Abstract
Human leukocyte antigen B (HLA-B) is a gene that encodes a cell surface protein involved in presenting antigens to the immune system. The variant allele HLA-B*15:02 is associated with an increased risk of Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) in response to carbamazepine treatment. We summarize evidence from the published literature supporting this association and provide recommendations for the use of carbamazepine based on HLA-B genotype (also available on PharmGKB: http://www.pharmgkb.org). The purpose of this article is to provide information to allow the interpretation of clinical HLA-B*15:02 genotype tests so that the results can be used to guide the use of carbamazepine. The guideline provides recommendations for the use of carbamazepine when HLA-B*15:02 genotype results are available. Detailed guidelines regarding the selection of alternative therapies, the use of phenotypic tests, when to conduct genotype testing, and cost-effectiveness analyses are beyond the scope of this document. Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines are published and updated periodically on the PharmGKB website at (http://www.pharmgkb.org).
Focused Literature Review
A systematic literature review focused on HLA-B*15:02 genotype and carbamazepine use (see Supplementary Material online) was conducted. Reviews were included to summarize much of the earlier literature.
Gene: HLA-B
Background
Human leukocyte antigen B (HLA-B) is a gene located on the short arm of chromosome 6 (6p21.3) that encodes a cell surface protein involved in presenting intracellular antigens to the immune system. These intracellular antigens are usually the normal breakdown products of intracellular proteins and are recognized as “self.” However, if the antigen presented derives from a pathogen or, in some cases, a transplanted tissue, it may be recognized as “nonself” and trigger an immune response. HLA-B is part of a large cluster of genes known as the human major histocompatibility complex. The cluster contains three subgroups: classes I, II, and III. The HLA-B gene is a part of the class I complex, along with HLA-A and HLA-C.
Because HLA proteins present a wide variety of peptides for immune recognition, the HLA genes, and specifically HLA-B, are among the most highly polymorphic genes in the human genome. HLA polymorphisms were previously ascertained serologically, but newer approaches that exploit genotyping and DNA sequencing methods have revealed much greater complexity of genetic variation within this locus. For example, according to the World Health Organization Nomenclature Committee for Factors of the HLA System (http://hla.alleles.org), there are >2,000 identified HLA-B alleles, many of which differ from one another by more than one nucleotide. Each allele is designated by the gene name followed by an asterisk and a four- or six-digit identifier giving information about the allele type (designated by the first two digits) and specific protein subtypes (second set of digits). The allele type may correspond to the antigen detected by serological methods. Subtypes differ at one or more nucleotide positions that alter the protein-coding sequence. The details of HLA nomenclature have been described in a previous CPIC guideline.1 The guidelines we present here specifically discuss only the HLA-B*15:02 allele as it relates to carbamazepine-induced Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), serious blistering cutaneous adverse drug reactions.
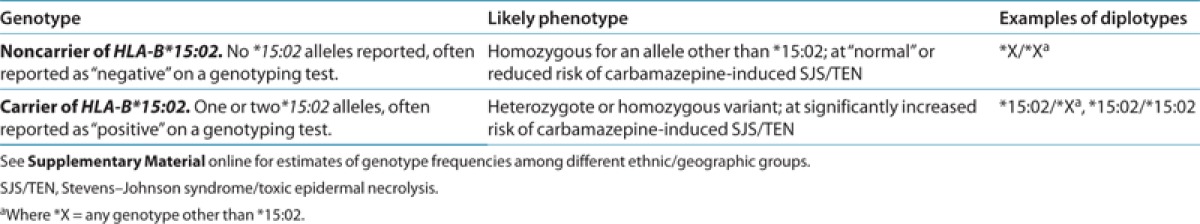
Genetic test interpretation
Clinical genotyping tests exist for identifying HLA-B alleles, including HLA-B*15:02. The HLA-B*15:02 allele predisposes to the development of carbamazepine-induced SJS/TEN but is not known to affect either carbamazepine pharmacokinetics or the development of other types of cutaneous adverse reactions (see below). Genotyping results are presented as “positive” if one or two copies of HLA-B*15:02 are present or as “negative” if no copies of HLA-B*15:02 are present. There is no intermediate genotype or phenotype. Phenotype assignments for HLA-B*15:02 genotypes are summarized in Table 1.
Table 1. Assignment of likely HLA-B phenotypes based on genotypes.
Available genetic test options
Several methods of HLA-B genotyping are commercially available. The Supplementary Material online and http://www.pharmgkb.org contain more information on available clinical testing options.
Incidental findings
no other diseases have been linked to HLA-B*15:02. However, there have been reports linking the HLA-B*15:02 allele to SJS/TEN from oxcarbazepine and phenytoin use, particularly in Asian populations.2,3,4,5,6,7,8 Other HLA-B alleles are also associated with adverse reactions to drugs, such as the association between HLA-B*57:01 and abacavir-induced hypersensitivity reaction,9 and the association between HLA-B*58:01 and increased risk of allopurinol-induced severe cutaneous adverse reactions (including but not limited to SJS/TEN).10 CPIC guidelines are available for the latter two HLA-B–associated adverse drug reactions.1,11
Other considerations
HLA-B*15:02 has a very distinct ethnic and regional distribution that is important to consider when evaluating population risk. Specifically, HLA-B*15:02 is most prevalent in Oceanian, East Asian, and South/Central Asian populations (see Supplementary Tables S1 and S2 online), ranging from 1 to >10% in some cases. The frequency of HLA-B*15:02 is highest in Han Chinese, for which some estimates from the Yunnan province have been as high as 36%. In general, rates in China range from 1 to 12%. Rates in Singapore and Hong Kong have also been estimated at 10–12%. Rates in Malaysia and Thailand are estimated at 6–8%, whereas in different regions of India, the rates range from 2 to 6%. Korea and Japan have low frequencies of the allele at 0.5 and 0.1%, respectively. The allele is also quite rare in African populations (not observed) and Europeans (0–0.02%).
Carbamazepine can cause a wide variety of cutaneous adverse drug reactions, including mild maculopapular eruptions (MPEs), drug hypersensitivity syndrome, in which a cutaneous eruption is associated with systemic manifestations, and SJS/TEN,12 the most severe manifestation. It is important to note that HLA-B*15:02 is specific for SJS and TEN; there is no evidence that it predisposes to MPEs or hypersensitivity syndrome.13 By contrast, another HLA allele, HLA-A*31:01, is associated with a wider range of carbamazepine hypersensitivity reactions, including MPEs, hypersensitivity syndrome, and SJS/TEN in both Caucasian and Japanese populations13 (see Supplementary Material online for further discussion). These associations underscore the potential importance of other alleles in other populations with different clinical manifestations.14,15
Drug: Carbamazepine
Background
Carbamazepine, an aromatic anticonvulsant related to the tricyclic antidepressants, is approved by the US Food and Drug Administration for the treatment of epilepsy and other seizure disorders, trigeminal neuralgia, and bipolar disorder. Carbamazepine reduces the propagation of abnormal impulses in the brain by producing a frequency- and voltage-dependent blockade of sodium channels, thereby inhibiting the generation of repetitive action potentials in the epileptic focus.16 Carbamazepine is commercially available as a regular-release or extended-release oral formulation, and therapy may be targeted by testing serum concentrations, with the traditionally accepted therapeutic range for treatment of epilepsy being 4–12 μg/ml.17 Above this therapeutic range, adverse effects include diplopia, drowsiness, nausea, and sedation. Carbamazepine adverse effects that are not clearly dose or concentration dependent include aplastic anemia, hyponatremia, leucopenia, osteoporosis, and hypersensitivity reactions such as MPEs, hypersensitivity syndrome, SJS/TEN, or drug-induced liver injury. For additional information regarding the pharmacokinetics and pharmacogenomics of carbamazepine, refer to the PharmGKB website (http://www.pharmgkb.org/pathway/PA165817070).18
Approximately 10% of patients develop mild cutaneous adverse drug reactions, e.g. MPEs,13 within the first 3 months of therapy.19,20 HLA-B*15:02 is specific for the carbamazepine-induced SJS and TEN. SJS is characterized by epidermal detachment affecting up to 10% of body surface area, whereas TEN usually involves >30% of the body surface area. Patients with between 10 and 30% of the body surface area blistered are defined as having an overlap syndrome. Mortality rates are <5% for SJS and >30% for TEN, with sepsis being the most frequent cause of death.21 An immune-mediated etiology has been shown for these reactions, which is consistent with the anamnestic response often seen clinically on drug rechallenge.22 In terms of the immunopathology, cytotoxic T cells, or CD8+ T cells (lymphocytes matured in the thymus that express the CD8 protein on their surface), are involved in SJS and TEN.23,24
Linking genetic variability to variability in drug-relatedphenotypes
There is substantial evidence linking HLA-B*15:02 genotype with the risk of SJS/TEN (see Supplementary Table S3 online). Application of a grading system to evidence linking genotypic variability to phenotypic variability indicates a high quality of evidence in the majority of cases (Supplementary Table S3). The evidence presented here and in Supplementary Table S3 provides the basis for the dosing recommendations in Table 2.
Table 2. Carbamazepine therapy recommendations based on HLA-B genotype.

An increased risk of SJS/TEN has been associated with the HLA-B*15:02 allele in Han Chinese and other Asian groups.19,25,26 The genetic association of carbamazepine-induced SJS/TEN with HLA-B*15:02 was first published by Chung et al. in 2004.25 In this case–control analysis, 44 Han Chinese individuals with carbamazepine-induced SJS/TEN living in Taiwan were compared with 101 carbamazepine-tolerant and 93 randomly selected healthy individuals never exposed to the drug. All 44 cases (100%) were positive for the HLA-B*15:02 allele, whereas only 3 (3%) carbamazepine-tolerant and 8 (8.6%) normal controls carried the allele. These results were replicated,19 and a similar result was found in a Han Chinese population residing in Hong Kong.26 The Food and Drug Administration issued a Health Alert in 2007 about changes to package labeling and recommendations for genetic testing in patients treated with carbamazepine.27
Consistent with the regional and ethnic distribution of the HLA-B*15:02 allele, studies have shown the genetic risk of carbamazepine-associated SJS/TEN to be higher in several Asian countries, including Vietnam,28 Cambodia,28 the Reunion Islands,28 Thailand,5,29 some parts of India,30 Malaysia,31 and Hong Kong.26 The HLA-B*15:02 allele has not been observed in cases of SJS/TEN in various ancestral groups such as Japanese and Korean populations or non-Asian descendants in Europe or North America.28,32,33,34,35 In the Han Chinese population, the sensitivity of HLA-B*15:02 as a predictive test for SJS/TEN has been estimated at 98% and specificity has been estimated at 97%; the positive predictive value is estimated at 7.7% and the negative predictive value is estimated at 100%.19 However, it is important to note that in one study, in a group of individuals thought to be of European origin, 4 of 12 individuals with SJS/TEN carried the HLA-B*15:02 allele.33 Subsequently, they were found to have some Asian ancestry. This example underscores the importance of considering the HLA-B*15:02 allele carrier status regardless of self-reported ethnicity.
Therapeutic recommendations
Currently, the Food and Drug Administration recommends that “patients with ancestry in at-risk populations should be screened for the presence of HLA-B*15:02 allele prior to starting carbamazepine” (http://www.fda.gov/Drugs/DrugSafety/ PostmarketDrugSafetyInformationforPatientsandProviders/ucm124718.htm). Individuals at highest risk are those of Han Chinese descent, followed by those in Vietnam, Cambodia, the Reunion Islands, Thailand, India (specifically Hindus), Malaysia, and Hong Kong. The frequency of HLA-B*15:02 is very low in other populations (see Supplementary Table S2 online for frequency information). However, it is important that the prescribing physician bear in mind that many people may be unaware of or fail to disclose more distant Asian ancestry in their families. In addition, much of the evidence (summarized in Supplementary Table S3 online) linking HLA-B*15:02 to SJS/TEN was generated in both children and adults. Therefore, regardless of ancestry or age of the individual, if the genetic testing results are “positive” for the presence of at least one copy of the HLA-B*15:02 allele, it is recommended that a different agent be used depending on the underlying disease, unless the benefits clearly outweigh the risk (Table 2).
Carbamazepine-induced SJS/TEN usually develops within the first 3 months of therapy; therefore, patients who have been taking carbamazepine for longer than 3 months without developing cutaneous reactions are at low risk (but not zero) of carbamazepine-induced adverse events in the future, regardless of HLA-B*15:02 status.36,37
Recommendations for incidental findings
Several drugs structurally and therapeutically similar to carbamazepine have also been associated with SJS/TEN and HLA-B*15:02. The drug-specific evidence linking HLA-B*15:02 and SJS/TEN is discussed in the Supplementary Material online and may have implications for choosing alternatives to carbamazepine in those who carry the HLA-B*15:02 allele.
In one study, the HLA-B*07:02 allele was absent in patients with carbamazepine-induced SJS/TEN but was present at frequencies of 18% in the control group and 14% in those with a mild hypersensitivity reaction, leading the authors to conclude that HLA-B*07:02 may protect against carbamazepine-induced SJS/TEN. However, there is no course of action suggested based on this genotype.32
Other considerations
Not applicable.
Potential benefits and risks for the patient
A potential benefit of HLA-B*15:02 testing is a significant reduction in the incidence of serious, sometimes fatal, SJS/TEN reactions to carbamazepine by identifying those who are at significant risk and recommending alternative treatments appropriate for the underlying indication. The success of HLA-B*15:02 prospective screening in reducing the rate of SJS/TEN has recently been demonstrated clinically in a Chinese population.38
A potential risk of HLA-B*15:02 testing is ruling out the use of carbamazepine in patients who may not have developed SJS/TEN; however, this risk is mitigated by the fact that there are often alternatives to carbamazepine with comparable effectiveness. Another potential risk would be an error in genotyping. In the event of a false-negative result, a high-risk patient could mistakenly be prescribed carbamazepine. However, because not all carbamazepine-induced SJS/TEN can be attributed to HLA-B*15:02, clinicians should carefully monitor all patients as standard practice. Genotype results are associated with a patient for a lifetime, and a genotyping error could have a broader impact on health care should other HLA-B*15:02 associations be identified in the future.
Caveats: appropriate use and/or potential misuse of genetic tests
Recently, a systematic review by Yip et al. of the relationship between carbamazepine-induced SJS/TEN and HLA-B*15:02 showed that the positive predictive value and negative predictive value for a screening test in Asians were 1.8% (7.7% in Han Chinese only) and 100%, respectively,13,39 and that 461 patients would need to be tested to prevent one case of SJS/TEN. Furthermore, they determined that carriage of HLA-B*15:02 in Asian patients was associated with a pooled odds ratio of 113.4 (95% confidence interval = 51.2–251.0; P < 1 × 10−5).13 Therefore, a significant percentage of the patients carrying the allele would not suffer from carbamazepine-induced SJS/TEN, and it is not currently possible to distinguish these carriers. However, the benefit of the high negative predictive value is clinically relevant, where Asian non-carriers of the risk allele are virtually at no risk to develop SJS/TEN, based on the study of Yip et al.13 Considering the severity of SJS/TEN, a negative test result will represent very valuable information when making treatment decisions related to carbamazepine. In the interest of patient safety, however, all patients should be monitored for cutaneous effects regardless of carrier status.
Acknowledgments
We acknowledge the critical input of members of CPIC of the Pharmacogenomics Research Network, particularly Mary V. Relling (St. Jude Children's Research Hospital) and Teri E. Klein (PharmGKB Stanford University), funded by the National Institutes of Health (NIH). This work is funded by NIH grants 2U19GM061390, R24 GM61374, MH92758, U19 HL065962, U01 GM092666, and U01 HL0105918. We thank the authors of the CPIC guidelines for abacavir dosing (ref. 1) for their contribution to this article.
CPIC guidelines reflect expert consensus based on clinical evidence and peer-reviewed literature available at the time they are written and are intended only to assist clinicians in decision making and to identify questions for further research. New evidence may have emerged since the time the guideline was submitted for publication. Guidelines are limited in scope and are not applicable to interventions or diseases not specifically identified. Guidelines do not account for all individual variation among patients and cannot be considered inclusive of all proper methods of care or exclusive of other treatments. It remains the responsibility of the health-care provider to determine the best course of treatment for the patient. Adherence to any guideline is voluntary, with the ultimate determination regarding its application to be solely made by the clinician and the patient. CPIC assumes no responsibility for any injury to persons or damage to property related to any use of CPIC guidelines, or for any errors or omissions.
The authors declared no conflict of interest.
Footnotes
SUPPLEMENTARY MATERIAL is linked to the online version of the paper at http://www.nature.com/cpt
Supplementary Material
References
- Martin M.A., Klein T.E., Dong B.J., Pirmohamed M., Haas D.W., Kroetz D.L., Clinical Pharmacogenetics Implementation Consortium Clinical pharmacogenetics implementation consortium guidelines for HLA-B genotype and abacavir dosing. Clin. Pharmacol. Ther. 2012;91:734–738. doi: 10.1038/clpt.2011.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankarkumar U., Shah K.N., Ghosh K. Letter: HLA B*1502 allele association with oxcarbamazepine-induced skin reactions in epilepsy patient from India. Epilepsia. 2009;50:1837–1838. doi: 10.1111/j.1528-1167.2009.02096.x. [DOI] [PubMed] [Google Scholar]
- Lin L.C., Lai P.C., Yang S.F., Yang R.C. Oxcarbazepine-induced Stevens-Johnson syndrome: a case report. Kaohsiung J. Med. Sci. 2009;25:82–86. doi: 10.1016/S1607-551X(09)70045-2. [DOI] [PubMed] [Google Scholar]
- Chen Y.C., Chu C.Y., Hsiao C.H. Oxcarbazepine-induced Stevens-Johnson syndrome in a patient with HLA-B*1502 genotype. J. Eur. Acad. Dermatol. Venereol. 2009;23:702–703. doi: 10.1111/j.1468-3083.2008.02988.x. [DOI] [PubMed] [Google Scholar]
- Locharernkul C., et al. Carbamazepine and phenytoin induced Stevens-Johnson syndrome is associated with HLA-B*1502 allele in Thai population. Epilepsia. 2008;49:2087–2091. doi: 10.1111/j.1528-1167.2008.01719.x. [DOI] [PubMed] [Google Scholar]
- He N., et al. Cutaneous reactions induced by oxcarbazepine in Southern Han Chinese: incidence, features, risk factors and relation to HLA-B alleles. Seizure. 2012;21:614–618. doi: 10.1016/j.seizure.2012.06.014. [DOI] [PubMed] [Google Scholar]
- Hu F.Y., Wu X.T., An D.M., Yan B., Stefan H., Zhou D. Pilot association study of oxcarbazepine-induced mild cutaneous adverse reactions with HLA-B*1502 allele in Chinese Han population. Seizure. 2011;20:160–162. doi: 10.1016/j.seizure.2010.11.014. [DOI] [PubMed] [Google Scholar]
- Hu F.Y., Wu X.T., An D.M., Yan B., Stefan H., Zhou D. Phenytoin-induced Stevens-Johnson syndrome with negative HLA-B*1502 allele in mainland China: two cases. Seizure. 2011;20:431–432. doi: 10.1016/j.seizure.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Martin A.M., et al. Predisposition to abacavir hypersensitivity conferred by HLA-B*5701 and a haplotypic Hsp70-Hom variant. Proc. Natl. Acad. Sci. U.S.A. 2004;101:4180–4185. doi: 10.1073/pnas.0307067101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung S.I., et al. HLA-B*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc. Natl. Acad. Sci. U.S.A. 2005;102:4134–4139. doi: 10.1073/pnas.0409500102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hershfield M.S., et al. Clinical Pharmacogenetics Implementation Consortium guidelines for human leukocyte antigen-B genotype and allopurinol dosing. Clin. Pharmacol. Ther. 2013;93:153–158. doi: 10.1038/clpt.2012.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirmohamed M., et al. Phenotype standardization for immune-mediated drug-induced skin injury. Clin. Pharmacol. Ther. 2011;89:896–901. doi: 10.1038/clpt.2011.79. [DOI] [PubMed] [Google Scholar]
- Yip V.L., Marson A.G., Jorgensen A.L., Pirmohamed M., Alfirevic A. HLA genotype and carbamazepine-induced cutaneous adverse drug reactions: a systematic review. Clin. Pharmacol. Ther. 2012;92:757–765. doi: 10.1038/clpt.2012.189. [DOI] [PubMed] [Google Scholar]
- Ozeki T., et al. Genome-wide association study identifies HLA-A*3101 allele as a genetic risk factor for carbamazepine-induced cutaneous adverse drug reactions in Japanese population. Hum. Mol. Genet. 2011;20:1034–1041. doi: 10.1093/hmg/ddq537. [DOI] [PubMed] [Google Scholar]
- McCormack M., et al. HLA-A*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N. Engl. J. Med. 2011;364:1134–1143. doi: 10.1056/NEJMoa1013297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean M.J., Macdonald R.L. Carbamazepine and 10,11-epoxycarbamazepine produce use- and voltage-dependent limitation of rapidly firing action potentials of mouse central neurons in cell culture. J. Pharmacol. Exp. Ther. 1986;238:727–738. [PubMed] [Google Scholar]
- Warner A., Privitera M., Bates D. Standards of laboratory practice: antiepileptic drug monitoring. National Academy of Clinical Biochemistry. Clin. Chem. 1998;44:1085–1095. [PubMed] [Google Scholar]
- Thorn C.F., et al. PharmGKB summary: carbamazepine pathway. Pharmacogenet. Genomics. 2011;21:906–910. doi: 10.1097/FPC.0b013e328348c6f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung S.I., et al. Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet. Genomics. 2006;16:297–306. doi: 10.1097/01.fpc.0000199500.46842.4a. [DOI] [PubMed] [Google Scholar]
- Locharernkul C., Shotelersuk V., Hirankarn N. Pharmacogenetic screening of carbamazepine-induced severe cutaneous allergic reactions. J. Clin. Neurosci. 2011;18:1289–1294. doi: 10.1016/j.jocn.2010.12.054. [DOI] [PubMed] [Google Scholar]
- Roujeau J.C., Stern R.S. Severe adverse cutaneous reactions to drugs. N. Engl. J. Med. 1994;331:1272–1285. doi: 10.1056/NEJM199411103311906. [DOI] [PubMed] [Google Scholar]
- Nassif A., et al. Drug specific cytotoxic T-cells in the skin lesions of a patient with toxic epidermal necrolysis. J. Invest. Dermatol. 2002;118:728–733. doi: 10.1046/j.1523-1747.2002.01622.x. [DOI] [PubMed] [Google Scholar]
- Nassif A., et al. Toxic epidermal necrolysis: effector cells are drug-specific cytotoxic T cells. J. Allergy Clin. Immunol. 2004;114:1209–1215. doi: 10.1016/j.jaci.2004.07.047. [DOI] [PubMed] [Google Scholar]
- Naisbitt D.J., et al. Hypersensitivity reactions to carbamazepine: characterization of the specificity, phenotype, and cytokine profile of drug-specific T cell clones. Mol. Pharmacol. 2003;63:732–741. doi: 10.1124/mol.63.3.732. [DOI] [PubMed] [Google Scholar]
- Chung W.H., et al. Medical genetics: a marker for Stevens-Johnson syndrome. Nature. 2004;428:486. doi: 10.1038/428486a. [DOI] [PubMed] [Google Scholar]
- Man C.B., et al. Association between HLA-B*1502 allele and antiepileptic drug-induced cutaneous reactions in Han Chinese. Epilepsia. 2007;48:1015–1018. doi: 10.1111/j.1528-1167.2007.01022.x. [DOI] [PubMed] [Google Scholar]
- Ferrell P.B., Jr, McLeod H.L. Carbamazepine, HLA-B*1502 and risk of Stevens-Johnson syndrome and toxic epidermal necrolysis: US FDA recommendations. Pharmacogenomics. 2008;9:1543–1546. doi: 10.2217/14622416.9.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonjou C., RegiSCAR Group et al. A marker for Stevens-Johnson syndrome.: ethnicity matters. Pharmacogenomics J. 2006;6:265–268. doi: 10.1038/sj.tpj.6500356. [DOI] [PubMed] [Google Scholar]
- Tassaneeyakul W., et al. Association between HLA-B*1502 and carbamazepine-induced severe cutaneous adverse drug reactions in a Thai population. Epilepsia. 2010;51:926–930. doi: 10.1111/j.1528-1167.2010.02533.x. [DOI] [PubMed] [Google Scholar]
- Mehta T.Y., et al. Association of HLA-B*1502 allele and carbamazepine-induced Stevens-Johnson syndrome among Indians. Indian J. Dermatol. Venereol. Leprol. 2009;75:579–582. doi: 10.4103/0378-6323.57718. [DOI] [PubMed] [Google Scholar]
- Chang C.C., Too C.L., Murad S., Hussein S.H. Association of HLA-B*1502 allele with carbamazepine-induced toxic epidermal necrolysis and Stevens-Johnson syndrome in the multi-ethnic Malaysian population. Int. J. Dermatol. 2011;50:221–224. doi: 10.1111/j.1365-4632.2010.04745.x. [DOI] [PubMed] [Google Scholar]
- Alfirevic A., Jorgensen A.L., Williamson P.R., Chadwick D.W., Park B.K., Pirmohamed M. HLA-B locus in Caucasian patients with carbamazepine hypersensitivity. Pharmacogenomics. 2006;7:813–818. doi: 10.2217/14622416.7.6.813. [DOI] [PubMed] [Google Scholar]
- Lonjou C., RegiSCAR study group et al. A European study of HLA-B in Stevens-Johnson syndrome and toxic epidermal necrolysis related to five high-risk drugs. Pharmacogenet. Genomics. 2008;18:99–107. doi: 10.1097/FPC.0b013e3282f3ef9c. [DOI] [PubMed] [Google Scholar]
- Kaniwa N., JSAR research group et al. HLA-B locus in Japanese patients with anti-epileptics and allopurinol-related Stevens-Johnson syndrome and toxic epidermal necrolysis. Pharmacogenomics. 2008;9:1617–1622. doi: 10.2217/14622416.9.11.1617. [DOI] [PubMed] [Google Scholar]
- Kim S.H., Zeon S.K., Choi B.W., Kim H.W., Won K.S., Kim S.J. Usefulness of F-18 FDG PET/CT in the evaluation of neck swelling in polymorphic posttransplant lymphoproliferative disorder after renal transplantation. Clin. Nucl. Med. 2011;36:587–589. doi: 10.1097/RLU.0b013e31821772bd. [DOI] [PubMed] [Google Scholar]
- Tennis P., Stern R.S. Risk of serious cutaneous disorders after initiation of use of phenytoin, carbamazepine, or sodium valproate: a record linkage study. Neurology. 1997;49:542–546. doi: 10.1212/wnl.49.2.542. [DOI] [PubMed] [Google Scholar]
- Roujeau J.C., et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N. Engl. J. Med. 1995;333:1600–1607. doi: 10.1056/NEJM199512143332404. [DOI] [PubMed] [Google Scholar]
- Chen P., Taiwan SJS Consortium et al. Carbamazepine-induced toxic effects and HLA-B*1502 screening in Taiwan. N. Engl. J. Med. 2011;364:1126–1133. doi: 10.1056/NEJMoa1009717. [DOI] [PubMed] [Google Scholar]
- Hung S.I., et al. Common risk allele in aromatic antiepileptic-drug induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Han Chinese. Pharmacogenomics. 2010;11:349–356. doi: 10.2217/pgs.09.162. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


