Abstract
We interviewed caretakers of 1,043 children < 5 years old in a baseline cross-sectional survey (April to May 2007) and > 20,000 children on five separate subsequent occasions (May of 2009 to December 31, 2010) to assess healthcare seeking patterns for diarrhea. Diarrhea prevalence during the preceding 2 weeks ranged from 26% at baseline to 4–11% during 2009–2010. Caretakers were less likely to seek healthcare outside the home for infants (versus older children) with diarrhea (adjusted odds ratio [aOR] = 0.33, confidence interval [CI] = 0.12–0.87). Caretakers of children with reduced food intake (aOR = 3.42, CI = 1.37–8.53) and sunken eyes during their diarrheal episode were more likely to seek care outside home (aOR = 4.76, CI = 1.13–8.89). Caretakers with formal education were more likely to provide oral rehydration solution (aOR = 3.01, CI = 1.41–6.42) and visit a healthcare facility (aOR = 3.32, CI = 1.56–7.07). Studies calculating diarrheal incidence and healthcare seeking should account for seasonal trends. Improving caretakers' knowledge of home management could prevent severe diarrhea.
Introduction
Diarrhea causes an estimated 1.87 million deaths among children < 5 years old annually, representing ∼19% of all child deaths1; 78% of the deaths occur in Africa and Asia.1 Recognizing the potential for dehydrating diarrheal illness to rapidly progress to death led to the introduction of oral rehydration solutions as the cornerstone of life-saving treatment in 1979.2 Early recognition of dehydration, home use of oral rehydration solutions (ORSs), increased fluids and continued feeding, promotion of breastfeeding, and timely medical attention for children with dehydration and diarrhea are important determinants for reducing childhood deaths from diarrhea.3 Few studies have evaluated patterns of healthcare use and home rehydration for young children with diarrhea in Kenya.4–6 As part of a multicenter, case-control study of acute diarrhea in children 0–59 months of age called the Global Enteric Multicenter Study (GEMS),7 we conducted a one-time comprehensive cross-sectional Healthcare Utilization and Attitudes Survey (HUAS) in 2007 followed by five additional abbreviated surveys from May of 2009 to December 31, 2010. The surveys were administered to caretakers of young children residing in western Kenya within the Health and Demographic Surveillance System (HDSS) area operated through collaboration between the Kenya Medical Research Institute and US Centers for Disease Control and Prevention (KEMRI/CDC). The baseline comprehensive HUAS was designed to estimate diarrhea prevalence and examine caretakers' knowledge, attitudes, and healthcare-seeking behaviors for children with diarrhea before the GEMS case-control study. The abbreviated surveys were carried out to provide additional information from different seasons and over time.8 The HUAS-lite information allows adjusted attributable fraction data for individual pathogens and moderate-to-severe diarrhea (MSD) incidence rates from sentinel health facilities to be extrapolated to the entire HDSS population.9
Methods and Materials
Study area and study population.
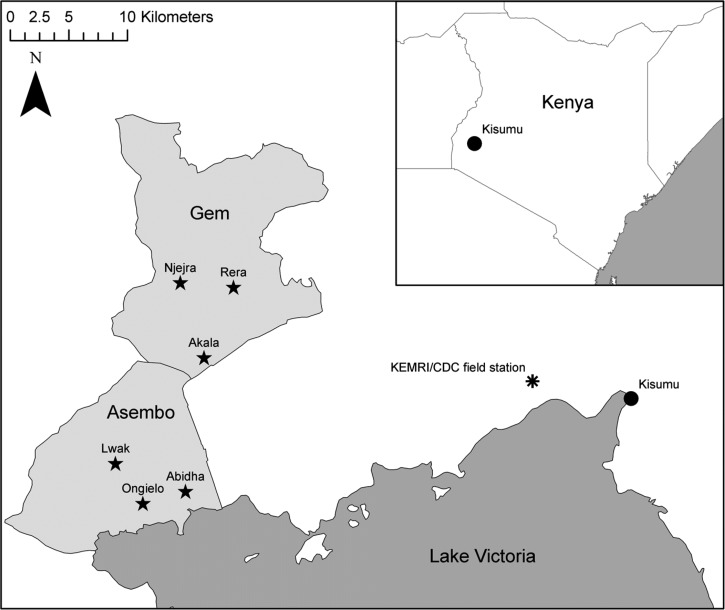
The KEMRI/CDC began implementing the HDSS in western Kenya in 2001.10,11 The HUAS and the five abbreviated surveys (called HUAS-lite surveys) were conducted in Asembo and Gem areas, which are part of the HDSS study area, representing an area of ∼500 km2 and a population of ∼135,000 persons (population density ∼300 persons/km2), about 50–65 km west of Kisumu city (Figure 1). The altitude is about 1,100 m, average monthly temperature is 24.5°C, and annual rainfall is 1,358 mm.12 Rainy seasons generally occur in March to May and October to November.10,11,13 Residents, predominantly of the Luo ethnic group,14 earn their living through small-scale business, farming, and fishing.15 The main source of cooking fuel is firewood,12 and the main source for drinking water is Lake Victoria, streams, and rivers.14 This region reports the highest adult human immunodeficiency virus (HIV) prevalence rates (approximately 15%) in Kenya.16,17 Malaria transmission is high and holoendemic.10,18 In 2007, 20,853 children < 5 years old (53% female) resided in 217 villages within the Asembo and Gem HDSS areas.
Figure 1.
Location of the Asembo and Gem HDSS areas in western Kenya. The stars located in Asembo and Gem designate the locations of the GEMS sentinel health facilities.
Definitions.
A resident of the HDSS area was defined as a person who has lived in the HDSS area for at least 4 consecutive months or a newborn child of such a person.
Diarrhea was defined as more than or equal to three loose stools within the previous 24 hours.
MSD was defined as diarrhea with one or more of the following characteristics: sunken eyes, loss of skin turgor, dysentery (blood in stool), receipt of intravenous rehydration, or required hospitalization.
Less severe diarrhea (LSD) was defined as diarrhea with absence of any characteristic of MSD (above).
Other definitions for this study have been detailed elsewhere.8
Sample size considerations.
HUAS.
The sample size considerations for the HUAS have been described elsewhere.8
HUAS-lite.
The HUAS-lite aimed at enrolling the entire population of caretakers of children < 5 years old registered as residents in the HDSS area during every round (N ∼ 20,000–22,000).
Sampling procedure.
HUAS.
From a sampling frame of ∼20,853 children < 5 years old registered in HDSS at the time of the survey, we sought to complete interviews with a minimum of 333 caretakers of children in each of three age strata: 0–11, 12–23, and 24–59 months old.
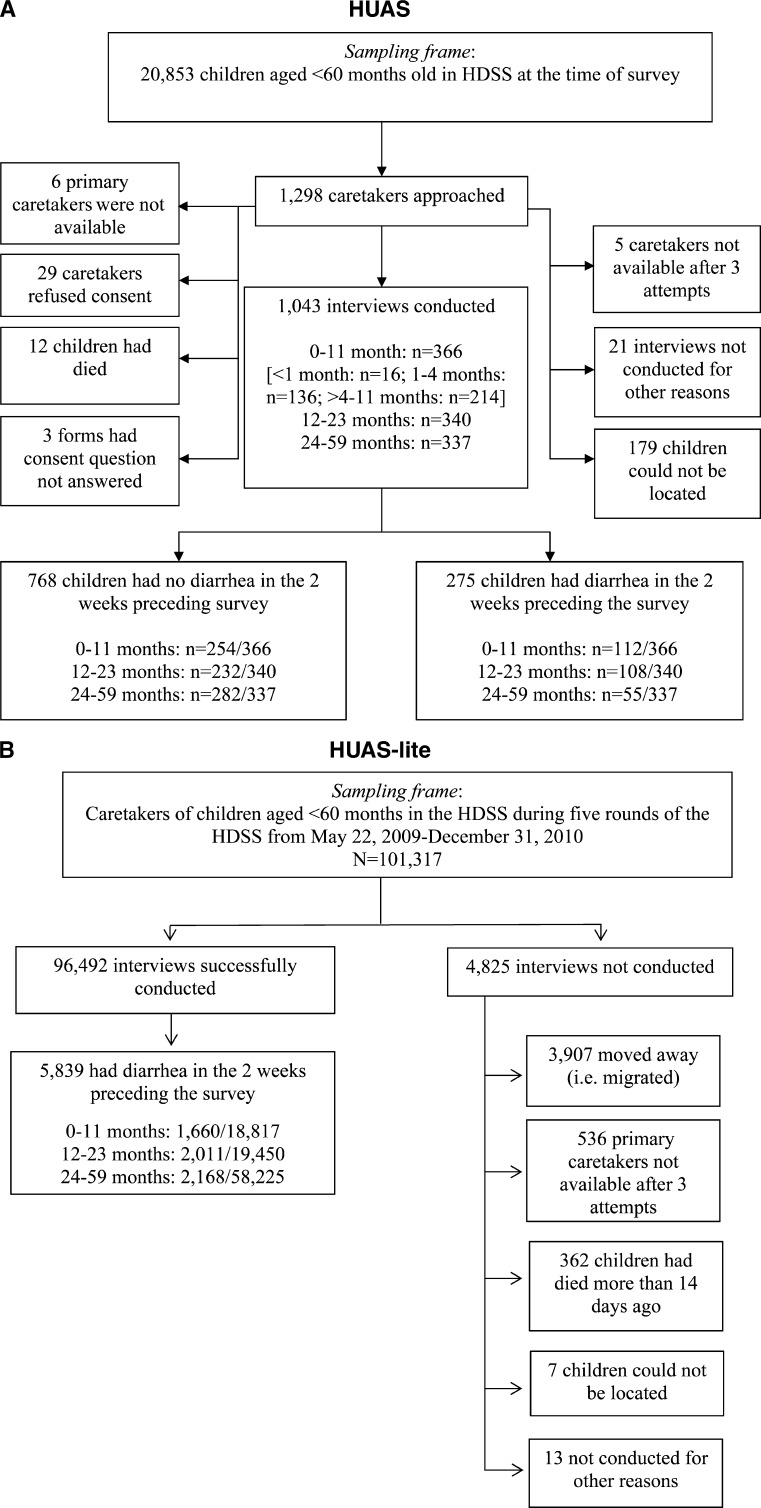
In total, 1,425 children were randomly selected to participate in the HUAS. To ensure that sufficient numbers of neonates < 1 month and children 1–4 months were represented, using the most updated census data collected through the HDSS, we supplemented the sample with a list of 100 pregnant mothers (collected from HDSS data from the most recent round; i.e., January to April of 2007) and 130 randomly selected children 1–4 months old from the most recently completed HDSS census round (January to April of 2007). All other children were randomly selected from the previous census round (September to December of 2006), including 230 children 5–11 months old, 370 children 12–23 months old, and 370 children 24–59 months old. To account for an estimated 20% loss in enrollment because of outmigration, death, and children being over age, we randomly selected an additional 75 children per age stratum. Among 1,425 children randomly selected, 553 children were ages 0–11 months (125 neonates, 155 1- to 4-month old children, and 255 5- to 11-month-old children), 445 children were ages 12–23 months, and 445 children were ages 24–59 months. Children who had moved from their residence, could not be traced, died, or were over age were replaced with a child in the appropriate age group. There was no replacement of children who had traveled (but still resided within the HDSS), refused to participate, or were not available after three attempts were made to contact their caretakers. In total, 1,298 caretakers were approached for interview (Figure 2A).
Figure 2.
(A) Study enrollment procedures for the cross-sectional HUAS of caretakers of children < 5 years old in western Kenya in 2007. (B) Study enrollment procedures for the HUAS-lite among children < 5 years old in western Kenya from May 22, 2009 to December 31, 2010.
HUAS-lite.
The KEMRI/CDC HDSS collects census and surveillance data through house-to-house interviews by trained staff on a regular basis through three rounds in each calendar year (January to April, May to August, and September to December).10 The HUAS-lites were conducted from May of 2009 to December 31, 2010 in conjunction with each of these data collection rounds (Figure 2B).
Data collection.
HUAS.
The baseline survey was carried out from April 25 to May 9, 2007 (the HUAS study period). Trained community interviewers located the households and interviewed the primary caretakers of the randomly selected children. Reinterviews were carried out in 10% of households.
After obtaining caretaker's written consent, community interviewers administered to the caretakers of all selected children a pre-tested questionnaire written in English and translated into the local dialect (Dholuo). Through 65 questions (administered over 30 minutes if the child had diarrhea), we collected information on demographics, child morbidity, parents' perception of illness and use of healthcare facilities, diarrhea history during the past 2 weeks (including signs and symptoms), home and health facility management of the child's diarrheal illness (including use of ORS), healthcare use, healthcare expenses, attitudes to healthcare and diarrhea, and hypothetical use of enteric vaccines should they become available. For children without diarrhea, the HUAS survey took, on average, 10 minutes.
HUAS-lite.
The HUAS-lite used a condensed version of the HUAS questionnaire with 21 questions; the child's primary caretaker was interviewed about information on demographics, the child's diarrhea history, and healthcare use. The first two questions screened caretakers to determine if that person was the child's primary caretaker and if the child had an illness with diarrhea during the last 14 days. If the child had diarrhea, then the additional HUAS-lite questions were asked; if not, the HUAS-lite interview was complete. For children with diarrhea, the HUAS-lite survey took, on average, 10 minutes to administer.
Data management.
HUAS.
Data were recorded on optical character recognition-enabled forms. After manual accuracy checks, the forms were electronically transmitted from KEMRI/CDC to the GEMS Data Coordinating Center (DCC) at the Perry Point Veterans Administration Hospital in Maryland, where data were captured by DataFax software (Clinical DataFax Systems Inc., Ontario, Canada). Cleaned data were exported to an SAS dataset (SAS Institute Inc., Cary, NC).
HUAS-lite.
The HUAS-lite survey form was developed and deployed to a handheld device (Personal Digital Assistant [PDA]; HTC Advantage X7500, HTC Corporation, Taoyuan City, Taiwan) running on Windows mobile 6.5 platform. The HUAS-lite questionnaire was developed and deployed to the PDA using Visual Studio.net 2005 and Microsoft SQL server 2005. For data quality, validation rules were programmed to avoid inconsistent or out of range values; repeat interviews were conducted in 3% of compounds per village, and supervisory oversight was conducted on at least 2% of weekly interviews. Weekly data were downloaded in the field to programmed netbooks, from which data inconsistency checks were undertaken. Data cleaning was performed using SAS version 9.2 (SAS Institute Inc., Cary, NC) on download at the KEMRI/CDC HDSS data section. Data were transmitted weekly to DCC through a web-based secure file transfer protocol server, where additional data cleaning and data validation were completed. Databases for each of the five HUAS-lite surveys were exported to SAS datasets.
Statistical analysis.
HUAS.
We used χ2 tests to examine the association between the characteristics of the child and the caretakers' knowledge, attitude, and health-seeking behavior (predictor factors) and any diarrhea, seeking care outside the home, use of ORS at home, and seeking care from a health facility (outcomes of interest). For all statistical tests, a two-sided P < 0.05 was considered statistically significant. Unadjusted odds ratios (ORs) and accompanying 95% confidence intervals (CIs) were used to assess the strength of the associations between categorical predictor factors and outcomes of interest.
Logistic regression was used to model separately for each outcome to evaluate the effect of specific variables and control for confounding. Variables with P ≤ 0.1 from the bivariate χ2 tests level were initially entered into the multivariable models. We used a backward stepwise regression method to arrive at our final models. All variables that were significant at P < 0.05 remained in the models. Adjusted odds ratios (aORs) for each variable are reported from the logistic regression model, controlling for the other variables in the model. The analyses were conducted taking stratification and sample weighting into account. The weighting accounted for child sex and age.
HUAS-lite.
For each survey, we estimated the 2-week period prevalence of any diarrhea, MSD, proportion of the diarrhea group seeking care outside the home, and proportion of the MSD group seeking care outside the home to one of the designated GEMS case-control study sentinel health facilities. Proportions and 95% CIs were calculated, controlling for correlation at the compound level, because more than one child may have been surveyed from the same compound. The Cochran–Armitage test for trend was used to examine differences across rounds.19 Analyses were performed using SAS statistical software version 9.2 (SAS Institute Inc, Cary, NC).
Scientific ethics.
For the HUAS, written informed consent was obtained in the local dialect from all participating caretakers before interview. For the HUAS-lite, verbal consent was sought as consent for data collection, because data collection elements for the HUAS-lite were already approved under the existing HDSS protocol (KEMRI Protocol #1801/CDC Protocol #3308).
The study protocols for the HUAS and HUAS-lite were reviewed and approved by the Scientific and Ethical Review Committees of the KEMRI (KEMRI Protocol #1155) and The Institutional Review Board (IRB) of the University of Maryland, Baltimore, MD (UMD Protocol #H-28327). The IRB for the CDC, Atlanta, GA, deferred its review to the UMD IRB (CDC Protocol #5038).
Results
Estimated prevalence for diarrhea in the HDSS from the HUAS.
Based on the weighted analysis, the estimated prevalence of any diarrheal episode during the past 2 weeks at baseline was 22.3% (CI = 19.5–25.0) among 20,853 children living in the HDSS area at the time of the HUAS survey.
Diarrhea prevalence in the HDSS from the HUAS-lite.
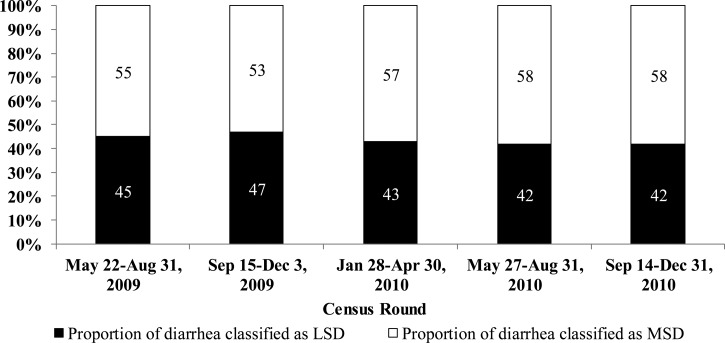
The prevalence of reported diarrhea in the past 2 weeks among children < 5 years old in the HDSS ranged from the highest rate of 10.8% (May 22 to August 31, 2009) to the lowest rate of 3.9% (September 14 to December 31, 2010) (Table 1). Among children with diarrhea in the past 2 weeks in the five rounds of the HUAS-lite, the proportion with MSD ranged from 53% (September 15 to December 3, 2009) to 58% (September 14 to December 31, 2010) (Figure 3).
Table 1.
Prevalence of diarrhea in the last 2 weeks among children < 5 years old and healthcare-seeking pattern for diarrhea by HUAS-lite round from May 22, 2009 to December 31, 2010 in western Kenya
| Characteristic | Round 1: May 22 to August 31, 2009 (n/N; %) | Round 2: September 15 to December 3, 2009 (n/N; %) | Round 3: January 28 to April 30, 2010 (n/N; %) | Round 4: May 27 to August 31, 2010 (n/N; %) | Round 5: September 14 to December 31, 2010 (n/N; %) | Overall (rounds 1–5): May 22, 2009 to December 31, 2010 (n/N; %; 95% CI) | P value for trend (rounds 1–5) |
|---|---|---|---|---|---|---|---|
| No. of HDSS resident children < 5 years approached | 20,256 (19.99) | 20,928 (20.68) | 20,687 (20.42) | 19,691 (19.44) | 19,755 (19.50) | 101,317 | < 0.0001 |
| No. of HDSS resident children < 5 years with interviews conducted | 19,221/20,556 (94.89) | 19,733/20,928 (94.29) | 19,735/20,687 (95.40) | 18,916/19,691 (96.06) | 18,887/19,755 (95.61) | 96,492/101,317 (95.24, 95.07–95.41) | < 0.0001 |
| Any diarrhea | 2,070/19,221 (10.77) | 1,017/19,773 (5.15) | 1,116/19,735 (5.65) | 898/18,916 (4.75) | 738/18,887 (3.91) | 5,839/96,492 (6.05, 5.88–6.23) | < 0.0001 |
| MSD | 1,137/2,070 (54.93) | 539/1,017 (52.99) | 641/1,116 (57.41) | 518/898 (57.68) | 427/738 (57.86) | 3,262/5,839 (55.87, 54.54–57.19) | 0.0351 |
| Sought care outside home | 915/1,137 (80.47) | 425/539 (78.85) | 537/641 (83.78) | 444/518 (85.71) | 354/427 (82.90) | 2675/3632 (82.00, 80.63–83.38) | < 0.012 |
| Sought care from a health facility | 627/915 (68.52) | 276/425 (64.94) | 354/537 (65.92) | 221/444 (49.77) | 179/354 (50.57) | 1,657/2,675 (61.94, 59.98–63.91) | < 0.0001 |
| Sought care from a GEMS sentinel health facility | 227/627 (36.20) | 87/276 (31.52) | 122/354 (34.46) | 77/221 (34.84) | 73/179 (40.78) | 586/1657 (35.37,32.82–37.91) | 0.496 |
| LSD | 933/2,070 (45.07) | 478/1,017 (47.00) | 475/1,116 (42.56) | 380/898 (42.32) | 311/738 (42.14) | 2,577/5,839 (44.13, 42.81–45.46) | 0.0351 |
| Sought care outside home | 609/933 (65.27) | 307/478 (64.23 | 354/475 (74.53) | 269/380 (70.79) | 195/311 (62.70) | 1,734/2,577 (67.29, 65.39–69.18) | 0.2711 |
| Sought care from a health facility | 330/609 (54.19) | 157/307 (51.14) | 186/354 (52.54) | 145/269 (53.90) | 111/195 (55.92) | 929/1734 (53.58, 51.07–56.08) | 0.6290 |
| Sought care from a GEMS sentinel health facility | 94/330 (28.48) | 51/157 (32.48) | 71/186 (38.17) | 39/145 (26.90) | 38/111 (34.23) | 293/929 (31.54, 28.29–34.79) | 0.3695 |
Figure 3.
Prevalence of MSD and LSD in the last 2 weeks among children < 5 years old by the HUAS-lite round from May 22, 2009 to December 31, 2010, in western Kenya.
HUAS study enrollment and background characteristics.
During the baseline HUAS, we successfully interviewed caretakers of 1,043 children 0–59 months of age; 275 (26%) children were reported to have had diarrhea during the 2 weeks preceding the interview (Figure 2A). The children with diarrhea included 112 (41%) infants, 108 (39%) toddlers (12–23 months), and 55 (20%) children (24–59 months).
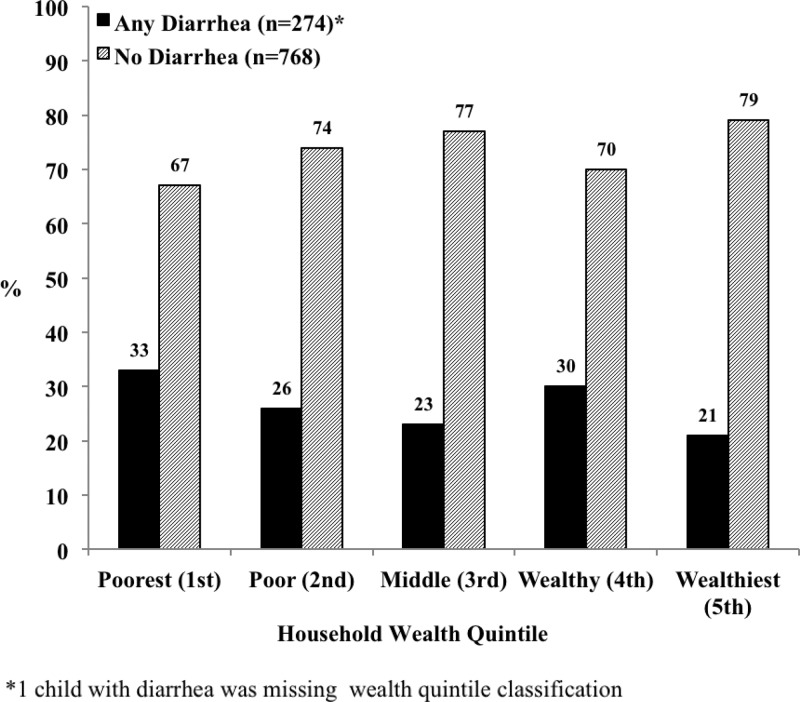
We used data on household asset ownership to rank household wealth from poorest to wealthiest using five quintiles. Overall, 34.3% of 1,043 respondents surveyed lived in households within the two lowest wealth quintiles; the highest proportion of children with diarrhea (33%) fell within the poorest wealth quintile (Figure 4). Other characteristics of the households of children with diarrhea in the 2 weeks preceding the study were similar to the characteristics of all households interviewed (Table 2). Among caretakers interviewed, 922 (88.4%) caretakers were mothers, 65 (6.2%) caretakers were fathers, 33 (3.2%) caretakers were grandmothers, and 23 (2.2%) caretakers were other relatives.
Figure 4.
Wealth quintile ranking of caretakers of children < 5 years old participating in the HUAS in western Kenya in 2007.
Table 2.
Description of the population surveyed in the HUAS study population in western Kenya in 2007 (unweighted analysis; N = 1,043)
| Characteristic | Interviewed caretakers (N = 1,043) | Interviewed caretakers of children with diarrhea in preceding 2 weeks (N = 275) | ||
|---|---|---|---|---|
| n/N | Percent | n/N | Percent | |
| Child's age stratum (months) | ||||
| 0–11 | 366 | 35 | 112 | 41 |
| 12–23 | 340 | 33 | 108 | 39 |
| 24–59 | 337 | 32 | 55 | 20 |
| Child's sex: female | 501 | 48 | 118 | 43 |
| Primary caretaker of the child interviewed was a parent | 987 | 95 | 266 | 97 |
| Child's mother lives in household | 1,016 | 97 | 271 | 99 |
| Child's father lives in household | 731 | 70 | 194 | 71 |
| Child's primary caretaker completed primary school or above | 549 | 53 | 131 | 48 |
| Median no. (IQR) of people living in house for past 6 months | 5 (4–7) | 5 (4–7) | ||
| Median no. (IQR) of rooms in house for sleeping | 2 (1–2) | 2 (1–2) | ||
| Median no. (IQR) of children ages < 60 months living in house | 2 (1–2) | 2 (1–2) | ||
IQR = interquartile range.
Caretakers knowledge, attitudes, and perceptions of illness and health seeking.
We asked caretakers what they would look for to determine if a child is dehydrated; 716 (68.6%) caretakers indicated that they would look for lethargy, 481 (46.1%) caretakers answered sunken eyes, 369 (35.4%) caretakers answered wrinkled skin, 297 (28.5%) caretakers answered dry mouth, and 297 (28.5%) caretakers answered thirst. In total, 206 (19.8%) caretakers said that they would look for both thirst and dry mouth to see if a child is dehydrated.
According to caretakers, the majority (86.2%) of 275 children who had an episode of any diarrhea in the preceding 2 weeks had three to six loose stools per day. Reported accompanying symptoms included lethargy (N = 225, 81.8%), fever (N = 201, 73.1%), being very thirsty (N = 193, 70.7%), mucus or pus in stool (N = 194, 70.6%), dry mouth (N = 188, 68.4%), rice watery stool (N = 163, 59.7%), sunken eyes (N = 162, 58.9%), decreased urination (N = 102, 40.2%), wrinkled skin (N = 92, 33.7%), vomiting (N = 89, 32.7%), coma or loss of consciousness (N = 67, 24.6%), and blood in stool (N = 34, 12.4%). Caretakers reported overall that 6.7% of children with diarrhea were hospitalized and that 6.6% received administered intravenous (IV) fluids for rehydration; 47% of the children hospitalized with diarrhea received IV fluids.
We asked caretakers what they offered their child to drink and eat during the child's diarrheal illness. Of 275 children with diarrhea, 41 (15%) caretakers said they offered the child more drink than usual, 51 (19%) caretakers reported offering the child the same amount, and 183 (67%) caretakers reported that they offered less than usual to drink during the child's diarrheal episode. Of those caretakers who offered less than usual, 96 (52%) children were offered somewhat less, 69 (38%) children were offered much less, and 18 (10%) children were offered nothing to drink during their diarrheal illness. Of 269 caretakers who reported what they offered their child to eat during their diarrheal episode, 3 (1%) caretakers offered more than usual, 43 (16%) caretakers offered the usual amount, and 223 (83%) caretakers stated that they offered less than usual to eat. Of those caretakers who offered less than usual, 74 (33%) caretakers offered somewhat less, 67 (30%) caretakers offered much less, and 82 (37%) caretakers offered nothing during the diarrheal illness. According to their caretakers, 66 (37%) of 180 and 77 (35%) of 220 children who were offered less than usual to drink and eat, respectively, had vomiting accompanying their diarrheal illness.
Healthcare was sought outside the home for 214 (77.8%) of 275 children with diarrhea. For any episode of diarrhea, the places visited as the first source of healthcare outside the home included licensed (62%) and unlicensed (11%) providers and pharmacies (27%). Seeking care outside the home was similar among caretakers of children with bloody compared with non-bloody diarrhea (27 [79%] of 34 versus 187 [78%] of 241, P > 0.05) and more common among caretakers of children who were very thirsty and had a dry mouth compared with children who did not have both conditions (142 [77%] of 184 versus 17 [46%] of 37, P < 0.05). Of 61 caretakers who did not seek care outside their home for their children with diarrhea, the main reasons that they gave were that the child did not seem to need care (44.3%), the cost of treatment was too high (32.8%), the clinic was too far from home (9.8%), and they were unable to find transportation (8.2%).
The most common means of transportation to the nearest health facility of choice was walking (74%) followed by commercial transportation (which included riding on the back of a bicycle; 13%) and personal transport (generally a bicycle; 4%).
We asked caretakers how long it would usually take to reach the health facility of choice; 770 (74%) of 1,035 respondents estimated that it would usually take less than 1 hour. The main circumstances that make it difficult for caretakers to reach their nearest health facility of choice were that it cost too much money (49%) followed by heavy rainfall or flooding (45%) and lack of transportation (24%).
We asked caretakers about who makes the decision to take the child to a health facility when sick; 809 (78%) of 1,041 respondents said that the child's mother makes the decision, whereas 232 (22%) said other relatives, including the child's father, make this decision. We asked all 1,043 caretakers who participated in this survey if they think that vaccines are important to their child's health; 99% said they think that vaccines are important.
Risk factors for diarrheal illness.
The weighted multivariate analysis of risk factors for any diarrheal illness showed that children ages < 12 months (30.5%, aOR = 2.19, CI = 1.50–3.21) and 12–23 months (31.4%, aOR = 2.24, CI = 1.53–3.30) compared with children ages 24–59 months (16.2%) were at increased risk of having an episode of diarrhea (regardless of severity) during the 2 weeks preceding the survey (Table 3). Also, caretakers who knew of a child who had died of bloody diarrhea (aOR = 2.30, CI = 1.50–3.54) and who knew that bloody diarrhea is more dangerous than other forms of diarrhea (aOR = 1.68, CI = 1.20–2.35) were associated with the caretaker reporting that their child had diarrhea in the 2 weeks preceding the survey (Table 3). The latter findings may indicate that mothers who understand how serious diarrhea can be may be more alert for it in their children and thus, more likely to report it during a survey.
Table 3.
Independent predictors of any diarrheal illness among children < 5 years old in the HUAS in western Kenya in 2007 (weighted analysis; N = 1,043)
| Variable* | Any diarrhea | Unadjusted OR (95% CI) | aOR† (95% CI) | |
|---|---|---|---|---|
| n/N | Weighted (%) | |||
| Child's age group (months) | ||||
| 0–11 | 112/366 | 30.5 | 2.27 (1.57–3.27) | 2.19 (1.50–3.21) |
| 12–23 | 108/340 | 31.4 | 2.37 (1.63–3.46) | 2.24 (1.53–3.30) |
| 24–59 | 55/337 | 16.2 | Reference | Reference |
| Child's sex | ||||
| Male | 157/542 | 24.7 | 1.32 (0.96–1.83) | 1.24 (0.88–1.75) |
| Female | 118/501 | 19.8 | ||
| Caretaker knows a child who died of bloody diarrhea | ||||
| Yes | 63/185 | 33.0 | 1.99 (1.34–2.97) | 2.30 (1.50–3.54) |
| No | 207/843 | 19.8 | ||
| Caretaker thinks bloody diarrhea is more dangerous than simple loose watery and cholera-like diarrhea | ||||
| Yes | 159/526 | 26.7 | 1.67 (1.21–2.31) | 1.68 (1.20–2.35) |
| No | 114/514 | 17.9 | ||
| Caretaker knows ways to prevent bloody diarrhea | ||||
| Yes | 102/458 | 17.6 | 0.60 (0.43–0.83) | 0.57 (0.41–0.81) |
| No | 173/585 | 26.4 | ||
Based on the inclusion criteria, 22 variables were initially included in the model; results are shown for the significant variables controlling for age and sex.
aORs, where all ORs control for other factors in the model.
Predictors of seeking healthcare outside the home for any diarrheal illness.
On weighted multivariate analysis, seeking healthcare outside the home for diarrheal illness was less common for infants than children ages 24–59 months (aOR = 0.33, CI = 0.12–0.87) (Table 4). Caretakers who said lack of transportation was the main factor preventing them from reaching the health facility of their first choice were more likely to seek care outside the home for any diarrhea compared with caretakers who did not answer in this way (90.5% versus 78.9%; aOR = 3.18, CI = 1.13–8.89). This result may indicate that caretakers who have an expressed preference for certain health facilities may be more willing to seek care, perhaps because they are generally more informed. Caretakers of children who had sunken eyes during their diarrheal illness compared with caretakers of children who did not have sunken eyes (92.2% versus 64.9%) sought care more frequently outside the home (aOR = 4.76, CI = 2.12–10.70) (Table 4).
Table 4.
Independent predictors of seeking care outside the home for children < 5 years old with any diarrhea in the HUAS in western Kenya in 2007 (weighted analysis; N = 275)
| Variable* | Sought care outside home for any diarrhea | Unadjusted OR (95% CI) | aOR† (95% CI) | |
|---|---|---|---|---|
| n/N | Weighted (%) | |||
| Child's age group (months) | ||||
| 0–11 | 76/112 | 67.7 | 0.31 (0.13–0.76) | 0.33 (0.12–0.87) |
| 12–23 | 90/108 | 84.3 | 0.80 (0.31–2.07) | 0.72 (0.26–1.97) |
| 24–59 | 48/55 | 87.1 | Reference | Reference |
| Child's sex | ||||
| Male | 123/157 | 81.9 | 1.06 (0.54–2.09) | 1.27 (0.57–2.81) |
| Female | 91/118 | 80.9 | ||
| Lack of transportation makes it difficult for caretakers to reach their health center of first choice | ||||
| Yes | 51/59 | 90.5 | 2.55 (1.09–5.99) | 3.18 (1.13–8.89) |
| No | 163/216 | 78.9 | ||
| Sunken eyes as a symptom that the child presented with during the diarrheal illness | ||||
| Yes | 145/162 | 92.2 | 6.38 (3.10–13.16) | 4.76 (2.12–10.70) |
| No | 69/113 | 64.9 | ||
| Antibiotic offered to the child at home during diarrheal illness | ||||
| Yes | 38/43 | 93.3 | 3.65 (1.34–9.97) | 3.41 (1.07–10.82) |
| No | 176/232 | 79.2 | ||
| Feeding practices at home during diarrheal illness | ||||
| Offered less than usual to eat | 189/223 | 86.5 | 4.57 (2.06–10.13) | 3.42 (1.37–8.53) |
| Offered usual or more than usual to eat | 23/46 | 58.3 | ||
| Caretaker thinks that medication is the best way to prevent any diarrheal illness | ||||
| Yes | 41/48 | 90.5 | 2.44 (0.99–6.00) | 3.51 (1.27–9.72) |
| No | 173/227 | 79.6 | ||
Based on the inclusion criteria, 16 variables were initially included in the model; results are shown for the significant variables controlling for age and sex.
aORs, where all ORs control for other factors in the model.
Predictors of seeking healthcare from a health facility among caretakers who sought care outside the home for any diarrheal illness.
On weighted multivariate analysis, seeking care from a licensed health facility (versus a non-licensed health facility) among those caretakers who sought care outside the home for any diarrheal illness was significantly more common for infants versus older children (aOR = 5.06, CI = 1.88–13.61), when the caretaker had some formal education versus none (aOR = 3.32, CI = 1.56–7.07), when caretakers thought that bloody diarrhea could cause harm or death (aOR = 3.25, CI = 1.16–9.09), when caretakers did not report circumstances that make it difficult to reach their preferred health facility (aOR = 3.90, CI = 1.47–10.35), when the child was lethargic during the diarrheal episode (aOR = 5.73, CI = 1.79–18.42), when the child had been offered ORS at home (aOR = 6.99, CI = 3.01–16.22), and when the child was offered no special (i.e., alternative) remedies at home (aOR = 10.17, CI = 2.84–36.37). The latter may possibly be indicative of caretakers' higher education, which was also a predictor of seeking care at a health facility (aOR = 3.32, CI = 1.56–7.07). Caretakers who did not report looking for thirst as a sign of dehydration were less likely to seek care from a health facility for their child's diarrheal illness (aOR = 0.21, CI = 0.09–0.47) (Table 5).
Table 5.
Independent predictors of seeking care from a health facility among children < 5 years old with any diarrhea in the HUAS in western Kenya in 2007 (weighted analysis; N = 214)
| Variable* | Sought care for any diarrhea at a health facility | Unadjusted OR (95% CI) | aOR† (95% CI) | |
|---|---|---|---|---|
| n/N | Weighted (%) | |||
| Child's age group (months) | ||||
| 0–11 | 53/76 | 69.7 | 2.30 (1.08–4.93) | 5.06 (1.88–13.61) |
| 12–23 | 46/90 | 51.8 | 1.08 (0.52–2.22) | 1.35 (0.57–3.21) |
| 24–59 | 24/48 | 49.98 | Reference | Reference |
| Child's sex | ||||
| Male | 77/123 | 54.7 | 1.03 (0.59–1.80) | 0.65 (0.32–1.34) |
| Female | 46/91 | 54.5 | ||
| Caretaker's education | ||||
| More than primary school (some formal education) | 67/104 | 65.1 | 2.35 (1.25–4.44) | 3.32 (1.56–7.07) |
| Less than primary school (no formal education) | 56/110 | 44.2 | ||
| Caretaker looks to see if the child is thirsty to assess dehydration | ||||
| Yes | 34/65 | 43.3 | 0.52 (0.27–1.03) | 0.21 (0.09–0.47) |
| No | 89/149 | 59.4 | ||
| Caretaker perceives that blood in stool can cause harm or death to the child | ||||
| Yes | 112/186 | 57.9 | 2.95 (1.15–7.60) | 3.25 (1.16–9.09) |
| No | 11/28 | 31.8 | ||
| Caretaker never endures circumstances that make it difficult to reach the health facility of choice | ||||
| Yes | 32/42 | 69.7 | 2.25 (0.93–5.44) | 3.90 (1.47–10.35) |
| No | 91/172 | 50.6 | ||
| Lethargy as a symptom during diarrheal illness | ||||
| Yes | 112/185 | 57.6 | 2.41 (0.92–6.30) | 5.73 (1.79–18.42) |
| No | 11/29 | 36.1 | ||
| Child was offered ORSs at home for diarrheal illness | ||||
| Yes | 43/56 | 75.5 | 3.50 (1.57–7.84) | 6.99 (3.01–16.22) |
| No | 80/158 | 46.8 | ||
| Child was offered no special remedies at home for diarrheal illness | ||||
| Yes | 22/27 | 79.1 | 3.73 (1.17–11.86) | 10.17 (2.84–36.37) |
| No | 101/187 | 50.4 | ||
Based on the inclusion criteria, 14 variables were initially included in the model; results are shown for the significant variables controlling for age and sex.
aORs, where all ORs control for other factors in the model.
Factors associated with ORS use among children with any diarrhea.
Most (89.5%) caretakers indicated that ORSs works well to treat diarrhea. However, only 63 (22.9%) of 275 children with any diarrhea, regardless of severity, were offered ORS at home according to their caretakers. A higher proportion of children with MSD (46 of 182, 25.3%) compared with LSD (17 of 93, 18.3%) were offered ORS at home (P > 0.05).
We examined factors associated with the use of ORSs at home for the child's diarrheal illness (Table 6). In the multivariate weighted analysis, caretakers were less likely to use ORSs at home for infants versus older children (aOR = 0.35, CI = 0.14–0.89). They were more likely to use ORSs at home if the primary caretaker had some formal education versus none (aOR = 3.01, CI = 1.41–6.42), if the caretaker perceived that dehydration could result in harm or death (aOR = 5.54, CI = 2.23–13.73), if the child had vomiting three or more times per day during the diarrheal episode (aOR = 3.33, CI = 1.56–7.11), if the caretaker knew of a child who died of bloody diarrhea (aOR = 2.73, CI = 1.20–6.20), if the child was offered the usual amount to eat or less than usual during their diarrheal episode (aOR = 8.24, CI = 1.80–37.73), and if the caretaker believed that breastfeeding prevents diarrheal illness (aOR = 16.19, CI = 1.32–199.21).
Table 6.
Independent factors associated with use of ORSs at home among children < 5 years old with any diarrhea in the HUAS in western Kenya in 2007 (weighted analysis; N = 275)
| Variable* | Reported ORS use at home for child's diarrheal illness | Unadjusted OR (95% CI) | aOR† (95% CI) | |
|---|---|---|---|---|
| n/N | Weighted (%) | |||
| Child's age group (months) | ||||
| 0–11 | 20/112 | 17.7 | 0.53 (0.25–1.14) | 0.35 (0.14–0.89) |
| 12–23 | 27/108 | 23.7 | 0.77 (0.37–1.61) | 0.85 (0.35–2.06) |
| 24–59 | 16/55 | 28.9 | Reference | Reference |
| Child's sex | ||||
| Male | 41/157 | 29.0 | 1.78 (0.90–3.53) | 1.64 (0.78–3.48) |
| Female | 22/118 | 18.7 | ||
| Caretaker's education | ||||
| More than primary school (some formal education) | 36/131 | 30.6 | 1.92 (0.99–3.70) | 3.01 (1.41–6.42) |
| Less than primary school (no formal education) | 27/144 | 18.7 | ||
| Caretaker perceives that diarrhea with vomiting can result in harm to or death of child | ||||
| Yes | 48/218 | 21.8 | 0.48 (0.22–1.01) | 0.10 (0.03–0.32) |
| No | 15/57 | 36.9 | ||
| Caretaker perceives that presence of dehydration can result in harm to or death of child | ||||
| Yes | 43/160 | 29.0 | 1.86 (0.94–3.71) | 5.54 (2.23–13.73) |
| No | 20/115 | 18.0 | ||
| Child has vomiting three or more times per day during diarrheal episode | ||||
| Yes | 32/89 | 35.2 | 2.19 (1.12–4.32) | 3.33 (1.56–7.11) |
| No | 31/183 | 19.9 | ||
| Caretaker knows a child who died of bloody diarrhea | ||||
| Yes | 21/63 | 32.6 | 1.86 (0.89–3.88) | 2.73 (1.20–6.20) |
| No | 40/207 | 20.7 | ||
| Feeding practices at home during diarrheal illness | ||||
| Offered usual/less than usual to eat | 59/223 | 28.1 | 5.10 (1.70–15.31)‡ | 8.24 (1.80–37.73) |
| Offered more than usual to eat | 4/46 | 7.1 | ||
| Caretaker believes that breastfeeding prevents childhood diarrheal illness | ||||
| Yes | 3/5 | 69.6 | 7.38§ | 16.19 (1.32–199.21) |
| No | 60/270 | 23.7 | ||
Based on the inclusion criteria, 17 variables were initially included in the model; results are shown for the significant variables controlling for age and sex.
aORs, where all ORs control for other factors in the model.
Exact Pearson χ2 P value is 0.0076.
Exact Pearson χ2 P value is 0.081. CI for OR is not presented because of small cell sizes.
Estimated care seeking for diarrhea in the HDSS from the HUAS and HUAS-lite.
Our weighted analysis estimated that caretakers of 81.5% (CI = 76.5–86.4) of children in the HDSS with any diarrheal episode in the past 2 weeks sought care outside the home. In general, care was sought from licensed providers (57.6%, CI = 49.9–65.5), unlicensed providers (12.5%, CI = 7.2–17.7), and pharmacies (29.9%, CI = 22.5–37.3).
Among children with reported diarrhea specifically in the HUAS-lite, 82.0% of those children with MSD (95% CI = 80.6–83.4) received care outside the home versus 67.3% (95% CI = 65.4–69.2) of children with LSD (when averaged over the five surveys) (Table 1).
Care seeking for moderate-to-severe diarrhea in the HDSS from the HUAS-lite.
Among those caretakers seeking care for MSD in the HUAS-lite, 61.9% (95% CI = 59.9–63.9) sought care from a health facility; 35.4% (95% CI = 32.8–37.9) of MSD cases seeking care at a health facility specifically visited one of the GEMS case-control study sentinel healthcare facilities (Table 1). Of note, there were no significant differences in the proportions of caretakers who sought care at GEMS case-control study sentinel health facilities for MSD (586/1657, 35.4%) or LSD (293/929, 31.5%) over the course of the five rounds (P = 0.496 for MSD; P = 0.369 for LSD).
Discussion
Our study found that the 2-week period prevalence of diarrhea was 26% at the baseline HUAS and decreased over the five HUAS-lite surveys of caretakers of all children in the HDSS from 11% to 4% between 2009 and 2010. The key findings of our surveys were that less than one-half of children with diarrheal disease receive care at a licensed healthcare facility and that substantial proportions of children with diarrhea are given less food and drink than normal and are not offered ORS. Health use surveys can be helpful in extrapolating burden data from surveillance studies, like GEMS, which use sentinel hospitals to capture patients. Because GEMS calculates population-based incidence of diarrheal disease and its specific attributed etiologies, having reliable estimates on the proportion of children with diarrheal disease who are seen at the sentinel study clinics provides a basis for using a multiplier to adjust incidence rates to account for what was missed because of the surveillance methodology.9
These surveys also provide guides to direct interventions to reduce the public health impact of diarrheal disease. For example, our survey documents that ORSs are underused in Kenya,20–23 similar to other locations in Africa.21,24 Findings from this study and others20–24 can provide an impetus for raising community and clinician awareness and parental demand for ORSs, an inexpensive remedy that has been estimated to save over 1.5 million children's lives per year.3,25 Community education is also needed to ensure that parents continue to feed and provide increased drink to children, particularly infants, with diarrhea. Failure to do so may hasten severe dehydration and death from diarrheal disease.
In developing countries, diarrhea is often inadequately managed at home,24 and delays in seeking care for moderate to severe pediatric diarrheal illness are common in Kenya, leading to poor outcomes.26 Strategies, policies, and interventions to reduce childhood diarrheal disease should take into consideration that the caretakers in Kenya (and possibly, in similar settings) are not familiar with the critical importance of appropriate home management of diarrhea, especially for infants who may be at highest risk of poor outcomes. A concerning observation from the HUAS is that 85.5% of caretakers of children with diarrhea, regardless of severity, knew that ORSs work well to treat diarrhea but only 22.9% of caretakers in practice offered their child ORSs at home during an episode. This finding, coupled with the finding that caretakers in the study population substantially decrease both fluid and food intake for their children during diarrheal illness, is worrisome and contrary to World Health Organization recommendations.3 Such findings have also been reported recently in a number of studies in rural and urban Kenya, and they are consistent with global trends in reductions in ORS use and the practice of decreasing the amount of fluid given to children during their diarrheal illness.21,24 Such inappropriate home management may have been a factor in the finding that caretakers were less likely to seek healthcare outside the home for infants with diarrhea, but among those caretakers who did seek healthcare, the location was most commonly a health facility. Furthermore, the finding that caretakers were significantly more likely to seek care when their ill child had lethargy, may represent inadequate home management of diarrheal illness as lethargy may have been a proxy for late presentation of infants to health facilities in a critical life threatening condition. Early home management may have avoided such situations.
Almost three-quarters of caretakers said that they usually walk the health facility of choice, and 74% of caretakers reported that it takes less than 1 hour to get to their health facility of choice. Moreover, the main reason that caretakers gave for not seeking care outside the home was that children did not seem to need care, which corroborates poor recognition of disease severity in children. Overprescription of antibiotics by clinicians and inappropriate use of antibiotics at home before seeking care have previously been reported in the study area and are responsible for the emergence of antimicrobial-resistant strains of enteric bacteria.26–28 In the HUAS, we found that 14% of children who reached a health facility had already been offered unprescribed antibiotics administered by the caretaker, which is consistent with previous observations.27 In recent qualitative studies in the area, caretakers reported a preference to using Western antimicrobial and antimotility drugs over fluid-based medicines, which are not as effective in stopping diarrhea.20 Empowering caregivers to be comfortable giving ORSs and know to continue feeding by educational messages and campaigns and increasing community ORS availability are essential to improving diarrhea management.22 Caretakers' knowledge of a child who had died of bloody diarrhea and their awareness that bloody diarrhea may be more dangerous than other forms of diarrhea were associated with the caretaker reporting that the child had diarrhea in the 2 weeks preceding the HUAS survey. This result could suggest that caretakers who are better informed on the potentially serious nature of diarrhea may be more astute in recognizing an episode of diarrhea among their young children. Caretakers were more likely to seek care in the HUAS if they reported that they never endure circumstances that make it difficult to reach their health facility of choice. This result may suggest that these particular caretakers have little or no circumstantial barriers (such as cost, flooding, or lack of transportation) to seeking care for their child's diarrhea.
Our study is subject to biases, because we depended on caretakers' recall of the occurrence of the child's diarrheal episode over the previous 2 weeks; also, we assumed that caretakers were familiar with signs and symptoms of diarrhea, such as sunken eyes, wrinkled skin, and dehydration, to classify diarrhea as MSD or LSD. Qualitative behavioral research among caretakers of young children coupled with the HUAS and HUAS-lite surveys would have aided in interpretation of the reasons for the lack of appropriate home management and beliefs related to seeking care. Although diarrhea among young children occurred frequently, it seemed to differ in this community at the time of the one-time cross-sectional HUAS survey (26%) compared with the five HUAS-lite surveys (4–11%). Data were collected from a sample of 1,425 children in the HDSS population in 2007 and the entire population of approximately 21,000 children during five census rounds from May of 2009 to December of 2010; thus, the HUAS-lite estimates are likely more precise estimates of diarrhea prevalence, because we captured the whole HDSS population and not just a random sample as in the HUAS cross-sectional survey. The difference in prevalence between the baseline and census rounds may also be a consequence of the differences in methods used between the baseline HUAS and the subsequent five surveys. The baseline survey was a cross-sectional survey conducted at a single point in time (during a rainy season) among a randomly selected subset of children in the HDSS; in contrast, in the HUAS-lite, which was conducted in the entire HDSS population, we approached all children in the HDSS for interview over a much longer period for each of the five surveys. In addition, there may have been differences in caregivers recall between the two surveys or interviewer bias, because different teams administered the HUAS and HUAS-lite. However, declines in diarrhea have also been noted in HDSS surveillance over the last few years (KEMRI/CDC, unpublished data) as coincident with hygiene and in-home water treatment promotion, increased use of ORSs, and seeking treatment of diarrhea at a health facility among HDSS residents.29 The proportion of childhood diarrhea episodes classified as MSD remained consistently between 50% and 60% when captured over the course of the five rounds of the HUAS-lite surveys. Given the findings from the HUAS-lite surveys that were carried out to assess seasonal trends in diarrhea prevalence and healthcare seeking, it is important that future studies calculating diarrheal incidence account for seasonality. The data collected on MSD prevalence and healthcare seeking from GEMS sentinel health facilities in the five HUAS-lite surveys will be used to extrapolate incidence rates from GEMS surveillance for MSD in Kenya, which was conducted during the same time period in sentinel health facilities within the same geographic area.
ACKNOWLEDGMENTS
This study includes data generated by the Kenya Medical Research Institute/Centers for Disease Control and Prevention (KEMRI/CDC) Health and Demographic Surveillance System (HDSS), which is a member of the International Network for the Demographic Evaluation of Populations and their Health (INDEPTH). We acknowledge the contributions of and thank the KEMRI/CDC HDSS team, especially the late Dr. Kubaje Adazu (1961–2009); the Global Enteric Multicenter Study (GEMS) Kenya staff for supporting the data collection and processing; Salome Omondi, Caleb Okonji, Alex Ondeng, Peter Jaron, Maquins Sewe, Onyango Emmanuel, and Gordon Orwa at the KEMRI/CDC, Kisumu, Kenya; John Crump, Elizabeth Blanton, and Kavita Trivedi at the CDC, Atlanta, GA; Daniel Feikin at the Johns Hopkins Bloomberg School of Public Health and Centers for Disease Control and Prevention, Baltimore, MD; the GEMS Data Coordinating Center, Perry Point Veterans Administration Medical Center, Perry Point, MD; and Dilruba Nasrin, University of Maryland, School of Medicine, Center for Vaccine Development, Baltimore, MD. We are grateful to the caretakers in the Asembo and Gem community who participated in this work. This manuscript is published with the approval of the director of KEMRI.
Disclaimer: The findings and conclusions in this report are the findings and conclusions of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Footnotes
Financial support: This study was funded by the Bill and Melinda Gates Foundation through the University of Maryland, School of Medicine, Center for Vaccine Development, Baltimore, MD (M.M.L., Principal Investigator).
Authors' addresses: Richard Omore, John Williamson, Fenny Moke, Vincent Were, David Obor, Frank Odhiambo, and Kayla F. Laserson, Kenya Medical Research Institute/Centers for Disease Control and Prevention Research and Public Health Collaboration, Kisian Campus, Kisumu, Kenya, E-mails: romore@kemricdc.org, jwilliamson@ke.cdc.gov, fmoke@kemricdc.org, vwere@kemricdc.org, dobor@kemricdc.org, fodhiambo@ke.cdc.gov, and Klaserson@ke.cdc.gov. Ciara E. O'Reilly and Eric D. Mintz, Division of Foodborne, Waterborne, and Environmental Diseases, Centers for Disease Control and Prevention, Atlanta, GA, E-mails: bwf1@cdc.gov and edm1@cdc.gov. Tamer H. Farag, Karen L. Kotloff, and Myron M. Levine, Center for Vaccine Development, University of Maryland School of Medicine, Baltimore, MD, E-mails: tfarag@medicine.umaryland.edu, Kkotloff@medicine.umaryland.edu, and mlevine@medicine.umaryland.edu. Anna Maria van Eijk, Liverpool School of Tropical Medicine, Liverpool, Merseyside, United Kingdom, E-mail: amvaneijk@yahoo.com. John Vulule, Centre for Global Health Research, Kenya Medical Research Institute, Kisumu, Kenya, E-mail: jvulule@kisian.mimcom.net. Robert F. Breiman, Emory Global Health Institute, Emory University, Atlanta, GA, E-mail: rfbreiman@emory.edu.
References
- 1.Boschi-Pinto C, Velebit L, Shibuya K. Estimating child mortality due to diarrhoea in developing countries. Bull World Health Organ. 2008;86:710–717. doi: 10.2471/BLT.07.050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nalin DR, Levine MM, Hornick RB, Bergquist EJ, Hoover D, Holley HP, Waterman D, VanBlerk J, Matheny S, Sotman S, Rennels M. The problem of emesis during oral glucose-electrolytes therapy given from the onset of severe cholera. Trans R Soc Trop Med Hyg. 1979;73:10–14. doi: 10.1016/0035-9203(79)90120-2. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Implementing the New Recommendations on the Clinical Management of Diarrhoea. Geneva: World Health Organization; 2006. [Google Scholar]
- 4.Burton DC, Flannery B, Onyango B, Larson C, Alaii J, Zhang X, Hamel MJ, Breiman RF, Feikin DR. Healthcare-seeking behaviour for common infectious disease-related illnesses in rural Kenya: a community-based house-to-house survey. J Health Popul Nutr. 2011;29:61–70. doi: 10.3329/jhpn.v29i1.7567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bigogo G, Audi A, Aura B, Aol G, Breiman RF, Feikin DR. Health-seeking patterns among participants of population-based morbidity surveillance in rural western Kenya: implications for calculating disease rates. Int J Infect Dis. 2011;14:e967–e973. doi: 10.1016/j.ijid.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 6.Breiman RF, Olack B, Shultz A, Roder S, Kimani K, Feikin DR, Burke H. Healthcare-use for major infectious disease syndromes in an informal settlement in Nairobi, Kenya. J Health Popul Nutr. 2011;29:123–133. doi: 10.3329/jhpn.v29i2.7854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levine MM, Kotloff KL, Nataro JP, Muhsen K. The Global Enteric Multicenter Study (GEMS): impetus, rationale, and genesis. Clin Infect Dis. 2012;55((Suppl 4)):S215–S224. doi: 10.1093/cid/cis761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nasrin D, Wu Y, Blackwelder WC, Farag TH, Saha D, Sow SO, Alfonso PL, Breiman RF, Sur D, Faruque ASG, Zaidi AKM, Biswas K, van Eijk AM, Walker DG, Levine MM, Kotlof KL. Health care seeking for childhood diarrhea in developing countries: evidence from seven sites in Africa and Asia. Am J Trop Med Hyg. 2013;89((Suppl 1)):3–12. doi: 10.4269/ajtmh.12-0749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blackwelder WC, Biswas K, Wu Y, Kotloff KL, Farag TH, Nasrin D, Graubard BI, Sommerfelt H, Levine MM. Statistical methods in the Global Enteric Multicenter Study (GEMS) Clin Infect Dis. 2012;55((Suppl 4)):S246–S253. doi: 10.1093/cid/cis788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adazu K, Lindblade KA, Rosen DH, Odhiambo F, Ofware P, Kwach J, Van Eijk AM, Decock KM, Amornkul P, Karanja D, Vulule JM, Slutsker L. Health and demographic surveillance in rural western Kenya: a platform for evaluating interventions to reduce morbidity and mortality from infectious diseases. Am J Trop Med Hyg. 2005;73:1151–1158. [PubMed] [Google Scholar]
- 11.Odhiambo FO, Laserson KF, Sewe M, Hamel MJ, Feikin DR, Adazu K, Ogwang S, Obor D, Amek N, Bayoh N, Ombok M, Lindblade K, Desai M, Ter Kuile F, Phillips-Howard P, van Eijk AM, Rosen D, Hightower A, Ofware P, Muttai H, Nahlen B, Decock K, Slutsker L, Breiman RF, Vulule JM. Profile: the KEMRI/CDC Health and Demographic Surveillance System–western Kenya. Int J Epidemiol. 2012;41:977–987. doi: 10.1093/ije/dys108. [DOI] [PubMed] [Google Scholar]
- 12.Feikin DR, Nguyen LM, Adazu K, Ombok M, Audi A, Slutsker L, Lindblade KA. The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Trop Med Int Health. 2009;14:54–61. doi: 10.1111/j.1365-3156.2008.02193.x. [DOI] [PubMed] [Google Scholar]
- 13.Feikin DR, Olack B, Bigogo GM, Audi A, Cosmas L, Aura B, Burke H, Njenga MK, Williamson J, Breiman RF. The burden of common infectious disease syndromes at the clinic and household level from population-based surveillance in rural and urban Kenya. PLoS One. 2011;6:e16085. doi: 10.1371/journal.pone.0016085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hawley WA, ter Kuile FO, Steketee RS, Nahlen BL, Terlouw DJ, Gimnig JE, Shi YP, Vulule JM, Alaii JA, Hightower AW, Kolczak MS, Kariuki SK, Phillips-Howard PA. Implications of the western Kenya permethrin-treated bed net study for policy, program implementation, and future research. Am J Trop Med Hyg. 2003;68:168–173. [PubMed] [Google Scholar]
- 15.Lindblade KA, Eisele TP, Gimnig JE, Alaii JA, Odhiambo F, ter Kuile FO, Hawley WA, Wannemuehler KA, Phillips-Howard PA, Rosen DH, Nahlen BL, Terlouw DJ, Adazu K, Vulule JM, Slutsker L. Sustainability of reductions in malaria transmission and infant mortality in western Kenya with use of insecticide-treated bednets: 4 to 6 years of follow-up. JAMA. 2004;291:2571–2580. doi: 10.1001/jama.291.21.2571. [DOI] [PubMed] [Google Scholar]
- 16.Amornkul PN, Vandenhoudt H, Nasokho P, Odhiambo F, Mwaengo D, Hightower A, Buve A, Misore A, Vulule J, Vitek C, Glynn J, Greenberg A, Slutsker L, De Cock KM. HIV prevalence and associated risk factors among individuals aged 13–34 years in rural western Kenya. PLoS One. 2009;4:e6470. doi: 10.1371/journal.pone.0006470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National AIDS and STI Control Program (NASCOP) Kenya AIDS Indicator Survey, 2007. Nairobi, Kenya: Ministry of Medical Services and Ministry of Public Health and Sanitation; 2007. [Google Scholar]
- 18.Gatei W, Kariuki S, Hawley W, ter Kuile F, Terlouw D, Phillips-Howard P, Nahlen B, Gimnig J, Lindblade K, Walker E, Hamel M, Crawford S, Williamson J, Slutsker L, Shi YP. Effects of transmission reduction by insecticide-treated bed nets (ITNs) on parasite genetics population structure: I. The genetic diversity of Plasmodium falciparum parasites by microsatellite markers in western Kenya. Malar J. 2010;9:353. doi: 10.1186/1475-2875-9-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11:375–386. [Google Scholar]
- 20.Blum LS, Oria PA, Olson CK, Breiman RF, Ram PK. Examining the use of oral rehydration salts and other oral rehydration therapy for childhood diarrhea in Kenya. Am J Trop Med Hyg. 2011;85:1126–1133. doi: 10.4269/ajtmh.2011.11-0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ram PK, Choi M, Blum LS, Wamae AW, Mintz ED, Bartlett AV. Declines in case management of diarrhoea among children less than five years old. Bull World Health Organ. 2008;86:E–F. doi: 10.2471/BLT.07.041384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olson CK, Blum LS, Patel KN, Oria PA, Feikin DR, Laserson KF, Wamae AW, Bartlett AV, Breiman RF, Ram PK. Community case management of childhood diarrhea in a setting with declining use of oral rehydration therapy: findings from cross-sectional studies among primary household caregivers, Kenya, 2007. Am J Trop Med Hyg. 2011;85:1134–1140. doi: 10.4269/ajtmh.2011.11-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Othero DM, Orago AS, Groenewegen T, Kaseje DO, Otengah PA. Home management of diarrhea among underfives in a rural community in Kenya: household perceptions and practices. East Afr J Public Health. 2008;5:142–146. doi: 10.4314/eajph.v5i3.38992. [DOI] [PubMed] [Google Scholar]
- 24.Forsberg BC, Petzold MG, Tomson G, Allebeck P. Diarrhoea case management in low- and middle-income countries—an unfinished agenda. Bull World Health Organ. 2007;85:42–48. doi: 10.2471/BLT.06.030866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 26.Kenya National Bureau of Statistics, Ministry of Public Health and Sanitation, National Coordinating Agency for Population and Development . Kenya Demographic and Health Survey 2008–09. Nairobi, Kenya: Kenya National Bureau of Statistics; 2009. [Google Scholar]
- 27.Shapiro RL, Kumar L, Phillips-Howard P, Wells JG, Adcock P, Brooks J, Ackers ML, Ochieng JB, Mintz E, Wahlquist S, Waiyaki P, Slutsker L. Antimicrobial-resistant bacterial diarrhea in rural western Kenya. J Infect Dis. 2001;183:1701–1704. doi: 10.1086/320710. [DOI] [PubMed] [Google Scholar]
- 28.Brooks JT, Ochieng JB, Kumar L, Okoth G, Shapiro RL, Wells JG, Bird M, Bopp C, Chege W, Beatty ME, Chiller T, Vulule JM, Mintz E, Slutsker L. Surveillance for bacterial diarrhea and antimicrobial resistance in rural western Kenya, 1997–2003. Clin Infect Dis. 2006;43:393–401. doi: 10.1086/505866. [DOI] [PubMed] [Google Scholar]
- 29.Hamel MJ, Adazu K, Obor D, Sewe M, Vulule J, Williamson JM, Slutsker L, Feikin DR, Laserson KF. A reversal in reductions of child mortality in western Kenya, 2003–2009. Am J Trop Med Hyg. 2011;85:597–605. doi: 10.4269/ajtmh.2011.10-0678. [DOI] [PMC free article] [PubMed] [Google Scholar]