Abstract
In the predominantly rural Manhiça district, in southern Mozambique, diarrhea is one of the leading causes of death among children under 5 years. Caretakers randomly selected from the Demographic Surveillance Database were invited to participate in a community-based survey on use of healthcare services for gastroenteritis. Of those caretakers reporting an episode of diarrhea during the recall period, 65.2% in the first survey and 43.8% in the second survey reported seeking care at a health facility. Independent risk factors for seeking care in health facilities in the first survey included the presence of diarrhea with fever and not knowing any sign of dehydration; having a television at home was related with an independent decreased use of the health facilities. In the second survey, the use of health services was significantly associated with diarrhea with fever and vomiting. Establishment of continuous prospective monitoring allows accounting for changes in healthcare use that may occur because of seasonality or secular events.
Introduction
The World Health Organization (WHO) ranks diarrheal disease as the second most common cause of mortality among children under 5 years (0–59 months) of age in developing countries. Each year, about 1.35 million children die of diarrhea in this age group, representing up to 15% of the total burden of pediatric deaths.1,2 The distribution of these deaths caused by diarrheal diseases, however, is very unbalanced, and the poorest countries are the most affected. More than 80% of all deaths in children younger than 5 years occur in sub-Saharan Africa and Southeast Asia, primarily as a result of worse social and sanitation conditions and lack of access to adequate treatments and healthcare services.3–6
Since the independence in 1975, the Government of Mozambique has tried to promote equitable access to basic health services through the continued expansion of the primary healthcare system and additionally, the elimination of healthcare fees for children under 5 years of age.7,8 However, despite increased availability of health resources, infant mortality rates remain unacceptably high; they are estimated at 138 of 1,000 live births, and they are related, in most cases, to easily preventable infectious diseases.9,10 In Mozambique, as usually occurs in most other sub-Saharan African countries, diarrheal disease carries a high burden of morbidity and mortality, especially among younger children. Thus, diarrhea is estimated to be the third leading cause of death (accounting for at least 10% of all mortality) among children ages 0–14 years in the city of Maputo, the capital and an urban environment.11 In the district of Manhiça (predominantly rural), diarrhea is the third leading cause of hospital admission among children ages 0–14 years and the fourth leading cause of death among children between 12 and 59 months12 according to verbal autopsies performed in the area.
In a country where up to 65% of the population lives in areas considered rural, many of these deaths occur at home and therefore, away from health centers or hospitals. This result is primarily because of structural problems, which lead to limited access to health systems and to a lesser extent, a lack of recognition by parents or primary caretakers of children of the symptoms associated with serious illness. Thus, according to data from the Mozambican Ministry of Health, 60% of the population (12 million of a total of 20 million) has no access to the health system; this inaccessibility is defined as living 20 miles or farther away from any health facility.13,14 It, therefore, seems appealing to try to understand in greater depth the functioning of these health systems and the constraints associated with their use. This understanding is even more important in the case of diarrheal diseases in particular, because they often are considered at the population level as trivial illnesses that are not serious or do not require specialized care, despite their high associated morbidity and mortality in developing countries. Understanding the challenges related to access to health systems would be useful for the development of policies and programs designed to counterbalance such barriers, encourage equity in care, promote a better use of the available services, and ultimately, improve their quality, not only to improve their use by children but also, the general population.
The main objective of this study was to assess the perceptions and attitudes of primary caretakers in the community about diarrheal disease and its associated danger and also, determine what conditions are associated in a rural area like Manhiça with the use of healthcare services in children under 5 years of age with diarrheal disease.
Materials and Methods
Study area and population.
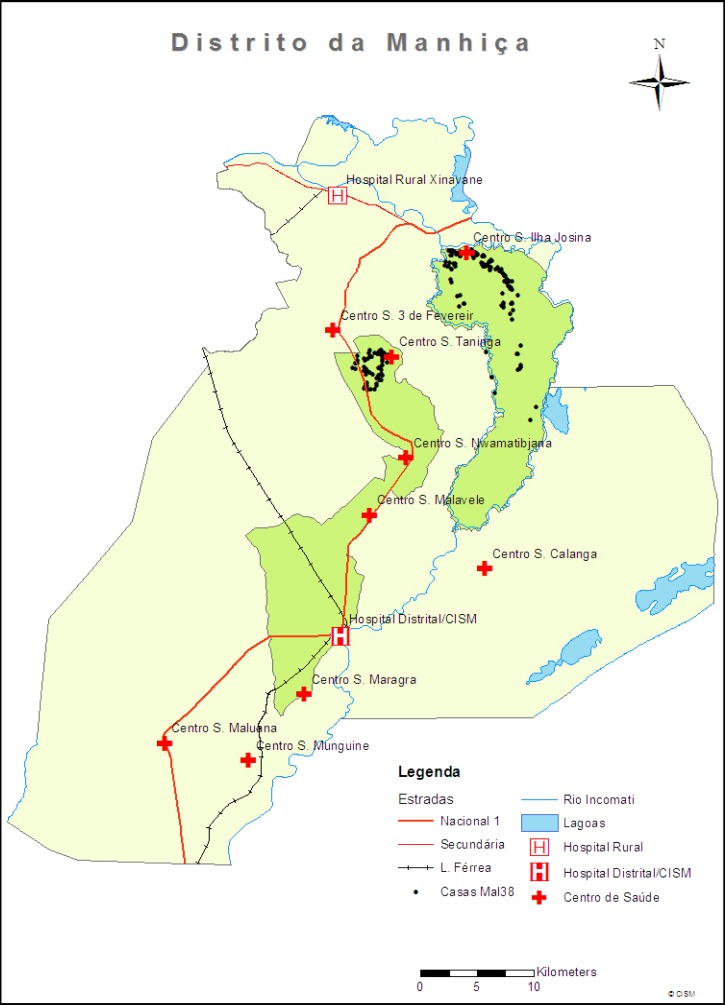
The study was based on two community surveys conducted in the District of Manhiça, a rural area located 80 km from the capital of Mozambique, Maputo (Figure 1). The first cross-sectional survey took place between May 8 and June 28 of 2007. The second survey included a series of four repeated cross-sectional assessments that took place between February 16, 2009 and December 30, 2010 and was conducted to account for changes in healthcare use that may occur because of seasonality (e.g., flooding, harvest season, and holidays) or secular events (e.g., elections and political unrest). In Manhiça, the climate is subtropical, with two distinct seasons: a warm and rainy season, usually spanning from November to April, and a generally cooler and drier season during the rest of the year. The average annual temperature ranges from 22°C to 24°C, and annual rainfall ranges from 600 to 1,000 mm. No droughts or floods occurred during the study period. Malaria transmission, mainly caused by Plasmodium falciparum, is perennial, with substantial seasonality and moderate intensity.15 At the time of the study, malaria in Manhiça accounted for one-third of all outpatient visits, one-half of the pediatric admissions, and 19% of all in-hospital pediatric deaths.16,17 Human immunodeficiency virus (HIV) prevalence in the district is very high18; in 2007, the prevalence of HIV among 646 hospitalized children included in a pneumonia study was 25%.19 The Manhiça district has about 150,000 inhabitants. The Centro de Investigação em Saúde da Manhica (CISM) has run a demographic surveillance system (DSS) within this district since 1996, involving intensive and regular monitoring of a population of about 80,000 inhabitants in an area of around 500 km2. About one-fifth (19%) of the study area inhabitants are children < 5 years of age.20,21 The first of the two surveys was restricted to a smaller area within the DSS, covering 100 km2 with 48,200 people, of which 17% (8,192) were children younger than 5 years of age.
Figure 1.
Manhiça study area.
Study design.
Many of these study methods were adapted from the Generic Protocols for: I) Hospital-Based Surveillance to Estimate the Burden of Rotavirus Gastroenteritis in Children and II) a Community-Based Survey on Utilization of Health Care Services for Gastroenteritis in Children from the WHO.22 Data collection was performed through interviews conducted with primary caretakers of children ages 0–59 months living in the District of Manhiça. For the first survey, 1,140 children were randomly selected from the DSS database and stratified into three age groups as follows: 400 children ages 0–11 months (a group larger than the rest because of the assumed higher difficulty for locating and recruiting children in this age group) and 370 children between 12–23 and 24–59 months. For the second survey, random sampling from the DSS occurred periodically to prevent a large number of children from ageing out of age strata. Children were not included in case of change of residence, death, migration, difficulties of finding the child's primary caretakers after three attempts, or if the child's age was confirmed to be older than 5 years at the time of the visit. In such cases, new candidates were included to complete the necessary numbers. A total of 1,289 households were visited during the first survey, and 3,601 households were visited in the four rounds of the second survey.
Study questionnaire.
A standardized questionnaire was used for each child contacted. The data collected through 60 questions included information about household and family composition, number of other children under the responsibility of the primary caregiver, the time of onset and clinical symptoms of the last episode of diarrheal disease (as described by primary caretakers), and the practices and attitudes of use of health services in the same episode. Distance from the health center as well as topologic barriers of healthcare use were also calculated and collected. Finally, information on the perception of respondents about the risk of diarrheal diseases in children and the importance of developing vaccines and other interventions against this disease were also collected. In the absence of episodes of diarrhea within 14 days before the interview, mothers or caretakers were also asked about their likely use of health centers should their children hypothetically develop diarrhea. For the second survey, the questionnaire was simplified to clinical spectrum, and certain questions were removed (socioeconomical status and information on the perception of respondents about the risk of diarrheal diseases in children).
Statistical analysis.
The analysis is based on the Global Enterics Multicenter Study (GEMS) Protocol regarding Healthcare Utilization and Attitudes Survey (HUAS). Briefly, analysis of data was performed using the Stata/SE software version 12.0 and its suite of survey data commands to account for stratified sample design and sampling weights. The survey was designed as a stratified random sample, with sex, age, and round (only for the second survey) as stratification factors. Sampling weights were constructed for each survey according to the DSS at CISM and applied to the sample data to produce accurate weighted population estimates. For each survey, we estimated the 2-week period prevalence of any diarrhea, moderate-to-severe diarrhea (MSD), proportion of diarrhea cases seeking care outside the home, and proportion of MSD cases seeking care at one of the designated GEMS case-control study sentinel health facilities; 95% confidence intervals (CIs) were calculated through Jackknife variance estimation.23 The χ2 test was used for differences in proportions, and linear regression models were estimated to compare means. Multivariate logistic regression was used for identifying the factors independently associated with healthcare-seeking behavior at a study health facility among children who had diarrhea in the last 2 weeks. The model estimated using a backward-stepwise procedure for selection of variables, with a removal criterion of P > 0.05 by Wald test. Variables used to estimate the multivariate model were all those variables that had a P value < 0.10 in the crude association and did not have empty cells by doing a cross-tabulation with the outcome variable.
Definitions.
Using the WHO protocol, diarrhea was defined as an increased frequency and volume and decreased consistency of stool from the norm.24 The presence of at least one of the following criteria, when reported by mothers or primary caretakers of children with diarrhea, defined an episode as MSD: (1) at least one of the following signs indicating MSD: sunken eyes significantly more than normal, wrinkled skin, or intravenous fluids administered at the health center (as referred by the mother in the interview), (2) dysentery (diarrhea with visible blood in stool), or (3) hospitalization for diarrhea or dysentery. Primary caretaker education was stratified in two groups: no formal education (no education or did not complete primary education) or some formal education (at least completed primary education).
Ethical considerations.
This study is part of a larger multicenter study conducted in six other developing countries investigating the etiology and epidemiology of diarrheal disease in infants and young children. The overall protocol and informed consent (obtained from the parents or legal guardians of minors) were both approved by the National Bioethics Committee of Mozambique (CNBS), the ethics committee of the Hospital Clinic of Barcelona, and the Institutional Review Board (IRB) at the University of Maryland.
Results
First survey.
A total of 1,059 households was included in the first survey (Table 1). Of these children, 389 children were aged 0–11 months, 319 children were ages 12–23 months, and 340 children were aged 24–59 months, representing 16%, 24%, and 60% of the DSS population, respectively. The male/female ratio of children included in the survey was 1:1. The interview respondent was the mother in 851 (77%) of households. Almost two-thirds (69%) of the primary caretakers did not complete primary school education. The vast majority (84%) of children lived in houses with cement floors. The mean number of people per family aggregate was seven, and the mean number of compartments in the household used to sleep was two. Almost 90% (958) of the caretakers would reach the hospital on foot, and among these caretakers, 449 (46%) needed over 30 minutes to get there. Ownership within aggregates of different variables defining the level of socioeconomic status included: telephone/mobile (60%), radio (50%), electricity (20%), bicycle (19%), television (18%), refrigerator/freezer (10%), and car/ truck (4%). One-fourth of the interviewed caregivers (25%) reported owning none of the above.
Table 1.
Characteristics of the children included in the two surveys
| Variables | 1° Survey n (%) | 2° Survey n (%) | ||
|---|---|---|---|---|
| Enrolled (N = 1,059) | DSS estimated population (N = 7,482) | Enrolled (N = 2,854) | DSS estimated population (N = 15,369) | |
| Age group (months) | ||||
| 0–11 | 400 (38) | 1,207 (16) | 880 (31) | 3,232 (21) |
| 12–23 | 319 (30) | 1,791 (24) | 973 (34) | 3,125 (20) |
| 24–59 | 340 (32) | 4,484 (60) | 1,001 (35) | 9,013 (59) |
| Sex | ||||
| Male | 547 (52) | 3,783 (51) | 1,448 (51) | 7,821 (51) |
| Female | 512 (48) | 3,699 (49) | 1,406 (49) | 7,548 (49) |
| Total diarrhea | 67 (6) | 321 (4) | 246 (9) | 1,027 (7) |
| Diarrhea with* | ||||
| Mucus/pus | 37 (55) | 172 (54) | – | – |
| Fever | 24 (36) | 109 (34) | 98 (40) | 428 (42) |
| Thirst | 26 (39) | 128 (40) | 85 (35) | 360 (36) |
| Rice watery stool | 9 (13) | 57 (18) | 108 (45) | 444 (44) |
| Sunken eyes | 16 (24) | 62 (19) | 74 (30) | 305 (30) |
| Vomits | 11 (16) | 42 (13) | 78 (32) | 327 (32) |
| Unable to drink | – | – | 72 (30) | 297 (29) |
| Lethargy/unconscious | 16 (24) | 64 (20) | 12 (5) | 53 (5) |
| Irritable/less play | – | – | 59 (24) | 250 (24) |
| Blood in stool | 4 (6) | 17 (5) | 18 (7) | 90 (9) |
| Wrinkled skin | 7 (10) | 23 (7) | 6 (2) | 26 (3) |
| Seek care outside home* | 44 (66) | 222 (69) | 125 (51) | 521 (51) |
| Sources of care seeking outside home† | ||||
| Healthcare use | 41 (93) | 208 (94) | 109 (87) | 449 (86) |
| Pharmacy | 3 (7) | 22 (10) | 3 (2) | 11 (2) |
| Unlicensed practitioner | 0 | 0 | 2 (2) | 13 (2) |
| Bought medicines | 1 (2) | 5 (2) | 3 (2) | 16 (3) |
| Traditional healer | 1 (2) | 3 (1) | 6 (5) | 21 (4) |
| Health use with age* (months) | ||||
| 0–11 | 20 (59) | 60 (59) | 51 (46) | 187 (46) |
| 12–23 | 15 (60) | 76 (60) | 45 (44) | 144 (44) |
| 24–59 | 6 (75) | 73 (79) | 13 (41) | 118 (41) |
Denominator: number of children with diarrhea.
Denominator: number of children who sought care outside home.
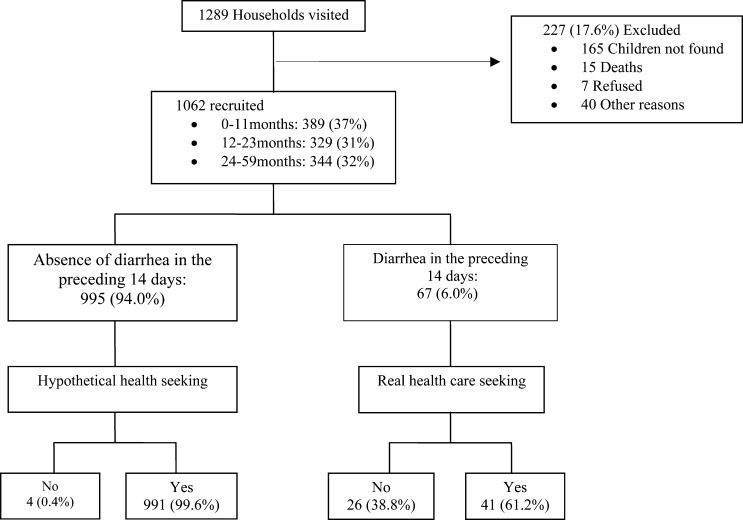
Diarrheal episode.
Of 1,062 children selected for inclusion, 67 caregivers (representing 4% of the DSS population) reported at least one episode of diarrhea during the 2 weeks before the interview. Of these 67 episodes, 21 (25%) were considered MSD. The mean duration of a diarrhea episode was 4 days, and 57 (85%) of the children had a maximum number of three to six loose stools per day (Figure 2). The most commonly reported symptoms during the diarrheal episodes were: mucus/pus in stool (54%), intense thirst (40%), fever (34%), lethargy (20%), and sunken eyes (19%). The risk of diarrhea decreased with increasing age (12–23 versus 0–11 months, odds ratio [OR] = 0.82, 95% CI = 0.48–1.42; 24–59 versus 12–23 months, OR = 0.29, 95% CI = 0.12–0.65; P = 0.002). There were no significant differences in symptoms according to age groups.
Figure 2.
Study profile. Diarrhea and its relation to health services use among Manhiça children (1° survey).
Attitudes and perceptions of diarrheal illness and healthcare-seeking behavior.
Mothers or primary caretakers were asked about the main factors that make a diarrheal episode severe, the defining manifestations of dehydration, and the type of preventive measures useful against diarrhea. The vast majority of the caretakers identified findings such as blood in stool (97%), stool increased frequency or decreased consistency (96%), vomiting (95%), rice watery stools (94%), or presence of dehydration (93%) as markers of severity accompanying a diarrheal episode. When enquired regarding defining manifestations of dehydration, the most common responses were the presence of sunken eyes (43%), thirst (43%), wrinkled skin (34%), decreased urinary frequency (33%), and lethargy (29%). Washing hands (45%), clean food or water (39%), and proper disposal of human waste (26%) were the most commonly identified measures for preventing diarrhea. There were no significant differences in the prevalence of reported diarrhea according to the knowledge of markers of dehydration, severity, or measures to prevent diarrhea. The vast majority of primary caretakers (98%) reported that vaccines are important for child's health and that they would be willing to use them, if available, to prevent any kind of diarrhea. Most parents (85%) reported no problems in accessing health systems, but among those parents stating the contrary, the most frequent included the presence of long lines at the hospital (8%) and the lack of transportation to get there (7%).
Care-seeking behavior outside the home and healthcare-seeking behavior.
Of those caretakers reporting diarrhea during the recall period, 41 (65.2%, 95% CI = 51.9–78.4) of the primary caretakers reported seeking care at sentinel health facilities; this proportion increased to 85.9% (95% CI = 69.6–102.1) among those caretakers with children with MSD. Sentinel health facilities were the main sources of care seeking outside the home for diarrheal disease. Other sources of care seeking outside the home included going to the pharmacy (3; 10%), directly buying medicines at shop/market (1; 2%), or using a traditional healer (1; 1%). Mothers made the decision to go to the hospital in 84% of the households, and about 39% of the diarrhea cases sought care in the first day of diarrhea. Healthcare use rose with increasing age: 58.8% (95% CI = 41.8–75.9) for children ages 0–11 months, 60.0% (95% CI = 39.8–80.2) for children ages 12–23 months, and 79.2% (95% CI = 46.1–112.2) for children ages 24–59 months. Impression of parents or primary caretakers that their children did not seem to need care was the main cause of not seeking care outside home.
According to the multivariate model, the following variables were independently associated with use of health services: the presence of diarrhea with fever (OR = 4.69, 95% CI = 1.25–17.52, P = 0.022) and not knowing any sign of dehydration (OR = 15.08, 95% CI = 1.56–145.43, P = 0.020). Contrarily, having a television at home (OR = 0.21, 95% CI = 0.05–0.84, P = 0.029) was independently associated with a decreased use of the health facilities. There was no association between consultations at a healthcare structure and the level of education of the caretaker, distance to that health structure, adequate knowledge by the caretakers of the manifestations that define severe diarrheal disease, or adequate understanding of the necessary preventive measures against diarrhea. Other sources of care-seeking behavior were not significantly associated with any diarrheal disease (data not shown).
Treatment and fluid administration.
Almost one-half of the children (29; 43%) did not receive any treatment at home before seeking care at the health center. However, among those caretakers administering treatments before going to hospital, herbal medication (30%) and oral rehydration salt (27%) were the most frequent referred treatments. When we enquired about “how much was offered to the child to drink during the diarrhea illness,” it was found that 11 (12%) of the mothers reduced or stopped their child's usual liquid/breast milk intake, 47 (73%) of the mothers maintained the usual amount of liquid or breast milk, and only 9 (16%) of the mothers gave an increased amount of liquid or breast milk to their children with diarrhea. Although not significant (P = 0.082), these differences were more markedly noticeable in the youngest age group (infants), which were offered fewer liquids in relation to the older age groups. Only seven (12%) children with diarrhea were hospitalized. Among all patients who sought care in health services on account of their diarrheal episode, 32 (48%) received oral rehydration solution, 13 (14%) received antibiotics, 8 (9%) received intravenous rehydration, and 16 (26%) received other different treatments.
Hypothetical health-seeking behavior.
All primary caretakers whose child did not have diarrhea during the preceding 2 weeks were asked about their likely use of health centers should their children hypothetically develop diarrhea, and almost all respondents (991/995; 99%) stated that they would seek medical attention for any diarrheal episode. Commonly referred sources of healthcare seeking outside the household in that group were the health center/hospital (75–99%) or the traditional healer (0.1–13%). Relatively few children would be taken to the pharmacy (0.4–9.0%) or a friend (0.1–1%). The answers were similar, regardless of whether the putative diarrhea was with or without blood (data not shown).
Second survey.
A total of 2,854 households was included in the second survey (Table 1); 880 children ages 0–11 months, 973 children ages 12–23 months, and 1,001 children ages 24–59 months represented 21%, 20%, and 59% of the DSS population, respectively. The male/female ratio of children included in the survey was 1. Of 2,854 children selected for inclusion, 246 caregivers (representing 7% of the DSS population) reported at least one episode of diarrhea during the recall period of 2 weeks. Of these 246 episodes, 103 (42%) episodes were considered MSD. The mean duration of a diarrhea episode was 4 days, and 213 (85%) of the children had a maximum number of three to six loose stools per day. The most common reported symptoms during the diarrhea episode were rice watery stool (44%), fever (42%), intense thirst (36%), vomiting (32%), and sunken eyes (30%). The risk of diarrhea decreased with increasing age (12–23 versus 0–11 months, OR = 0.82, 95% CI = 0.62–1.09; 24–59 versus 12–23 months, OR = 0.28, 95% CI = 0.19–0.42; P < 0.0001).
Of those caretakers reporting diarrhea during the recall period, 21 (41.5%, 95% CI = 25.9–57.1) in the first round, 36 (44.7%, 95% CI = 32.1–57.2) in the second round, 11 (43.6%, 95% CI = 22.1–65.1) in the third round, and 41 (44.0%, 95% CI = 32.9–55.1) in the fourth round used the health structures. Healthcare use increased in case of MSD to 51.8% (95% CI = 25.9–77.7) in the first round, 59.0% (95% CI = 41.6–76.5) in the second round, 70.6% (95% CI = 25.2–116.0) in the third round, and 54.2% (95% CI = 35.5–73.0) in the fourth round. Overall, healthcare use was 43.8% (95% CI = 36.9–50.6) and 56.9% (95% CI = 46.2–67.7) for total diarrhea and MSD, respectively. About 25% of the diarrhea cases sought care in the first day of diarrheal illness. Only two (1%) children with diarrhea were hospitalized. Impression of parents or primary caretakers that their children did not seem to need care was again the main cause of not seeking care outside home. Other sources of care seeking outside the home included seeing a traditional healer (6; 4%), directly buying medicines at shop/market (3; 3%), going to the pharmacy (3; 2%), and seeing an unlicensed practitioners (2; 2%).
Table 2 describes factors independently associated with seeking healthcare at a health center or hospital. The use of health services was significantly associated with diarrhea with fever (OR = 1.88, 95% CI = 1.01–3.51, P = 0.046) and vomiting (OR = 2.78, 95% CI = 1.53–5.08, P < 0.001). Once again, other sources of care seeking were not significantly associated with any diarrheal disease.
Table 2.
Factors independently associated with the use of health services in a multivariate adjusted analysis
| Variables | Multivariate analysis | |||
|---|---|---|---|---|
| OR | 95% CI | P value | ||
| Lower | Upper | |||
| 1° Survey | ||||
| Diarrhea with fever | 4.69 | 1.25 | 17.52 | 0.022 |
| Not knowing any sign of dehydration | 15.08 | 1.56 | 145.43 | 0.020 |
| Having television at home | 0.21 | 0.05 | 0.84 | 0.029 |
| 2° Survey | ||||
| Diarrhea with fever | 1.88 | 1.01 | 3.51 | 0.046 |
| Diarrhea with vomiting | 2.78 | 1.53 | 5.08 | < 0.001 |
When enquired about “how much was offered to the child to drink during the diarrhea illness,” it was found that the majority (193; 79%) of the mothers reduced or stopped the child's usual liquid/breast milk intake, whereas 3 (1%) caretakers maintained the usual amount of liquid or breast milk; only 49 (20%) caretakers provided an increased amount of liquid or breast milk to the children with diarrhea. Among all patients with a diarrheal episode, 136 (55%) received oral rehydration solution, 34 (16%) received home fluids, and 69 (28%) received no treatments. Within the preceding 14 days, the majority (185; 77%) of the children with diarrhea had improved, whereas some (6; 23%) continued with diarrhea.
Discussion
The use of health services in case of illness is a complex behavior influenced by norms, moral values, beliefs, preferences, and socioeconomic potential as well as the perceived need of the users. Understanding the determinants of healthcare use in a determined population regarding specific illnesses may, therefore, provide useful information to improve their prognosis.
The study observed that, despite health access challenges in a rural area such as Manhiça, health services are used regularly from an early age by almost one-half (46–59%) of the children in their first year of life. However, these frequencies were lower than those numbers reported among children younger than 12 months of age (68.4%) in the general population of Mozambique in relation to the three most common infectious diseases together, namely malaria, diarrhea, and respiratory infections.25
In the first survey, the final model of health services use was independently associated with diarrhea with fever, an easily recognized sign in a malaria-endemic region. This result is something expected and consistent with previous studies regarding the use of health services, which indicate that the main determinant of the use of services is the perceived need.26,27 However, high education, which has been described to be an important determinant of health service use,28 was not shown to directly affect healthcare use when controlled by other cofounders. This result could be explained by the fact that, in Mozambique, the promotion campaigns of healthcare use are largely accomplished through the mass media (radio), and in Manhiça district particularly, healthcare use promotion is increased during DSS activities. Promotion campaigns consist of explaining to caretakers about problems that endanger life for the most prevalent diseases, such as malaria, acquired immunodeficiency syndrome (AIDS), and diarrhea, to serve as a warning. Thus, “not knowing any sign of dehydration,” a variable that may be associated with lower education, was found to be associated with increased healthcare use, possibly as a result of a lower capacity of the primary caretakers to perceive illness severity and monitor sick children, which may cause more severe episodes that require health center use. Contrarily, having television at home, a higher socioeconomic level variable, was associated with a marked decrease in the use of health services, suggesting that residents with high income have a tendency to use healthcare sources other than those sources provided by the national public system.
One of the main objectives of the second survey was to determine the proportion of care-seeking behavior from the DSS healthcare for MSD. Similar to the first survey, determinants of MSD were not associated to healthcare use. The use of health services was significantly associated with diarrhea with vomiting and fever. Vomiting was one of the most frequently reported symptoms by caretakers as a marker of disease severity in relation to the diarrheal episode, suggesting that it is widely used in the community as a red flag for diarrhea requiring urgent care.
In both the first and second surveys, the health structures were the main source of healthcare. Moreover, the other sources of care seeking were not significantly associated with any diarrhea, suggesting that the population considers DSS healthcare as the primary source of treatment of diarrhea. However, one must not minimize the misuse of over-the-counter medication and the potential role of traditional healers. Although their use was found to be low, the traditional healers are known to be the suppliers of herbal medication, which usually, is the first home treatment given to the child with diarrhea. The knowledge of the potential benefits or risks of some herbal medicines used in the community is still limited, and such treatments may even be detrimental to the diarrhea episode. This finding underlines the necessity for better communication between health professionals and caregivers regarding the use of herbal therapy29,30 or any other medication without medical prescription. Future studies on the determinants of seeking care outside home and healthcare use among patients with diarrhea should investigate the above associations and local practices to further clarify the main determinants of healthcare use in rural communities such as Manhiça.
It is also remarkable that the vast majority of patients without episodes of diarrhea reported that they would use health services, possibly conditioned by the fact that the community associated the study interviewers with hospital staff. For this reason, the prevalence of the hypothetical use was almost 100%, thus precluding any analyses of risk factors associated with the hypothetical use. Although this result probably induced a significant response bias, it should be noted that the proportion of patients with MSD episodes who really used the health services was considerably high (86%) in any case.
The low prevalence of diarrhea found in this study (4.0–7.0% of patients enrolled) in a tropical country where diarrhea has been described as one of the major causes of pediatric morbidity and mortality is striking, but it is in line with other important decreasing trends for other important morbidity causes in the DSS area.12,16,31 However, it should be noted that, although each round of the second survey took 3–5 months and involved all DDS area, the first survey was restricted to a small study area, and additionally, it was performed between May and June, a cold and dry period, in which the prevalence and incidence of diarrhea in the area are lower than during the rest of the year. The results of diarrhea history characteristics are consistent with the literature.32,33
In children, reduction of the usual diet intake is a common but not recommended practice during any diarrheal episode. The WHO recommends increasing the amount of liquid during diarrhea to avoid dehydration.34,35 Despite the considerable knowledge of the manifestations of dehydration and diarrhea severity by caretakers, according to our findings, liquid intake did not seem encouraged at the community level during a diarrheal episode, something that was even more markedly pronounced among infants than older children. Moreover, additional administration of oral rehydration salt was not commonly referred as the first home treatment of children with diarrhea in the first survey, but it was the first home treatment in the second survey. These fundamental perception mistakes regarding diarrhea management need to be urgently addressed. The promotion of breastfeeding and/or increased liquid intake during a diarrheal episode, plus the addition of oral rehydration salts as supporting medication, should become an essential part of any community-based training program to improve the prognosis of diarrheal disease.
It seems pertinent to make some methodological observations from the analysis of the strengths and limitations of this study that should be taken into account in the design of subsequent studies. The biggest strength was the continuous prospective monitoring realized in the second survey that revealed lower prevalence (43.75%) of healthcare use compared with the finding of the first cross-sectional study (65.16%); however, no important variation of healthcare use was seen during the continuous monitoring. Limitations of the study include the fact that a cross-sectional study design involves the measurement of cause and effect at the same time, introducing the problem of temporal ambiguity in establishing causal relationships, and a reporting bias related to the presence of the researcher, conditioned by the hypothetical relationship between the interviewers and paramedical staff. Finally, because of the characteristics of the sample in the first survey (small sample size in the group of children who had diarrhea and the small number of events in a category of the dependent variable hypothetical use), consideration of the hypothetical effect between variables (interactions) could not be analyzed; furthermore, it led to large 95% CIs that do not allow highly accurate estimates.
Limitations aside, it is possible to conclude that the use of national health services in case of diarrhea in children under 5 years is fundamentally associated with the perceived need; lower knowledge of dehydration signs and may be hampered by economic status. Community knowledge of the disease, its manifestations, and the risk factors associated with severity seemed adequate, contrary to the knowledge regarding best practices to treat such episodes, such as, for instance, the recommendation of increasing liquid intake. Understanding determinants of health services use may help to improve health planning. Additionally, the establishment of continuous prospective monitoring allows accounting for changes in healthcare use that may occur because of seasonality or secular events.
ACKNOWLEDGMENTS
The authors thank all study participants (children and caretakers) and all workers of the Centro de Investigação em Saúde da Manhiça for their help in obtaining the data, and the Centre for International Health Research in Barcelona and Center for Vaccine Development, University of Maryland School of Medicine for encouraging the realization of this project. The authors also thank the district health authorities for their collaboration in the research activities ongoing in the Manhiça district. The authors finally thank the Gulbenkian Foundation grant for predoctoral research to the corresponding author (T.N.).
Footnotes
Financial support: This work was supported by the Bill & Melinda Gates Foundation.
Authors' addresses: Tacilta Nhampossa, Inacio Mandomando, Sozinho Acacio, Delino Nhalungo, Charfudin Sacoor, Ariel Nhacolo, Eusebio Macete, and Arnaldo Nhabanga, Centro de Investigação em Saúde de Manhiça, Maputo, Mozambique, E-mails: taciltanha@yahoo.com, inacio.mandomando@manhica.net, sozinho.acacio@manhica.net, delino.nhalungo@manhica.net, charfudin.sacoor@manhica.net, ariel.nhacolo@manhica.net, Eusebio.Macete@manhica.net, and arnaldo.nhabanga@manhica.net. Llorenç Quintó, Barcelona Centre for International Health Research, Hospital Clínic, University of Barcelona, Barcelona, Spain, E-mail: LQUINTO@clinic.ub.es. Karen Kotloff, Myron M. Levine, Dilruba Nasrin, and Tamer Farag, Center for Vaccine Development, University of Maryland School of Medicine, Baltimore, MD, E-mails: kkotloff@medicine.umaryland.edu, Mlevine@medicine.umaryland.edu, dnasrin@medicine.umaryland.edu, and tfarag@medicine.umaryland.edu. Quique Bassat, Barcelona Institute for Global Health, Barcelona Centre for International Health Research, Hospital Clínic, University of Barcelona Carrer Rosello, Barcelona, Spain, E-mail: quique.bassat@cresib.cat. Pedro Alonso, Barcelona Institute for Global Health, Barcelona Centre for International Health Research, Hospital Clínic, University of Barcelona Carrer Rosello, Barcelona, Spain, and Centro de Investigação em Saúde de Manhiça, Maputo, Mozambique, E-mail: pedro.alonso@isglobal.org.
References
- 1.UNICEF/WHO . Diarrhoea: Why Children Are Still Dying and What Can Be Done. New York, NY: UNICEF/WHO; 2009. [Google Scholar]
- 2.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Liu L, Mathers C. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2008;375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 3.Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bull World Health Organ. 2003;81:197–204. [PMC free article] [PubMed] [Google Scholar]
- 4.Boschi-Pinto C, Velebit L, Shibuya K. Estimating child mortality due to diarrhoea in developing countries. Bull World Health Organ. 2008;86:710–717. doi: 10.2471/BLT.07.050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boschi-Pinto C, Lanata CF, Black RE. The global burden of childhood diarrhea. In: Ehiri J, editor. Maternal and Child Health: Global Challenges, Programs and Policies. Boston, MA: Springer Science+Business Media, LLC; 2009. pp. 225–243. [Google Scholar]
- 6.Bern C, Martines J, de Zoysa I, Glass RI. The magnitude of the global problem of diarrhoeal disease: a ten-year update. Bull World Health Organ. 1992;70:705–714. [PMC free article] [PubMed] [Google Scholar]
- 7.MISAU . Health Sector Strategic Plan. Maputo: Ministério da Saúde location; 2009. [Google Scholar]
- 8.Lindelow MWP, Zorzi N. Primary Health Care in Mozambique: Service Delivery in a Complexy Hierarchy. New York, NY: UNICEF/WHO; 2004. [Google Scholar]
- 9.UNICEF . Mozambique: National Mortality Child Study. New York, NY: UNICEF/WHO; 2009. [Google Scholar]
- 10.World Health Organization . Accelerated Child Survival and Development. Geneva: WHO; 2010. http://www.unicef.org/mozambique/pt/child_survival.html Available at. [Google Scholar]
- 11.Dgedge M, Novoa A, Macassa G, Sacarlal J, Black J, Michaud C, Cliff J. The burden of disease in Maputo City, Mozambique: registered and autopsied deaths in 1994. Bull World Health Organ. 2001;79:546–552. [PMC free article] [PubMed] [Google Scholar]
- 12.Sacarlal J, Nhacolo AQ, Sigauque B, Nhalungo DA, Abacassamo F, Sacoor CN, Aide P, Machevo S, Nhampossa T, Macete EV, Bassat Q, David C, Bardaji A, Letang E, Saute F, Aponte JJ, Thompson R, Alonso PL. A 10 year study of the cause of death in children under 15 years in Manhica, Mozambique. BMC Public Health. 2009;9:67. doi: 10.1186/1471-2458-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Machava JR. Situation of Poverty in Mozambique: Regional Differences and Main Challenges. São Paulo: Estudos Geográficos, Rio Claro; 2007. pp. 27–46. [Google Scholar]
- 14.INE, Instituto Nacional de Estadísticas Country Data Portal Mozambique. 2012. http://www.ine.gov.mz Available at. Accessed June 14, 2012.
- 15.Saute F, Aponte J, Almeda J, Ascaso C, Vaz N, Dgedge M, Alonso P. Malaria in southern Mozambique: incidence of clinical malaria in children living in a rural community in Manhica district. Trans R Soc Trop Med Hyg. 2003;97:655–660. doi: 10.1016/s0035-9203(03)80097-4. [DOI] [PubMed] [Google Scholar]
- 16.Guinovart C, Bassat Q, Sigauque B, Aide P, Sacarlal J, Nhampossa T, Bardaji A, Nhacolo A, Macete E, Mandomando I, Aponte JJ, Menendez C, Alonso PL. Malaria in rural Mozambique. Part I: children attending the outpatient clinic. Malar J. 2008;7:36. doi: 10.1186/1475-2875-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bassat Q, Guinovart C, Sigauque B, Mandomando I, Aide P, Sacarlal J, Nhampossa T, Bardaji A, Morais L, Machevo S, Letang E, Macete E, Aponte JJ, Roca A, Menendez C, Alonso PL. Severe malaria and concomitant bacteraemia in children admitted to a rural Mozambican hospital. Trop Med Int Health. 2009;14:1011–1019. doi: 10.1111/j.1365-3156.2009.02326.x. [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez R, Munguambe K, Aponte J, Bavo C, Nhalungo D, Macete E, Alonso P, Menendez C, Naniche D. High HIV prevalence in a southern semi-rural area of Mozambique: a community-based survey. HIV Med. 2012;13:581–588. doi: 10.1111/j.1468-1293.2012.01018.x. [DOI] [PubMed] [Google Scholar]
- 19.Bassat Q, Machevo S, O'Callaghan-Gordo C, Sigauque B, Morais L, Diez-Padrisa N, Ribo JL, Mandomando I, Nhampossa T, Ayala E, Sanz S, Weber M, Roca A, Alonso PL. Distinguishing malaria from severe pneumonia among hospitalized children who fulfilled integrated management of childhood illness criteria for both diseases: a hospital-based study in Mozambique. Am J Trop Med Hyg. 2011;85:626–634. doi: 10.4269/ajtmh.2011.11-0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nhacolo A, Nhalungo D, Sacoor C, Aponte J, Thompson R, Alonso P. Levels and trends of demographic indices in southern rural Mozambique: evidence from demographic surveillance in Manhica district. BMC Public Health. 2006;6:291. doi: 10.1186/1471-2458-6-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alonso P, Saúte F, Aponte JJ, Gómez-Olive FX, Nhacolo A, Thompson R, Macete E, Abacassamo F, Ventura PJ, Bosch X, Menendez C, Dgedge M. Manhiça Demographic Surveillance System, Mozambique . Population, Health, and Survival at INDEPTH Sites 1 1969–87. Ottawa: International Development Research Centre (IDRC); [Google Scholar]
- 22.WHO . Generic Protocols for: I) Hospital-Based Surveillance to Estimate the Burden of Rotavirus Gastroenteritis in Children and II) a Community-Based Survey on Utilization of Health Care Services for Gastroenteritis in Children. Geneva: WHO; 2002. [Google Scholar]
- 23.Blackwelder WC, Biswas K, Wu Y, Kotloff KL, Farag TH, Nasrin D, Graubard BI, Sommerfelt H, Levine MM. Statistical methods in the Global Enteric Multicenter Study (GEMS) Clin Infect Dis. 2012;55((Suppl 4)):S246–S253. doi: 10.1093/cid/cis788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morris SS, Cousens SN, Lanata CF, Kirkwood BR. Diarrhoea—defining the episode. Int J Epidemiol. 1994;23:617–623. doi: 10.1093/ije/23.3.617. [DOI] [PubMed] [Google Scholar]
- 25.Lindelow M. The utilisation of curative healthcare in Mozambique: does income matter? J Afr Econ. 2005;14:435–482. [Google Scholar]
- 26.Taffa N, Chepngeno G. Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop Med Int Health. 2005;10:240–245. doi: 10.1111/j.1365-3156.2004.01381.x. [DOI] [PubMed] [Google Scholar]
- 27.Field KS, Briggs DJ. Socio-economic and locational determinants of accessibility and utilization of primary health-care. Health Soc Care Community. 2001;9:294–308. doi: 10.1046/j.0966-0410.2001.00303.x. [DOI] [PubMed] [Google Scholar]
- 28.Buor D. Mothers' education and childhood mortality in Ghana. Health Policy. 2003;64:297–309. doi: 10.1016/s0168-8510(02)00178-1. [DOI] [PubMed] [Google Scholar]
- 29.Rodriguez-Fragoso L, Reyes-Esparza J, Burchiel SW, Herrera-Ruiz D, Torres E. Risks and benefits of commonly used herbal medicines in Mexico. Toxicol Appl Pharmacol. 2008;227:125–135. doi: 10.1016/j.taap.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Araz N, Bulbul S. Use of complementary and alternative medicine in a pediatric population in southern Turkey. Clin Invest Med. 2001;34:E21–E29. doi: 10.25011/cim.v34i1.14909. [DOI] [PubMed] [Google Scholar]
- 31.Bassat Q, Guinovart C, Sigauque B, Aide P, Sacarlal J, Nhampossa T, Bardaji A, Nhacolo A, Macete E, Mandomando I, Aponte JJ, Menendez C, Alonso PL. Malaria in rural Mozambique. Part II: children admitted to hospital. Malar J. 2008;7:37. doi: 10.1186/1475-2875-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pickering LK. Gastroenteritis. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson Tratado de Pediatrita. Madrid: Elservier editorial; 2004. pp. 1272–1276. [Google Scholar]
- 33.Oliveira RG. Belo Horizonte: Blach Book Pediatria. Belo Horizonte: Blackbook editora; 2005. pp. 295–308. [Google Scholar]
- 34.Suh JS, Hahn WH, Cho BS. Recent advances of oral rehydration therapy (ORT) Electrolyte Blood Press. 2010;8:82–86. doi: 10.5049/EBP.2010.8.2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gutierrez G, Tapia-Conyer R, Guiscafre H, Reyes H, Martinez H, Kumate J. Impact of oral rehydration and selected public health interventions on reduction of mortality from childhood diarrhoeal diseases in Mexico. Bull World Health Organ. 1996;74:189–197. [PMC free article] [PubMed] [Google Scholar]