Abstract
Maternal practices regarding children's health care have been recognized as an important factor associated with mortality rates among children < 5 years of age. We focused on health care-seeking practices of primary caretakers of children < 5 years of age with diarrheal disease in Kolkata. We interviewed caretakers of 1,058 children in a baseline survey and 6,077 children on six subsequent surveys. The prevalence of diarrhea during the preceding 2 weeks was 7.9% in the baseline survey and 5.7% (lowest 3.5% to highest 7.8%) in subsequent surveys. Multivariate logistic regression showed that formal education of primary caretakers was associated with seeking care outside the home (odds ratio [OR] = 15.5; 95% confidence interval [CI] [2.5–85.7]; P = 0.002). Multinomial logistic regression showed that formal education of the primary caretaker (OR = 21.4; 95% CI [3.2–139.0]; P = 0.002) and presence of dry mouth during diarrhea (OR = 17.3; 95% CI [2.7–110.9]; P = 0.003) were associated with seeking care from licensed providers compared with the children for whom care was not sought outside of the home. This health care utilization and attitudes survey (HUAS) can serve as a tool to identify the factors that influence a better health care-seeking pattern in urban slums of Kolkata.
Introduction
In most developing countries there is insufficient investment in public health activities, and there is a need for improved health policies. A thorough understanding of the health care-seeking behavior of a population and its use of resources and expenditures on health services is needed to guide improved practices toward reducing disease burden. Several studies in India regarding health care-seeking practices have focused on household health expenditures.1–3 To formulate an effective and pertinent health policy, prior in-depth knowledge of diseases of public health importance is needed, and understanding the caretakers' perceptions about the disease itself. The attitudes and practices of parents and caretakers toward a disease vary with their perception about its seriousness (especially for young children)4; this work focuses on diarrheal diseases and health care-seeking practices of the primary caretakers of children < 5 years of age.
Diarrhea is a leading cause of childhood morbidity and mortality and holds the second rank (after pneumonia) for mortality in children < 5 years of age, despite the advances in case management and diagnostic technologies over the last decades.5,6 Diarrheal deaths accounted for ∼15% of the global estimated 8.7 million under-five deaths.7 In India, pneumonia and diarrhea account for 50% of the under-five deaths.8 Inability of caretakers to recognize early signs of dehydration and improper management results in gross fluid loss and electrolyte imbalance, which contribute to fatal outcomes. The majority of these deaths can be averted by timely intervention with oral rehydration therapy and continued feeding practices.9
Caretakers play a pivotal role in managing childhood illness.10 Maternal practices regarding children's health care have been recognized as an important factor behind mortality rates among children < 5 years of age.11 Timely care seeking for diarrheal disease is positively related to survival.12 Some studies have evaluated health care-seeking behavior and health care use among mothers in developing countries in relation to diarrheal diseases,13 and identified various factors that influence the seeking of health care services for diarrheal diseases.14 The perception of caretakers about the severity of diarrheal illness ultimately affects the decision for seeking treatment and influences the type of therapies received.15 Achieving Millennium Development Goal-4 of reducing child mortality by two-thirds by the year 2015 requires evidence-based intervention to reduce burden of childhood illnesses.16
An understanding of health care practices is essential for the rational planning of health care services. Data on factors that affect slum dwellers' child health care-seeking practices in India are scarce. As part of the Global Enteric Multicenter Study (GEMS), we conducted a comprehensive health care utilization and attitude survey (HUAS) in 2007, followed by a series of abbreviated surveys (HUAS-lite) during 2009 and 2010. In the initial baseline comprehensive survey we assessed caretakers' knowledge, attitude, and health care-seeking behavior for diarrhea in a young child. The abbreviated surveys provided diarrhea prevalence and care-seeking patterns over time. The data on clinic use by diarrheal syndrome will be used to adjust incidence data from surveillance for diarrheal disease conducted in sentinel health centers.
Materials and Methods
Study site and study population.
Kolkata, capital of the State of West Bengal in India, is divided into 15 boroughs and 141 wards (administrative units) under the Kolkata Municipal Corporation (KMC) area. It has been estimated that 40% of the total population of Kolkata lives in 5,500 overcrowded slum areas (Census of India 2001) where they do not have proper access to basic amenities including water and sanitation.
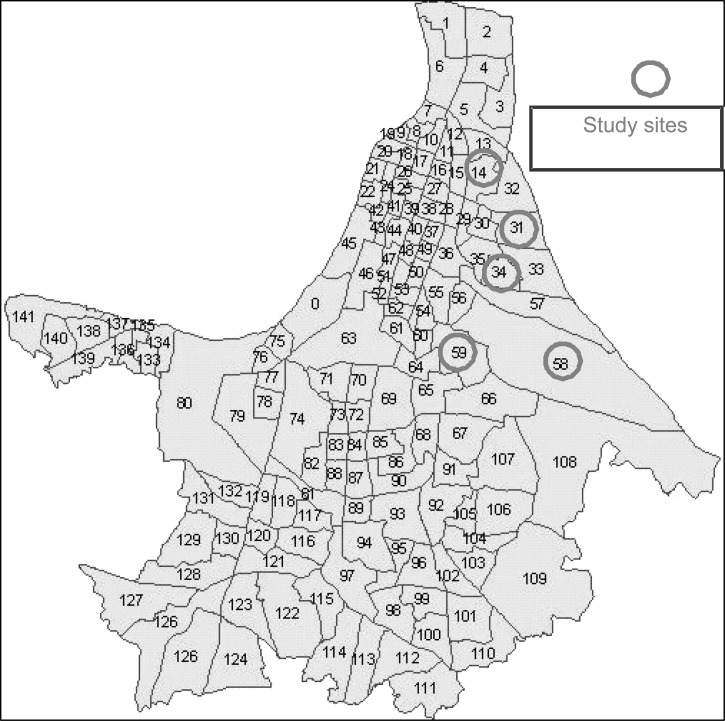
A demographic surveillance system (DSS) was established for GEMS to provide a longitudinal vital events registration program in which each household in the defined geographic area was visited three times per year to record births, deaths, pregnancies, and migrations. The study area includes bustees, which are legally recognized, registered slums within Wards 14, 31, 34, 58, and 59 in the eastern part of Kolkata Municipal Corporation (Figure 1); the bustees are typical of their counterparts in other parts of the city. Streets are narrow with little space between houses, piped municipal water supply is intermittent, and several households share one or two latrines and water taps. At times the households are faced with extreme scarcity of water and overcrowded sanitary facilities. Most sewage is collected in open gutters that overflow during the rainy season. The underground water and sewage pipelines lie close to each other and are prone to leakage and contamination resulting in outbreaks. The median monthly household expenditure is Indian Rupees (INR) 3,000 or US$ 67.17 Some factors known to enhance the transmission of diarrheal pathogens such as unhygienic personal health practices, sharing of toilets, and the lack of proper hand washing practices are prevalent.18 Selling of prepared food and cut fruits, etc., is widely practiced and toddlers and young children, as well as adults, consume them regularly.
Figure 1.
Study site: Map of the Kolkata Municipal Corporation.
Immunization is conducted at the government and municipal clinics, free of cost and in accordance with the schedule of the Expanded Program of Immunization in India (EPI). Apart from the EPI schedules, pulse polio administration is being carried out in these areas following the national and sub-national immunization programs for under-5 children.
The data for this study have been obtained as part of the on-going collaborative GEMS project, which aims to estimate the burden, causes, and sequelae of diarrheal disease among young children, a collaborative study of the National Institute of Cholera and Enteric Diseases (ICMR) and Center for Vaccine Development, University of Maryland, Baltimore, MD. Of the total 194,172 population from the census conducted during December 2006 and January 2007, 12,548 were children < 5 years of age.
Sampling frame for HUAS and HUAS-lite surveys.
Many of the HUAS methods were adapted from a Generic Protocol published by the World Health Organization for performing community-based surveys to estimate the use of health care services for gastroenteritis for children < 5 years of age.19 For the HUAS survey, the computerized program randomly selected ∼400 children from the 0- to 11-month age group and 370 from each of the two older age strata (12–23 months and 24–59 months) using the updated census list with the aim of having 333 children in each age group for analysis. The purpose of starting out with a larger sample was to allow for refusal and children who are on the list but are not actually eligible for the HUAS. Possible reasons for ineligibility included aging out of the age group for which the list was prepared, a child no longer living or miscoded as living in the HUAS area, death of a child, and errors in the census and/or surveillance.
For HUAS-lite, we used a shorter version of the HUAS questionnaire that asked questions about the child's diarrhea history and care seeking for diarrhea. The surveys were conducted at 4-month intervals in conjunction with the routine demographic surveillance. During the study period, six rounds of HUAS-lite were conducted from February 2009 to December 2010. The main purpose of this HUAS-lite survey was to estimate the prevalence of all diarrhea and moderate-to-severe diarrhea (MSD), considering temporal variation and the proportion of children who sought care at the four GEMS sentinel health centers for treatment of MSD. The MSD was defined as an acute diarrheal episode with three or more abnormally loose stools within the last 24 hours, and at least one of the following observations by the caretaker: sunken eyes (more than usual), wrinkled skin, receipt of intravenous rehydration, visible blood in stool, or hospitalization for diarrhea.
Questionnaire and survey methods, sample size, data management, and statistical tests.
The standardized questionnaire and survey methods, sample size calculation, data entry, data management, and statistical analysis methods are all described in depth in the Overview article.20 We defined “formal education” as a minimum of completed primary school education. Briefly, statistical analysis was carried out using the survey modules in STATA v12.0 (STATA, College Station, TX) and R for quintiles and censored data analysis. In calculating the overall percentages and 95% confidence intervals (CIs), site-specific sampling weights were used; the weights were defined from the DSS population and the number of HUAS participants for each combination of age groups (0–11, 12–23, and 24–59 months) and sex.20 The χ2 test was used to compare categorical variables. Poisson regression with jackknife standard errors21 was used to produce prevalence ratios and 95% CIs. Adjustments for multiple comparisons were not performed.
Independent variables (age stratum, gender of the child, primary caretaker's education, and clinical signs and symptoms) were examined by the χ2 test for any association with multi-category-dependent variables (primary caretakers' health care-seeking practices). The data were examined in two ways. The outcome variable, i.e., seeking care for a child's diarrheal illness, has been dichotomized (no care versus care sought from outside the home). Binary logistic regression for survey data were used to estimate weighted adjusted odds ratios with 95% CIs using the Wald P-value. Thereafter, multivariate survey logistic regression was applied to identify the factors associated with care-seeking behavior, controlling the other variables. As “care-seeking outside home” is a much broader term, it was subdivided into two categories: 1) care from unlicensed providers including pharmacy, and 2) care from a licensed provider. Licensed care providers were defined as practitioners having formal medical education, and a degree from a recognized institution. Unlicensed health care providers included traditional healers, providers without any formal degree, untrained providers, and pharmacists. Multinomial survey logistic regression was thereupon performed to assess the effect of independent variables to health-seeking behavior for unlicensed providers and licensed providers compared with no care.
Ethical review and informed consent.
The study protocol was approved by the NICED Institutional Ethics Committee and by The Institutional Review Board (IRB) of the University of Maryland, Baltimore, MD. Written informed consent for the interview was obtained from the mothers or other primary caretakers. The HUAS questionnaire is the main source of information.
Results
Results from baseline HUAS.
The baseline HUAS was conducted during April–August 2007. A total of 1,140 children were randomly selected for the survey. Of the 1,140 selected children, caretakers of 1,058 (92.8%) were interviewed. The characteristics of the participating households and the nature of the diarrheal illnesses that their children experienced during the preceding 2 weeks are presented in Table 1. Among the caretakers interviewed, the overwhelming majority 1,023 (96.6%) were the child's mother. Nearly all children (98.9%) lived with their mothers, and 96.5% lived with both parents. Most of the primary caretakers (63.5%) had some degree of formal education, having completed at least primary school. The median number of members of the household was five (ranging in age from 2 to 20 years). Most homes (94.5%) had a finished floor, i.e., polished with wood/cement/ceramic tiles.
Table 1.
Household characteristics of children and primary caretakers (N = 1058) in the baseline Health Care Utilization and Attitudes Survey (HUAS)
| Characteristics | N (weighted %)* |
|---|---|
| Children age stratum (in months) | |
| 0–11 | 427 (15.4) |
| 12–23 | 297 (20.0) |
| 24–59 | 334 (64.6) |
| Gender of child | |
| Female | 511 (48.6) |
| Mothers interviewed as primary caretaker of the child | 1023 (96.6) |
| Mother lives in the household | 1050 (98.9) |
| Both Parents live in the household | 1025 (96.5) |
| Primary caretaker completed primary school or above | 685 (63.5) |
| Household with finished floor | 999 (94.5) |
| Perception of primary caretaker about the symptoms to see if the child is dehydrated during diarrhea | |
| Dry mouth | 403 (36.7) |
| Sunken Eyes | 513 (48.4) |
| Lethargy | 881 (84.4) |
| Thirsty | 123 (12.8) |
| Perception of primary caretaker about type of diarrhea which may cause serious harm/death in a child | |
| Rice/watery diarrhea | 991 (93.1) |
| Bloody diarrhea | 988 (93.6) |
| Diarrhea with vomiting | 1005 (95.0) |
| Dehydration with diarrhea | 872 (83.1) |
Weighted according to the proportion of children in the same age and sex categories in the demographic surveillance system (DSS) population.
When asked to list the signs of dehydration, primary caretakers reported the following: lethargy (84.4%), sunken eyes (48.4%), dry mouth (36.7%), thirst (12.8%) and skin turgor (2.0%). Rice water diarrhea (93.1%), bloody diarrhea (93.6%), and vomiting (95%) were commonly perceived by the caretakers as signs of a more severe form of diarrheal illness that might cause serious harm or death to the child. The decision whether to take their child to a health center for treatment of diarrhea was usually made by (80.9%, predominantly mothers).
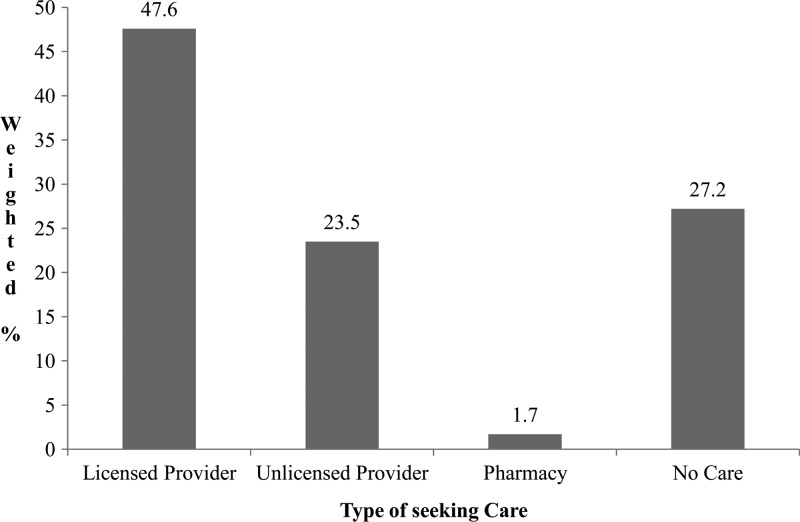
Caretakers of 92 children (7.9%) reported that their child had experienced a diarrheal episode within the 2 weeks before the interview; caretakers of 72 (72.8%) children sought some care outside the home, whereas no care was sought for 20 children (27.2%). Figure 2 depicts the practices of mothers seeking treatment of their child's diarrheal illness. Of the 92 children who had an episode of diarrhea during the previous 2 weeks, 46.5% were male, 42 were aged 0–11 months, 26 were 12–23 months, and 24 were 24–59 months of age. Caretakers of 10 of the 92 children (13.0%) reported that their children had blood in stool and 43.3% said that their child had fever during the diarrheal episode; 62.5% noted mucus in the child's stools, 5.2% observed rice/watery stools, 70.2% noted lethargy, 78.7% reported thirst, 74.7% reported sunken eyes, and 78.2% reported dry mouth. In the survey of binary logistic regression, factors significantly associated with seeking care outside the home included formal education of the primary caretaker (i.e., he or she completed at least primary school), and caretakers who reported that their child had fever, lethargy, sunken eyes (more than usual), and dry mouth (Table 2). Furthermore, multivariate logistic regression was used including five variables in the model; the results are presented in Table 3. Formal education of the primary caretaker (odds ratio [OR] = 15.5; 95% CI [2.5–85.7]; P = 0.002), presence of lethargy (OR = 5.9; 95% CI [1.1–31.7], P = 0.04), and dry mouth (OR = 19.9; 95% CI [4.3–90.9]; P = 0.0001) during diarrhea showed a significant association with seeking care outside of the home for children with diarrhea. The health care-seeking patterns were also examined as multi-category outcome variables (no care, care from an unlicensed provider, and care from a licensed provider). Formal education of the primary caretaker, presence of fever, lethargy, sunken eyes, and dry mouth during diarrhea showed a significant (P < 0.05) association with different care-seeking patterns by mothers in bivariate analysis. Multinomial logistic regression was used to estimate the effect of independent variables on different categories of the dependent variable; “No care” is used as the reference category. The likelihood of seeking care from a licensed provider, and from an unlicensed provider, was compared with the children for whom caretakers did not seek care from outside the home. We observed that formal education of the primary caretaker (OR = 21.4; 95% CI [3.2–139.0]; P = 0.002) and presence of dry mouth (OR = 17.3; 95% CI [2.7–110.9]; P = 0.003) were associated with seeking care from a licensed provider compared with no care. When “unlicensed provider” was compared with “no care,” formal education of the primary caretaker (OR = 7.0; 95% CI [1.0–49.6]; P = 0.05), dry mouth (OR = 37.0; 95% CI [4.4–308.9] P = 0.001), and lethargy (OR = 13.6; 95% CI [1.6–118.7]; P = 0.02) were associated with seeking care from an unlicensed provider.
Figure 2.
Health care-seeking pattern for diarrhea—results from baseline Health Care Utilization and Attitudes Survey (HUAS).
Table 2.
Health care-seeking pattern of primary caretakers whose children had diarrhea in the preceding 2 weeks, comparing those who sought no care with those who sought care
| Health Care Utilization Survey | No care (N = 20) N (weighted %) | Sought care (N = 72) N (weighted %) | OR (95% CI) | P value | |
|---|---|---|---|---|---|
| Age category | 0–11 mos. | 7 (11.9) | 35 (22.0) | 1.6 (0.9–2.8) | 0.13 |
| 12–23 mos. | 5 (15.9) | 21 (24.5) | 2.1 (0.6–7.6) | 0.26 | |
| 24–59 mos. | 8 (72.3) | 16 (53.4) | Ref | ||
| Sex | Male | 8 (46.9) | 36 (46.3) | Ref | |
| Female | 12 (53.1) | 36 (53.7) | 1.0 (0.3–3.5) | 0.96 | |
| Education of primary caretaker | No Formal* | 13 (75.9) | 24 (37.8) | Ref | |
| Some Formal | 7 (24.1) | 48 (62.1) | 5.1 (1.4–18.9) | 0.02 | |
| Fever | No | 14 (79.2) | 36 (48.1) | Ref | |
| Yes | 6 (20.3) | 36 (51.9) | 4.2 (1.1–16.0) | 0.027 | |
| Blood | No | 18 (88.1) | 64 (85.6) | Ref | |
| Yes | 2 (11.9) | 8 (13.4) | 1.1 (0.2–7.6) | 0.88 | |
| Rice/watery stool | No | 19 (96.7) | 65 (94.0) | Ref | |
| Yes | 1 (3.2) | 7 (6.0) | 1.9 (0.2–17.7) | 0.51 | |
| Lethargy | No | 14 (57.3) | 21 (19.6) | Ref | |
| Yes | 6 (42.6) | 51 (80.4) | 5.5 (1.6–19.6) | 0.01 | |
| Thirst | No | 5 (31.5) | 16 (17.4) | Ref | |
| Yes | 15 (68.5) | 56 (82.6) | 2.2 (0.5–8.7) | 0.32 | |
| Sunken eyes | No | 12 (54.0) | 16 (14.6) | Ref | |
| Yes | 8 (46.0) | 56 (85.4) | 6.8 (1.9–25.1) | 0.01 | |
| Dry mouth | No | 13 (63.6) | 9 (6.2) | Ref | |
| Yes | 7 (36.4) | 63 (93.8) | 26.5 (6.2–102.1) | 0.001 | |
| Mucus | No | 6 (23.0) | 31 (42.9) | Ref | |
| Yes | 14 (77.0) | 41 (57.1) | 0.4 (0.1–1.4) | 0.14 | |
No formal education (i.e., did not complete primary school).
Table 3.
Multivariate logistic regression model to identify factors associated with seeking care outside the home when a child had a diarrheal illness
| Variable | OR | 95% CI | P value |
|---|---|---|---|
| Education of primary caretaker: completed primary school or above | 15.5 | 2.8–85.7 | 0.002 |
| Fever | 1.7 | 0.3–9.3 | 0.52 |
| Lethargy | 5.9 | 1.1–31.7 | 0.04 |
| Sunken Eyes | 1.1 | 0.3–4.2 | 0.93 |
| Dry Mouth | 19.9 | 4.3–90.9 | 0.0001 |
Results from HUAS-lite.
The prevalence of diarrhea and MSD reported in the last 2 weeks at different rounds of HUAS-lite surveys is presented in Table 4. Overall, 5.7% of caretakers (lowest 3.5% in Sep–Dec 2010, highest 7.8% during Feb–Apr 2009) reported that their child had diarrhea in the previous 2 weeks. According to the definition of MSD, which we used for the case/control study, 78.1% of all diarrhea were considered to be the degree of severity of MSD, as recalled by the caretaker. Overall, 85.4% of the caretakers (range 76.2–95.9% between rounds) sought care from outside the home when their children had MSD; 13.5% caretakers (range 11.1–18.1%) sought care from one of the GEMS sentinel health centers.
Table 4.
Patterns of health care seeking among children who had any diarrhea or moderate-to-severe diarrhea as determined by serial Health Care Utilization and Attitude Surveys designated “HUAS-lite”
| Characteristics | Round 1 | Round 2 | Round 3 | Round 4 | Round 5 | Round 6 | Total |
|---|---|---|---|---|---|---|---|
| (Feb 09–Apr 09) N (weighted %)* | (May 09–Aug 09) N (weighted %)* | (Sep 09–Dec 09) N (weighted %)* | (Jan 10–Apr 10) N (weighted %)* | (May 10–Aug 10) N (weighted %)* | (Sep 10–Dec 10) N (weighted %)* | (Feb 09–Dec 10) N (weighted %)* | |
| Number of children randomly selected | 1,187 | 1,266 | 1,206 | 1,233 | 1,215 | 1,210 | 7,317 |
| No. (%) interviewed | 1,010 (83.2) | 1,015 (80.1) | 999 (82.4) | 1,014 (82.7) | 1,017 (83.2) | 1,022 (83.8) | 6,077 (82.6) |
| No. (%) with: | |||||||
| Diarrhea | 92 (7.8) | 76 (6.1) | 79 (6.8) | 66 (5.1) | 62 (4.5) | 49 (3.5) | 424 (5.7) |
| Sought health care outside the home | 66 (69.7) | 64 (82.3) | 68 (85.0) | 60 (93.2) | 52 (78.5) | 38 (75.1) | 348 (80.1) |
| No. (%) with: | |||||||
| Moderate-to-severe diarrhea (MSD) | 65 (70.1) | 64 (78.4) | 63 (79.1) | 55 (80.5) | 56 (89.6) | 37 (77.4) | 340 (78.1) |
| Sought health care: | |||||||
| Outside the home | 51 (76.2) | 57 (88.7) | 57 (91.4) | 52 (95.9) | 47 (77.5) | 31 (82.7) | 295 (85.4) |
| At a GEMS Sentinel Health Center | 9 (12.1) | 11 (16.1) | 8 (10.6) | 8 (11.1) | 9 (16.0) | 9 (18.1) | 54 (13.5) |
Weighted according to the proportion of children in the same age and sex categories in the demographic surveillance system (DSS) population.
GEMS = Global Enterics Multicenter Study; Sentinel Health Centers are health care facilities where the GEMS case/control study was conducted.
Discussion
In this study, it was seen that 72 (72.8%) of the 92 children suffering from diarrhea within the 2 weeks before the HUAS interview went to care providers for treatment. Contrary to common belief about a lower rate of care seeking for children in poor socio-economic settings, our study revealed that even in the poor settings like Kolkata slums, licensed health care providers were the most common (48%) source of care for childhood diarrhea. When we compared no care with treatment by licensed and unlicensed care providers, the only factors that influenced health care-seeking practices were education of the primary caretaker, i.e., the mother, and presence of signs of dehydration, i.e. lethargy and dry mouth.
Our study showed that caretakers who had completed primary school education were more likely to seek care from a licensed provider for children's diarrhea. It is difficult to compare care-seeking practices across different countries, cultures, and levels of development, particularly when different instruments (questionnaires) have been used. Nevertheless, it is interesting to note that a study in Kenyan slums showed that more than 75% of caretakers sought health care outside the home for sick children22; notably, children with diarrhea were more likely to be taken to treatment centers than those with cough and fever. In another study conducted in Mexico, 66% of children who had bloody diarrhea, vomiting, fever, or prolonged diarrhea were taken to health facilities.23 Because of the lack of knowledge of mothers about signs of dehydration (like sunken eyes and dry mouth), they did not consider it necessary to take dehydrated children to health care facilities. In contrast, in our study signs of dehydration played an important role in health care seeking, irrespective of the age stratum or nature of the health care provider.
This is noteworthy, especially when we speak of treatment pattern and approach of the care providers toward children suffering from acute watery diarrhea, with special reference to antibiotic use and misuse. Because there is a huge variation in health care-seeking options for diarrhea in urban slums of Kolkata,24 it is an important finding that 48% of the mothers sought care from licensed doctors. The licensed practitioners might be more likely to follow recommended management algorithms, including when to prescribe antibiotics, which is particularly important in this era of emergence of multi-drug-resistant diarrheal and enteric infections.25–30
About 78% of all diarrheal episodes were considered by caretakers as MSD in this study. There are several reasons for this high MSD proportion. For one, we relied on caretakers' memory during the previous 2 weeks and also relied on caretakers' ability to diagnose the signs and symptoms suggesting dehydration. In addition, this high MSD prevalence may be explained by caretakers' selective memory of recalling the more severe episodes.
Despite several plans to institute diarrheal disease control programs and the advent of low cost, effective interventions in countries like India, programs aimed at reducing the morbidity and mortality from pediatric diarrheal disease have not achieved their expected target because of a lack of knowledge at the individual and community level, and inconsistencies in local and international policy making. The major factors, though, are the gaps of knowledge in individual and community practices where there is inadequate awareness of the disease and its danger signs, low educational levels and socioeconomic status, and poor sanitation and hygiene. However, the other confounders like deficient local health infrastructure and health care delivery systems, inappropriate allocation of funds to different programs, and inadequate coordination and collaboration among different sectors and agencies also contribute to the inability to achieve greater success.
ACKNOWLEDGMENTS
The investigators are grateful to the participants and field workers and supervisors, for conducting the interviews and quality control.
Footnotes
Financial support: This study was part of the Global Enteric Multicenter Study supported by a grant from the Bill and Melinda Gates Foundation.
Authors' addresses: Byomkesh Manna, Department of Biostatistics, National Institute of Cholera and Enteric Diseases, Kolkata, India, E-mail: mannab2000@yahoo.co.in. Dilruba Nasrin, Karen L. Kotloff, and Myron M. Levine, Centre for Vaccine Development, University of Maryland, Baltimore, MD, E-mails: dnasrin@medicine.umaryland.edu, Kkotloff@medicine.umaryland.edu, and Mlevine@medicine.umaryland.edu. Suman Kanungo, Subhasis Roy, and Dipika Sur, Division of Epidemiology, National Institute of Cholera and Enteric Diseases, Kolkata, India, E-mails: sumankanungo@gmail.com, subhasisarjo@gmail.com, and dipikasur@hotmail.com. Thandavarayan Ramamurthy, Division of Microbiology, National Institute of Cholera and Enteric Diseases, Kolkata, India, E-mail: rama1murthy@yahoo.com.
References
- 1.Duggal R. Health Expenditure in India. Mumbai: Foundation for Research in Community Health; 1986. Foundation for Research in Community Health Newsletter 1.1. [Google Scholar]
- 2.Seal SC. Reports of the General Survey in Madhya Pradesh, Bengal, Bihar, Rajasthan, Assam, Uttar Pradesh, and Manipur. New Delhi: Directorate General of Health Services; 1961, 1962, 1963. [Google Scholar]
- 3.Sundar R. Household Survey of Health Care Utilization and Expenditure. New Delhi: National Council of Applied Economic Research; 1995. Working Paper No. 53. [Google Scholar]
- 4.Deshmukh PR, Dongre AR, Sinha N, Garg BS. Acute childhood morbidities in rural Wardha: some epidemiological correlates and health care seeking. Indian J Med Sci. 2009;63:345–354. [PubMed] [Google Scholar]
- 5.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–2234. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 6.Bryce J, Boschi-Pinto C, Shibuya K, Black ER. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–1152. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 7.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Liu L, Mathers C. for the Child Health Epidemiology Reference Group of WHO and UNICEF Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 8.Bassani DG, Kumar R, Awasthi S, Morris SK, Paul VK, Shet A, Ram U, Gaffey MF, Black RE, Jha P. Million Death Study Collaborators Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1853–1860. doi: 10.1016/S0140-6736(10)61461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Victoria CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhea through oral rehydration therapy. Bull World Health Organ. 2000;78:1246–1255. [PMC free article] [PubMed] [Google Scholar]
- 10.Pelto PJ, Pelto PH. Developing applied medical anthropology in Third World countries. Soc Sci Med. 1992;35:1389–1395. doi: 10.1016/0277-9536(92)90042-o. [DOI] [PubMed] [Google Scholar]
- 11.Shaik BT, Hatcher J. Health-seeking behavior and health service utilization in Pakistan: challenging the policy makers. Advance Access Publication. 2004;27:49–54. doi: 10.1093/pubmed/fdh207. [DOI] [PubMed] [Google Scholar]
- 12.Claeson M, Waldman RJ. The evolution of child health programmes in developing countries: from targeting diseases to targeting people. Bull World Health Organ. 2000;78:1234–1245. [PMC free article] [PubMed] [Google Scholar]
- 13.Awasthi S, Agarwal S. Determinants of childhood mortality and morbidity in urban slums in India. Indian Pediatr. 2003;40:1145–1161. [PubMed] [Google Scholar]
- 14.Sakisaka K, Jimba M, Hanada K. Changing poor mothers' care-seeking behaviors in response to childhood illness: findings from a cross-sectional study in Granada, Nicaragua. BMC Int Health Hum Rights. 2010;10:10. doi: 10.1186/1472-698X-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stuyf PV, Sorensen SC, Delgado E, Bocaletti E. Health seeking behavior for child illness in rural Guatemala. Trop Med Int Health. 1996;2:161–170. doi: 10.1111/j.1365-3156.1996.tb00022.x. [DOI] [PubMed] [Google Scholar]
- 16.Martines J, Paul VK, Bhutta ZA, Koblinsky M, Soucat A, Walker N, Bahl R, Fogstad H, Costello A. Neonatal Survival Steering Team Neonatal survival: a call for action. Lancet. 2005;365:1189–1197. doi: 10.1016/S0140-6736(05)71882-1. [DOI] [PubMed] [Google Scholar]
- 17.Sur D, Deen JL, Manna B, Niyogi SK, Deb AK, Kanungo S, Sarkar BL, Kim DR, Danovaro-Holliday MC, Holliday K, Gupta VK, Ali M, von Seidlein L, Clemens JD, Bhattacharya SK. The burden of cholera in the slums of Kolkata, India: data from a prospective, community based study. Arch Dis Child. 2005;90:1175–1181. doi: 10.1136/adc.2004.071316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Badowski N, Castro CM, Montgomery M, Pickering AJ, Mamuya S, Davis J. Understanding household behavioral risk factors for diarrheal disease in Dar es Salaam: a photovoice community assessment. J Environ Public Health Epub. 2011;2011:130467. doi: 10.1155/2011/130467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization . Geneva: WHO; 2002. Generic protocols for (i) hospital-based surveillance to estimate the burden of rotavirus gastroenteritis in children and (ii) a community-based survey on utilization of health care services for gastroenteritis in children: Field test version. [Google Scholar]
- 20.Nasrin D, Wu Y, Blackwelder WC, Farag TH, Saha D, Sow SO, Alonso PL, Breiman RF, Sur D, Faruque ASG, Zaidi AKM, Biswas K, Van Eijk AM, Walker DG, Levine MM, Kotloff KL. Health care seeking for childhood diarrhea in developing countries: evidence from seven sites in Africa and Asia. Am J Trop Med Hyg. 2013;89((Suppl 1)):3–12. doi: 10.4269/ajtmh.12-0749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Korn EL, Graubard BI. Analysis of Health Surveys. New York: Wiley; 1999. pp. 124–125. [Google Scholar]
- 22.Breiman RF, Olack B, Shultz A, Roder S, Kimani K, Feikin DR, Burke H. Healthcare-use for major infectious disease syndromes in an informal settlement in Nairobi, Kenya. J Health Popul Nutr. 2011;29:123–133. doi: 10.3329/jhpn.v29i2.7854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pérez-Cuevas R, Guiscafré H, Romero G, Rodríguez L, Gutiérrez G. Mothers' health-seeking behavior in acute diarrhea in Tlaxcala, Mexico. J Diarrhoeal Dis Res. 1996;14:260–268. [PubMed] [Google Scholar]
- 24.Sur D, Manna B, Deb AK, Deen JL, Danovaro-Holliday MC, von Seidlein L, Clemens JD, Bhattacharya SK. Factors associated with reported diarrhea episodes and treatment-seeking in an urban slum of Kolkata, India. J Health Popul Nutr. 2004;22:130–138. [PubMed] [Google Scholar]
- 25.Sengupta PG, Mandal S, Sen D, Das P, Deb BC, Pal SC. Multidrug resistant epidemic Shigellosis in a village in west Bengal, 1984. Indian J Public Health. 1990;34:15–19. [PubMed] [Google Scholar]
- 26.Garg P, Chakraborty S, Basu I, Datta S, Rajendran K, Bhattacharya T, Yamasaki S, Bhattacharya SK, Takeda Y, Nair GB, Ramamurthy T. Expanding multiple antibiotic resistance among clinical strains of Vibrio cholerae isolated from 1992–97 in Calcutta, India. Epidemiol Infect. 2000;124:393–399. doi: 10.1017/s0950268899003957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Srinivasa H, Baijayanti M, Raksha Y. Magnitude of drug resistant Shigellosis: a report from Bangalore. Indian J Med Microbiol. 2009;27:358–360. doi: 10.4103/0255-0857.55460. [DOI] [PubMed] [Google Scholar]
- 28.Dutta S, Rajendran K, Roy S, Chatterjee A, Dutta P, Nair GB, Bhattacharya SK, Yoshida SI. Shifting serotypes, plasmid profile analysis and antimicrobial resistance pattern of shigellae strains isolated from Kolkata, India during 1995–2000. Epidemiol Infect. 2002;1299:235–243. doi: 10.1017/s0950268802007240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roychowdhury A, Pan A, Dutta D, Mukhopadhyay AK, Ramamurthy T, Nandy RK, Bhattacharya SK, Bhattacharya MK. Emergence of tetracycline-resistant Vibrio cholerae O1 serotype Inaba, in Kolkata, India. Jpn J Infect Dis. 2008;61:235–243. [PubMed] [Google Scholar]
- 30.Bhattacharya K, Kanungo S, Sur D, Sarkar BL, Manna B, Lopez AL, Bhattacharya M, Nandy S, Niyogi SK. Tetracycline-resistant Vibrio cholerae O1, Kolkata, India. Emerg Infect Dis. 2011;17:568–569. doi: 10.3201/eid1703.101176. [DOI] [PMC free article] [PubMed] [Google Scholar]