pharmacies (definitions may operate as a faculty in the provision of pharmacy services in the community or hospital settings by International Pharmaceutical Federation) was 43,629, while there are only 12,000 pharmacists.25 Therefore, pharmacies are largely staffed by EDPharm or SDPharm. Particularly, private pharmacies are largely staffed with pharmacists’ assistants or even untrained personnel, while the pharmacists in charge are often absent. Career opportunities in the pharmaceutical industry also seem abundant and promising. Positions ranging from research or quality control management to product marketing are readily available. Many young pharmacists start to work as pharmaceutical sales representatives in the first years after graduation and then open a private pharmacy for extra income when they have gained 5 years of experience. Domestic drug manufacturing companies have focused on research and development capabilities to gain a competitive advantage over foreign drug companies,34 and this is likely to expand the number of job opportunities in the future. There is a considerable shortage of pharmacists in hospitals and healthcare facilities. However, many graduates are unwilling to assume the role of hospital pharmacist because of low salaries and a heavy supply management and administrative workload.
The majority of pharmacists with an MPharm or PhDPharm degree work in pharmacy schools, research institutions, and hospitals. These pharmacists with postgraduate degrees often have positions of high responsibility in pharmaceutical settings, such as regulatory agencies, hospitals, and the pharmaceutical industry. Those graduating from overseas MSc or PhD programs often decide to return to work in Vietnam and contribute enormously to foster innovation in pharmacy education, research, and practice.
Pharmacist’s assistants account for about 82% of the pharmacy workforce and represent about 85% of the annual supply of newly qualified pharmacy personnel.26,28 The expected role of pharmacist’s assistants is to assist a pharmacist in his day-to-day duties. However, because of the serious lack of pharmacists in all settings, pharmacy assistants in many settings around the country, such as community pharmacies, primary healthcare facilities, and small hospitals, are performing tasks that are usually considered to be solely the domain of qualified pharmacists. There is a wide gap between Vietnam’s increasing demand for qualified pharmacists and its limited capacity to train sufficient numbers to meet the need. For the foreseeable future, pharmacists will continue to be in short supply in Vietnam and pharmacist’s assistants will continue to shoulder most of the responsibilities.
EDUCATIONAL BARRIERS
While the roles of pharmacists have rapidly evolved and broadened, the existing pharmacy programs have yet to prepare graduates adequately for these professional demands. Obstacles to the improvement of quality pharmacy education include:
A lack of involvement of professional bodies in the improvement of the quality of pharmacy education. Vietnamese pharmacy programs focus heavily on the basic sciences and the curriculum is still product oriented. Laboratory-based courses are still seen as an important method of teaching skills, but clinical training and practical experience have not received adequate attention.
There is a lack of qualified pharmacy academics and a poor institutional infrastructure (basic facilities as well as learning and teaching resources are insufficient).
Innovative teaching methodologies (eg, case-based learning, teaching in small groups, student presentations) are being introduced at several schools, but this is often hampered by large class size. Traditional teaching methods restricted to large group lectures using a white board and PowerPoint slides still dominate.
Places in postgraduate pharmacy programs are limited.
Continuing education opportunities for life-long learning by all practitioners are few and not compulsory.
RECENT AND FUTURE DIRECTIONS OF PHARMACY EDUCATION
In Vietnam, serious shortages in the number of trained pharmacists and concerns over competency have spurred reforms in pharmacy education. A coordinated and multifaceted effort to advance pharmacy workforce planning, training, and education is being made in order to train an adequate number of highly qualified pharmacists:2,26,34-36
To overcome the shortage of pharmacists in disadvantaged areas, pharmacy schools are allowed to:
Organize in-service pharmacy education programs for workers from health centers, hospitals, drug regulatory agency, pharmaceutical company, etc, who are unable to attend academic programs.
Develop bridging programs for pharmacy staff members to earn a BPharm degree.
Strengthen needs-based education of the pharmacy workforce in mountainous and other disadvantaged regions by waiving admission criteria for applicants.
Some efforts to develop the system of pharmacy schools include:
Enlarging existing pharmacy schools and encouraging the establishment of new pharmacy schools.
Enhancing the autonomy of pharmacy schools financially, administratively, and in designing their own curricula and the modalities of teaching, evaluation, and research.
Increasing investment in public pharmacy schools; upgrading teaching facilities such as classrooms, laboratories, teaching instruments, materials, and computerized services.
To improve the quality of pharmacy education, some strategies include:
Set up a national framework of pharmacy programs as guidelines for pharmacy schools to develop their own specific curricula.
Promote participative learning and teaching methods.
Elaborate standard pharmacy textbooks with updated and advanced content.
Improve the quality of postgraduate pharmacy programs and increase the number of students enrolled.
Promote cooperation between pharmacy schools and research centers, hospitals, and industry.
Train pharmacy academics (lecturers, educational managers) through government projects or in cooperation with overseas organizations.
Enhance the research capacity of pharmacy schools.
Offer continuing education to upgrade the knowledge and skills of the existing pharmacy workforce.
Perform quality control and accreditation of pharmacy education programs.
CONCLUSION
With the rapid expansion in the number of pharmacy schools and degree programs, ensuring high-quality pharmacy education is a major challenge for Vietnam. The need for increased academic capacity and building strategies should be taken seriously. Data collection on the characteristics of the pharmacy workforce and pharmacy practices, identifying the specific needs of the country, and using these to develop comprehensive education is considered as a first step towards improving the quality of pharmacy education in Vietnam. Like many (if not most) Southern countries, clinical pharmacy education and practice in Vietnam is not or only partially integrated into patient care.22 The recent legislative changes and innovations in pharmacy education in general are predicted to be a springboard for the further development of training in clinical pharmacy in the near future in Vietnam.
ACKNOWLEDGEMENTS
We wish to thank Viet-Thanh Truong, Minh-Nguyet Le, MSc, Department of Pharmacy, Hue University of Medicine and Pharmacy, for their assistance during the preparation of this article and Dr Alison Foote (Grenoble Clinical Research Centre) for critically reading and editing the manuscript. Thi-Ha Vo is a PhD candidate funded by The Vietnamese Ministry of Education and Training’s Scholarship. Bedouch P is funded by a Poste d’accueil CNRS/CHU Grenoble award of the CNRS (French Center for Scientific Research).
REFERENCES
- 1.General Statistics Office of Vietnam. Statistical data. http://www.gso.gov.vn/default_en.aspx?tabid=491. Accessed January 9, 2013. [Google Scholar]
- 2.International Pharmaceutical Federation. 2009 FIP Global Pharmacy Workforce and Migration Report. http://www.fip.org/menu_sitemap?page=hrfh_introduction. Accessed January 9, 2013. [Google Scholar]
- 3.Bourdon O, Ekeland C, Brion F. Pharmacy education in France. Am J Pharm Educ. 2008;72(6):Article 132. doi: 10.5688/aj7206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sosabowski MH, Gard PR. Pharmacy education in the United Kingdom. Am J Pharm Educ. 2008;72(6):Article 130. doi: 10.5688/aj7206130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ministry of Education and Training – Health Ministry of Vietnam. [Inter-ministerial Circular on guidelines for the conversion between post-graduate diplomas and programs in health education] (No.30/2003/TTLT-BGDDT-BYT) http://thuvienphapluat.vn/archive/Thong-tu-lien-tich/Thong-tu-lien-tich-30-2003-TTLT-BGDDT-BYT-huong-dan-chuyen-doi-van-bang-trinh-do-dao-tao-sau-dai-hoc-linh-vuc-y-te-vb51522t24.aspx. Accessed January 9, 2013. [Google Scholar]
- 6.HoChiMinh University of Medicine and Pharmacy. [Announcement of postgraduate enrollment 2012] http://www.yds.edu.vn/?Content=thongtinDV&idTin=4933. Accessed February 8, 2013. [Google Scholar]
- 7.Hanoi University of Pharmacy. [Annoucement of master's and doctoral enrollement 2012]. http://www.hup.edu.vn/cpbdv/psdh/noidung/Lists/TuyenSinh/View_Detail.aspx?ItemID=29.
- 8.Ministry of Education and Training of Vietnam. [University and college admission Guidelines 2012 (updated)]. http://www.moet.gov.vn/?page=1.26&view=4032. Accessed January 9, 2013. [Google Scholar]
- 9.Ministry of Education and Training of Vietnam. [Regulations on Doctoral training programs] (No. 10 /2009/TT-BGDĐT) http://vanban.moet.gov.vn/?page=1.15&script=viewdoc&view=1170&opt=brpage. Accessed January 9, 2013. [Google Scholar]
- 10.Ministry of Education and Training of Vietnam. [Regulation on the determination of admission criteria, procedure of registration, reporting, inspection and handling, to postgraduate, univeristy, college and vocational secondary schools] ( 795/QĐ-BGDĐT) http://thuvienphapluat.vn/archive/Quyet-dinh-795-QD-BGDDT-xac-dinh-chi-tieu-tuyen-sinh-quy-trinh-dang-ky-vb102207.aspx. Accessed February 18 2013. [Google Scholar]
- 11.HoChiMinh University of Medicine and Pharmacy. [The curriculum of study of the Elementary Diploma in Pharmacy]. http://uphcm.edu.vn/images/upload/tintuc/muctieuvachuongtrinh.pdf. Assessed July 4 2013. [Google Scholar]
- 12.Health Ministry of Vietnam. [Decree announcing the national SDPharm curriculum framework] (No.475 /2003/QĐ-BYT) http://www.moh.gov.vn/wps/portal/boyte/vanban/chitiet?presentationtemplate=pt_vbtt&WCM_GLOBAL_CONTEXT=9dcda08047269b14bc32bf06a5b06b14. Accessed January 9, 2013. [Google Scholar]
- 13.Ministry of Education and Training of Vietnam. [Circular of the Minister of Education and Training announcing the national college-level curriculum framework for health science education] (No.11 /2010/TT-BGDĐT) http://vanban.moet.gov.vn/?page=1.15&script=viewdoc&view=2147&opt=brpage. Accessed January 9, 2013. [Google Scholar]
- 14.Ministry of Education and Training of Vietnam. [Decree announcing the national college-level and university-level curriculum framework for health science education] (No.12/2001/QĐ-BGD&ĐT) http://vanban.moet.gov.vn/?page=1.15&script=viewdoc&view=15763&opt=brpage. Accessed January 9, 2013. [Google Scholar]
- 15.Ministry of Education and Training of Vietnam. [Circular of the Minister of Education and Training announcing the national university-level curriculum framework for health science education] (No.01/2012/TT-BGDĐT) http://vanban.moet.gov.vn/?page=1.15&script=viewdoc&view=3954&opt=brpage. Accessed January 9, 2013. [Google Scholar]
- 16.Hanoi University of Pharmacy. [BPharm Pharmacy education programs] http://www.hup.edu.vn/cpbdv/psdh/noidung/Lists/CaoHoc/Attachments/58/Chuong%20trinh%20dao%20tao%20Thac%20si%20duoc%20hoc.pdf. Accessed February 8, 2013. [Google Scholar]
- 17.HochiMinh University of Medicine and Pharmacy. [Master's degree training] http://moodle.yds.edu.vn/yds2/?Content=thongtinDV&idTin=546. Accessed February 8, 2013. [Google Scholar]
- 18.Health Ministry of Vietnam. [Regulations on Training Specialists to level I] (No.1636/QĐ-BYT) http://www.tnmc.edu.vn/webdhyd/index.php?language=vi&nv=news&op=Sau-dai-hoc/Quy-che-dao-tao-Chuyen-khoa-cap-I-sau-dai-hoc-43. Accessed January 9, 2013. [Google Scholar]
- 19.Health Ministry of Vietnam. [Regulations on Training Specialists to level II] (No.1637/QĐ-BYT) http://www.tnmc.edu.vn/webdhyd/index.php?language=vi&nv=news&op=Sau-dai-hoc/Quy-che-dao-tao-Chuyen-khoa-cap-II-sau-dai-hoc-44. Accessed January 9, 2013. [Google Scholar]
- 20.Thi-Kim-Huyen Hoang. [Textbook of Clinical Pharmacy] Hanoi: Vietnamese Medical Press; 2006. [Google Scholar]
- 21.Thi-Ha Vo, Pierrick Bedouch, Thi-Lien-Huong Nguyen, et al. The 2011 National Survey on Clinical Pharmacy Services in Vietnamese Central and Provincial Hospitals. Paper presented at: The 41st European Society of Clinical Pharmacy Symposium, 2012; Barcelona, Spain. [Google Scholar]
- 22.University of Groningen. Strengthening the training quality of clinical pharmacists in Vietnam. http://www.rug.nl/internationalrelations/developmentcooperation/nptniche/pharmacie/index. Accessed January 9, 2013. [Google Scholar]
- 23.Health Ministry of Vietnam. [Circular defining the organization and the operation of Hospital Pharmacy Departments] (No.22/2011/TT-BYT) http://www.soyte.hanoi.gov.vn/?u=dt&id=4200. Accessed January 9, 2013. [Google Scholar]
- 24.Health Ministry of Vietnam. [Circular on guidelines for the implementation of Clinical pharmacy practice in health care facilities (drafting)] http://www.moh.gov.vn/wps/portal/boyte/gopyduthao/chitiet?presentationtemplate=pt_vanbanduthao&WCM_GLOBAL_CONTEXT=2a5c7c8049c32a85984efe047d342be7. Accessed January 9, 2013. [Google Scholar]
- 25.International Pharmaceutical Federation. 2012 FIP Global Pharmacy Workforce Report. http://www.fip.org/static/fipeducation/2012/FIP-Workforce-Report-2012/?page=hr2012#/8. Accessed January 9, 2013. [Google Scholar]
- 26.Health Ministry of Vietnam - Health Partnership Group. Joint annual health review 2009 - Human resources for Health in Vietnam. http://jahr.org.vn/index.php?option=com_content&view=frontpage&lang=en. Accessed January 9, 2013. [Google Scholar]
- 27.Hanoi University of Pharmacy. [2011 Self-assessment Report of Hanoi University of Pharmacy] http://fr.slideshare.net/VoHa1/ban-danh-gia-cua-dh-duoc-hn Accessed January 9, 2013. [Google Scholar]
- 28.Drug Administration of Vietnam - Health Ministry of Vietnam. [Final Report of Pharmaceutical Affairs 2008-Implementation Plan 2009] http://www.vnpca.org.vn/story/bao-cao-tong-ket-cong-tac-du-c-nam-2008-trien-khai-ke-hoach-nam-2009tai-lieu-phuc-vu-hoi-nghi-0. Accessed January 9, 2013. [Google Scholar]
- 29.Vietnam Pharmaceutical Companies Association. [Data for 2010 Pharmaceutical Human Resources] http://www.vnpca.org.vn/story/so-lieu-ve-tinh-hinh-nhan-luc-du-c-2010. Accessed January 9, 2013. [Google Scholar]
- 30.Thi-Phuong-Anh Vu. [Quality assurance of university education in Vietnam and demand for integration] http://www.udn.vn/bcns/view/278/151Accessed July 4, 2013. [Google Scholar]
- 31.Ministry of Education and Training of Vietnam. [Regulations on procedures and cycles of quality audits of universities, colleges and vocational secondary schools] (No.76/2007/QĐ-BGDĐT) http://vanban.moet.gov.vn/?page=1.15&script=viewdoc&view=17564&opt=brpage. Accessed January 9, 2013. [Google Scholar]
- 32.HoChiMinh University of Medicine and Pharmacy. [Public announcement of the actual quality of training in university and college establishments] http://www.yds.edu.vn/?Content=thongtinDV&idTin=5078. Accessed February 8, 2013. [Google Scholar]
- 33.Vietnamese Government. [Decree detailing a number of articles of the Law of Pharmacy] (79/2006/ND-CP) http://moj.gov.vn/vbpq/Lists/Vn%20bn%20php%20lut/View_Detail.aspx?ItemID=15534.
- 34.Vietnamese Prime Minister. [The master plan for development of the Vietnamese pharmaceutical industry in the period 2011-2020 with the extension to 2030] http://www.google.fr/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CC8QFjAA&url=http%3A%2F%2Fwww.dav.gov.vn%2FDesktopModules%2FVietTotal.Documents%2FDownloadAttachment.aspx%3F%26AttachmentId%3D843&;ei=NVkTUZHOBcHK0QWMuYD4DQ&usg=AFQjCNHHbi8ImhIVB7RDP2cRkn48t3Ntxg&bvm=bv.42080656,d.d2k. Accessed February 8, 2013. [Google Scholar]
- 35.Vietnamese Government. [Resolution on basic and comprehensive innovations in higher education in Vietnam during the period of 2006-2020] (No. 14/2005/NQ-CP) http://vanban.moet.gov.vn/?page=1.15&script=viewdoc&view=15003&opt=brpage. Accessed January 9, 2013. [Google Scholar]
- 36.Ministry of Education and Training of Vietnam. [The 2011-2016 action programs of the Ministry of Education and Training] http://www.moet.gov.vn/?page=6.4&view=4132. Accessed February 8, 20. [Google Scholar]