Abstract
Objective. To describe the development of an integrated pain and palliative care course and to investigate the long-term effectiveness of the course during doctor of pharmacy (PharmD) students’ advanced pharmacy practice experiences (APPEs) and in their practice after graduation.
Design. Roseman University College of Pharmacy faculty developed a 3-week elective course in pain and palliative care by integrating relevant clinical and pharmaceutical sciences. Instructional strategies included lectures, team and individual activities, case studies, and student presentations.
Assessment. Students who participated in the course in 2010 and 2011 were surveyed anonymously to gain their perception about the class as well as the utility of the course during their APPEs and in their everyday practice. Traditional and nontraditional assessment of students confirmed that the learning outcomes objectives were achieved.
Conclusions. Students taking the integrated course on pain management and palliative care achieved mastery of the learning outcome objectives. Surveys of students and practicing pharmacists who completed the course showed that the learning experience as well as retention was improved with the integrated mode of teaching. Integrating basic and clinical sciences in therapeutic courses is an effective learning strategy.
Keywords: curricular design, pain, palliative care, integrated course
INTRODUCTION
The practice of pharmacy demands that pharmacists have knowledge of and skills in applying basic science concepts to ensure sound, evidence-based decision making. However, the foundational role of the basic sciences in the PharmD program is often not completely appreciated by students. Because of this, colleges and schools of pharmacy are intent on developing pedagogies that will increase students’ awareness of the critically important relationships between basic science concepts and clinical application. In support of this goal, the Accreditation Council for Pharmacy Education states that curriculum be “…developed, with attention to sequencing and integration of content.”1 However, the traditional approach to teaching pharmacy education is often contrary to this goal in that basic science topics are generally separated from the clinical portion of the curriculum and vice versa. This lack of crosstalk results in students learning in “silos” that counter efforts to prepare them for contemporary, evidence-based pharmacy practice.2 Several organizations including the ACPE and the American Association of Colleges of Pharmacy (AACP) have recommended that basic and clinical sciences be integrated within the curriculum in an effort to enhance knowledge delivery and retention. There have been several reforms in healthcare education focused on defining novel mechanisms for training students in navigating the increasing complexity of patient care. Integration of the basic and clinical sciences into 1 course, although not novel, is one possible solution to this issue.
Basic pharmaceutical and clinical sciences are taught separately at Roseman University of Health Sciences College of Pharmacy (RUCOP), just as they are at the majority of US colleges and schools of pharmacy. Considering the in-house availability of faculty expertise in the basic and clinical aspects of pain management and palliative care, these topics were identified as ideal for developing into an integrated elective course. Also, pain management and palliative care are topics commonly encountered in pharmacy practice. One of the most common reasons for patients to seek medical help is pain. According to an Institute of Medicine report, more adult patients experience chronic pain than the number of adults with heart disease, diabetes, and all cancers combined.3 Pain is also a common problem that pharmacists encounter in their practice on a day-to-day basis, irrespective of practice setting. The topic of pain management is complex, mainly because of the complex and varied pathophysiology of different pain conditions. In addition to pain, palliative care is often not sufficiently included as a curricular topic in colleges and schools of pharmacy.4 Pharmacists and student pharmacists are likely to encounter patients with hospice and palliative care needs because of the large growth of patients receiving hospice and palliative care services. From 2000-2008, the number of palliative care programs in hospitals with 50 beds or more grew from 24.5% to 58.5%.5 The number of hospice programs in the United States has grown from approximately 3,650 in 2004 to approximately 5,150 in 2010.6
The major goals of this study were to: (1) develop and implement an elective course focused on the need for increased education in pain and palliative care by healthcare providers as outlined in an Institute of Medicine report,3 (2) deliver a complex subject in an integrated manner to enhance learning and retention, (3) determine the perceptions of students on the delivery of curricular content in this integrated course, and (4) determine the effectiveness of this course longitudinally.
DESIGN
While basic sciences such as biochemistry, pharmacology, and pharmaceutics were taught in the first (P1) year of the college’s 3-year pharmacy curriculum, clinical sciences were taught in the second (P2) year. However, some of the clinical science topics such as pharmacy calculations, Top 200 drugs, etc, were taught in the P1 year in a longitudinal format. The integrated elective course in pain and palliative care was developed with the aim to introduce a new organization of educational content and to train students in the area of pain and palliative care, which would be crucial to their practice. Apart from this elective course, the pharmacy students attended standard lectures on pain in the neurology block of the curriculum but did not receive any education in palliative care. Pain pharmacology received 12 lecture hours of coverage in the P1 year and pain management received 12 hours of coverage in the P2 year.
Based on guidelines from the Pain Curricular Summit, 3 faculty members with expertise in pain and palliative care developed a 3-week curriculum that integrated relevant pharmaceutical and clinical sciences. The course was organized over approximately 6 months. During this time, key faculty members were identified, a block plan with learning outcomes was created and approved by the curriculum committee, and course materials were developed. The learning outcomes and course materials were developed after several discussions between basic science and clinical science faculty members about the appropriateness and relevance of these outcomes and materials in helping the students to understand pain pharmacotherapy, and necessary changes were made based on the discussions. Major course topics identified by the faculty members are discussed in detail in the course content section.
In the elective course, the first 18 hours were spent on teaching the pathophysiology of pain states, pain pharmacology, medicinal chemistry, and pain drug formulations and delivery. This was followed by 42 hours on the clinical aspects of pain management pertaining to pharmacy practice. Instructors collaborated before starting the course and during the course. In order to have a smooth transition between the basic science and clinical science topics, some of the basic science and clinical science faculty members observed each other’s lectures and activities. The Pain and Palliative Care elective course was first offered in the summer of 2010.
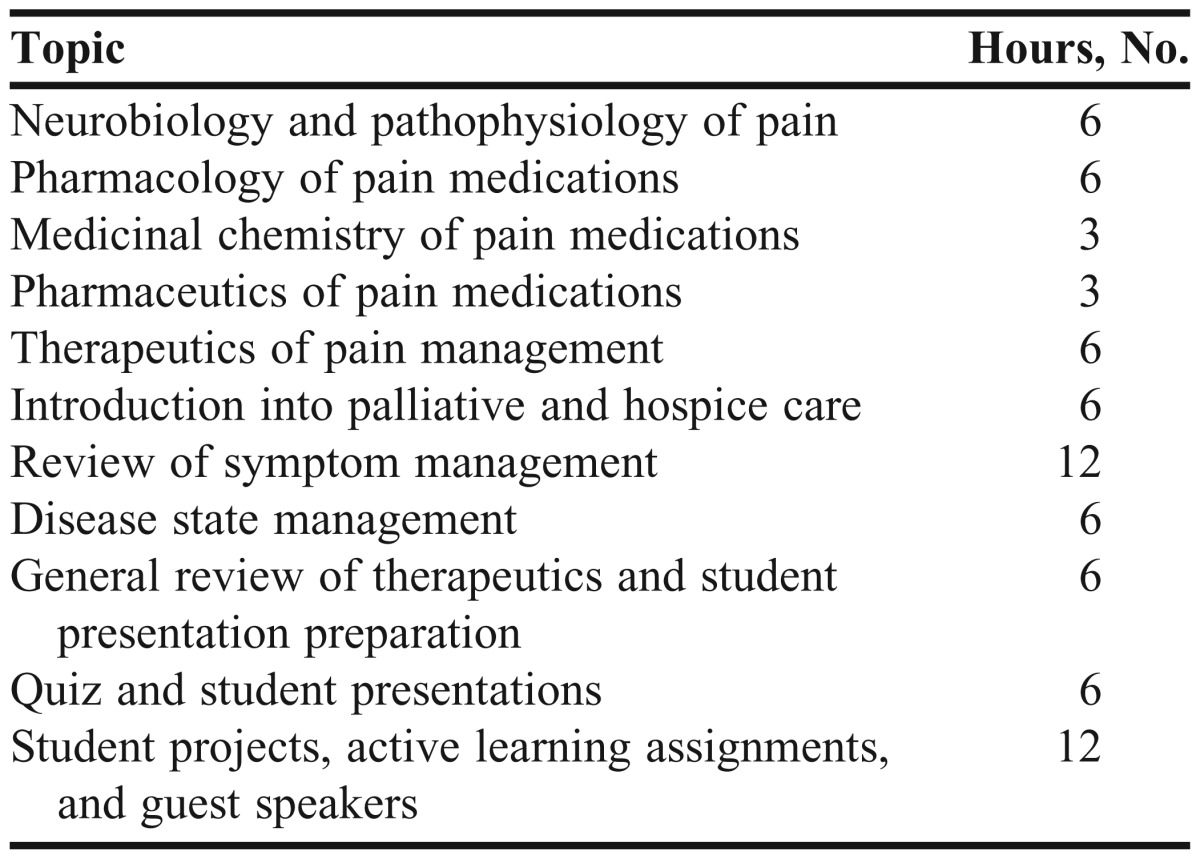
Learning outcomes for the elective course are listed in Appendix 1. After identifying the major course topics, the faculty members determined that the duration of the course would be 72 hours (4 credit hours), to be delivered over 3 weeks (Table 1). Instructional strategies used to deliver information included lectures, team and individual activities, case studies, and student presentations. In the basic science component, students were taught concepts and their relevance in understanding clinical aspects of pain management and palliative care. In the clinical science component, students were taught how to differentiate various pain and palliative care conditions and how to pharmacologically and nonpharmacologically manage these conditions from a pharmacist’s perspective.
Table 1.
Time Spent on Topics Taught in an Integrated Elective Course on Pain Management and Palliative Care
The elective course was offered at 2 of the college’s campuses: Henderson, Nevada, and South Jordan, Utah. To maximize interactions between faculty members and students, the course was initially capped at 30 students, but later changed to 20 students as a result of student feedback. Students were enrolled on a first come, first served basis. Prerequisites for the course included successful completion of the neurology therapeutics block and P3 status. Basic science topics were taught by faculty members with doctorate degrees in their respective fields, and the clinical topics were taught by faculty members who were clinical practitioners in their respective fields.
Course Content
Medicinal chemistry of pain medication. Learning outcomes for medicinal chemistry of pain medications were focused on 3 main classes of analgesic/anesthetic medications: opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. A review of medicinal chemistry textbooks (eg, Foye’s Principles of Medicinal Chemistry and Wilson and Gisvold’s Textbook of Organic, Medicinal and Pharmaceutical Chemistry) illustrated that these classes of drugs share a robust history of research, study, and clinical usage. These drug classes were specifically chosen because they are commonly prescribed and because they allowed discussion of several important medicinal chemistry topics. General topics presented with each drug class included drug design and development processes, general pharmacophore and structure-activity relationship (SAR) development, and structural concerns affecting side-effect profiles. Topics unique to each drug class were also presented, such as Portoghese’s message-address concept for opioid (and especially opiate) drugs, selectivity concerns for the inhibition of COX enzymes by nonsteroidal anti-inflammatory drugs (NSAIDs), and pharmacokinetic effects of amide vs ester local anesthetics.
Pharmaceutical perspectives on pain management. Having no textbook available on the pharmaceutical perspectives on pain management, the faculty members used pharmaceutical industry publications (eg, Drug Development & Delivery, Drug Development and Industrial Pharmacy) as well as drug-product prescribing information to prepare the lecture content. Lectures discussed and compared not only dosage form design principles and pharmacokinetics, but also their relationships with other factors such as types of pain, patient status, patient compliance, degree of opioid tolerance, risk of addiction, and cost. Potent μ opioids were chosen as the major example for teaching because a variety of opioid products are available and selection of one product over another can be confusing. In addition, discussions were held on the new developments in the pharmaceutical industry such as the innovative specialized opioid products (eg, novel pulmonary, transmucosal, and intranasal fentanyl products) that are used to improve the management of breakthrough cancer pain. During team activities, students were given clinical cases and asked to select appropriate routes of administration and drug products to demonstrate the importance and relevance of pharmaceutical and pharmacokinetic knowledge in pain management.
Pain neurobiology, pain pathophysiology, basic pharmacology of pain management. Based on topics in standard textbooks of pain (eg, Wall and Melzack Textbook of Pain), and pharmacology (Goodman and Gilman), the faculty members drafted outcomes on pain neurobiology, pathophysiology, and pharmacology that they thought would be relevant and useful to pharmacy students for understanding the pharmacotherapy of pain. The materials distributed during the Pain Curricular Summit, and the International Association for the Study of Pain Core Curriculum for Professional Education in Pain were also used in identifying appropriate learning outcomes. The major areas included were basic terminology in pain; classification of pain; basic neurobiology of pain; brief pathophysiology of various types of pain; drug targets based on pathophysiology in various pain conditions; classification of traditional and nontraditional analgesic agents and local anesthetics, their mechanisms of action, major drug interactions, and major adverse drug reactions. The various topics were presented in the class in the context of their application in pharmacotherapy, and the relevance of these topics in understanding pharmacotherapy of pain was always emphasized.
Pharmacotherapy of pain management and palliative care. Based upon various clinical guidelines and materials distributed during the Pain Curricular Summit, outcomes were drafted for pharmacotherapy related to pain and palliative care. The primary symptoms in addition to pain covered by the learning outcomes include dyspnea, terminal secretions, cough, agitation, and nausea and vomiting. Clinical guidelines considered included the most recent guidelines published for management of chronic malignant and nonmalignant pain, neuropathic pain, and palliative care. As clear and focused guidelines on symptom management for hospice care are not readily available, several tertiary resources (Oxford Textbook of Palliative Medicine, Palliative Medicine, Palliative Pharmacy Care) were used. Also, a physician board certified in palliative care and a hospice volunteer coordinator were invited to the class to talk about the practical aspects of pain management and palliative care.
EVALUATION AND ASSESSMENT
The effectiveness of the course curriculum was assessed using a 2-pronged approach: (1) assessing student achievement of learning outcomes using traditional and nontraditional assessment methods such as administering tests that contain multiple-choice questions, short-essay questions, and assigning SOAP notes and patient care plans; and (2) assessing long-term effectiveness of the course using longitudinal survey instruments among students.
Achievement of Learning Objectives
Students were assessed using various methods at different time points in the course including written and oral presentations, and mid-term and final examinations that included written and multiple-choice questions. The assessment questions were set to assess the student’s capability at various levels of Bloom’s taxonomy. For example, objective tests including selected response questions (multiple choice) and constructed response questions (fill-in-the-blank) were used to assess the “remember and understand” cognitive process domains. In addition to these, the students were required to write up a SOAP (subjective, objective, assessment, plan) note and then orally present the SOAP note on a given pain or palliative care patient case to one of the course faculty members. SOAP (subjective, objective, assessment, plan) notes mimic an essay style assessment and were used to assess the “apply, analyze, and evaluate” cognitive process domains. Finally, PowerPoint presentations were used to assess the “create” cognitive process domain.
Students also were assigned either a common hospice diagnosis or common hospice symptom and asked to give a 10-15 minute PowerPoint presentation of their assigned topic. A grading rubric developed by the clinical faculty was used to assess the SOAP note and presentations. The intent of the SOAP notes and PowerPoint presentations was to give the students an opportunity to practice looking up drug/disease information topics, develop presentations, and give verbal pharmacotherapy recommendations. The grading breakdown between basic science and clinical science was 40% and 60%, respectively. Basic science assessment consisted of multiple-choice questions and short-essay questions, both having approximately equal weight. Clinical science assessment consisted of 42% SOAP notes, 33% presentation, and 25% multiple-choice questions, fill-in-the-blanks, short answers, and opioid conversions.
Based on the university’s general curricular policy, students were required to obtain a cumulative 90% in assessments to receive a passing grade. Remediation assignments and assessments were offered to students who did not initially obtain the 90% standard.
Thirty-seven students completed the course during the 2010 and 2011 semesters. While writing the questions for the various student assessments, care was taken to tie the assessment questions and assignment objectives to the learning outcomes. About 80% of the students passed these on the first attempt. Eventually 100% of the students passed the course through the remediation process which is built into all RUCOP courses.
Long-term Effectiveness
Survey instruments were used to evaluate the long-term effectiveness of the integrated model of curricular content delivery (1) immediately after the course, (2) while students were completing their APPEs, (3) and a year after graduating from the PharmD program. Data were collected from both campuses (Nevada, Utah) for the years 2010 and 2011 using SurveyMonkey (SurveyMonkey Inc. Palo Alto, California). Thirty-seven students completed the course across the 2 summers and both campuses. The analyses involved using both years’ data because the same faculty members taught the material and there was no major change in the course material or learning outcomes. For the longitudinal survey instrument that was sent out a year after the students started practicing as pharmacists, the data is only from 2010, since the 2011 class was still completing their APPEs when data were collected for this study. Because no student identifying information was collected, the university’s institutional review board did not require that informed consent be obtained.
The survey instrument consisted of both closed-ended and open-ended questions. The questionnaire was developed based on the learning outcomes from the course as well as the input from faculty members. The questionnaire was tested for content validity by sending it out to all faculty members involved in teaching the course. One of the objectives of the questionnaires was to understand how students perceived the difference between traditional ways of teaching and the integrated approach to teaching used in the course. The open-ended questions allowed the students to express their opinions about the positive and negative aspects of the course in addition to the perceived value of the various team activities and assessment styles used in the classroom. The questionnaire sent to students enrolled in APPEs or who were practicing as pharmacists mainly focused on the applicability of the course material in practice and any retrospective comments they had about the course.
Descriptive analyses were carried out to determine the percentage of students who agreed to each of the statements in the survey instrument. A content analysis was carried out to determine emerging themes from response on open-ended items.
Of the 37 students who took the course, 27 responded to the open-ended section of the questionnaire (73% response rate) and 28 responded to the closed-ended section of the questionnaire (76% response rate) that were distributed immediately after the course. No demographic data on the students were collected. The survey instrument was sent to all 37 students who took the class while they were in their APPEs, and 25 responded (68% response rate). Survey instruments were sent out to 21 alumni, who took the course as a student and were practicing as pharmacists, and we received 11 responses (response rate = 52%).
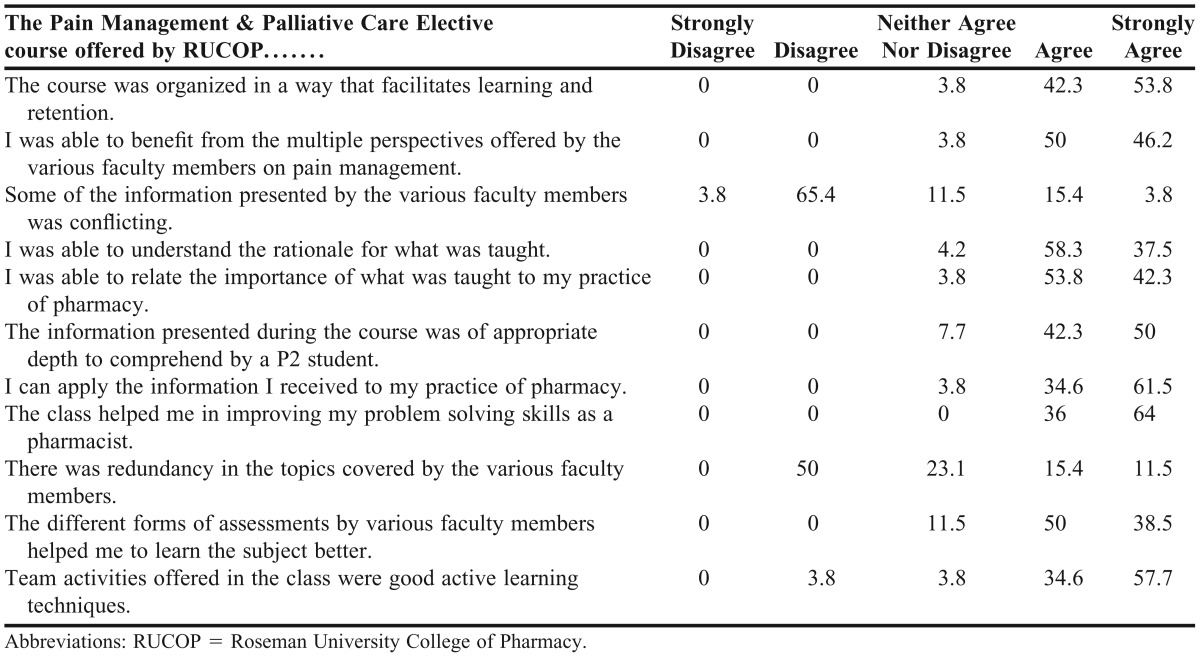
The students who completed the survey administered immediately after completing the elective course found it very or extremely relevant (78%), interesting (67%), practical (59%), necessary (52%), and informative (67%). While more than 60% of the respondents found the course to be very or extremely challenging; more than 90% found it very or slightly difficult and demanding, with more students responding “slightly” demanding. When asked to compare the traditional teaching approach with the integrated teaching approach, a large majority of the respondents either agreed or strongly agreed that the integrated course was better than the traditional approach to learning in terms of retaining information, application of basic sciences in clinical knowledge, the rational and logic of the course materials, and ability to solve problems from multiple domains (Table 2 and Table 3). When asked about the length of each course topic in the integrated course, more than 90% of respondents felt the length of the medicinal chemistry section was appropriate and around 80% of the respondents felt the length of the pharmaceutics section was appropriate. None of the respondents felt it was too long. While two-thirds of the respondents felt that the pharmacology section was the right length, the remainder was divided between feeling it was too long or too short. However, only about half of the respondents felt that the therapeutics section was the correct length. Forty-two percent felt not enough time was allotted for the course.
Table 2.
Pharmacy Students’ Comparison of the Integrated Course Model on Pain and Palliative Care With Traditional Ways of Teaching (N = 28), %
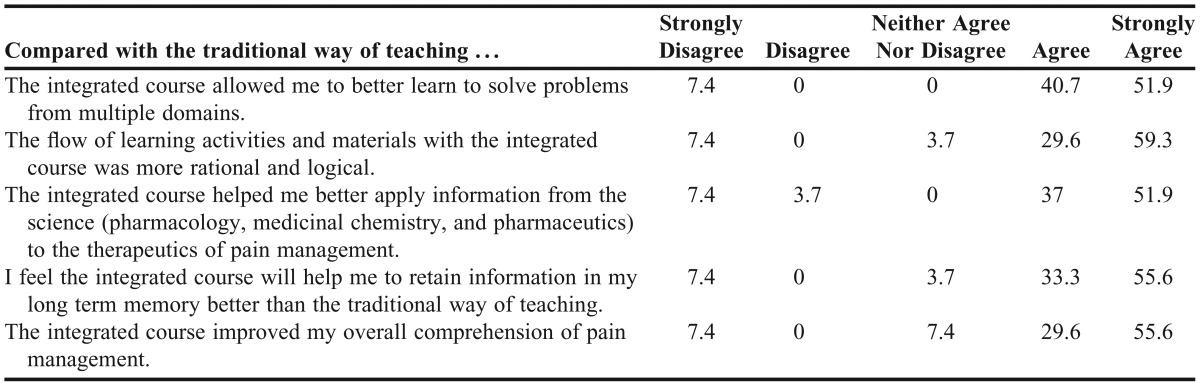
Table 3.
Student’s Perceptions About the Pain Management and Palliative Care Elective Course (N = 28), %
Students’ overall impressions of the course were positive. When asked to list 3 positive points about the course, the ones most frequently given were small class size, use of short answers for assessment, focus on learning rather than passing the assessment, and structure that allowed students to build on previously taught material. The small class size allowed students to have better interaction with faculty members such as asking questions. Students also liked the short-answer assessment style which allowed them to break away from the “memorization” strategy usually used to prepare for multiple-choice examinations. Another positive outcome noted by the students from the class was the Patient Care Plan at the end of the course. The comment “no need to memorize” was repeated. When asked about ways in which the course could be improved, the 2 dominating responses were the need for more patient cases and the need to better organize student presentations. When the students were asked to compare the integrated course with the traditional way in which the material had been taught (Basic Pharmaceutical Sciences in P1 year and Clinical Pharmacy in P2 year), their responses were in favor of the integrated style of teaching. The reasons provided by the students included slow pace in the class and small class size that allowed for better interaction, which in turn allowed the students to have better retention of the class material as well as the opportunity to learn along with the class. The other major reason was the “class to case” approach allowing them to apply the basic pharmaceutical concepts to clinical applications. When asked about the team activities offered in the class, the majority answered positively. The small size of the team was mentioned twice as the reason for the positive response. Those students who were not in favor of team activities wanted to work on the cases by themselves and then as a class with the faculty members. When asked about the different forms of assessments used by faculty members, the majority preferred the short-answer format, with a few students preferring the Patient Care Plan format. On asking about the topics that should be addressed in greater or lesser detail, a significantly repeating response could not be found. However, increasing the length of the course was repeated. When asked whether they would recommend this course to other students, 100% said they would.
Longitudinal Survey Results. Eighty-five percent of the respondents to the survey administered while they were completing their APPEs felt that the elective course prepared them well enough for their pain and palliative care practice experiences and more than 90% agreed that they would recommend the course to incoming students. More than 80% of respondents felt that they were able to recall the information they learned in the course when needed, improved their problem-solving skills as a pharmacist as a result of taking the course, were able to communicate with their preceptors about pain medications in a comfortable way, and felt confident about their knowledge of pain medications during their practice experiences. When asked whether the course helped them with their APPEs (n = 25), 84% of the respondents either agreed or strongly agreed.
All the respondents (n = 11) to the survey administered to practicing pharmacists (those who completed the elective course in 2010) felt that the class prepared them well enough for their pharmacy practice experiences and that they would recommend the course to incoming students. In addition, all the respondents felt that they could recall the information learned in the course when needed, that the course improved their problem-solving skills as a pharmacist, that they could communicate with their preceptors about pain medications in a comfortable way, and that they felt confident about their knowledge of the pain medications during their practice experiences. When asked how the course had helped them in their pharmacy practice, all of them agreed that the course had increased their confidence in providing counseling for pain medications.
DISCUSSION
One of the challenges often faced by health students is not understanding the relevance of basic sciences in their everyday clinical practice. The results from the study showed that integrating basic sciences and clinical sciences resulted in better learning outcomes and improved learning experience for students. The Accreditation Council for Pharmacy Education guidelines strongly recommend the need for integrating curricular content and reinforcement of curricular content by both basic science and pharmacy practice faculty members.1 In their article about addressing competencies for the future in the professional curriculum, Jungnickel and colleagues talk about integrating basic science activities into patient care to develop the skills needed for a pharmacist.7 In an editorial about “integrating basic sciences and clinical pharmacy,” Ratka points out how these 2 disciplines are intertwined and interdependent.8 The integrated style of delivering curricular content resulted in better retention of class materials than the traditional style of teaching. Some of the adjectives used by Ratka in her editorial about the integrated model were similar responses from the students in the open-ended questionnaire such as “better interaction with faculty,” “improves conceptual understanding,” and “clinical relevance to basic sciences.”
Basic science courses are usually taught in the first year of pharmacy school and students frequently complain about not being able to retain the information by the time they are learning clinical science. A study conducted at the University of Saskatchewan showed that there was considerable loss of basic science knowledge among first-year medical students by the end of the first year.9 In contrast, the results from this study showed that the course was beneficial and that the students retained knowledge better, even on a longitudinal basis. Information recall was not a problem for all the alumni who responded to the survey instrument, even a year after graduation. Thus, the integrated model of teaching will enable better retention of course materials as evidenced from this study. However almost half of the students wanted to increase the time allotted for the therapeutics section. Though we are not completely sure of their reasons, we can speculate that the students may not have perceived the importance of basic science in their everyday practice which in turn is related to the perception that therapeutics is more related to their daily functions in a pharmacy.
Stull and Carter promoted the integrated curriculum model in pharmacy as a way to encourage students to view various topics from the perspectives of different disciplines.10 They argued that this method would develop problem-solving skills in pharmacy students. A study on integrating basic sciences and clinical sciences within a medicinal chemistry course reported it was a positive experience for faculty members and students.11 Other studies have reported on integrating basic sciences and clinical pharmacy in teaching various pharmaceutics and pharmacotherapy courses.12-15 All of these studies reported that the integrated course model was a success not only in achieving the course outcome objectives, but also in improving the student’s perceptions about applying basic science principles in clinical pharmacy. The concept of teaching basic sciences and clinical courses concurrently and in an integrated manner has been successful in the medical and dental school curricula as well.16-24
There are several potential challenges to implementing an integrated pain and palliative care course. The first challenge is identifying pharmaceutical sciences and pharmacy practice faculty members with interest, experience, and expertise in pain and palliative care topics. Once faculty members are identified, coordination of schedules to communicate and develop course themes and learning outcomes can represent another challenge. Another potential challenge is the time requirement for developing such a course. Approximately 6 months was required to design this course, devoting many hours to content development. Through effective planning and communication, faculty members were able to overcome challenges to develop the integrated pain and palliative care course.
The study is not without limitations. Because the elective course was offered only in the summer, students who chose to take it were probably highly motivated to do so and already had a strong interest in pain management, which may have affected the positive responses on the questionnaires. Also, the class size was controlled to achieve better interaction among students and between students and faculty members, and the students who were not able to enroll in the class may have performed better or worse than those who took the course. Both of these conditions may have biased the study results. Also, apart from 2 alumni who described their work activities that related to the course, it is unknown whether others were involved in hospice and palliative care in their current positions. Though the students achieved mastery of learning as outlined by the school curriculum committee, the study did not objectively measure how students performed compared to when taught using traditional methods. Being a newly developed elective course, no comparison data were available.
SUMMARY
A new elective course, Pain Management and Palliative Care, was developed based on the integrated learning model, integrating basic pharmaceutical sciences and pharmacy practice. Traditional and nontraditional assessment of students confirmed that the learning outcomes objectives were achieved. Determining the perceptions of students regarding the usefulness of an integrated course model and the applicability of the course in practice proved that this model for delivering a pain management and palliative care module was successful.
ACKNOWLEDGEMENT
We would like to thank the following colleagues for their help in the development of the class and manuscript: Tyler Rose, Jin Zhang, Renee Coffman, and Gary Levin.
Appendix 1. Pain Neurobiology and Management Course Learning Outcomes
1. Describe epidemiology of pain in the US & appreciate pain as a public health problem.
2. Classify pain conditions according to different systems of classifications.
3. Define common terminologies in pain: Analgesia, Anesthesia, Allodynia, Dysesthesia, Hyperalgesia, Hypoalgesia, Hyperpathia, Paresthesia, and Causalgia.
4. Distinguish between acute pain and chronic pain.
5. Describe general pain pathways.
6. Explain how pain signals are transduced, transmitted, modulated and perceived.
7. List the common pain conditions.
8. Identify, assess and quantify pain in a clinical setting.
9. Describe the pathophysiology of various types of pain such as inflammatory pain, neuropathic pain, fibromyalgia, cancer pain.
10. Identify various possible drug targets based on pathophysiology in various pain conditions, and pain modulatory mechanisms.
11. Classify traditional and non-traditional analgesic agents, and local anesthetics (LAs).
12. Recall commonly used drugs in each class and facts associated with their R&D.
13. Identify members of each class based on their chemical structure.
14. Explain the structure-activity (SAR) relationships relevant to the pharmacodynamic properties of various opioid, NSAID, and LA drugs.
15. Explain the structure-activity (SAR) relationships relevant to the pharmacokinetics and toxicities of various opioid, NSAID, and LA drugs.
16. Explain the MOA, major adverse drug reactions, drug interactions of each of the analgesic class and LAs.
17. Describe the pathophysiology of addiction with emphasis on opioid addiction.
18. Compare and contrast the advantages and disadvantages of various routes of administration in pain management.
19. Differentiate pharmaceutical differences in oral opioid products and explain their pharmacotherapeutic differences in management of pain.
20. Understand the pharmacokinetic fundamentals of using methadone for pain management.
21. Understand the pharmaceutical and pharmacokinetic properties of fentanyl patch and compare the active and passive topical/transdermal systems for pain management.
22. Compare and contrast the various delivery technologies for breakthrough pain.
23. Compare and contrast different types of pain based upon patient information.
24. Evaluate a patient’s pain characteristics using the PQRST mnemonic device.
25. Calculate equianalgesic doses of opioids.
26. Select the most appropriate pain medication therapy based on specific patient data.
27. Distinguish a true allergic reaction from side effects caused by opioids based upon patient-specific information.
28. Recommend a treatment plan for side effects caused by opioids.
29. Develop an appropriate monitoring plan based on a specific medication therapy.
30. Compare and contrast advantages and disadvantages of methadone therapy.
31. Adjust a patient’s medication treatment plan based upon given information.
32. Identify the requirements for using patient controlled analgesia.
33. Recommend the most appropriate muscle relaxant for a patient.
34. Differentiate direct CNS administration of opioids from other routes of administration.
35. Classify analgesics according to Federal Controlled Substance Act of 1970.
36. State the regulations regarding prescription, storage and dispensing of controlled drugs.
REFERENCES
- 1.Accreditation Council for Pharmacy Education. Accreditation standard and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed January 8, 2013. [Google Scholar]
- 2.Yanchick VA. Multidisciplinary education: a challenge for pharmacy education. Am J Pharm Educ. 2004;68(3):Article 77. [Google Scholar]
- 3.Institute of Medicine of the National Academies. Relieving pain in America a blueprint for transforming prevention, care, education, and research. June 2011. http://www.iom.edu/∼/media/Files/Report%20Files/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research/Pain%20Research%202011%20Report%20Brief.pdf. Accessed September 18, 2012. [PubMed] [Google Scholar]
- 4.Herndon CM, Jackson K, 2nd, Fike DS, Woods T. End-of- life care education in United States pharmacy schools. Am J Hosp Palliat Care. 2003;20(5):340–344. doi: 10.1177/104990910302000507. [DOI] [PubMed] [Google Scholar]
- 5.Center to Advance Palliative Care. Making the case for hospital based palliative care. 2009. http://www.capc.org/building-a-hospital-based-palliative-care-program/case. Accessed September 18, 2012. [Google Scholar]
- 6.National Hospice and Palliative Care Organization. NHPCO Facts and Figures: Hospice Care in America. Alexandria, VA: 2011 Sept; http://www.nhpco.org/files/public/statistics_research/2011_facts_figures.pdf. Accessed September 18, 2012. [Google Scholar]
- 7.Jungnickel PW, Kelley KW, Hammer DP, Haines ST, Marlowe KF. Addressing competencies for the future in the professional curriculum. Am J Pharm Educ. 2009;73(8):Article 156. doi: 10.5688/aj7308156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ratka A. Integration as a paramount educational strategy in academic pharmacy. Am J Pharm Educ. 2012;76(2):Article 19. doi: 10.5688/ajpe76219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Eon MF. Knowledge loss of medical students on first year basic science courses at the University of Saskatchewan. BMC Med Educ. 2006;6(5) doi: 10.1186/1472-6920-6-5. doi:10.1186/1472-6920-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stull R, Carter RA. Integrating the pharmacy curriculum: more to consider than improving learning. Am J Pharm Educ. 2002;66(4):407–410. [Google Scholar]
- 11.Ives TJ, Deloatch KH, Ishaq KS. Integration of medicinal chemistry and pharmcotherapeutics courses: A case-based, learner-centered approach. Am J Pharm Educ. 1998;62(4):406–411. [Google Scholar]
- 12.Conway SE, Johnson JL, Ripley TL. Integration of team-based learning strategies into a cardiovascular module. Am J Pharm Educ. 2010;74(2):Article 35. doi: 10.5688/aj740235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stewart AL, Buckner IS, Wildfong PD. A shared assignment to integrate pharmaceutics and pharmacy practice course concepts. Am J Pharm Educ. 2011;75(3):Article 44. doi: 10.5688/ajpe75344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolluru S, Roesch DM, de la Fuente AA. A multi-instructor, team-based, active-learning exercise to integrate basic and clinical sciences content. Am J Pharm Educ. 2012;76(2):Article 33. doi: 10.5688/ajpe76233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marshall LL, Nykamp D. Active-learning assignments to integrate basic science and clinical course material. Am J Pharm Educ. 2010;74(7):Article 119. doi: 10.5688/aj7407119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schapiro R, Stickford-Becker AE, Foertsch JA, Remington PL, Seibert CS. Integrative cases for preclinical medical students: connecting clinical, basic science, and public health approaches. Am J Prev Med. 2011;41(4 Suppl 3):S187–S192. doi: 10.1016/j.amepre.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Wikerson L, Stevens CM, Krasne S. No content without context: integrating basic, clinical, and social sciences in a pre-clerkship curriculum. Med Teach. 2009;31(9):812–821. doi: 10.1080/01421590903049806. [DOI] [PubMed] [Google Scholar]
- 18.Green BN, Johnson CD, Vuong J, Luckock AS, Waagen G. Use of a clinical seminar to horizontally integrate basic science and clinical topics for year-one students. J Allied Health. 2008;37(3):e160–e176. [PubMed] [Google Scholar]
- 19.DiLullo C, Morris HJ, Kriebel RM. Clinical competencies and the basic sciences: an online case tutorial paradigm for delivery of integrated clinical and basic science content. Anat Sci Educ. 2009;2(5):238–243. doi: 10.1002/ase.97. [DOI] [PubMed] [Google Scholar]
- 20.Paley B, O’Connor MJ, Baillie SJ, Guiton G, Stuber ML. Integrating case topics in medical school curriculum to enhance multiple skill learning: Using fetal alcohol spectrum disorders as an exemplary case. Acad Psych. 2009;33(2):143–148. doi: 10.1176/appi.ap.33.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crane E, Clark J. Integrative basic sciences: change in mental status. Clin Pediatr (Phila). 2009;48(3):284–290. doi: 10.1177/0009922808324953. [DOI] [PubMed] [Google Scholar]
- 22.Kingsley K, O’Malley S, Stewart T, Galbraith GM. The integration seminar: a first-year dental course integrating concepts from the biomedical, professional, and clinical sciences. J Dent Educ. 2007;71(10):1322–1332. [PubMed] [Google Scholar]
- 23.Lantz MS, Chaves JF. What should biomedical sciences education in dental schools achieve? J Dent Educ. 1997;61(5):426–433. [PubMed] [Google Scholar]
- 24.Iacopino AM. The influence of “new science” on dental education: current concepts, trends, and models for the future. J Dent Educ. 2007;71(4):450–462. [PubMed] [Google Scholar]


