Abstract
An increasingly complete compendium of recurrently mutated genes in myelodysplastic syndromes (MDS) has been defined, and the application of massively parallel sequencing to identify mutations in clinical practice now promises to improve the care of patients with this disease. More than 25 recurrent MDS-associated somatic mutations have been identified, involving biological pathways as diverse as chromatin remodeling and pre-mRNA splicing. Several of these mutations have been demonstrated to have prognostic implications that are independent of existing risk stratification systems based on clinical and pathological parameters. Application of these recent discoveries to diagnosis, prognosis, risk stratification and treatment selection for patients with MDS has the potential to improve patient outcomes. Here, we review recent advances in MDS and discuss potential applications of these discoveries to clinical practice.
Background
The myelodysplastic syndromes (MDS) comprise a clinically and pathologically heterogeneous group of hematologic neoplasms, collectively characterized by clonal hematopoiesis, aberrant myeloid differentiation, ineffective hematopoiesis leading to cytopenias, and a risk of progression to acute myeloid leukemia (AML)(1). The risk of developing MDS is increased both by exogenous factors, such as exposure to cytotoxic chemotherapy, radiation or benzene, and by inherited genetic predisposition, including that associated with congenital bone marrow failure disorders or several non-syndromic familial disorders that predispose to MDS/AML.
The diagnosis of MDS is based on persistent cytopenias in association with characteristic dysplastic findings in the peripheral blood (PB) and bone marrow (BM), excess blasts, or a cytogenetic or molecular marker proving clonality, as well as exclusion of other diseases(2). The 2008 World Health Organization (WHO) classification of hematologic neoplasms includes several MDS subtypes, defined by the proportion of blood and marrow blasts, the presence or absence of monocytosis or ring sideroblasts, cytogenetic findings, and the specific cell lineages involved by dysplasia(3). Despite the clinical utility of WHO subgrouping, significant heterogeneity in phenotype and outcome persists within WHO-defined MDS categories(4, 5) and there are also challenging cases where a diagnosis of MDS is possible but minimal diagnostic criteria are not met(6).
Because of wide variation in the clinical course of MDS, treatment algorithms for MDS rely heavily on accurate prognostic stratification. Investigators have made multiple attempts to incorporate clinical and pathological information into risk models for patients with MDS, in order to guide treatment recommendations. The International Prognostic Scoring System (IPSS), published in 1997, was developed to assess prognosis of untreated adult patients with primary MDS(7). Since then, a number of other classification and prognostic scoring schemata have been developed with the goal of more accurately identifying disease subtypes with similar outcomes and risks of evolution to AML(8-12). Most recently, the revised IPSS (IPSS-R) defines five major prognostic categories based on five cytogenetic risk subgroups (including a broader range of karyotypic abnormalities than the original IPSS), BM blast percentage, and number and severity of cytopenias(4).
Clinicians currently tailor therapeutic recommendations to each patient's situation, depending on the predicted risk of disease and the patient's age, comorbid conditions, and functional status(13). Integration of somatic mutation assays into MDS diagnosis, risk stratification, and prediction of therapeutic response, has the potential to greatly improve treatment outcomes for this patient population. In addition, better understanding of the biologic basis of MDS will aid in the design of targeted, rationally designed novel therapies.
On The Horizon
Identification of Recurrent Somatic Mutations in MDS
Genetic lesions that drive the phenotype of MDS contribute to enhanced or acquired self-renewal and impaired differentiation. Additional abnormalities in the BM microenvironment and in the epigenetic state of malignant cells may independently contribute to disease pathogenesis(14, 15). The compendium of genes with recurrent somatic mutations in MDS has grown dramatically over the last few years with the application of single nucleotide polymorphism (SNP) arrays, whole exome sequencing, and whole genome sequencing.
The genes mutated in MDS can be grouped into several categories: (1) transcription factors (e.g., TP53, RUNX1, ETV6)(16-18), (2) epigenetic regulators and chromatin remodeling factors (e.g., TET2, DNMT3A, ASXL1, IDH1/2, EZH2)(19-23), (3) pre-mRNA splicing factors (e.g., SF3B1, U2AF1, SRSF2)(24-26), and (4) signaling molecules (e.g., NRAS, JAK2, NPM1)(16, 27) (summarized in Table 1). Over 70% of patients with MDS harbor somatic mutations or clonal cytogenetic abnormalities, and more than 50% of MDS patients carry at least one somatic mutation(28). Somatic mutations in SF3B1, TP53, TET2, and ASXL1 are among the most commonly identified changes, whereas those in TP53, EZH2, ETV6, RUNX1 and ASXL1 have been found to predict clinical phenotype and survival independent of other variables such as the IPSS score(16)(Table 1). Similarly, a number of chromosomal aberrations, such as deletions of chromosomes 5q, 7 or 7q, Y, or 20q; trisomy 8; and recurrent translocations and inversions involving chromosome 3q, among others, have prognostic relevance (Table 2).
Table 1.
Summary of the currently known somatic mutations in MDS and their effect on overall survival.
| MDS (% cases) | MPN (% cases) | AML (% cases) | Effect on OS (MDS) | Independent risk predictor? | |
|---|---|---|---|---|---|
| RNA Splicing | |||||
| SF3B1 | 14-28% | rare | ↑/↔ | ||
| U2AF1 | 8% | rare | ↓ | ||
| SRSF2 | 15% | rare | ↓ | ||
| ZRSR2 | 6% | ↔/↓ | |||
| SF3A1 | 1.3% | ||||
| PRPF40B | 1.3% | ||||
| U2AF65 | <1% | ||||
| SF1 | 1.3% | ||||
| PRPF8 | rare | ||||
| LUC7L2 | rare | ||||
| Epigenetic Regulators | |||||
| DNMT3A | 10% | 22% | ↓ | ||
| TET2 | 19-26% | 14-24% | ↔ | ||
| EZH2 | 6% | ↓ | + | ||
| ATRX | <1% | ||||
| IDH1/IDH2 | 4-12% | 15-25% | ↓ (IDH1) | ||
| ASXL1 | 10-20% | 10% | 5-30% | ↓ | + |
| UTX | 1% | ||||
| Transcription Factors | |||||
| TP53 | 4-14% | ↓ | + | ||
| RUNX1 | 10-20% | 12% | ↓ | + | |
| ETV6 | 1-3% | 1-3% | ↓ | + | |
| WT1 | rare | ||||
| PHF6 | rare | ||||
| Receptor Tyrosine Kinases/Signaling | |||||
| FLT3 | 2-3% | 30% | ↓ | ||
| c-KIT | 1% | 2% | |||
| JAK2 | 3% | 50-95% | |||
| CBL | 3% | 3% | |||
| CBLB | rare | ||||
| PTPN11 | <1% | ||||
| GNAS | <1% | ||||
| KRAS | 1-2% | ||||
| NRAS | 10% | 15% | ↓ | ||
| CDKN2A | <1% | ||||
| BRAF | <1% | ↓ | |||
| MPL, CSF1R | rare | ||||
| PTEN | <1% | ||||
| Others | |||||
| NPM1 | 2-3% | ||||
MDS (myelodysplastic syndromes), MPN (myeloproliferative neoplasms), AML (acute myeloid leukemia), OS (overall survival), independent risk predictor (predictor of OS independent of IPSS score, age, and other mutations), ↑ (increased OS), ↓ (decreased OS), ↔ (no effect on OS), + (mutation determined to be an IPSS independent risk predictor based on multivariablee analysis (16).
Table 2. Summary of the most common chromosomal aberrations in MDS and their effect on overall survival.
| MDS (% cases) | Effect on OS | |
|---|---|---|
| Chromosomal Aberrations | ||
| Del(5q) | 10-15% | ↑ |
| Monosomy 7, del 7q | 10% | ↓ |
| Trisomy 8 | 8% | ↔ |
| t(3q), inv(3q) | <5% | ↓ |
| i(17q) | rare | ↔ |
| Del(20q), Del(12p) | <5% | ↑ |
| Del Y, Del(11q) | <5% | ↑ ↑ |
MDS (myelodysplastic syndromes), OS (overall survival), ↑ (increased OS), ↑ ↑ (significantly increased OS), ↓ (decreased OS), ↔ (no effect on OS)
The phenotypic heterogeneity within MDS – as highlighted by the presence of variable number and severity of cytopenias, blast proportion, rate of progression to AML, response to treatment, and overall survival (OS) – is likely driven, to a great extent, by the specific pattern of these genetic changes and their interaction with therapeutic choices. Since many patients have several detectable genetic changes, it will be important to understand the interaction of these mutations with each other, as well as the impact of varying allele burden (i.e. degree of clonality) and its influence on the clinical phenotype.
Decoding the Epigenetic Landscape of MDS
Alteration in epigenetic mechanisms of regulation of gene expression are key drivers of malignant phenotype in different cancer types, including hematologic malignancies(29). Given the success of DNA methyltransferase inhibitors azacitidine and decitabine in the treatment of MDS, multiple studies have been undertaken to better define the epigenetic landscape of MDS, even though it is still unclear whether these agents exert their clinical effect entirely via DNA hypomethylation(30).
Promoter CpG island hypermethylation studies in MDS primary cells have identified widespread promoter hypermethylation of specific genes, including cell cycle and apoptosis regulators, and adhesion and motility genes, although the methylation status correlates poorly with treatment response(29). In addition, both MDS and AML have widespread promoter hypermethylation, with epigenetic deregulation of both cancer and non-cancer associated genes(31), which has also been linked to prognostic relevance(32, 33). It is still unclear whether abnormal methylation patterns are usually driven by somatic mutations that alter epigenetic state, such as the mutations in DNMT3A, IDH1/2, and TET2 that affect DNA methylation status, or whether epigenetic abnormalities are themselves primary drivers of the disease in some cases.
Moving Toward Improved Diagnostics
The diagnostic evaluation of MDS has not changed significantly in the last 30 years and still relies on PB findings, morphologic evaluation and G-banded metaphase karyotyping of a BM sample(34). However, morphologic diagnosis of MDS remains challenging and often lacks inter-observer concurrence, with a 12% discordance rate among different pathologists with respect to diagnosing dysplasia, and even greater discrepancy when assigning a specific MDS subtype(35-37). Uncertainty about MDS diagnosis impairs prognostic assessment and therapeutic decision making.
The advent of multiparameter flow cytometry (MFC) in late 1980s improved identification and purification of different stem and progenitor cell populations within the context of both normal and malignant hematopoiesis. MDS cells often display an aberrant immunophenotype that can aid in their identification, and whereas standardization is still lacking and the optimal role of MFC in MDS diagnostics and risk stratification remains unclear(38, 39), addition of MFC to cytomorphology and cytogenetics can significantly increase diagnostic yield(40). MFC analysis of high- and low- risk MDS BM samples show differential expansion of stem and progenitor populations, which in turn correlate with specific genetic, epigenetic and transcriptomic alterations(41). Additional studies of highly fractionated stem and progenitor compartments in MDS and understanding of their functional and clinical relevance remain active areas of research.
Identification of somatic mutations aids in diagnosis of uncertain cases of MDS and provides additional IPSS-independent information about prognosis. Therefore, testing for the presence of these mutations in PB or BM using deep sequencing is likely going to become routine, similar to our current practice of testing for JAK2 mutations or BCR/ABL fusion in patients with myeloproliferative neoplasms. Given the remarkable advances in DNA sequencing technologies over the last few years and ever dropping costs, multiple platforms are now becoming widely available for mutational profiling in clinical practice(42). Although whole genome sequencing provides the most comprehensive analysis of somatic mutations, high cost and our lack of understanding of clinical relevance of non-coding DNA changes impede its adaptation into routine clinical practice at this time. Targeted sequencing, such as hybrid capture of selected exons or whole exome sequencing, can yield much higher coverage of relevant parts of the genome at a lower cost. Hybrid capture platforms currently offer excellent coverage at a reasonable cost and turnaround time (∼2 weeks).
It remains to be determined whether the natural history of MDS diagnosed primarily on the basis of mutation testing has a similar natural history to MDS diagnosed using conventional criteria. The presence of an MDS-associated somatic mutation can at least confirm the presence of clonally-restricted hematopoiesis. For example, it has been shown that elderly individuals without any evidence of hematologic malignancy can acquire clonal hematopoiesis with recurrent somatic TET2 mutations(43). The contribution of such mutations to oncogenic transformation remains an area of active research.
Lastly, it is possible that a broad range of clinicians, including primary care providers, will eventually be able to evaluate their patients with new-onset cytopenias via PB testing for the presence of MDS-defining mutations, once a few common non-clonal causes of cytopenias such as nutritional deficiencies have been excluded. Having non-invasive option for diagnosis of MDS would be predicted to lower the threshold for testing and result in earlier identification of cases. Furthermore, although the initial diagnostic confirmation would most likely still involve a BM biopsy with a karyotype analysis even in patients with documented somatic mutations in their PB, serial repeat BM biopsies could become less critical for monitoring treatment response and disease progression.
Moving Toward Improved Classification and Prognostication
Multiple classification and prognostic scoring systems have been developed to identify MDS subtypes or risk groups with similar outcomes, as discussed above(4, 7-12). These schemes are based on morphology, clinical variables such as cytopenias, and cytogenetics. Somatic mutations are fundamental determinants of MDS pathophysiology, but are not part of any of the existing risk stratification systems.
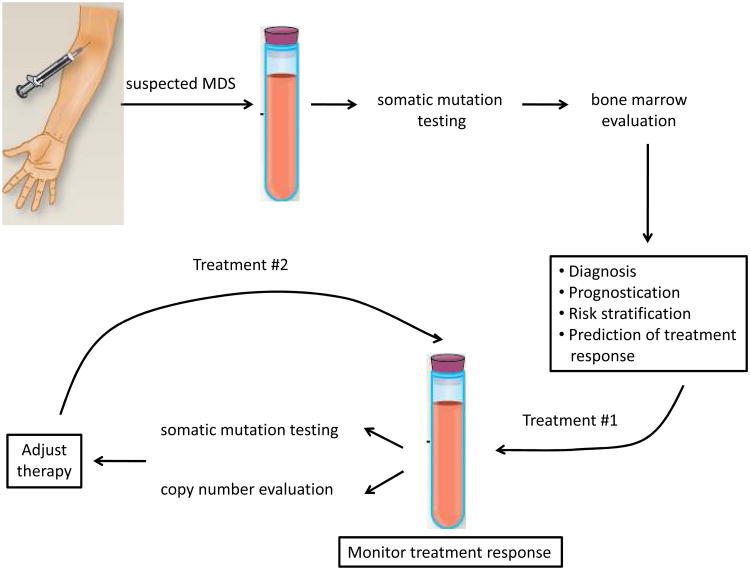
Future classification and prognostic scoring systems may incorporate somatic mutations into existing models. Alternatively, new classification schemes and prognostic scoring systems may be developed that are fundamentally based on molecular abnormalities. If all mutations can be detected in PB by deep sequencing, it is possible that MDS could be diagnosed, classified and followed over time using PB without the need for repeat BM biopsies (Figure 1).
Figure 1.
Proposed work-up of suspected MDS with incorporation of MDS-specific somatic mutation testing into clinical practice. Copy number evaluation is currently performed by cytogenetic analysis but will most likely be captured from sequencing data in the future.
Identification of Predictors of Response to Treatment
MDS patients with interstitial deletions in the long arm of chromosome 5, in the absence of complex cytogenetics or TP53 mutations, demonstrate a striking response to treatment with the thalidomide derivative lenalidomide(44). In a Phase III randomized double blind study of lenalidomide in red blood cell (RBC) transfusion dependent patients with low/intermediate-1-risk MDS with del(5q), treatment with lenalidomide resulted in RBC-transfusion independence in 56% patients, a cytogenetic response in 50% of patients, and increased OS with decreased risk of transformation to AML(45, 46). The exact mechanism of response is the subject of ongoing investigation.
Other than del(5q) for lenalidomide and serum erythropoietin levels predicting response to erythropoiesis-stimulating agents, there are no widely used biomarkers to aid clinicians in selection of therapy. Somatic mutations may serve as such biomarkers if they can be shown to consistently predict response to treatment. For example, in a recent Phase II study of lenalidomide and azacitadine in patients with IPSS intermediate-1, -2 and high risk MDS, the presence of TET2, DNMT3A, IDH1 or IDH2 mutations was predictive of achieving complete response, even in the presence of other somatic mutations that ordinarily carry a bad prognosis in MDS(47). In another retrospective study of 86 patients with MDS treated with azacitidine, the presence of a TET2 mutation was associated with an 82% response rate, compared to a 45% response rate in TET2 wild-type patients(48). Additional studies designed to identify genetic predictors of response to different treatment modalities, such as hypomethylating agents or stem cell transplantation, will be critical for tailoring appropriate therapy to each patient and minimizing toxicities from treatments with a low likelihood of therapeutic benefit.
Monitoring Response to Treatment
The ability to monitor treatment response via a non-invasive test would provide critical information to clinicians about ongoing therapeutic response and the development of resistance. Response to treatment would primarily be assessed by following the size of the malignant clone(s) over time compared to healthy cells, i.e., the percentage of cells bearing particular somatic mutations.
Next-generation sequencing studies have recently revealed and characterized the clonal architecture of MDS, and subsequent progression to secondary AML, in unprecedented detail. In the patients analyzed to date, more than 90% of the BM cells bore clonal somatic mutations at the time of MDS diagnosis, even among patients without excess blasts(49). The percentage of cells in the BM with somatic mutations does not increase significantly with progression from MDS to AML, but the genetics of the dominant clone do change. These results imply that clonal hematopoiesis involving majority of the BM is present even at early stages of MDS. Moreover, MDS is clearly a genetically complex disease, with multiple co-existing clones present in both MDS and AML, reflecting sequential acquisition of mutations and, in some cases, the parallel evolution of independent clones, some of which become extinct over time. With progression to secondary AML, the pre-existing MDS-founding clone always persists, though the MDS clone is outcompeted by more aggressive daughter subclones that drive the AML phenotype.
Ascertainment of the quantitative allele burden for different somatic mutations would be achieved by determining mutant allele frequencies (adjusted for chromosomal number) by means of deep sequencing of serial PB or BM samples. Since the size of each clone can be evaluated by the mutant frequency allele, mutant allele frequencies would delineate each subclone. Defining clonal heterogeneity of each patient at the time of diagnosis and with treatment will be instrumental in monitoring treatment response and early evidence of resistance and could result in much more timely change in treatment. The value of this approach will likely become apparent in prospective clinical trials.
Conclusions
Tremendous progress has been made in defining the genetic basis of myeloid malignancies, and MDS in particular. The identification of a growing compendium of recurrent genetic lesions in MDS and the development of technologies to track these mutations in a clinical setting have the potential to fundamentally alter the approach to patients with MDS, from diagnosis, prognosis and risk stratification, and treatment. We envision that assays for clinically relevant somatic mutations will soon become part of routine evaluation of patients in clinic (Figure 1) as well as provide fertile ground for the development of novel therapeutic strategies for the treatment of MDS.
Acknowledgments
This work was funded by the NIH (grants R01 HL082945 and P01 CA108631), the Leukemia and Lymphoma Society, and the Burroughs-Wellcome Fund.
Footnotes
Disclosures: Dr. Ebert has served as a consultant for Genoptix, Celgene, and Concert. Dr. Steensma has served as a consultant to Array Biopharma, Boehringer Ingelheim, and Genoptix.
References
- 1.Cogle CR, Craig BM, Rollison DE, List AF. Incidence of the myelodysplastic syndromes using a novel claims-based algorithm: high number of uncaptured cases by cancer registries. Blood. 2011 Jun 30;117(26):7121–5. doi: 10.1182/blood-2011-02-337964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valent P, Horny HP, Bennett JM, Fonatsch C, Germing U, Greenberg P, et al. Definitions and standards in the diagnosis and treatment of the myelodysplastic syndromes: Consensus statements and report from a working conference. Leuk Res. 2007 Jun;31(6):727–36. doi: 10.1016/j.leukres.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009 Jul 30;114(5):937–51. doi: 10.1182/blood-2009-03-209262. [DOI] [PubMed] [Google Scholar]
- 4.Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012 Sep 20;120(12):2454–65. doi: 10.1182/blood-2012-03-420489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Germing U, Gattermann N, Strupp C, Aivado M, Aul C. Validation of the WHO proposals for a new classification of primary myelodysplastic syndromes: a retrospective analysis of 1600 patients. Leuk Res. 2000 Dec;24(12):983–92. doi: 10.1016/s0145-2126(00)00088-6. [DOI] [PubMed] [Google Scholar]
- 6.Wimazal F, Fonatsch C, Thalhammer R, Schwarzinger I, Mullauer L, Sperr WR, et al. Idiopathic cytopenia of undetermined significance (ICUS) versus low risk MDS: the diagnostic interface. Leuk Res. 2007 Nov;31(11):1461–8. doi: 10.1016/j.leukres.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997 Mar 15;89(6):2079–88. [PubMed] [Google Scholar]
- 8.Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007 Aug 10;25(23):3503–10. doi: 10.1200/JCO.2006.08.5696. [DOI] [PubMed] [Google Scholar]
- 9.Kantarjian H, O'Brien S, Ravandi F, Cortes J, Shan J, Bennett JM, et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original International Prognostic Scoring System. Cancer. 2008 Sep 15;113(6):1351–61. doi: 10.1002/cncr.23697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia-Manero G, Shan J, Faderl S, Cortes J, Ravandi F, Borthakur G, et al. A prognostic score for patients with lower risk myelodysplastic syndrome. Leukemia. 2008 Mar;22(3):538–43. doi: 10.1038/sj.leu.2405070. [DOI] [PubMed] [Google Scholar]
- 11.Della Porta MG, Malcovati L, Boveri E, Travaglino E, Pietra D, Pascutto C, et al. Clinical relevance of bone marrow fibrosis and CD34-positive cell clusters in primary myelodysplastic syndromes. J Clin Oncol. 2009 Feb 10;27(5):754–62. doi: 10.1200/JCO.2008.18.2246. [DOI] [PubMed] [Google Scholar]
- 12.Malcovati L, Della Porta MG, Strupp C, Ambaglio I, Kuendgen A, Nachtkamp K, et al. Impact of the degree of anemia on the outcome of patients with myelodysplastic syndrome and its integration into the WHO classification-based Prognostic Scoring System (WPSS) Haematologica. 2011 Oct;96(10):1433–40. doi: 10.3324/haematol.2011.044602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stone RM. How I treat patients with myelodysplastic syndromes. Blood. 2009 Jun 18;113(25):6296–303. doi: 10.1182/blood-2008-09-038935. [DOI] [PubMed] [Google Scholar]
- 14.Bejar R, Levine R, Ebert BL. Unraveling the molecular pathophysiology of myelodysplastic syndromes. J Clin Oncol. 2011 Feb 10;29(5):504–15. doi: 10.1200/JCO.2010.31.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindsley RC, Ebert BL. Molecular Pathophysiology of Myelodysplastic Syndromes. Annu Rev Pathol. 2012 Aug 28; doi: 10.1146/annurev-pathol-011811-132436. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011 Jun 30;364(26):2496–506. doi: 10.1056/NEJMoa1013343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steensma DP, Gibbons RJ, Mesa RA, Tefferi A, Higgs DR. Somatic point mutations in RUNX1/CBFA2/AML1 are common in high-risk myelodysplastic syndrome, but not in myelofibrosis with myeloid metaplasia. Eur J Haematol. 2005 Jan;74(1):47–53. doi: 10.1111/j.1600-0609.2004.00363.x. [DOI] [PubMed] [Google Scholar]
- 18.Akagi T, Ogawa S, Dugas M, Kawamata N, Yamamoto G, Nannya Y, et al. Frequent genomic abnormalities in acute myeloid leukemia/myelodysplastic syndrome with normal karyotype. Haematologica. 2009 Feb;94(2):213–23. doi: 10.3324/haematol.13024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delhommeau F, Dupont S, Della Valle V, James C, Trannoy S, Masse A, et al. Mutation in TET2 in myeloid cancers. N Engl J Med. 2009 May 28;360(22):2289–301. doi: 10.1056/NEJMoa0810069. [DOI] [PubMed] [Google Scholar]
- 20.Walter MJ, Ding L, Shen D, Shao J, Grillot M, McLellan M, et al. Recurrent DNMT3A mutations in patients with myelodysplastic syndromes. Leukemia. 2011 Jul;25(7):1153–8. doi: 10.1038/leu.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boultwood J, Perry J, Pellagatti A, Fernandez-Mercado M, Fernandez-Santamaria C, Calasanz MJ, et al. Frequent mutation of the polycomb-associated gene ASXL1 in the myelodysplastic syndromes and in acute myeloid leukemia. Leukemia. 2010 May;24(5):1062–5. doi: 10.1038/leu.2010.20. [DOI] [PubMed] [Google Scholar]
- 22.Thol F, Weissinger EM, Krauter J, Wagner K, Damm F, Wichmann M, et al. IDH1 mutations in patients with myelodysplastic syndromes are associated with an unfavorable prognosis. Haematologica Oct. 95(10):1668–74. doi: 10.3324/haematol.2010.025494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ernst T, Chase AJ, Score J, Hidalgo-Curtis CE, Bryant C, Jones AV, et al. Inactivating mutations of the histone methyltransferase gene EZH2 in myeloid disorders. Nat Genet. 2010 Aug;42(8):722–6. doi: 10.1038/ng.621. [DOI] [PubMed] [Google Scholar]
- 24.Yoshida K, Sanada M, Shiraishi Y, Nowak D, Nagata Y, Yamamoto R, et al. Frequent pathway mutations of splicing machinery in myelodysplasia. Nature. 2011 Oct 6;478(7367):64–9. doi: 10.1038/nature10496. [DOI] [PubMed] [Google Scholar]
- 25.Papaemmanuil E, Cazzola M, Boultwood J, Malcovati L, Vyas P, Bowen D, et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011 Oct 13;365(15):1384–95. doi: 10.1056/NEJMoa1103283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thol F, Kade S, Schlarmann C, Loffeld P, Morgan M, Krauter J, et al. Frequency and prognostic impact of mutations in SRSF2, U2AF1, and ZRSR2 in patients with myelodysplastic syndromes. Blood. 2012 Apr 12;119(15):3578–84. doi: 10.1182/blood-2011-12-399337. [DOI] [PubMed] [Google Scholar]
- 27.Bacher U, Haferlach T, Kern W, Haferlach C, Schnittger S. A comparative study of molecular mutations in 381 patients with myelodysplastic syndrome and in 4130 patients with acute myeloid leukemia. Haematologica. 2007 Jun;92(6):744–52. doi: 10.3324/haematol.10869. [DOI] [PubMed] [Google Scholar]
- 28.Bejar R, Stevenson KE, Caughey BA, Abdel-Wahab O, Steensma DP, Galili N, et al. Validation of a prognostic model and the impact of mutations in patients with lower-risk myelodysplastic syndromes. J Clin Oncol. Sep 20;30(27):3376–82. doi: 10.1200/JCO.2011.40.7379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Issa JP. Epigenetic changes in the myelodysplastic syndrome. Hematol Oncol Clin North Am. 2010 Apr;24(2):317–30. doi: 10.1016/j.hoc.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fandy TE, Herman JG, Kerns P, Jiemjit A, Sugar EA, Choi SH, et al. Early epigenetic changes and DNA damage do not predict clinical response in an overlapping schedule of 5-azacytidine and entinostat in patients with myeloid malignancies. Blood. 2009 Sep 24;114(13):2764–73. doi: 10.1182/blood-2009-02-203547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Figueroa ME, Skrabanek L, Li Y, Jiemjit A, Fandy TE, Paietta E, et al. MDS and secondary AML display unique patterns and abundance of aberrant DNA methylation. Blood. 2009 Oct 15;114(16):3448–58. doi: 10.1182/blood-2009-01-200519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uchida T, Kinoshita T, Nagai H, Nakahara Y, Saito H, Hotta T, et al. Hypermethylation of the p15INK4B gene in myelodysplastic syndromes. Blood. 1997 Aug 15;90(4):1403–9. [PubMed] [Google Scholar]
- 33.Quesnel B, Guillerm G, Vereecque R, Wattel E, Preudhomme C, Bauters F, et al. Methylation of the p15(INK4b) gene in myelodysplastic syndromes is frequent and acquired during disease progression. Blood. 1998 Apr 15;91(8):2985–90. [PubMed] [Google Scholar]
- 34.Yunis JJ, Rydell RE, Oken MM, Arnesen MA, Mayer MG, Lobell M. Refined chromosome analysis as an independent prognostic indicator in de novo myelodysplastic syndromes. Blood. 1986 Jun;67(6):1721–30. [PubMed] [Google Scholar]
- 35.Vardiman JW. Hematopathological concepts and controversies in the diagnosis and classification of myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2006:199–204. doi: 10.1182/asheducation-2006.1.199. [DOI] [PubMed] [Google Scholar]
- 36.Naqvi K, Jabbour E, Bueso-Ramos C, Pierce S, Borthakur G, Estrov Z, et al. Implications of discrepancy in morphologic diagnosis of myelodysplastic syndrome between referral and tertiary care centers. Blood. 2011 Oct 27;118(17):4690–3. doi: 10.1182/blood-2011-03-342642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DeLima M, Albitar M, O'Brien S, Pierce S, Kantarjian H, Andreeff M, et al. Comparison of referring and tertiary cancer center physician's diagnoses in patients with leukemia. Am J Med. 1998 Mar;104(3):246–51. doi: 10.1016/s0002-9343(98)00032-1. [DOI] [PubMed] [Google Scholar]
- 38.van de Loosdrecht AA, Westers TM, Westra AH, Drager AM, van der Velden VH, Ossenkoppele GJ. Identification of distinct prognostic subgroups in low- and intermediate-1-risk myelodysplastic syndromes by flow cytometry. Blood. 2008 Feb 1;111(3):1067–77. doi: 10.1182/blood-2007-07-098764. [DOI] [PubMed] [Google Scholar]
- 39.Loken MR, van de Loosdrecht A, Ogata K, Orfao A, Wells DA. Flow cytometry in myelodysplastic syndromes: report from a working conference. Leuk Res. 2008 Jan;32(1):5–17. doi: 10.1016/j.leukres.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 40.Kern W, Haferlach C, Schnittger S, Haferlach T. Clinical utility of multiparameter flow cytometry in the diagnosis of 1013 patients with suspected myelodysplastic syndrome: correlation to cytomorphology, cytogenetics, and clinical data. Cancer. 2010 Oct 1;116(19):4549–63. doi: 10.1002/cncr.25353. [DOI] [PubMed] [Google Scholar]
- 41.Will B, Zhou L, Vogler TO, Ben-Neriah S, Schinke C, Tamari R, et al. Stem and progenitor cells in myelodysplastic syndromes show aberrant stage-specific expansion and harbor genetic and epigenetic alterations. Blood. 2012 Sep 6;120(10):2076–86. doi: 10.1182/blood-2011-12-399683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Metzker ML. Sequencing technologies - the next generation. Nat Rev Genet. 2010 Jan;11(1):31–46. doi: 10.1038/nrg2626. [DOI] [PubMed] [Google Scholar]
- 43.Busque L, Patel JP, Figueroa ME, Vasanthakumar A, Provost S, Hamilou Z, et al. Recurrent somatic TET2 mutations in normal elderly individuals with clonal hematopoiesis. Nat Genet. 2012 Nov;44(11):1179–81. doi: 10.1038/ng.2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ebert BL, Pretz J, Bosco J, Chang CY, Tamayo P, Galili N, et al. Identification of RPS14 as a 5q- syndrome gene by RNA interference screen. Nature. 2008 Jan 17;451(7176):335–9. doi: 10.1038/nature06494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.List A, Dewald G, Bennett J, Giagounidis A, Raza A, Feldman E, et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med. 2006 Oct 5;355(14):1456–65. doi: 10.1056/NEJMoa061292. [DOI] [PubMed] [Google Scholar]
- 46.Fenaux P, Giagounidis A, Selleslag D, Beyne-Rauzy O, Mufti G, Mittelman M, et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion-dependent patients with Low-/Intermediate-1-risk myelodysplastic syndromes with del5q. Blood. 2011 Oct 6;118(14):3765–76. doi: 10.1182/blood-2011-01-330126. [DOI] [PubMed] [Google Scholar]
- 47.Sekeres MA, Tiu RV, Komrokji R, Lancet J, Advani AS, Afable M, et al. Phase 2 study of the lenalidomide and azacitidine combination in patients with higher-risk myelodysplastic syndromes. Blood. 2012 Aug 22; doi: 10.1182/blood-2012-06-434639. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Itzykson R, Kosmider O, Cluzeau T, Mansat-De Mas V, Dreyfus F, Beyne-Rauzy O, et al. Impact of TET2 mutations on response rate to azacitidine in myelodysplastic syndromes and low blast count acute myeloid leukemias. Leukemia. 2011 Jul;25(7):1147–52. doi: 10.1038/leu.2011.71. [DOI] [PubMed] [Google Scholar]
- 49.Walter MJ, Shen D, Ding L, Shao J, Koboldt DC, Chen K, et al. Clonal architecture of secondary acute myeloid leukemia. N Engl J Med. Mar 22;366(12):1090–8. doi: 10.1056/NEJMoa1106968. [DOI] [PMC free article] [PubMed] [Google Scholar]