Abstract
Objective. To assess the integration of problem-based learning and technology into a self-care course.
Design. Problem-based learning (PBL) activities were developed and implemented in place of lectures in a self-care course. Students used technology, such as computer-generated virtual patients and iPads, during the PBL sessions.
Assessments. Students’ scores on post-case quizzes were higher than on pre-case quizzes used to assess baseline knowledge. Student satisfaction with problem-based learning and the use of technology in the course remained consistent throughout the semester.
Conclusion. Integrating problem-based learning and technology into a self-care course enabled students to become active learners.
Keywords: self-care, problem-based learning, technology, simulation
INTRODUCTION
The concept of problem-based learning originated in the 1950s, mainly in medical schools, such as Case Western Reserve University and McMaster University in Canada. While business and nursing schools have incorporated PBL activities into their curriculum for many years, implementation within pharmacy colleges and schools has only become prevalent in the last decade. Problem-based learning can be combined with innovative forms of technology to create unique teaching and learning experiences.
In 2010, PBL enhanced with innovative technology was introduced into a Self-Care and Home Diagnostic Testing course in the School of Pharmacy at Duquesne University. The required 4-credit course previously had been presented in a traditional lecture format with PowerPoint slides.
The motivation to incorporate PBL into the course came from multiple sources, including concerns raised in a survey of community pharmacy preceptors; a lack of PBL use at the school, especially in courses with large class sizes; and recent changes to the North American Pharmacist Licensure Examination (NAPLEX).
The primary motivating factor was the survey responses from 21 community pharmacy preceptors regarding their experiences with practice experience students who had completed the self-care course. On the items regarding students’ patient counseling skills and over-the-counter medication knowledge, preceptors had given students an average rating of 2.6 on a 5-point Likert-type scale (1 being lowest and 5 being highest).
The second motivating factor was the authors’ review of the literature, which found that the use of PBL in pharmacy education, and especially in self-care courses, was limited. Implementing this type of learner-centered instructional design with a large number of students, had only been attempted by a few colleges and schools of pharmacy.2 When PBL was used, it was implemented on a much smaller scale, such as in laboratory or practicum settings.3-5
The final motivating factor was updates made in March 1, 2010, to the NAPLEX blueprint to include a competency (3.2.4.)6 stating that students will be able to “recommend and provide information regarding the selection, use, and care of medical/surgical appliances and devices, self-care products, and durable medical equipment, as well as products and techniques for self-monitoring of health status and medication conditions.” Thus, to pass the national licensure examination, pharmacy students must be competent in self-care.
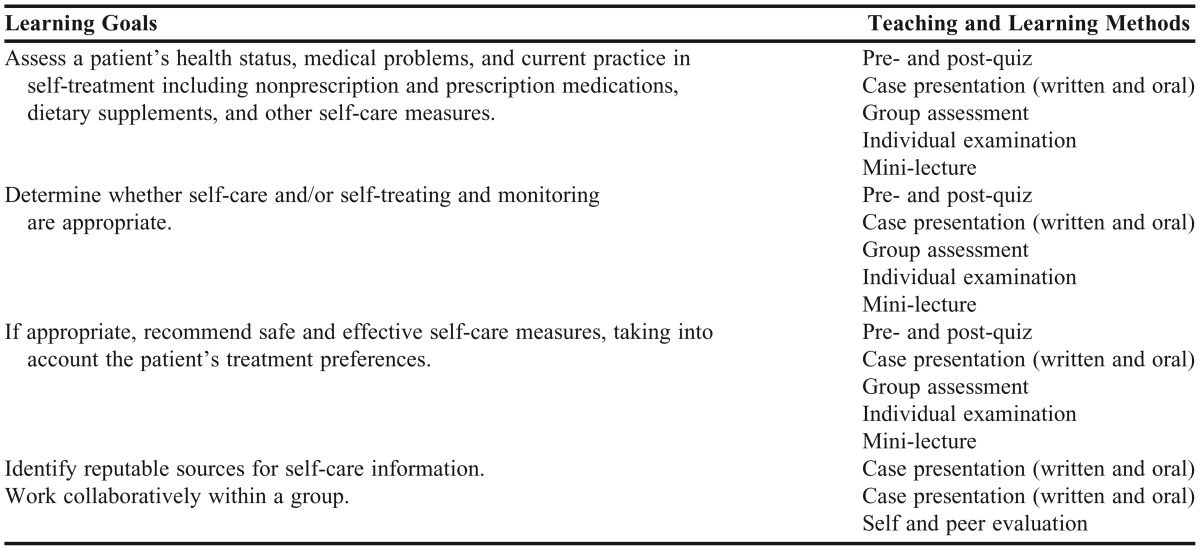
Adding PBL activities to the self-care course would also address the Accreditation Council for Pharmacy Education’s requirement to integrate active-learning strategies into courses.1 The 5 learning goals for the revised PBL self-care course are listed in Table 1 along with the teaching and learning methods used to achieve and assess these goals. This paper describes development and implementation of the revised course and the associated outcomes.
Table 1.
Teaching and Learning Methods Used to Achieve the Learning Goals for a Self-Care Course
DESIGN
The Self-Care and Home Diagnostic Testing course was a required 4-credit course offered in the second (P2) year of the school’s doctor of pharmacy (PharmD) curriculum. Typical student enrollment fluctuated between 150 and 180 students. The course previously had been taught in the typical “socratic” method. Students attended 50-minute PowerPoint lecture 4 times a week. The PowerPoint slides included detailed information about the self-care topic that was discussed and students were able to print out partially completed handouts that they were expected to fill in during the lecture.
A PBL, student-centered teaching philosophy was developed for the self-care course. Technology skills, prevalent among nearly all students in the early 20s age group, were targeted. The key was to combine the problem-based learning method with innovative technology in a way to not only excite the students about this new way of learning, but to also encourage them to want to continue to learn and to learn how to learn (metacognition) long after the conclusion of the class (life-long learning).
Problem-based learning was integrated throughout the entire 15-week course requiring the entire course to be redesigned and redeveloped. A few self-care topics (Home Testing Kits, Botanical and Nonbotanical Natural Medicines, and Dermatologic Disorders) that contained subsections and thus were too complex to present in a PBL format were still delivered in lecture format (using PowerPoint).
The introductory lecture on PBL was essential. Most students were not familiar with the term and those who were had an incorrect interpretation of PBL. Most students, when asked what PBL was, stated that it was reviewing cases after attending a lecture. The difference between true PBL and case-based reviews was discussed. A video tutorial of the instructor presenting a sample PBL session was posted for the students to view. At the end of this preparation, students were adequately prepared for the first PBL case.
Cases were created using several methods. Some cases were created based on real encounters by the author or other colleagues from a traditional community pharmacy setting. Some were based on published cases in textbooks or online and modified for the purpose of the class. Others were original cases developed specifically for a PBL environment. To preserve the integrity of these cases for use in future classes, various forms of information could be modified to make the case unique (eg, modify the age, disease states, or other medications that the patient is on, add another concomitant self-care condition).
Students were randomly assigned to 28 groups of 5 or 6 students using the Advanced Group Management tool in Blackboard (Blackboard Inc., Washington, DC). Because of the unfavorable physical layout of the stadium-style lecture hall, a seating chart was devised.
All students were required to have a laptop or iPad and a personal digital assistant (PDA) or mobile device upon entering the professional phase of the pharmacy curriculum. In this course, students used a laptop or iPad to complete pre- and post-case quizzes in Blackboard. Students also downloaded the eBook Handbook of Nonprescription Drugs to their laptops and used it as a primary reference when looking for information related to the pathophysiology, clinical presentation, nonpharmacologic therapy, and/or pharmacologic therapy of a self-care condition. Students were also required to have access to the mobile electronic resource Epocrates Essentials either from a PDA or mobile device. Finally, a laptop or iPad was used to gather information pertaining to the PBL case and to prepare the case for electronic submission.
Each PBL experience was designed to be completed within a 4-day block (Table 2). At the beginning of each PBL experience, students completed a pre-case quiz for which there was no preparation.
Table 2.
Description of the Problem-based Learning Process
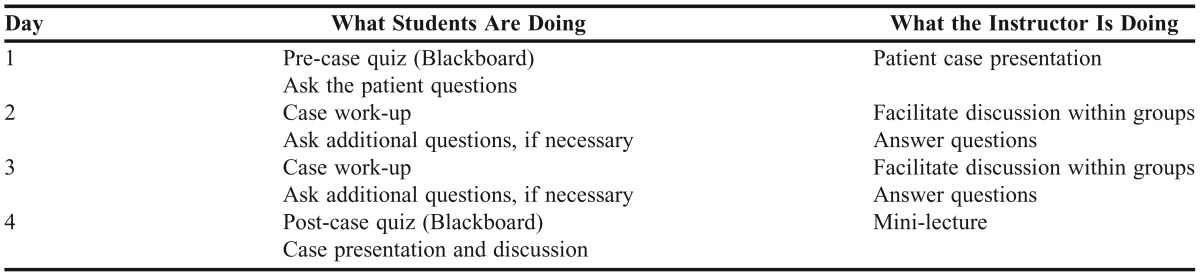
Students were not given a traditional lecture or any information pertaining to the self-care topic prior to the patient case presentation. Instead, after all students completed the pre-case quiz, the patient case presentation began. All of the groups were presented with the same PBL case. The case was not presented in the typical paper-based bullet-point format. Instead, animated computer-based virtual patients that moved and expressed emotions were developed using VoxProxy (Right Seat Software, Inc., Golden, CO) software. These patients also talked using Microsoft speech engines. Patients were programmed to have language barriers, some to have physical disabilities (eg, hard of hearing, vision difficulties), and others to have challenging personality traits: mean, impatient, and forgetful. Students were able to interact with the patient by asking questions. The virtual patient was projected on the lecture hall screen. The patient made leading comments such as, “Can you help me? I have been coughing for the last few days and I feel miserable.” At this point the students, sitting in their groups, formulated a list of questions they would ask the patient. After a period of time, the students were able to ask the patient questions. Some patient responses were preprogrammed, however, the software allowed for the instructor to quickly enter an “on demand” response if a student asked a question that was not part of the original programmed script.
Students worked on their cases using the PBL method on days 2 and 3. Students had to decide what they already knew, what they did not know, and what references they would use to research the self-care topic to ultimately develop a treatment plan for the patient. The instructor was no longer the “sage on the stage” but rather a facilitator for the groups. The instructor walked around the lecture hall during the class period and interacted with all of the groups, listening to their discussions and offering guidance if the students were “off track.” A discussion board in Blackboard was developed for each group in the event that additional work, outside of class, was necessary. Students used a template based on the QuEST/SCHOLAR method to prepare their case.7 Each group had to upload the completed document to Blackboard by 11:00 pm on the night before the case presentation.
On day 4 of each PBL case, the instructor administered a post-quiz and then each group was randomly chosen to present a part of the patient case they had researched to the entire class. Interspersed throughout the case presentations were mini-lectures to ensure that students had learned the foundational knowledge of the self-care topic. However, students were responsible, as is the ultimate goal of problem-based learning, for all of the content associated with the self-care topic.
After the conclusion of the case presentations in class, the instructor converted all documents uploaded to Blackboard to PDF files, downloaded them to an iPad, and used iAnnotate to evaluate each case and provide formative feedback directly on the document. These cases were uploaded to the discussion board in Blackboard for the groups to review. This feedback was provided within 1 week of case submission.
EVALUATION AND ASSESSMENT
The students’ baseline knowledge level of the self-care problem to be covered was established prior to commencing each PBL case by administering a pretest using the Blackboard Assessment tool. Pre- and post-case quiz scores were analyzed using a paired t test for each of the 28 groups. The post-case quiz scores were significantly higher than the pre-case quiz scores for every PBL case covered in the course (p < 0.05).
Three group assessments were administered to students during the semester. Each group was presented with a unique case during class and was given 50 minutes to work together to assess the patient, develop a treatment plan, and decide how to counsel the patient. This format was similar to the template that each group completed during the PBL cases. Table 4 shows the average scores for each group assessment. A rubric for grading the group assessments was not developed. As long as the group defended their choices and cited evidence supporting those choices, they were given full credit.
Table 4.
Group Assessment and Examination Results
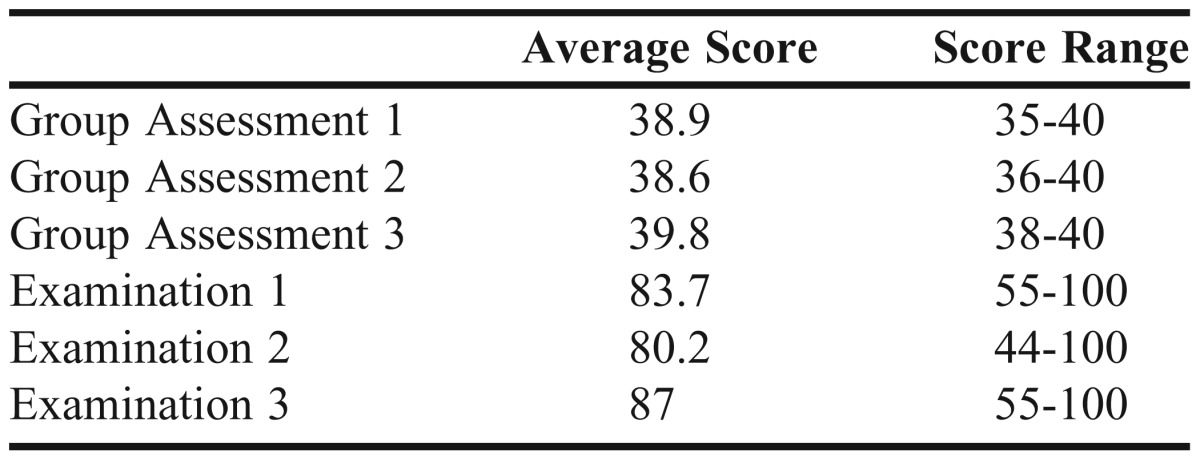
Three examinations were administered to students during the semester, 1 after each of the group assessments. These individual examinations were given to ensure each student had gained an understanding of the foundational knowledge required for the course. The examinations consisted of multiple-choice or true/false questions. All students passed all 3 individual examinations.
In order to determine student satisfaction and to gain feedback regarding this new way of teaching (or learning), mid-course and post-course survey instruments were posted in Blackboard for students to complete (Table 3).Students were generally satisfied with the integration of PBL and technology as is demonstrated by students’ consistent or slightly increased ratings as the semester progressed.
Table 3.
Pharmacy Students’ Opinions Regarding Implementation of Problem-based Learning in a Self-Care Course (N = 127)
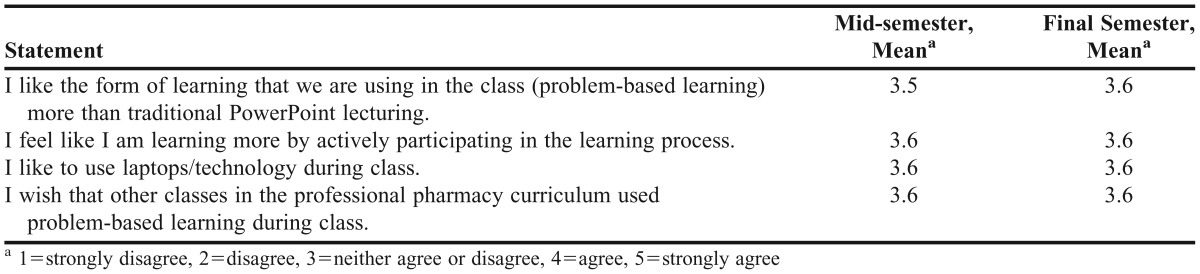
Students, especially those who described themselves as “hands-on” learners, seemed to enjoy PBL and the integration of technology. Students also liked the mini-lectures because information was reinforced.
DISCUSSION
Students were able to use the information gathered during the PBL process to successfully complete post-case quizzes. The significant difference between pre- and post-case quiz scores showed that students were able to learn basic information on their own and with peer-to-peer instruction. The instructor was there only as a guide and not the primary source of information transmission. This enabled students to actively participate in their own learning process.
By the third examination, students were more comfortable in self-directed learning and were able to adequately prepare for the examination without formal instruction and relied solely on the PBL method of learning (Table 4).
Group dynamics were an essential part of the problem-based learning process as peer-to-peer teaching can be a powerful tool. To ensure that all groups ran smoothly and that all students participated, students were required to complete a self-evaluation and peer evaluation of each group member at the midpoint and end of the semester. Individual students scores were averaged and included as part of each student’s final grade.
Consistent student satisfaction throughout the semester was important. When a new learning method or approach is introduced, students often focus on the negative aspects and their satisfaction decreases. However, student satisfaction was consistent throughout this course, even increasing slightly, which was a positive outcome.
Limiting factors included the increased number of students in the class, instructors’ lack of comfort with teaching some of the material and with deviating from the traditional use of overhead projectors and PowerPoint slides, increased time required for class restructure and redevelopment, physical classroom limitations (eg, stadium-style seating, immovable seats), and the various expenses incurred. More than 1 year was spent researching various PBL methods and creating PBL cases.
Increased expenses can be attributed to the use of technology. Additional iPads were purchased so that each group had at least one iPad to use during the PBL sessions. Also, software applications (apps) such as Keynote and Pages were purchased and loaded onto each iPad. The VoxProxy software also had a cost associated with its use.
Future plans include adding more PBL sessions, but with a modified format. Students seemed to lose focus by the end of each 4-day PBL session. Future PBL sessions will be reduced to 2 days with a 2-hour session held the first day and a 50-minute session held the second. This should give the students adequate time for group discussion, but will require them to complete out-of-class research. The community preceptors whose feedback served as part of the impetus to overhaul the course will be resurveyed, to determine if there are any significant changes in students’ self-care knowledge and skills.
Any college or school of pharmacy could easily incorporate problem-based learning into their curriculum, with or without technology. While each college or school will have unique characteristics and challenges (eg, number of students, technology-related issues, structural barriers), PBL can be modified to fit any situation. This learning approach could even be incorporated into courses taught via distance learning. Patient-case presentations (with the VoxProxy software) could be recorded as screencasts and posted in Blackboard or another course management system. If the group members could not meet in person, they could use discussion boards or video-conferencing, such as Skype.
SUMMARY
The time, expense, and creativity involved in developing a student-centered problem-based learning self-care course using multiple forms of technology resulted in increased student performance and satisfaction. Problem-based learning, enhanced with innovative technology, is an exciting way for pharmacy students to become active-learners in the educational process. Increased scores on examinations and other forms of assessment, as well as consistent student satisfaction support this. Problem-based learning methods and educational technology will continue to be used and enhanced in this self-care course.
ACKNOWLEDGEMENTS
The author would like to thank Holly Lassila, DrPH, RPh, for her contribution to the statistical analysis of the direct and indirect evidence collected.
REFERENCES
- 1.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed December 11, 2012.
- 2.Nicholl T, Lou K. A model for small-group problem-based learning in a large class facilitated by one instructor. Am J Pharm Educ. 2012;76(6):Article 117. doi: 10.5688/ajpe766117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benedict N. Virtual patients and problem-based learning in advanced therapeutics. Am J Pharm Educ. 2010;74(8):Article 143. doi: 10.5688/aj7408143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Winslade N. Large group problem-based learning: a revision from traditional to pharmaceutical care-based therapeutics. Am J Pharm Educ. 1984;58(1) [Google Scholar]
- 5.Pawlak S, Popovich N, Blank J, et al. Development and validation of guided design scenarios for problem-solving instruction. Am J Pharm Educ. 1989;53(1) [Google Scholar]
- 6.National Association of Boards of Pharmacy. NAPLEX Blueprint: The NAPLEX competency statements. http://www.nabp.net/programs/examination/naplex/naplex-blueprint. Accessed February 23, 2013.
- 7.Buring S, Kirby J, Conrad W. A structured approach for teaching students to counsel self-care patients. Am J Pharm Educ. 2007;71(1):Article 8. doi: 10.5688/aj710108. [DOI] [PMC free article] [PubMed] [Google Scholar]


