In 2010, 7.6 million children died before the age of five,1 two-thirds unnecessarily.2 A concise list of evidence-based, life-saving interventions guides health policy makers, planners, and program implementers to decrease child mortality in low and middle income countries.2,3 Adding to the list, through discovery science, is challenging and exciting. Bringing existing interventions to families who need them, through delivery science, is at the same time more challenging, perhaps a bit less exciting, but more life-saving. The greatest gains to be made in intervention coverage across the continuum of care are for newly introduced interventions, as expected, and for existing curative interventions.4 Similarly, modeling exercises have repeatedly shown that the greatest reductions in mortality for children less than five years of age are to be achieved through increasing the coverage of treatment interventions for the three major causes of childhood mortality: pneumonia, malaria, and diarrhea.5
Because millions live at or beyond the periphery of the health system, there is a need to improve access to care for common childhood infectious diseases by bringing treatment closer to the community, especially in rural settings where distance, cost, and limited availability of primary health centers exist. Integrated community case management (iCCM) is a strategy to train, support, and supply community health workers (CHWs) to provide diagnostics and treatments for pneumonia, diarrhea, and malaria for sick children of families with difficult access to case management at health facilities. A pro-equity strategy, iCCM is not easy to implement.6 Health systems tend to be the most challenged in those high mortality settings in which iCCM is most needed. Moreover, iCCM has many steps that must be performed sequentially and completely for care to be successful. Deviations can result in bad outcomes for the sick child, the community (i.e., increased drug resistance), and the program. In addition, CHWs delivering iCCM must master ancillary skills, such as documentation and supply management, among others. The global health community needs guidance for implementing iCCM.
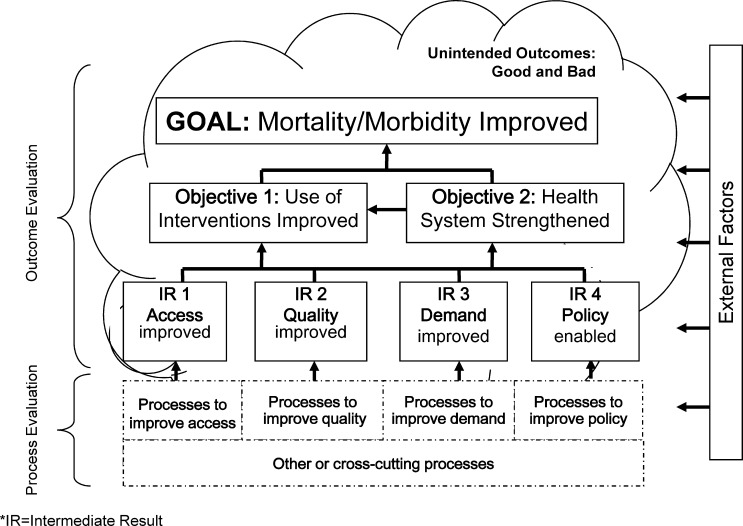
In response, a World Health Organization–Tropical Disease Research/United Nations Children's Fund (WHO-TDR/UNICEF) Joint Meeting for Community Case Management of Fever (Geneva, June 2008) produced a CCM research agenda.7 The global CCM Operations Research Group (ccm.org) further refined the agenda at a UNICEF meeting in New York (October 2008) and at a Program for Global Pediatric Research workshop on CCM for pneumonia in Vancouver (May 2010).8 This agenda remains in place today (Table 1).9 In Stockholm (May 2009), ccm.org proposed a generic evaluation framework for iCCM (Figure 1).9 On the basis of a results framework,10 the schema includes outcomes (boxes in top three rows) and processes (partitioned box at the bottom) to implement the strategy.
Table 1.
Global CCM operations research agenda with contributions from this supplement*
| Topic | Question | Supplement contribution |
|---|---|---|
| Front-line health workers | 1. What is the effect on the performance of CHW when management of one or more disease is added to the existing responsibility? | Chinbuah and others,15 Kayemba and others19 |
| 2. Are CHWs able to assess, classify, and treat various illnesses under integrated CCM? | Mukanga and others16 | |
| 3. What are the best ways to improve and sustain performance of CHWs? | ||
| 4. What are the cost and performance of different training methods for (illiterate/literate) CHWs? | ||
| 5. What are the best methods for evaluating the quality of service provided by CHW? | Cardemil and others28 | |
| 6. What is the optimal number of CHWs to give near universal coverage to a given geographic area? | Guenther and others13 | |
| 7. What are the best ways of supervising CHWs? | ||
| 8. Which factors increase recruitment and reduce attrition? | Strachan and others26 | |
| 9. Which methods of remuneration/incentivization are effective and sustainable? | ||
| Implementation | 10. What are the cost and cost-effectiveness of CCM? | Sadruddin and others29 |
| 11. What are appropriate methods for cost recovery and financing? | ||
| 12. How can effective coverage be achieved by CCM (equity, community effectiveness, etc.)? | Guenther and others,13 Kalyango and others18 | |
| 13. How can the private sector become involved in delivering integrated CCM? | Awor and others23 | |
| 14. How acceptable are CHWs to the health system, and how can CCM requirements for drugs, supplies, supervision, etc. be met? | Callaghan-Koru and others,21 Chandani and others27 | |
| 15. What are health system effects of CCM on referral and caseload and mix? | Nsona and others,20 Lainez and others,30 Seidenberg and others25 | |
| 16. What is the effect of CCM on antibiotic resistance? | ||
| 17. What is the impact of CCM on drug use and therapeutic outcomes in the community? | Kalyango and others,18 Mukanga and others16 | |
| Management of illness | 18. How can available tools (RDTs, clinical signs, timers, drugs, pulse oximeters, etc.) be combined into clinical algorithms? | |
| 19. What is the algorithm performance in different epidemiologic scenarios? | ||
| 20. What is the appropriate duration of antibiotic treatment of WHO-defined non-severe pneumonia in African settings? | ||
| 21. Can CHWs treat WHO-defined severe pneumonia in the community? | Sadruddin and others29 | |
| 22. How can age-dose regimens for different drugs be harmonized, and what are the effects on treatment of different packaging techniques? | ||
| 23. What is the impact of pre-referral drugs on clinical outcomes of children with severe disease? | ||
| 24. What is the most appropriate antibiotic for treatment of pneumonia? | ||
| 25. What is the most appropriate formulation of antibiotics? | ||
| Families and caregivers | 26. Do family members recognize the disease and promptly seek care? | Seidenberg and others,25 Nanyongo and others,24 Awor and others23 |
| 27. What are the elements that facilitate family members to use CCM services? | Rutebemberwa and others17 | |
| 28. Do family members follow treatment recommendations properly? | ||
| 29. How does prescription of multiple medicines for multiple diseases (e.g., malaria and pneumonia) impact adherence? | ||
| Impact | 30. What is the impact of integrated CCM on health and survival of children? | Chinbuah and others,15 Mukanga and others16 |
| 31. Does CCM lead to increased penetration in terms of reaching the poor? (effective coverage) | Guenther and others,13 George and others22 |
CCM = community case management; CHW = community health worker; RDT = rapid diagnostic test; WHO = World Health Organization.
Figure 1.
Evaluation framework.
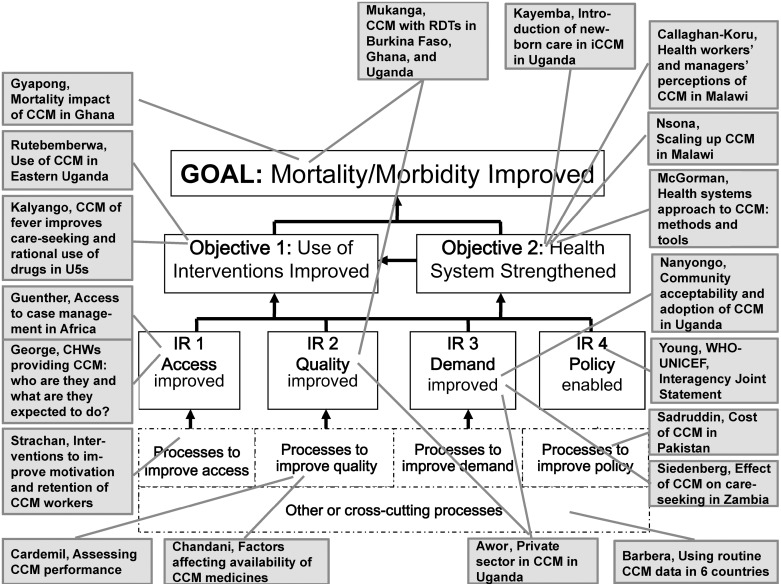
The World Health Organization and UNICEF have just released a Joint Statement for iCCM as an equity-focused strategy to improve access to case management.11 This supplement commences with a re-publication of this document,12 which summarizes much of the global evidence base until now. The purpose of these papers is to augment the experience base and evidence base for iCCM, and then chart the way forward for future research. We have mapped the included contributions against the research questions (Table 1) and results and/or processes (Figure 2). This large collection of CCM research informs 16 research questions. The country reports are almost exclusively from sub-Saharan Africa, with analyses from the Democratic Republic of the Congo, Ethiopia, Ghana, Côte d'Ivoire, Malawi, Mali, Rwanda, Sierra Leone, Uganda, Zambia, and Pakistan. Other papers address global issues, such as methods to measure access to case management13 and indicators to monitor iCCM programs.14
Figure 2.
Evaluation framework with Supplement contributions. iCCM = integrated community case management; CHW = community health worker; WHO-UNICEF = World Health Organization–United Nations Children's Fund.
This supplement informs nearly all results and processes in the evaluation framework (Figure 2). Chinbuah and others15 evaluated the impact on all-cause mortality of children 2–59 months of age, adding an antibiotic for pneumonia to an existing home-based antimalarial for fever strategy in Ghana. Mukanga and others16 reported the effect of implementing the iCCM package on the clinical outcome of febrile disease and on the quality of drug use in Uganda, Ghana, and Burkina Faso. Regarding use of CCM in eastern Uganda, Rutebemberwa and others17 measured care-seeking from community medicine distributors in urban and rural settings, and Kalyango and others18 compared the effect of iCCM and home-based management of fever strategies on care-seeking from community medicine distributors and on community drug use. Kayemba and others.19 reported health system implications for adding newborn care to iCCM in Uganda. In Malawi, Nsona and others20 described the national scale-up of iCCM, and Callaghan-Koru and others21 studied health workers' and managers' perceptions of the iCCM strategy and the CHWs delivering it. McGorman and others14 proposed, through a health systems lens, benchmarks and indicators for planning, introducing, and scaling up iCCM. Guenther and others13 measured and modeled access to case management with and without iCCM in Malawi, Mali, and Zambia. George and others22 characterized the CHWs relied upon to increase access to case management across sub-Saharan Africa. Regarding demand for iCCM in Uganda, Awor and others23 studied care-seeking for sick children, noting the potential role for and the uneven quality of care in the private sector; and Nanyongo and others24 reported community acceptability of iCCM. In Zambia, Seidenberg and others25 reported the effect of iCCM on care-seeking practices for sick children. Regarding policy, the joint statement of Young and others12 endorses iCCM globally, to encourage countries and donors alike.
Regarding processes to ensure access, Strachan and others26 reported stakeholder perceptions of approaches to improve CHW retention and motivation. Chandani and others27 studied determinants of medicine supply for CCM in three countries, and Cardemil and others28 compared methods to assess case management performance; both papers highlighted processes to ensure service quality. Sadruddin and others29 reported the household cost savings afforded by CCM for severe pneumonia in Pakistan, an important process to enable the policy environment. Lainez and others30 report practical applications of routine CCM service statistics, a cross-cutting process informing several intermediate results. The 19 reports in this supplement make important additions to a growing evidence base, which must still grow further.31
Footnotes
Authors' addresses: David R. Marsh, Save the Children Federation, Westport, CT, E-mail: dmarsh@savechildren.org. Davidson H. Hamer, Center for Global Health and Development, Boston University, Boston, MA, E-mail: dhamer@bu.edu. Franco Pagnoni, Global Malaria Programme, World Health Organization, Geneva, Switzerland, E-mail: pagnonif@who.int. Stefan Peterson, Uppsala University, Uppsala, Sweden, Makerere University, Kampala, Uganda, and Karolinska Instituet, Stockholm, Sweden, E-mail: Stefan.Peterson@ki.se.
References
- 1.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE. Global, regional, and national causes of child mortality: and updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 2.Jones G, Steketee R, Black RE, Bhutta ZA, Morris SS. Bellagio Child Survival Study Group How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 3.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Lancet Neonatal Steering Team Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–988. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. UNICEF . Countdown to 2015 Decade Report (2000–2010): Taking Stock of Maternal, Newborn and Child Survival. Geneva: World Health Organization and New York: UNICEF; 2010. [Google Scholar]
- 5.Bryce B, Friberg IK, Kraushaar D, Nsona H, Afenyadu GY, Nare N, Kyei-Faried S, Walker N. LiST as a catalyst in program planning: experiences from Burkina Faso, Ghana and Malawi. International J Epi. 2010;39:i40–i47. doi: 10.1093/ije/dyq020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNICEF . Review of Systematic Challenges to the Scale-up of Integrated Community Case Management: Emerging Lessons and Recommendations from the Catalytic Initiative (CI/IHSS) New York: United Nations Children's Fund (UNICEF), Knowledge Management and Implementation Research Unit, Health Section, Program Division; 2012. [Google Scholar]
- 7.WHO-TDR/UNICEF Joint Meeting for Community Case Management of Fever. http://www.who.int/tdr/news/2008/meetings-networks/en/index1.html Available at. Accessed April 23, 2012.
- 8.Qazi S, Bhutta Z. Program for Global Pediatric Research Workshop. http://www.globalpaediatricresearch.org/pdfs/36551-Group%205%20Report.pdf Available at. Accessed April 23, 2012.
- 9.Pagnoni F. Integrated Community Case Management. Operations Research. http://www.ccmcentral.com/?q=operations_research Available at. Accessed April 23, 2012.
- 10.Marsh DR, Alegre JC, Waltensperger KZ. A results framework serves both program design and delivery science. J Nutr. 2008;138:630–633. doi: 10.1093/jn/138.3.630. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. UNCEF . Joint Statement – Integrated Community Case Management, June 2012. Geneva: World Health Organization, and New York: UNICEF; 2012. [Google Scholar]
- 12.Young M, Wolfheim C, Marsh DR, Hammamy D. World Health Organization/United Nations Children's Fund joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children. Am J Trop Med Hyg. 2012;87((Suppl 5)):6–10. doi: 10.4269/ajtmh.2012.12-0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guenther T, Sadruddin S, Chimuna T, Sichamba B, Yeboah-Antwi K, Diakite B, Modibo B, Swedberg E, Marsh DR. Beyond distance: an approach to measure effective access to case management for sick children in Africa. Am J Trop Med Hyg. 2012;87((Suppl 5)):77–84. doi: 10.4269/ajtmh.2012.11-0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGorman L, Marsh DR, Guenther T, Gilroy K, Barat LM, Hammamy D, Wansi E, Peterson S, Hamer DH, George A. A health systems approach to integrated community case management of childhood illness: methods and tools. Am J Trop Med Hyg. 2012;87((Suppl 5)):69–76. doi: 10.4269/ajtmh.2012.11-0758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chinbuah MA, Kager PA, Abbey M, Gyapong M, Awini E, Nonvignon J, Adjuik M, Aikins M, Pagnoni F, Gyapong JO. Impact of community management of fever (using antimalarials with or without antibiotics) on childhood mortality: a cluster randomized controlled trial in Ghana. Am J Trop Med Hyg. 2012;87((Suppl 5)):11–20. doi: 10.4269/ajtmh.2012.12-0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mukanga D, Tiono AB, Anyorigiya T, Källander K, Konaté AT, Oduro AR, Tibenderana JK, Amenga-Etego L, Sirima SB, Cousens S, Barnish G, Pagnoni F. Integrated community case management of fever in children under five using rapid diagnostic tests and respiratory rate counting: a multi-country cluster randomized trial. Am J Trop Med Hyg. 2012;87((Suppl 5)):21–29. doi: 10.4269/ajtmh.2012.11-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rutebemberwa E, Kadobera D, Katureebe S, Kalyango JN, Mworozi E, Pariyo G. Use of community health workers for management of malaria and pneumonia in urban and rural areas in eastern Uganda. Am J Trop Med Hyg. 2012;87((Suppl 5)):30–35. doi: 10.4269/ajtmh.2012.11-0732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kalyango JN, Lindstrand A, Rutebemberwa E, Ssali S, Kadobera D, Karamagi C, Peterson S, Alfven T. Increased use of community medicine distributors and rational use of drugs in children less than five years of age in Uganda caused by integrated community case management of fever. Am J Trop Med Hyg. 2012;87((Suppl 5)):36–45. doi: 10.4269/ajtmh.2012.11-0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kayemba CN, Sengendo HN, Ssekitooleko J, Kerber K, Källander K, Waiswa P, Aliganyira P, Guenther T, Gamache N, Strachan C, Ocan C, Magumba G, Counihan H, Mbonye AK, Marsh DR. Introduction of newborn care within integrated community case management in Uganda. Am J Trop Med Hyg. 2012;87((Suppl 5)):46–53. doi: 10.4269/ajtmh.2012.12-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nsona H, Mtimuni A, Daelmans B, Callaghan-Koru JA, Gilroy K, Mgalula L, Kachule T, Zamasiya T. Scaling-up integrated community case management of childhood illness: update from Malawi. Am J Trop Med Hyg. 2012;87((Suppl 5)):54–60. doi: 10.4269/ajtmh.2012.11-0759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Callaghan-Koru JA, Hyder AA, George A, Gilroy KE, Nsona H, Mtimuni A, Bryce J. Health workers' and managers' perceptions of the integrated community case management program for childhood illness in Malawi: the importance of expanding access to child health services. Am J Trop Med Hyg. 2012;87((Suppl 5)):61–68. doi: 10.4269/ajtmh.2012.11-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.George A, Young M, Nefdt R, Basu R, Sylla M, Clarysse G, Bannicq MY, de Sousa A, Binkin N, Diaz T. Community health workers providing government community case management for child survival in sub-Saharan Africa: who are they and what are they expected to do? Am J Trop Med Hyg. 2012;87((Suppl 5)):85–91. doi: 10.4269/ajtmh.2012.11-0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Awor P, Wamani H, Bwire G, Jagoe G, Peterson S. Private sector drug shops in integrated community case management of malaria, pneumonia, and diarrhea in children in Uganda. Am J Trop Med Hyg. 2012;87((Suppl 5)):92–96. doi: 10.4269/ajtmh.2012.11-0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nanyonjo A, Nakirunda M, Makumbi F, Tomson G inSCALE Study Group. Community acceptability and adoption of integrated community case management in Uganda. Am J Trop Med Hyg. 2012;87((Suppl 5)):97–104. doi: 10.4269/ajtmh.2012.11-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seidenberg PD, Hamer DH, Iyer H, Pilingana P, Siazeele K, Hamainza B, MacLeod WB, Yeboah-Antwi K. Impact of integrated community case management on health-seeking behavior in rural Zambia. Am J Trop Med Hyg. 2012;87((Suppl 5)):105–110. doi: 10.4269/ajtmh.2012.11-0799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strachan DL, Källander K, ten Asbroek AHA, Kirkwood B, Meek SR, Benton L, Conteh L, Tibenderana J, Hill Z. Interventions to improve motivation and retention of community health workers delivering integrated community case management (iCCM): stakeholder perceptions and priorities. Am J Trop Med Hyg. 2012;87((Suppl 5)):111–119. doi: 10.4269/ajtmh.2012.12-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chandani Y, Noel M, Pomeroy A, Andersson S, Pahl MK, Williams T. Factors affecting availability of essential medicines among community health workers in Ethiopia, Malawi, and Rwanda: solving the last mile puzzle. Am J Trop Med Hyg. 2012;87((Suppl 5)):120–126. doi: 10.4269/ajtmh.2012.11-0781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cardemil CV, Gilroy KE, Callaghan-Koru JA, Nsona H, Bryce J. Comparison of methods for assessing quality of care for community case management of sick children: an application with community health workers in Malawi. Am J Trop Med Hyg. 2012;87((Suppl 5)):127–136. doi: 10.4269/ajtmh.2012.12-0389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sadruddin S, Shehzad S, Bari A, Khan A, ul-Haque I, Khan A, Qazi S. Household costs for treatment of severe pneumonia in Pakistan. Am J Trop Med Hyg. 2012;87((Suppl 5)):137–143. doi: 10.4269/ajtmh.2012.12-0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barberá Laínez Y, Wittcoff A, Mohamud AI, Amendola P, Perry HB, D'Harcourt E. Insights from community case management data in six sub-Saharan African countries. Am J Trop Med Hyg. 2012;87((Suppl 5)):144–150. doi: 10.4269/ajtmh.2012.12-0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamer DH, Marsh DR, Peterson S, Pagnoni F. Integrated community case management: next steps in addressing the implementation research agenda. Am J Trop Med Hyg. 2012;87((Suppl 5)):151–153. doi: 10.4269/ajtmh.2012.12-0505. [DOI] [PMC free article] [PubMed] [Google Scholar]