Abstract
Objective. To measure the impact of a depression training day for pharmacists that included a 75-minute session with a consumer educator.
Design. The training day included interactive lectures on depression; the effects and side effects of and indications for the use of antidepressants; adherence issues; non-drug treatment options for depression; and basic skills in communication. Pharmacists also participated in a session with a consumer educator and in counseling exercises that included role playing.
Assessment. The study used a randomized, clustered, comparative design to measure pharmacists' stigma, attitudes, and current practice related to the provision of pharmaceutical care to people with depression. Mean scores for depression-care practice after the training session were significantly higher in the intervention group than in the control group. Analysis of the changes between baseline and postintervention measures in both the control and intervention groups confirmed a significant difference in the change in both social distance and practice but no significant difference in the change in attitude between the 2 groups of pharmacists.
Conclusion. A continuing-education depression training day for pharmacists that involve consumer educators may improve the care delivered in the community pharmacy to people with depression.
Keywords: community pharmacy, consumer educator, depression, pharmaceutical care, stigma, attitude
INTRODUCTION
In the last 20 years, community pharmacists’ roles have evolved worldwide. The pharmacy profession and pharmacy education have undergone significant change and renewal. In many countries, the orientation of the pharmacist has shifted from being product-to-patient-focused: attention is now centered on the pharmaceutical needs of the patient rather than the traditional tasks associated with dispensing medications. These patient-focused activities have evolved into the concept of “pharmaceutical care.”1 In relation to mental health, this change and renewal is still ongoing. Pilot projects have shown that pharmacists have the potential to improve the quality of mental healthcare and outcomes by enhancing adherence, adjusting medications, and monitoring and managing adverse effects.2 Among people undergoing antidepressant therapy, treatment monitoring is known to improve patient satisfaction with and adherence to medication therapy.3-6 Specifically, antidepressant telemonitoring by community pharmacists improves the level of patient feedback to pharmacists and enhances the pharmacist-patient collaboration.7,8 In Belgium, the impact of pharmacists’ involvement in the provision of depression care has not been thoroughly investigated, although between 2002 and 2010, the number of daily doses of antidepressants dispensed in community pharmacy continued to grow from 171 to 272 million. More than half of the antidepressant prescriptions in 2010 were for selective serotonin reuptake inhibitors (59%), while atypical antidepressants accounted for 35%, tricyclic antidepressants for less than 6%, and monoamine oxidase inhibitors for only 0.1%.9
Community pharmacists and their services are mostly perceived as positive by people with mental illness.10 Nonetheless, 1 in 4 persons with mental illness experienced discomfort and stigma at community pharmacies. Likewise, a study showed that community pharmacists have stigmatizing attitudes toward patients with depression.11 There are significant differences among professional groups in attitude toward mentally ill people, with psychologists holding the most positive attitudes, psychiatrists having the most negative attitudes, and nurses and other therapists falling somewhere in between.12 Further, the current practice of pharmacists for people with depression is significantly different from that for people with physical illnesses.13,14 Pharmacists who lack self-efficacy may provide less care for people with depression than for other people and may avoid involvement in depression care, as they do not believe they are capable of performing a role in caring for depressed individuals. 13
Lack of mental health pharmacy education has been described as the main barrier to successful provision of pharmaceutical care for people with depression.14 Therefore, it has been questioned whether the education provided at European universities adequately prepares pharmacists to provide mental healthcare services.15 Further education for pharmacists on mental health in general is called for,16,17 and on depression specifically.14,18,19 Advanced mental health education has the potential to improve US pharmacy students’ perspectives on mental illness.20 Education and training may increase pharmacists’ self-efficacy and, thereby, the likelihood of better pharmaceutical care for people with depression.13 However, the literature on the impact of pharmacy education for depression is scarce, especially in continuing education.
Since the World Health Organization recognized people with mental illness as key stakeholders in the development of mental health education for providers, there has been growing support for consumer participation in training programs for professionals.21 A consumer educator in mental health care is defined in the literature as a person who has previously received mental health care and works, often on a voluntary basis, to inform and educate professionals, students, and the wider community on mental illness and its effects on individuals, families, and society.22,23 The use of mental health consumers as educators has been well received in nursing and medical education, especially in Australia.24 A study demonstrating the potential value of consumer educators in the education of community pharmacists stated that use of consumer educators should be considered as a strategy for improving the confidence and communication skills of community pharmacists in providing pharmaceutical care for people with mental illnesses such as depression.23,25 Meanwhile, several studies demonstrated that using consumer educators for pharmacy students reduced mental health stigma,17,26 improved attitudes, and increased students’ self-reported sense of empathy toward people with schizophrenia and depression, even on a long-term basis.22 However, these studies have reported the impact of consumer educators only in undergraduate training. To our knowledge, there is no published research on the impact of consumer educators in continuing education and in the daily practice of experienced pharmacists.
The authors hypothesized that attending a depression training day for pharmacists would have a positive effect on pharmaceutical care of patients with depression. This paper describes the development of a training day and a comprehensive pre- and postintervention survey to assess the impact on pharmacists.
DESIGN
We measured the impact of a depression training day for pharmacists, which included a 75-minute session with a consumer educator, on (1) stigma toward people with depression, (2) depression care attitudes, and (3) depression care practice. This study was part of a larger study on the impact of medication counseling by community pharmacists for patients starting treatment with antidepressant drugs. Approval was obtained from the Ethics Committee of the University Hospital Leuven/KU Leuven. The research was performed within the Surplus Network, 1 of the largest pharmacy chains in Flanders, Belgium, which includes 97 pharmacies and employs 181 pharmacists, from all 5 Flemish provinces, including Brussels.
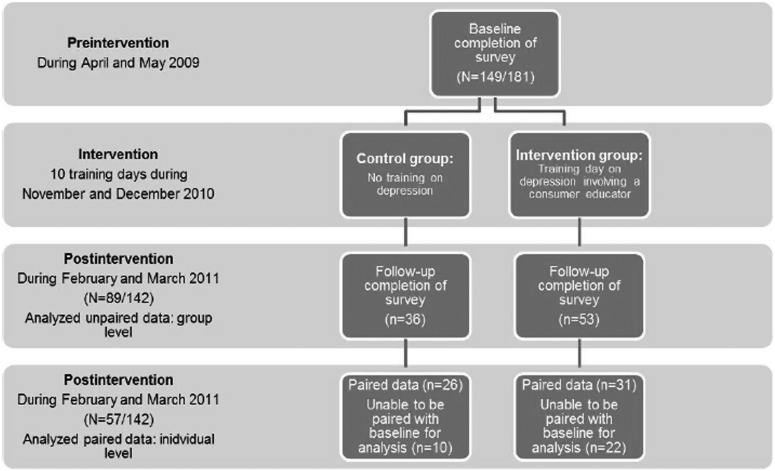
The study used a 2-group, randomized, clustered, comparative design, with 1 group of pharmacists allocated to receive no training (control group) and another group to receive 1 day of training on depression (intervention group) (Figure 1). All pharmacists attending obligatory regional meetings of the Surplus Network during April and May 2009 were asked to complete and return a survey instrument (baseline measurement) at the end of the meeting. The interactive training day on depression for pharmacists of the intervention group was held between November and December 2010. Seventy-one pharmacists were trained in groups of no more than 10 participants each. The content of the first part of the training, provided by a coauthor and lecturer in pharmacotherapy/pharmaceutical care at KU Leuven, covered depression in a broad sense, with a focus on the indications for the use of antidepressants, pharmacotherapy, causes of depression based on the Bio-Psycho-Social model,27 effects and side effects of antidepressants, and adherence issues explained by the Health Beliefs Model.28 Further, an introduction to psychotherapy was provided by one of the coauthors who is a clinical psychologist affiliated with the pharmacy department of KU Leuven, explaining the nondrug treatment options for depression and presenting a theoretical background on basic skills in communication.
Figure 1.
Outline of Study Design
During the second part of the training, pharmacists were divided into 2 groups, each with 1 consumer educator. Consumer educators had been taking antidepressants for at least 1 year and had previous experience with group exercises in medical training programs. The consumer educators gave an introduction about themselves and their history with depression and the antidepressants they were taking. Pharmacists had the opportunity to interview the consumer educators for 75 minutes, with a focus on medication counseling and personal experiences with depression and antidepressants. The third part of the training day focused on counseling people with a prescription of antidepressants in pharmacy practice, an exercise that involved practicing communication skills, aided by the use of pharmacy software. At the end of the training day, participants practiced new and repeated antidepressant prescription counseling through role-play with simulated patients in a training pharmacy. Feedback on their counseling and communication skills (including empathy) was provided by both trainers. In addition, participants had the opportunity to observe their colleagues in action through a 1-way screen and to learn from watching others.
EVALUATION AND ASSESSMENT
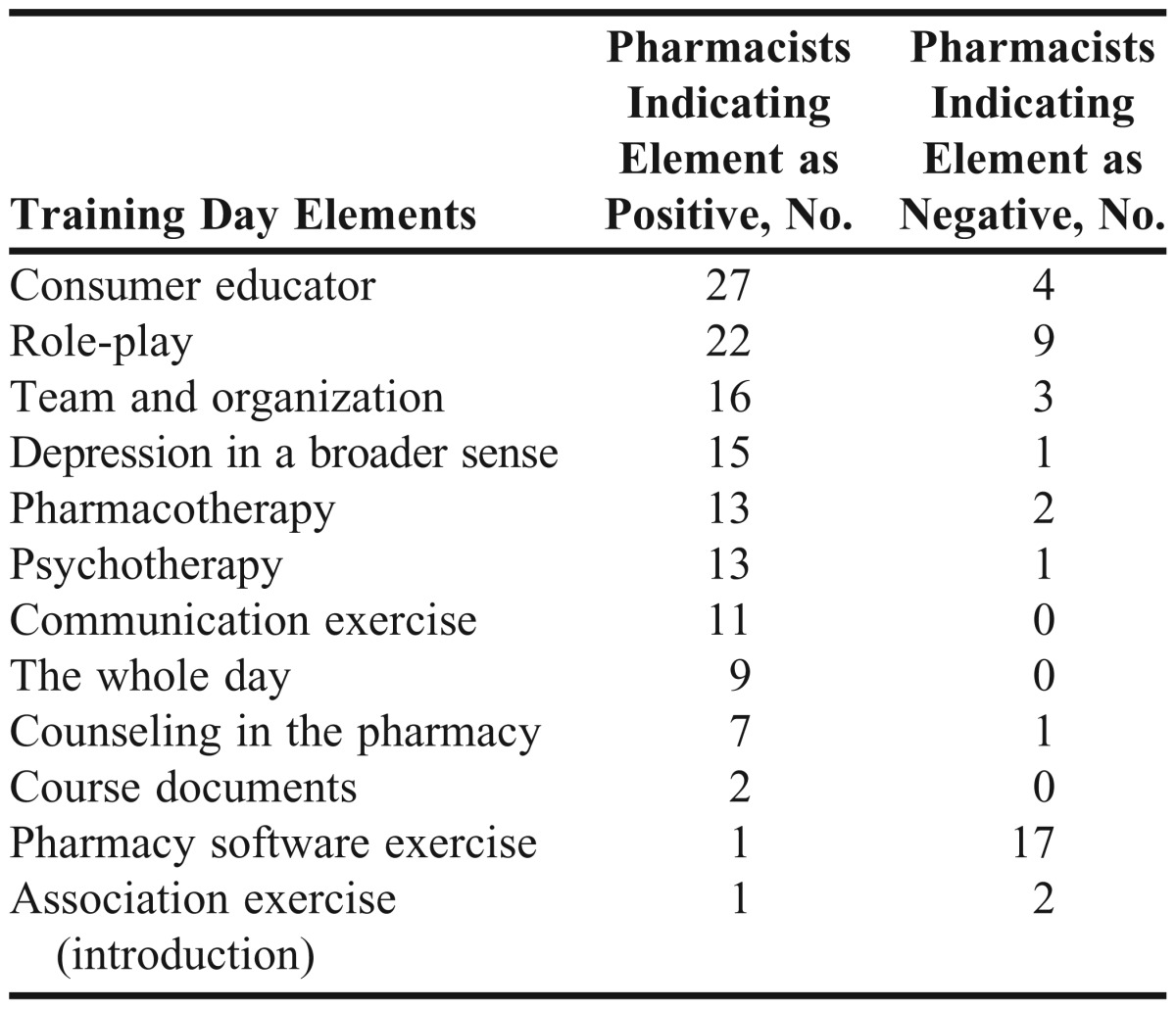
The positive and negative elements of the training session, as indicated by the participants of the intervention group at the conclusion of training, are listed in Table 1. The interview with the consumer educator was evaluated most favorably (n=27), followed by role-play (n=22), and appreciation for the team and overall organization (n=16). The exercise with pharmacy software was perceived as the most negative element of the training day (n=17), as demonstrated by participants perceiving the exercise as redundant and unnecessary. Role-play was also perceived as a negative element (N=9), as participants reported that this exercise made them feel uncomfortable and insecure in front of their colleagues.
Table 1.
Positive and Negative Elements of the Depression Care Training Day (N= 51)
Survey Instrument
The survey instrument consisted of 3 different previously tested and validated scales,11,13 which were used to explore pharmacists’ stigma toward people with depression, current practice, and attitudes toward pharmaceutical care for people with depression.
Stigma was measured by the Social Distance Scale for Depression, which asks respondents to indicate their willingness to engage in relationships of varying intimacy with a person previously hospitalized for depression. All 7 items are rated on a 4-point Likert scale ranging from 1 (definitely willing) to 4 (definitely unwilling), with lower scores indicating less social distance and higher scores indicating more social distance. Items on the Depression Care Practice and Attitude Scales were based on previous research,14 which delineated a set of 9 potential roles in pharmaceutical care for patients with depression. By splitting up the role “follow-up symptoms and side effects” into follow-up symptoms and follow-up side effects, 10 items were generated for the current research. Other potential roles in depression care covered in this study included maintain a trusting relationship, know the patient’s medication history, provide information on condition, provide information on medication, follow-up medication adherence, provide support and listen to the patient, advise the patient to consult a doctor when you recognize symptoms, and advise the patient to consult a doctor when symptoms worsen. Asking participants, “to what extent do you agree you should provide…,” these 10 roles served as attitude items about depression, rated on a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The same 10 roles were then used as current practice assessment, which asked participants “to what degree do you currently provide…” These practice items were rated on a 4-point Likert scale, ranging from 1 (I provide … to no patients) to 4 (I provide … to all patients).
Demographic information was collected from each pharmacist, including age, gender, years of pharmacy experience, personal experience with depression, and frequency of contact with depressed people in pharmacy practice. At the end of the training day, participants were also asked to identify in writing the highlights of the experience as well as the negative and less-useful elements.
Preintervention and Postintervention Surveys
Pharmacists who attended the meetings of the Surplus Network where the baseline measurement was taken had the option to complete or refuse to complete the survey instrument. Confidentiality was secured by asking participants to use a unique identifier based on day and month of birth and the last 3 numbers of their identification number in the national register.
During the baseline measurement, 149 survey instruments were returned (response rate of 82%). Respondents were a mean age of 43.3 ± 10.8 years and had been in practice for 17.0 ± 10.3 years. This sample was considered representative of the population of Flemish pharmacists (N=11,713), 72.6% (N=8503) of whom were female (p=0.406), with 19.3 ± 11.3 years of experience (p=0.010) (personal communication, Pharmaceutical Chamber, Brussels, Belgium, October 2010).
Seven to 11 weeks after the training session was conducted, 141 pharmacists were contacted by mail and asked to participate in a post-intervention survey. Only chief pharmacists and adjunct pharmacists were invited to participate; pharmacists working at more than 1 site were excluded. Of the 141 pharmacists invited, 89 (63%) responded, 40% (n=36) from the control group and 60% (n=53) from the intervention group.
Data were analyzed using the Statistical Package for the Social Sciences, version 17.1 (SPSS, Inc, Chicago). Individual pharmacists’ responses were matched across the 2 time points of the study using unique identifiers. Total scale scores were calculated by summing the individual responses for each item. To verify the assumptions for normal distribution of the data, normality tests (Kolmogorov-Smirnov and Shapiro-Wilk tests) were carried out. Normality of the data was assumed when p>0.05 or when the histograms showed a symmetric distribution of the data, the data points in the Normal Q-Q plot showed a straight line, and no systematic pattern in the Detrended Normal Q-Q plot was observed.
Independent samples t tests were used to compare age, years of experience, and the different total postintervention scale scores (n=89) between the intervention and control groups. For categorical data (gender, personal experience with depression), Pearson chi-square tests were used; however, when more than 20% of the cells had expected counts of less than 5, Fisher exact tests were used. For the data on pharmacists who had unique identifiers that matched for the 2 time points (ie, baseline and postintervention) (n=57), paired samples t tests and 1-way ANOVA on the difference in change between the 2 time points were carried out for the total scale scores. Positive and negative elements of the training day, as reported by the pharmacists, were coded and grouped into categories.
The mean number of years of experience in the intervention group (19.6 ± 11.5) was not significantly different from that in the control group (18.4 ± 10.2) (p=0.611). Likewise, the mean age of pharmacists in the intervention group (45.0 ± 11.3) was not significantly different from that in the control group (43.0 ± 10.3) (p=0.404). There was no significant relationship between gender (p=0.205) or frequency of contact with people with depression in the community pharmacy (p=0.877) between pharmacists in the intervention and control groups, and no significant relationship (p=0.509) between personal experience with depression (“I have suffered from depression myself”) and group. Likewise there was no significant relationship (p=0.158) between personal experience (“My close family or friends suffered from depression”) and group. The mean social distance toward people with depression in the intervention group (16.8 ± 3.8) was lower than that in the control group (18.5 ± 4.4), although this difference was not significant (p=0.059).
In the intervention group, the mean social distance toward people with depression was significantly lower at postintervention (16.5 ± 3.3) than at baseline (17.9 ± 4.4) (p=0.048). This finding is in contrast to the control group, in which the mean social distance toward people with depression was not significantly different at baseline (17.4 ± 4.6) and postintervention (18.4 ± 4.8) (p=0.310). One-way ANOVA analysis between control and intervention group on the difference in change in social distance at baseline and postintervention confirmed these significant results (p=0.045).
At postintervention, the mean depression care attitude in the intervention group (41.9 ± 4.2) was not significantly different from the mean depression care attitude in the control group (40.8 ± 4.2) (p=0.194). This finding was in contrast to the mean depression care practice score, which, at postintervention, was significantly higher in the intervention group (27.7 ± 4.5) than in the control group (23.2 ± 4.9) (p=0.000).
In the intervention group, the mean attitude was higher at postintervention (42.4 ± 3.6) than at baseline (41.2 ± 3.4), but this difference was not significant (p=0.118). In the control group, the mean attitude toward providing care for people with depression was significantly higher at postintervention (41.0 ± 4.2) than at baseline (39.2 ± 3.5) (p=0.005). However, 1-way ANOVA analysis shows no significant difference in attitude change between the control and intervention groups (p=0.537).
In the intervention group, the mean depression care practice at postintervention (30.9 ± 5.2) was significantly higher (p= 0.001) than at baseline (28.2 ± 4.0). In the control group, the mean depression care practice at baseline (26.0 ± 4.2) was not significantly different from the mean depression care at postintervention (25.4 ± 4.6) (p=0.307). There was a significant difference in depression care practice change at baseline and postintervention between the control and intervention groups (p=0.002).
DISCUSSION
After the training session, pharmacists in the intervention group preferred less social distance toward people with depression compared with pharmacists in the control group. Social distance can be considered as one of the most commonly used and reliable measures of stigmatization.29,30 The preferred social distance reflects an individual’s self-report on relative willingness to participate in different types of relationships of varying degrees of intimacy with a person who has a stigmatized identity.30-32 More specific data analysis of baseline and postintervention scores showed that pharmacists’ mean social distance decreased after a training day including a consumer educator. Further, the change in social distance at baseline and postintervention was significantly different between the intervention and control groups. These results are consistent with those of previous studies showing a decrease in pharmacy students’ preferred social distance after contact in an educational setting with consumer educators who have a mental illness. 17,22,26,33
We have previously shown that although most pharmacists have extensive professional experience with people who have depression as a result of seeing them in the pharmacy workplace at least weekly or even daily, most pharmacists endorse social distance.11 The current results provide further evidence that it is not the quantity but the quality and the type of contract with people with mental illness that influence stigma reduction.22,34,35 Previous research has shown that basic health education and experience alone are not sufficient to reduce stigma.35 Stigma reduction seems to require the full experience of relating to a person with mental illness who embodies the hope of recovering and living a full life. Such an experience can result in the personal, affective ingredients for stimulating empathy and connection.36 Therefore, we believe that including sessions with consumer educators in training sessions has the potential to change stigma among future pharmacists. As reducing stigma is considered one of the most important elements in improving mental health,30 including consumer educators may be one of the best options to enhance patient-pharmacist contacts and, hence, to make a positive difference on the level of patient care.
There was no significant difference in attitude toward providing depression care between the intervention and control groups. There was no significant difference in change in depression care attitude at baseline compared with postintervention. However, pharmacists’ attitudes significantly differed at baseline compared with postintervention. In the intervention group, the pharmacists’ attitude was also more positive at postintervention compared with baseline, but this difference could not be considered significant. These nonsignificant results might be attributable to a ceiling effect, as the pharmacists’ current scores could be considered close to the maximum score of 50. Previous results revealed pharmacists’ positive attitude toward their role in depression care,13 even without training. Hence, the training was not able to significantly improve the already-positive attitude of pharmacists toward depression care.
The mean depression care practice at postintervention was significantly higher in the group of pharmacists who received training compared to those who did not. Pharmacists in the intervention group reported providing more depression care after the training day. The pharmacists who did not receive training showed no difference in reported depression care between baseline and postintervention measurements. Further, there was a significant difference in practice change between the groups from baseline to postintervention measures. These findings suggest that a depression training day including a 75-minute session with a consumer educator might improve the care delivered in the community pharmacy to people with depression. Therefore, colleges and schools of pharmacy as well as providers of continuing pharmacy education should not hesitate to redesign the curriculum and to include intensive training on mental health, as this will provide future pharmacists the knowledge and skills to take up their role in mental health care and bridge the gap between positive attitude and daily practice.
The current study investigated the impact of a depression training day, involving a consumer educator, on different outcomes in a group of experienced community pharmacists. Previous studies in this area have investigated the impact solely on students.17,22,26 Further, the current study was the first to explore the impact on pharmacists’ current depression care practice. One of the limitations of the study that should be taken into account when interpreting the results is that the survey responses were self-reported. Moreover, the current study did not contain direct measures of actual practice. In order to appear as a caring and good pharmacist, respondents might have denied negative attitudes and bad practice and answered in a socially desirable way. Therefore, the results might underestimate the extent of bad practice and negative attitudes toward depression care. Nonetheless, the results showed a difference between the intervention and the control groups regarding stigma and current practice. Additional limitations include the small sample size, the lower response rate of 63% at postintervention compared with 80% at baseline, and the inability to evaluate distinct effects from individual aspects of the intervention. Future research could study the impact of single aspects of the training, such as consumer educators, on different levels of education (including the doctor of pharmacy curriculum), and areas of pharmacy practice.
CONCLUSION
A depression training day including a 75-minute session with a consumer educator is an effective strategy to decrease community pharmacists’ stigma toward people with depression and increases their self-reported depression care practice. As community pharmacists encounter people with depression daily, advanced training in mental health care is essential in preparing pharmacists to provide pharmaceutical care for this population.
ACKNOWLEDGMENTS
The authors thank Marijn Wouters (PharmD) and Chantal Leirs (PharmD) for sampling of the baseline data, Piet Van Maercke (PharmD) of the Pharmaceutical Chamber for providing data on the population of Flemish pharmacists, and pharmacists of the Surplus Network for participating in the study. We greatly appreciate the input from Dr. Gert Scheerder and Prof. Dr. Chantal Van Audenhove in constructing the survey instrument, from Dr. Franciska Desplenter in comparing data from the study population with those of the total population of Flemish pharmacists, and from the Scientific Information Center of Escapo C.V. in conducting the study.
REFERENCES
- 1.Anderson S. The state of the world's pharmacy: a portrait of the pharmacy profession. J Interprof Care. 2002;16(4):391–404. doi: 10.1080/1356182021000008337. [DOI] [PubMed] [Google Scholar]
- 2.Capoccia KL, Boudreau DM, Blough DK, et al. Randomized trial of pharmacist interventions to improve depression care and outcomes in primary care. Am J Health-Syst Pharm. 2004;61(4):364–372. doi: 10.1093/ajhp/61.4.364. [DOI] [PubMed] [Google Scholar]
- 3.Bultman DC, Svarstad BL. Effects of pharmacist monitoring on patient satisfaction with antidepressant medication therapy. J Am Pharm Assoc. 2002;42(1):36–43. doi: 10.1331/108658002763538053. [DOI] [PubMed] [Google Scholar]
- 4.Bell S, McLachlan AJ, Aslani P, Whitehead P, Chen TF. Community pharmacy services to optimise the use of medications for mental illness: a systematic review. Aust New Zealand Health Policy. 2005;2:29. doi: 10.1186/1743-8462-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crockett J, Taylor S, Grabham A, Stanford P. Patient outcomes following an intervention involving community pharmacists in the management of depression. Aust J Rural Health. 2006;14(6):263–269. doi: 10.1111/j.1440-1584.2006.00827.x. [DOI] [PubMed] [Google Scholar]
- 6.George PP, Molina JA, Cheah J, Chan SC, Lim BP. The evolving role of the community pharmacist in chronic disease management - a literature review. Ann Acad Med Singapore. 2010;39(11):861–867. [PubMed] [Google Scholar]
- 7.Rickles NM, Svarstad BL, Statz-Paynter JL, Taylor LV, Kobak KA. Pharmacist telemonitoring of antidepressant use: effects on pharmacist-patient collaboration. J Am Pharm Assoc. 2005;45(3):344–353. doi: 10.1331/1544345054003732. [DOI] [PubMed] [Google Scholar]
- 8.Rickles NM, Svarstad BL, Statz-Paynter JL, Taylor LV, Kobak KA. Improving patient feedback about and outcomes with antidepressant treatment: a study in eight community pharmacies. J Am Pharm Assoc. 2006;46(1):25–32. doi: 10.1331/154434506775268715. [DOI] [PubMed] [Google Scholar]
- 9.RIZIV/INAMI. Pharmaceutical Statistics, Pharmaceutical Service, Ambulatory Care 2010. Brussels: RIZIV/INAMI, 2012. http://www.riziv.fgov.be/drug/nl/statistics-scientific-information/pharmanet/pharmaceutical-tables/index.htm. Accessed February 4, 2013. [Google Scholar]
- 10.Black E, Murphy AL, Gardner DM. Community pharmacist services for people with mental illnesses: preferences, satisfaction, and stigma. Psychiatr Serv. 2009;60(8):1123–1127. doi: 10.1176/ps.2009.60.8.1123. [DOI] [PubMed] [Google Scholar]
- 11.Liekens S, Smits T, Laekeman G, Foulon V. Factors determining social distance toward people with depression among community pharmacists. Eur Psychiatry. 2012;27(7):528–535. doi: 10.1016/j.eurpsy.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Lauber C, Nordt C, Braunschweig C, Rossler W. Do mental health professionals stigmatize their patients? Acta Psychiatr Scand Suppl. 2006;429:51–59. doi: 10.1111/j.1600-0447.2005.00718.x. [DOI] [PubMed] [Google Scholar]
- 13.Liekens S, Smits T, Laekeman G, Foulon V. Pharmaceutical care for people with depression: Belgian pharmacists' attitudes and perceived barriers. Int J Clin Pharm. 2012;34(3):452–459. doi: 10.1007/s11096-012-9628-0. [DOI] [PubMed] [Google Scholar]
- 14.Scheerder G, De Coster I, Van Audenhove C. Pharmacists' role in depression care: a survey of attitudes, current practices, and barriers. Psychiatr Serv. 2008;59(10):1155–1160. doi: 10.1176/ps.2008.59.10.1155. [DOI] [PubMed] [Google Scholar]
- 15.Koski I, Heikkila A, Bell JS. Mental health pharmacy education at 16 European universities. Am J Pharm Educ. 2009;73(8):Article 139. [PMC free article] [PubMed] [Google Scholar]
- 16.Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55(12):1434–1436. doi: 10.1176/appi.ps.55.12.1434. [DOI] [PubMed] [Google Scholar]
- 17.Bell JS, Johns R, Rose G, Chen TF. A comparative study of consumer participation in mental health pharmacy education. Ann Pharmacother. 2006;40(10):1759–1765. doi: 10.1345/aph.1H163. [DOI] [PubMed] [Google Scholar]
- 18.Scheerder G, De Coster I, Van Audenhove C. Community pharmacists' attitude toward depression: a pilot study. Res Social Adm Pharm. 2009;5(3):242–252. doi: 10.1016/j.sapharm.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Crockett J, Taylor S. Rural pharmacist perceptions of a project assessing their role in the management of depression. Aust J Rural Health. 2009;17(5):236–243. doi: 10.1111/j.1440-1584.2009.01084.x. [DOI] [PubMed] [Google Scholar]
- 20.Gable KN, Muhlstadt KL, Celio MA. A mental health elective to improve pharmacy students' perspectives on mental illness. Am J Pharm Educ. 2011;75(2):Article 34. doi: 10.5688/ajpe75234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. Advocacy for mental health. Geneva: 2003. http://www.who.int/mental_health/resources/en/Advocacy.pdf. Accessed August 14, 2012. [Google Scholar]
- 22.O'Reilly CL, Bell JS, Chen TF. Consumer-led mental health education for pharmacy students. Am J Pharm Educ. 2010;74(9):Article 167. doi: 10.5688/aj7409167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell JS, Whitehead P, Aslani P, Sacker S, Chen TF. Design and implementation of an educational partnership between community pharmacists and consumer educators in mental health care. Am J Pharm Educ. 2006;70(2):Article 28. doi: 10.5688/aj700228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Happell B, Pinikahana J, Roper C. Attitudes of postgraduate nursing students towards consumer participation in mental health services and the role of the consumer academic. Int J Ment Health Nurs. 2002;11(4):240–250. doi: 10.1046/j.1440-0979.2002.00255.x. [DOI] [PubMed] [Google Scholar]
- 25.Bell JS, Whitehead P, Aslani P, Sacker S, Chen TF. Design and implementation of an educational partnership between community pharmacists and consumer educators in mental health care. Am J Pharm Educ. 2006;70(2):Article 28. doi: 10.5688/aj700228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buhler AV, Karimi RM. Peer-level patient presenters decrease pharmacy students' social distance from patients with schizophrenia and clinical depression. Am J Pharm Educ. 2008;72(5):Article 106. doi: 10.5688/aj7205106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schotte CK, Van Den Bossche B, De DD, Claes S, Cosyns P. A biopsychosocial model as a guide for psychoeducation and treatment of depression. Depress Anxiety. 2006;23(5):312–324. doi: 10.1002/da.20177. [DOI] [PubMed] [Google Scholar]
- 28.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 29.Jorm AF, Oh E. Desire for social distance from people with mental disorders. Aust N Z J Psychiatry. 2009;43(3):183–200. doi: 10.1080/00048670802653349. [DOI] [PubMed] [Google Scholar]
- 30.Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophr Bull. 2004;30(3):511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- 31.Bowman JT. Attitudes toward disabled persons: social distance and work competence. J Rehabil. 1987;53:41–44. [Google Scholar]
- 32.Corrigan PW, Edwards AB, Green A, Diwan SL, Penn DL. Prejudice, social distance, and familiarity with mental illness. Schizophr Bull. 2001;27(2):219–225. doi: 10.1093/oxfordjournals.schbul.a006868. [DOI] [PubMed] [Google Scholar]
- 33.Dipaula BA, Qian J, Mehdizadegan N, Simoni-Wastila L. An elective psychiatric course to reduce pharmacy students' social distance toward people with severe mental illness. Am J Pharm Educ. 2011;75(4):Article 72. doi: 10.5688/ajpe75472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Couture SM, Penn DL. Interpersonal contact and the stigma of mental illness: a review of the literature. J Ment Health. 2003;12(3):291–305. [Google Scholar]
- 35.Sadow D, Ryder M. Reducing stigmatizing attitudes held by future health professionals: the person is the message. Psychol Serv. 2008;5(4):362–372. [Google Scholar]
- 36.Sadow D, Ryder M, Webster D. Is education of health professionals encouraging stigmatowards the mentally ill? J Ment Health. 2002;11(6):657–665. [Google Scholar]