Abstract
Objective. To characterize the use of team-based learning (TBL) in US colleges and schools of pharmacy, including factors that may affect implementation and perceptions of faculty members regarding the impact of TBL on educational outcomes.
Methods. Respondents identified factors that inhibit or enable TBL use and its impact on student learning. Results were stratified by type of institution (public/private), class size, and TBL experience.
Results. Sixty-nine of 100 faculty members (69%) representing 43 (86%) institutions responded. Major factors considered to enable TBL implementation included a single campus and student and administration buy-in. Inhibiting factors included distant campuses, faculty resistance, and lack of training. Compared with traditional lectures, TBL is perceived to enhance student engagement, improve students’ preparation for class, and promote achievement of course outcomes. In addition, TBL is perceived to be more effective than lectures at fostering learning in all 6 domains of Bloom’s Taxonomy.
Conclusions. Despite potential implementation challenges, faculty members perceive that TBL improves student engagement and learning.
Keywords: Team-based learning, active learning, pharmacy, education
INTRODUCTION
Team-based learning (TBL) is an active-learning method used in health professions education programs, including colleges and schools of pharmacy.1 There are 3 phases in TBL: phase 1 is student pre-class preparation, such as a reading assignment and recorded lecture. Phase 2 begins in class with students taking individual and team readiness-assurance tests (iRATs and tRATs, respectively). In phase 3, students work in learning teams to complete team assignments, apply course content to real-world problems, and participate in discussions within and among groups. Team-based learning is a strategy that facilitates active learning in a large-group setting using limited faculty resources. Its use may expand as a result of the Accreditation Council for Pharmacy Education (ACPE) standards’ requirement that active-learning methods be used to develop problem-solving and critical-thinking skills.2 Recommendations made as part of the American Association of Colleges of Pharmacy (AACP) Curricular Change Summit, include future professional pharmacy curricula developing abilities such as self-directed learning and interprofessional collaboration through interactive learning experiences that strongly engage students.3 Team-based learning is a highly interactive method that provides opportunities to practice and improve communication, interpersonal, and collaboration skills as part of preparing student pharmacists for interprofessional practice.
TBL implementation in colleges of medicine has resulted in positive outcomes.4 For example, TBL resulted in improved performance on examination questions, with the most benefit observed among lower-achieving students.5 Factors important for successful TBL implementation have been identified, as well as factors that enable and inhibit its continued use. Inhibiting factors include resistance from students and faculty members, lack of textbooks, and large class sizes. Enabling factors include resources, quality training and support, faculty member engagement/buy-in, and smaller class size.6,7
Documented benefits of TBL compared with lecture-based courses in pharmacy education include improved student performance and student perceptions. 8-14 In addition to improving performance in higher-level cognitive skills, TBL has a favorable impact on communication skills, professionalism, and the ability to work effectively in teams. Research describing the prevalence of TBL as well as factors that enable and inhibit TBL in pharmacy education is limited. The purpose of this study was to examine and characterize TBL use in colleges and schools of pharmacy, including factors that may affect implementation and the perceptions of faculty members regarding its impact on educational outcomes.
METHODS
Faculty members representing 7 US colleges and schools of pharmacy collaborated on this research project as a component of the AACP Academic Leadership Fellows Program (ALFP) during the 2011-2012 academic year. The ALFP is a longitudinal year-long leadership program conducted by AACP to prepare leaders in academic pharmacy. The project received Institutional Review Board approval from each institution.
Pharmacy faculty members with TBL experience were identified by means of a literature search and the AACP Council of Deans and Assessment listservs. Reference lists for articles identified were also searched. US pharmacy faculty members who had used TBL in at least 1 pharmacy course were eligible to participate in the study. One hundred faculty members (administrators and course instructors) representing 50 institutions met the inclusion criterion. An e-mail describing the study along with a consent form and a link to the survey instrument was sent to each faculty member. A follow-up e-mail was sent to nonrespondents on 2 occasions (day 8 and day 15) after the initial e-mail. The data were collected over a 3-week period.
A survey instrument was developed using information from a literature search on TBL focusing on health professions literature. Survey questions included quantitative questions (multiple choice and rating scale) and qualitative questions (single text box). (The survey instrument is available upon request from the corresponding author.) The majority of survey questions were quantitative, but several qualitative questions were included to collect opinions and ideas about specific areas of interest. The instrument was divided into 4 sections and included 27 items. The first section included 11 items that focused on the use of TBL in the curriculum and the degree to which faculty members adhere to the standard components of TBL. The second section contained 4 items that asked respondents to identify factors that inhibit or enable the implementation of TBL. The third section included 4 items that focused on the impact of TBL on educational outcomes, and the last section included 8 items that collected demographic data, including whether the respondent’s college or school of pharmacy is located on a single or multiple campuses.
The draft survey instrument was evaluated by 2 assessment experts and 2 pharmacy faculty members who did not participate in the study. Selection of the assessment experts was based on prior experience with assessment-related activities. Pharmacy faculty members were selected based on prior significant experience with TBL in a pharmacy course. The 2 assessment experts, who were not familiar with TBL, evaluated face validity to identify any ambiguity in the survey questions. The 2 pharmacy faculty members, who were familiar with TBL, evaluated content validity to determine how appropriate the survey questions were with respect to the study. Each of the individuals was asked to review the survey questions and evaluate whether they would produce measurable results. The survey instrument, which was generated using Survey Monkey (survey Monkey, Portland, OR), was modified based on feedback from these evaluators. Data were analyzed using descriptive statistics. Significance was defined a priori as p≤0.05. Statistical analysis was performed using STATA (StataCorp LP, College Station, TX).
RESULTS
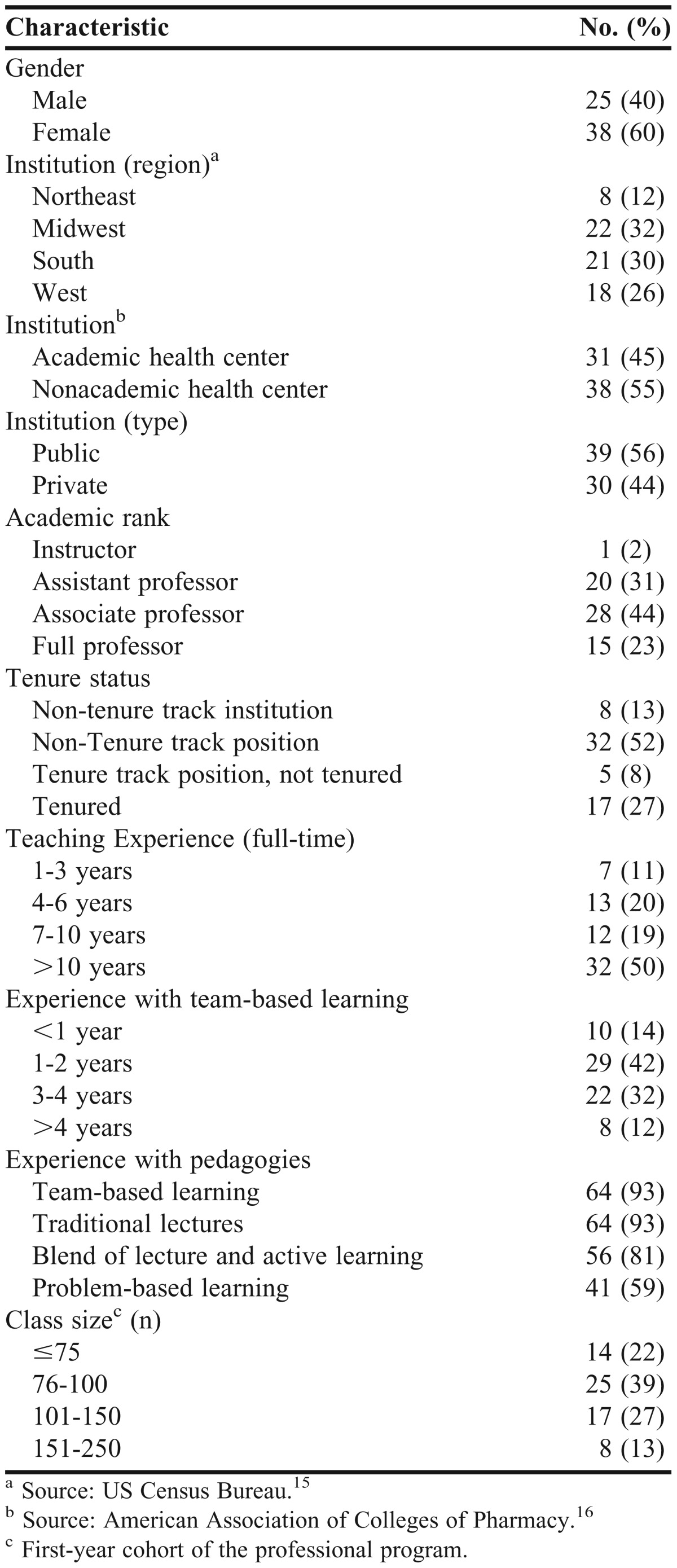
Sixty-nine of 100 (69%) faculty members surveyed responded, representing 43 (86%) of the 50 institutions invited to participate. A wide range of faculty members and institutions were represented in the survey instrument (Table 1). Approximately 60% of the respondents were female and roughly 30% were from the Midwest, South, or West. A slight majority of respondents were from public institutions or not at an academic health center. More respondents held the rank of associate professor (44%) than other ranks, and most respondents were either at an institution that did not grant tenure (13%) or were not in a tenure-track position (52%). Approximately half of the respondents had more than 10 years of full-time teaching experience; however, almost 60% had no more than 2 years of experience with TBL. Nonetheless, more than 90% of respondents had some experience with TBL, and more than 90% had some experience with a traditional, lecture-based pedagogy. Approximately 60% of respondents taught classes of 100 or fewer students.
Table 1.
Demographics of Faculty Members Responding to a Survey Instrument Regarding Team-Based Learning (N = 69)
TBL was used primarily by faculty members teaching courses on a single campus (77%). Responses indicated that TBL had been used in both required and elective classroom courses, as a module within a course, and as the pedagogy for an entire course. Thirty-four respondents indicated that TBL was used in multiple required courses, whereas 10 respondents indicated that TBL was used throughout all required courses of the entire classroom pharmacy curriculum. More than half of the respondents reported that TBL had been used in small classes (50 or fewer students, 71% of respondents), medium-sized classes (51 to 100 students, 86% of respondents), and large classes (101 or more students, 70% of respondents).
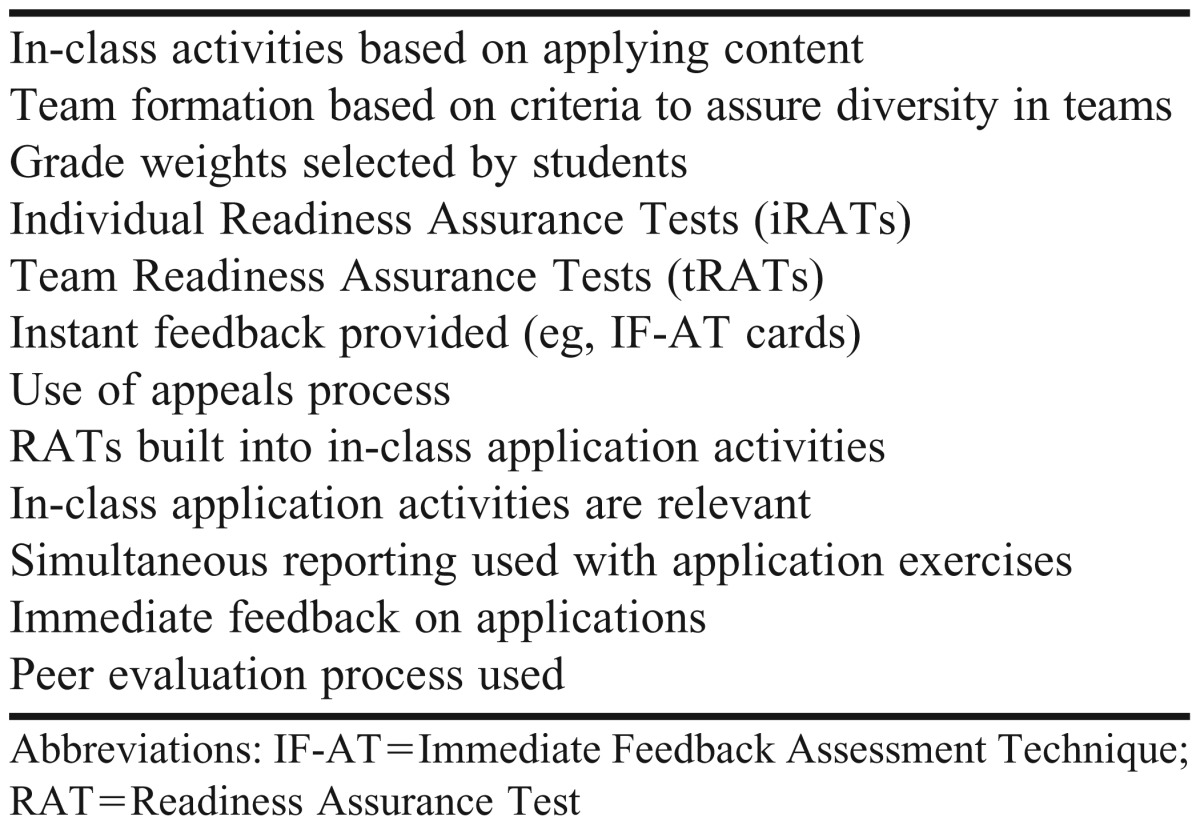
Each of the components of the standardized TBL method, which are presented in Table 2, had been used by between 27% and 99% of respondents. For example, in-class activities based on applying content had been used by 99% of the respondents. Similarly, team readiness assurance tests (tRATs) and individual readiness assurance tests (iRATs) had been used by more than 85% of respondents. In contrast, RATs built into in-class application activities had been used by only 33% of respondents, and grade weights selected by students had been used by only 27% of respondents. Naturally, relatively few respondents had used every component of the standardized TBL method; the greatest fraction of respondents (19%) used only 7 of the 12 TBL components. A large majority (84%) of respondents reported using iRATs and tRATs, and 59% reported using iRATs, tRATs, and peer evaluation. Almost half of the respondents (49%) reported using iRAT, tRAT, peer evaluation, and a group formation strategy that ensured diversity.
Table 2.
Components of Standard Team-Based Learning Implementation
The most commonly reported strategy for grade determination was iRAT plus team performance (57%), followed by the use of a customized progression strategy (33%) and individual performance alone (eg, iRAT and individual examinations, 10%). According to 48% of respondents, a student would pass a course if the student’s individual scores were below passing but combined individual and team scores were above passing.
Commonly reported faculty resources available for TBL included IF-AT (Immediate Feedback Assessment Technique) forms (74%), audience response systems (58%), and teaching assistants (33%). Teaching assistants were more prevalent in public than in private institutions. Additional faculty resources reported by respondents include Web-based materials (eg, tutorials/modules, quizzes, wikis, iRATs, VoiceThread software [VoiceThread.com], Camtasia software [Techsmith.com]), student-mediated feedback, readings, cases, write-ups, course-specific rubrics, standard office supplies (eg, bulk paper, white boards, smart boards, paper tablets, and colored index cards), Scantron sheets (Scantron.com), and fourth-year pharmacy students (teaching assistants). The most commonly reported number of faculty facilitators for each TBL class session was 1 (69%), followed by 2 (20%), and 3 or more (11%).
Commonly reported resources available to students for class preparation included instructor notes or PowerPoint slides (74%), textbooks (59%), textbooks with guided questions or objectives (59%), journal articles (49%), audio or video recording of lectures or other online learning tools (46%), and journal articles with guided questions or objectives (42%). Other resources available to students included national guidelines, executive summaries that highlight specific areas to master prior to class, problem sets, old examinations, TBL sessions after live lecture, and traditional library resources.
Although the majority of respondents were from single-campus institutions, TBL had also been used by multi-campus institutions. Of the 9 respondents who indicated that their institution used TBL on multiple campuses, 5 reported that they used distance technology to deliver TBL content from 1 site to multiple campuses, and 4 reported that TBL sessions were facilitated independently on each campus.
Using a 4-point Likert scale, 80% of respondents perceived TBL to have some degree of value at their institution (very=27%; somewhat=54%; not very=15%; none=5%). The overall mean response was 3.0, with faculty members at public institutions perceiving slightly greater value than those at private institutions (3.04 vs 3.03).
Student course evaluations were the most common method (66%) for assessing TBL effectiveness, followed by longitudinal comparisons of student grades (52%), final examination scores (51%), summative assessments (48%), and formative assessments (46%). End-of-year examinations (10%) and capstone projects (7%) were used less extensively, as were teamwork surveys (4%), professionalism surveys (4%), student perception surveys (4%), assessment of problem-solving skills (4%), pre-course assessments (1%), and experiential education evaluations (1%).
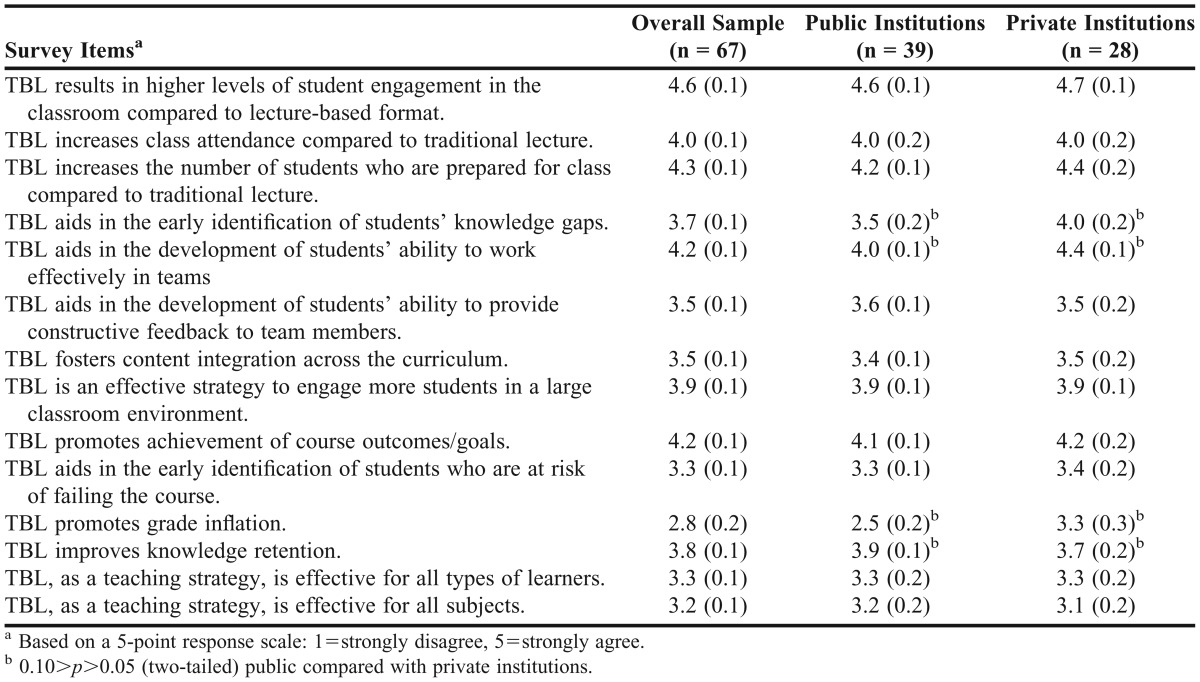
Respondents’ perceptions of the impact of TBL are presented in Table 3. Overall, TBL was seen as an effective incentive for students to prepare for class and to be engaged and work as a team during class. Respondents did not indicate that TBL promotes grade inflation and provided mixed responses when asked if TBL improves knowledge retention. There were no significant differences in responses from faculty members at public or private institutions.
Table 3.
Faculty Perceptions of the Impact of Team-Based Learning (TBL) on Various Educational Parameters
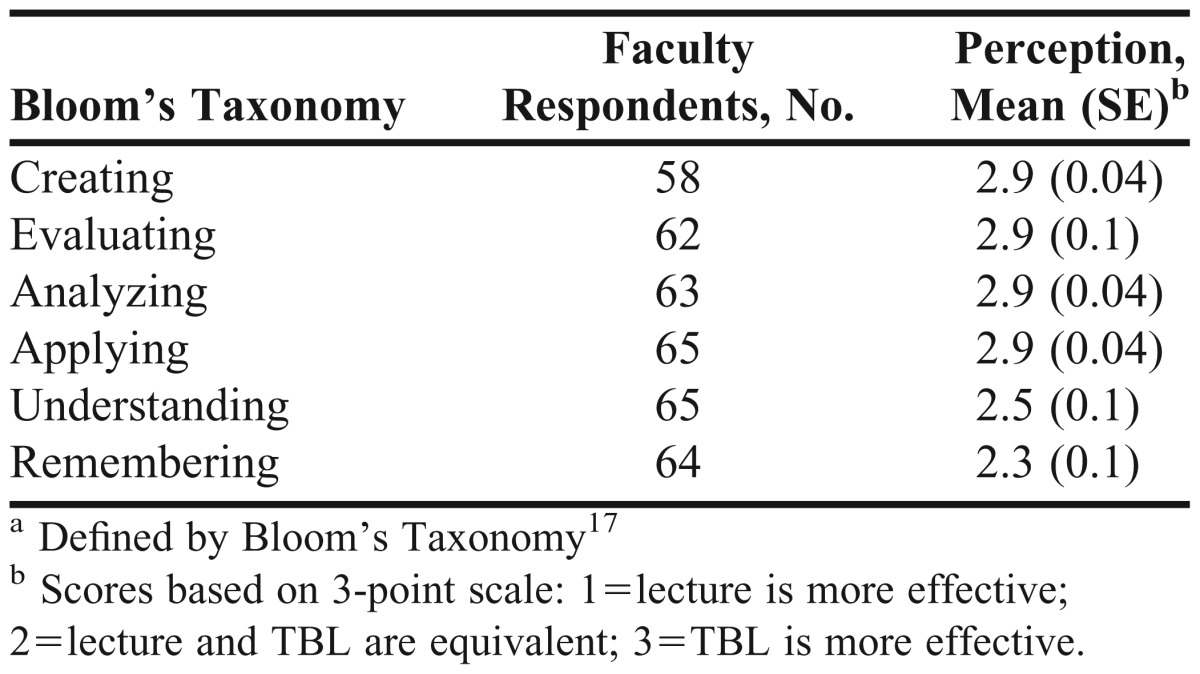
Finally, TBL was perceived to be more effective than traditional lectures in fostering learning for each domain in Bloom’s Taxonomy (Table 4). The order of domain achievement from highest to lowest was: applying, analyzing, evaluating, creating, understanding, and remembering. The differences between TBL and traditional lectures in learning efficacy were greater for the higher levels of learning domains (applying, analyzing, evaluating, creating) than lower levels (remembering, understanding). Typically, respondents from public institutions indicated that TBL was associated with slightly more favorable outcomes than did respondents from private institutions, but the differences were not significant.
Table 4.
Faculty Perceptions of the Ability to Achieve Educational Outcomesa Using Traditional Lecture vs Team-Based Learning (TBL)
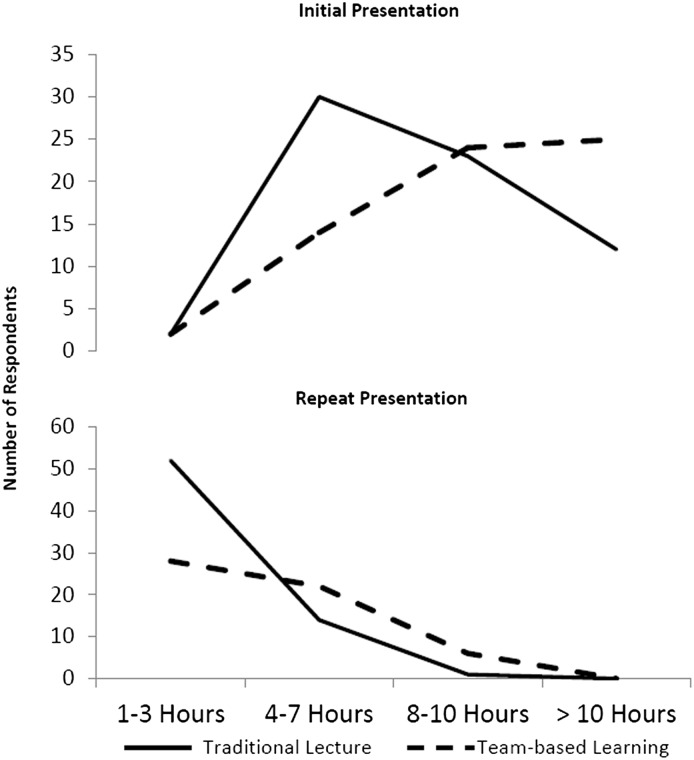
The amount of time required for faculty members to prepare for a TBL session was compared with that for a 1-hour lecture (Figure 1). Respondents indicated that TBL sessions/lectures given for the first time required greater preparation time than those that had been modified from previous efforts. Moreover, respondents indicated that TBL sessions required greater preparation time than did traditional lectures, regardless of whether the presentations were being given for the first time or had been modified from previous efforts. However, the difference in time required to prepare for TBL sessions and traditional lectures was smaller for modified presentations than for first-time presentations.
Figure 1.
Estimated preparation time required for presentation of course material using traditional lecture and team-based learning for initial presentation (top) and repeat presentations in subsequent years (bottom).
Despite that greater initial effort was required to prepare a TBL session than a traditional lecture, 9% of respondents indicated plans to offer other courses in TBL format, 14% of respondents indicated plans to expand TBL use in courses that do not use TBL exclusively, and 72% of respondents indicated plans to maintain their current use of TBL. Whereas 4% of respondents indicated plans to decrease their use of TBL, only 1% of respondents indicated plans to discontinue TBL entirely.
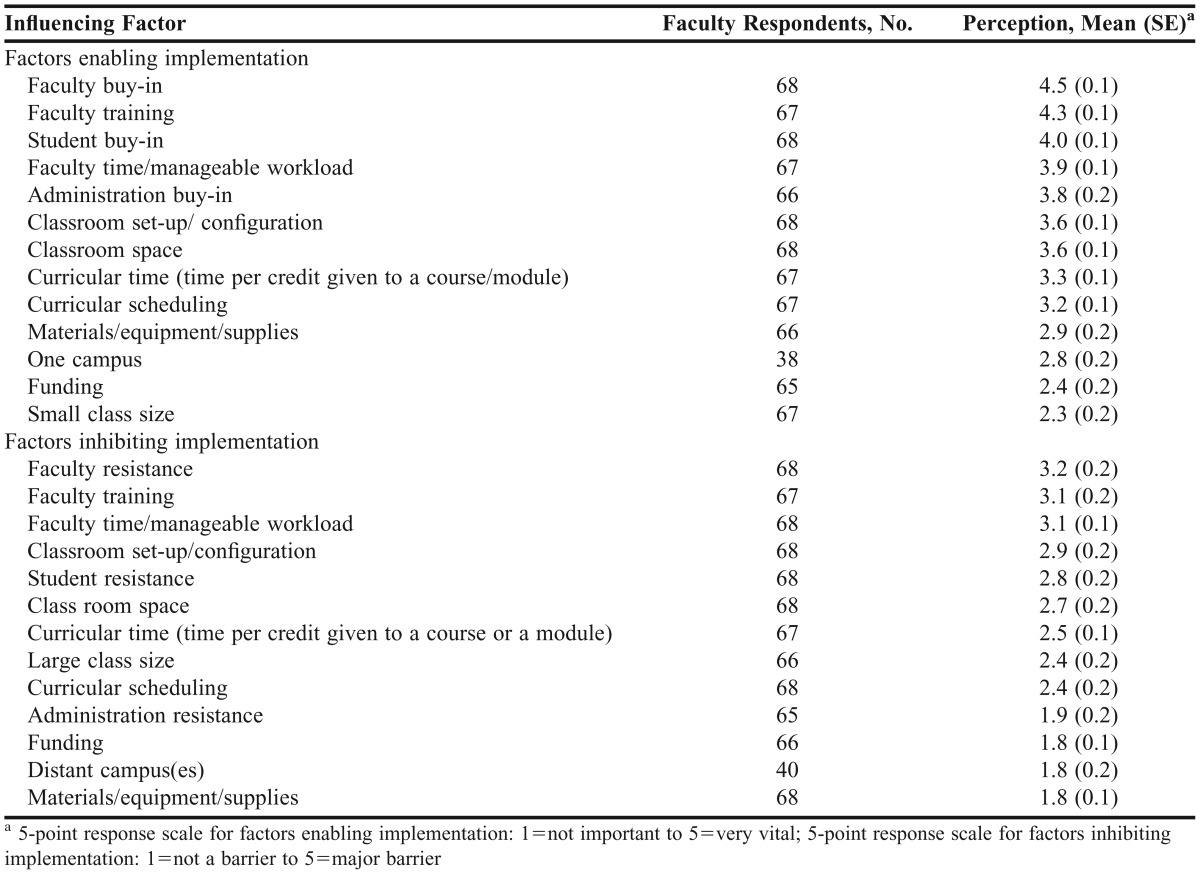
As indicated in Table 5, respondents identified factors that enable or inhibit implementation of TBL using a 5-point Likert scale (for potential enabling factors, 1=not important, 5=very vital; for potential inhibiting factors, 1=not a barrier; 5=major barrier). Factors seen as enabling use of TBL included faculty training and student, faculty and administrator buy-in. Major inhibitors of TBL implementation included faculty member resistance, and faculty member training. Issues related to faculty member workload ranked as the fourth most important enabling and the fourth-most important inhibiting factor.
Table 5.
Faculty Perceptions of the Importance of Factors Enabling and Inhibiting Implementation of Team-Based Learning at Their Respective Institutions
Respondents were also asked to identify insurmountable barriers to increasing TBL implementation. A majority of respondents (n=41; 59%) stated that there are no insurmountable barriers. There was little consensus among those who indicated that there were insurmountable barriers. Faculty member resistance (n=4), student resistance (n=2), negative perception of TBL by students, faculty, and administrators (n=2), multiple campuses (n=1), large classes (n=1), quantitative faculty (n=1), course scheduling challenges (n=1), inappropriate classroom configuration (n=1), and being the sole proponent of TBL at the institution (n=1) were all cited as being insurmountable barriers at the respondents’ respective institutions.
Respondents were asked to describe strategies used to overcome barriers to TBL implementation. Strategies being used to overcome the perceived barrier of multiple campuses included placing a faculty facilitator or teaching assistant at each campus or conducting separately facilitated sessions at each site. Numerous respondents reported overcoming faculty resistance by implementing TBL faculty-development programs. Other strategies used to overcome faculty resistance included inviting faculty members to observe TBL, securing support from administration, allowing adequate time to transition to a TBL pedagogy, implementing TBL 1 course at a time, hiring a dedicated pharmacy instructional designer, using a focus group consisting of an outside facilitator and selected students to evaluate TBL, implementing only selected components of TBL, involving faculty members in creating TBL sessions, purchasing Michaelsen’s book,1 using credible experts as resources, conducting TBL-focused research, and hiring faculty members willing to use TBL.
A commonly used strategy to overcome student resistance was communication with students regarding the benefits of TBL and the rationale for its use. Other strategies included concept-mapping in the active-learning sessions, reinforcing concepts learned in a previous class in the next course offering, allowing for an adjustment period by being persistent in implementing TBL, using student focus groups to avoid disengagement, using a student appeal process, and emphasizing the implementation of TBL during the student recruiting and admissions processes.
The most prevalent strategy used to overcome classroom limitations was the creative use of existing space (ie, using multiple small rooms for team exercises, encouraging students to face their teammates, seating students in a rectangular or circular configuration rather than in long rows, assigning seats in class/team rooms, and being proactive in requesting teaching space). When possible, new classrooms were built to create a classroom environment more conducive to TBL.
DISCUSSION
Team-based learning is a teaching strategy that facilitates incorporation of active learning into curricula in colleges and schools of pharmacy. Challenges associated with implementation of TBL exist but can be overcome. Use of technology and independent facilitation of TBL sessions were strategies used to overcome the obstacle of multiple or distance campuses. Faculty development and support from administration helped overcome resistance from faculty members, whereas clear communication with students about TBL was used to overcome student resistance. Creative use of existing space helped faculty members overcome logistical barriers.
Faculty members who had implemented TBL perceived that the strategy improved student preparation for and engagement during class and promoted achievement of course outcomes. Further, faculty members perceived TBL to be more effective than traditional lectures at fostering learning in all 6 domains of Bloom’s Taxonomy.
The findings presented in the current study are noteworthy in that they represent perceptions of faculty teaching in approximately one-third of colleges and schools of pharmacy in the United States, representing all 4 US regions (Northeast, Midwest, South, and West) and public and private institutions with both large and small class sizes.
Factors perceived as enabling implementation of TBL included buy-in from administration, faculty members, and students. Additionally, faculty member workload was seen as an important factor to consider. Logistics also scored high among respondents who perceived a single campus, classroom space, and classroom configuration to be important issues to address. Overall, faculty training, resistance, and workload issues were perceived to be significant barriers to implementing TBL. Whereas faculty training was perceived to be the least important enabling factor in the implementation of TBL, it was perceived to be the third most important barrier. The offering of TBL development programs was the most commonly used strategy to overcome faculty resistance.
This study identified several important factors that both enabled and inhibited TBL implementation; these findings are consistent with those identified in previous investigations into the use of TBL in medical education.7 When present, factors that foster buy-in from faculty members and students and support from administration are considered enabling the use of TBL, and when absent, they are seen as barriers.
Faculty member workload was designated as both an enabling and an inhibiting factor. For institutions that use problem-based learning, TBL presented a workload advantage in that 1 or 2 faculty members can facilitate an entire class. Preparation for the initial delivery of course content using TBL has been perceived as being more labor intensive than that for traditional lectures. However, with repeated presentations, there was little perceived difference in workload between preparations for TBL and preparations for lecture. Recognizing the benefits of TBL may overcome the barrier of the greater amount of time needed to develop initial TBL sessions. Continued research on long-term benefits of TBL is warranted. Programs considering implementation of TBL would be more likely to ensure early success by gaining consensus among administration and faculty members, conducting faculty training workshops, and considering the workload and logistical needs of this teaching strategy. Although funding was not perceived as important in either enabling or inhibiting TBL implementation, respondents noted that supportive factors included the availability of IF-AT response forms, clicker technology, teaching assistants, and the ability to use educational spaces creatively.
Assessing the effectiveness of TBL is a challenge as important as assessing the effectiveness of traditional teaching methodologies. Many of the respondents indicated that they use student evaluations as measures of effectiveness. Moreover, approximately half of respondents reported using additional methods, including longitudinal comparisons of student grades, final examination grades, and formative and summative assessments. Assessment of teaching effectiveness with TBL, as with other pedagogies, requires thoughtful consideration of feedback from multiple sources. Peer-teaching assessment tools for faculty members using team-based learning are needed. Ideally, such tools would assess TBL processes as well as achievement of student learning outcomes.
Future pharmacy graduates will face many challenges, leading to the call from several professional groups for changes in the ways students learn and the abilities they acquire as part of their education. In Standard number 11 of Standards 2007, ACPE recommends implementing teaching and learning methods that foster the development and maturation of critical thinking and problem-solving skills and enable students to transition from dependent to active, self-directed, lifelong learners.2 Following the 2009 AACP Curricular Summit, there were calls for redefining pharmacy curricula to meet future needs of the profession. Specific abilities needed for success include self-directed learning competencies.3 As noted in an ACCP white paper, the knowledge base required to provide patient care is rapidly expanding, and advances in information technology allow for ongoing access to new knowledge.18 In this dynamic environment, self-directed learning is essential for pharmacists if they are to be viewed as experts in pharmacotherapy.19 Team-based learning is an active-learning strategy that requires students to be fully engaged. The use of individual readiness-assurance tests holds students accountable for pre-class reading and preparation, which reinforces self-directed learning behaviors. Based on these factors, TBL is an educational strategy that allows pharmacy educators to meet the challenges facing future graduates.
Limitations of this study include the potential bias that may arise from evaluating responses from early adopters of TBL. Faculty champions of TBL, particularly those who have taught multiple courses using the strategy, may be more likely to have favorable perceptions of TBL. Additionally, the current study sought feedback from faculty members who have successfully overcome barriers to implementing TBL. Faculty members who have considered but not implemented TBL in their courses were not identified as potential survey respondents. Feedback from those faculty members may provide more insight into perceived insurmountable barriers to TBL implementation at their institutions, along with possible reasons why those barriers could not be overcome.
CONCLUSIONS
Faculty in approximately one-third of US schools and colleges of pharmacy have implemented team-based learning in stand-alone courses or across the curriculum. In the presence of administrative support and buy-in from faculty members and students, TBL can be successfully implemented in colleges and schools of pharmacy. Faculty members perceive TBL to be a teaching strategy that fosters student learning and engagement and supports achievement of educational outcomes.
ACKNOWLEDGEMENTS
The authors acknowledge Anne Lin, PharmD, (School of Pharmacy, Notre Dame of Maryland University), who served as the Dean Facilitator for our research project as part of AACP’s Academic Leadership Fellows Program. We also thank the AACP staff, specifically Robert (Buzz) Kerr, PharmD, and Bradford Miller. Additionally, we thank Drs. Persky, Gleason, Will O’Shea, and Cat Marlow for their assistance with survey validation and Robert Haight for his assistance with data analysis. Finally, we thank the Dean mentors at our respective institutions: Kathleen Kennedy, PharmD, Xavier University of Louisiana College of Pharmacy; Arcelia Johnson-Fannin, PharmD, University of the Incarnate Word, Feik School of Pharmacy; Marie Chisholm-Burns, PharmD, MPH, University of Tennessee Health Science Center College of Pharmacy; Susan Stein, BS, MS, DHEd, Pacific University School of Pharmacy; Janet Houser, PhD, Rueckert-Hartman College for Health Professions, Regis University; R. Lee Evans, PharmD, Auburn University Harrison School of Pharmacy.
REFERENCES
- 1.Michaelsen LK, Parmalee DX, McMahon LL, Levine RE, editors. Team-Based Learning for Health Professions Education: A Guide to Using Small Groups for Improving Learning. Sterling. VA: Stylus Publishing; 2008. [Google Scholar]
- 2.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Version 2.0. The Accreditation Council for Pharmacy Education Inc. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed September 11, 2012. [Google Scholar]
- 3.Jungnickel P, Kelly K, Hammer D, Haines S, Marlowe K. Addressing competencies for the future in the professional curriculum. Am J Pharm Educ. 2009;73(8):Article 156. doi: 10.5688/aj7308156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Searle NS, Haidet P, Kelly PA, Schneider VF, Seidel CL, Richards BF. TBL in medical education: initial experiences at ten institutions. Acad Med. 2003;78(10 suppl):S55–S58. doi: 10.1097/00001888-200310001-00018. [DOI] [PubMed] [Google Scholar]
- 5.Koles PG, Stolfi A, Borges NJ, Nelson S, Parmelee DX. The impact of team-based learning on medical students’ academic performance. Acad Med. 2010;85(11):1739–1745. doi: 10.1097/ACM.0b013e3181f52bed. [DOI] [PubMed] [Google Scholar]
- 6.Thompson BM, Schneider VF, McMahon K, Levine R, Perkowski L, Richards BF. Team-based learning at ten medical schools: two years later. Med Educ. 2007;41(3):250–257. doi: 10.1111/j.1365-2929.2006.02684.x. [DOI] [PubMed] [Google Scholar]
- 7.Thompson BM, Schneider VF, Haidet P, Perkowski LC, Richards BF. Factors influencing implementation of team-based learning in health sciences education. Acad Med. 2007;82(10 Suppl):S53–S56. doi: 10.1097/ACM.0b013e3181405f15. [DOI] [PubMed] [Google Scholar]
- 8.Letassy NA, Fugate SE, Medina MS, Stroup JS, Britton ML. Using team-based learning in an endocrine module taught across two campuses. Am J Pharm Educ. 2008;72(5):Article 103. doi: 10.5688/aj7205103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beatty SJ, Kelley KA, Metzger AH, Bellebaum KL, McAuley JW. Team-based learning in therapeutics workshop sessions. Am J Pharm Educ. 2009;73(6):Article 100. doi: 10.5688/aj7306100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zingone MM, Franks AS, Guirguis AB, George CM, Howard-Thompson A, Heidel RE. Comparing team-based and mixed active learning methods in an ambulatory care elective course. Am J Pharm Educ. 2010;74(9):Article 160. doi: 10.5688/aj7409160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conway SE, Johnson JL, Ripley TL. Integration of team-based learning strategies into a cardiovascular module. Am J Pharm Educ. 2010;74(2):Article 35. doi: 10.5688/aj740235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Persky AM, Pollack GM. A modified team-based learning physiology course. Am J Pharm Educ. 2011;75(10):Article 204. doi: 10.5688/ajpe7510204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grady SE. Team-based learning in pharmacotherapeutics. Am J Pharm Educ. 2011;75(7):Article 136. doi: 10.5688/ajpe757136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Persky AM. The impact of team-based learning on a foundational pharmacokinetics course. Am J Pharm Educ. 2012;76(2):Article 31. doi: 10.5688/ajpe76231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US Census Bureau. Census Regions and Divisions of the United States. https://www.census.gov/geo/www/us_regdiv.pdf. Accessed November 30, 2012. [Google Scholar]
- 16.American Association of Colleges of Pharmacy. Institutional information and graduate degree programs anticipated for 2013-14. http://www.aacp.org/resources/student/pharmacyforyou/admissions/Documents/Table%203.pdf. Accessed November 30, 2012. [Google Scholar]
- 17.Krathwohl DR. A revision of Bloom’s Taxonomy: An overview. Theory Into Practice. 2002;41(4):212–218. [Google Scholar]
- 18.Burke JM, Miller WA, Spencer AP, et al. Clinical pharmacist competencies. Pharmacotherapy. 2008;28(6):806–815. doi: 10.1592/phco.28.6.806. [DOI] [PubMed] [Google Scholar]
- 19.Brown D, Ferrill M, Hinton A, Shek A. Self-directed professional development: the pursuit of affective learning. Am J Pharm Educ. 2001;65(3):240–247. [Google Scholar]