Abstract
Background:
Vaccination is one of the most common painful procedures in infants. Despite the irreparable consequences and complications of acute pain in infants, and existence of pharmacological and non-pharmacological methods for pain control, pain control in infants has received less attention. Therefore, this research aimed to compare the vaccination-related pain in infants younger than 6 months who receive vapocoolant spray and breastfeeding during injection, in order to suggest a strategy to provide emotional, mental, and physical health for infants.
Materials and Methods:
This is a randomized clinical trial study on 144 infants less than 6 months of age, referred to Ibn Sina Health Care Center in 2009, who were selected by convenience sampling. Forty-eight infants were allocated through systematic random sampling to each study group (i.e., breastfeeding, vapocoolant spray, and control group). Inclusion criteria were: Fully conscious infants, lack of any disease (sensory, motor abnormalities, cold, etc.), taking no medication, exclusive breastfeeding, vaccination for hepatitis B and DTP, regular visits to health care center, infants with Iranian nationality, and quiet infants who did not cry. The infant was excluded if he/she was crying and it was impossible to make him/her quiet before injection. Data were gathered by a questionnaire (six questions) and checklist [neonatal infant pain scale (NIPS)]. Data were analyzed by descriptive and inferential statistical methods through SPSS.
Results:
The findings suggest that breastfeeding during vaccination has a more analgesic effect on vaccination pain, compared to application of vapocoolant spray before vaccination. In 64.6% of the infants, breastfeeding during vaccination caused analgesia, while 25% of the infants who received vapocoolant spray experienced analgesic effect. There was a significant difference in pain between the infants who received vapocoolant spray and those on breastfeeding during injection (P < 0.001).
Conclusion:
It seems that breastfeeding during vaccination in infants under 6 months of age is an effective, natural, safe, accessible, and inexpensive method without side effects to reduce vaccination-related pain.
Keywords: Breastfeeding, pain, vaccination, vapocoolant spray
INTRODUCTION
Vaccination is one of the most painful procedures in infants.[1] Its immediate effects include syncope,[2] fear, irritability, sleep disorder, and a reduction in nutrition. Its short-term effects include a delay in wound healing, a change in immunity system function, endocrine and biochemical changes, increased cortisol and catecholamine release, increased glucagon, growth hormone, rennin, aldosterone, and antidiuretic hormones, and decreased insulin secretion. They also include physiological changes such as apnea, bradycardia, skin color changes, sweating palms, tachycardia, hypertension, increased respiration rate and muscular tonicity, increased intracranial pressure and oxygen intake, and behavioral changes including fretting, crying, etc.[3,4] Long-term effects of vaccination are delayed development and having different responses to similar painful experiences, long-term effects on neurotransmitters and endocrinal systems, as well as long-term complications on brain development and fear of future injections.[5,6] Researchers have shown that human is physiologically and anatomically able to perceive pain in fetal period.[4] On the other hand, effective pain control methods have been proved to be a practical management for pain control with positive outcomes for the patients.[7]
Medicational, non-medicational,[7] and surgical[8] methods are employed to control pain. In medicational method, local analgesics, sedatives, nonsteroid anti-inflammatory drugs, antidepressants and anti-evulsions,[9] assistive pain control drugs, nitrogen oxide, ketamine, and depolarizing neuromuscular blocking agents[10] are used. Use of vapocoolant sprays is among the other non-medicational methods to control pain.[2] They act as an analgesic factor on skin through a sudden decrease in skin temperature to 0°C (due to quick evaporation within seconds),[11] which has an immediate effect after being sprayed on the skin.[2] Vapocoolants have been proved to be safe and effective in humans[12] with no negative effect on vaccination[13] except for minor occasional skin irritation.[2]
Non-medicational method includes physical treatments (massage,[3] heat,[14] cold[15]), acupuncture, neural stimulation through skin, and cognitive therapies [distraction by use of toys, imagination, and/or combination of both like music,[16] visualization, artificial sleep, music, and psychotherapies, as well as behavioral treatments[8] (sports, relaxation)]. Another non-medicational method to control infants’ pain is breastfeeding which has analgesic effects on painful repetitive, short-term, and acute procedures.[7] Breastfeeding reduces the suffering caused by painful procedures such as vaccination through infant's distraction by sucking, skin touch of mother and infant, feeling of peace,[17] and with help of mother's milk components such as fat, protein, sugar, tryptophan, and precursors of melatonin (β-endorphin synthesis stimulants),[18] and through blocking neuron pathways in the spinal cord.[17] Midwives, as professionals, should know about safe and complication-free pain control methods, as well as the permanent and negative effects of infants’ first painful experience (vaccination), to educate the parents. No previous research studying the simultaneous effect of these two strategies on vaccination pain has been conducted. Since vaccination pain control is yet ignored in health centers, this study aimed at comparing vaccination pain in vapocoolant spraying method and breastfeeding in infants, and its association with infants’ age and sex, in order to administer the most practical, complication-free pain control method as a strategy to provide emotional, psychological, and physical health of infants with the help of the findings in the present study.
MATERIALS AND METHODS
This is a one-stage, three-group, and multivariable clinical trial study. The subjects were initially selected through convenient sampling and based on sample size calculation (accuracy of 0.3 and IC 95%). The subjects comprised 144 two-month, four-month, and six-month-old infants referred to Ibne Sina Health Care Center in Isfahan, who satisfied the inclusion criteria. They were randomly divided into three groups of vapocoolant, breastfeeding, and control (48 subjects in each group) through systematic random sampling. Inclusion criteria were: Infant's complete conscientiousness, age up to 6 months, lack of any diseases, no medication for the infant, absolute breastfeeding, vaccination for hepatitis B and DTP, quiet infant (not crying), hugged by the mother in all three groups, and regular and on-time reference to health care center for vaccination. If the infant was crying and would not get calm, he/she was excluded from the study. The data were collected by personal characteristics questionnaire (age and sex) and type and vaccination schedule, the method of pain control, and neonatal infant pain scale (NIPS) 2 pain assessment checklist. This checklist has been designed for measurement of pain in infants and includes six sections of facial status, cry, breathing pattern, arms, legs, and state of arousal.
The lowest score is zero and the highest is 7 (score over 3 shows pain).[1] NIPS is a standard tool to measure pain whose reliability and validity have been already confirmed by Razak[19] and Dilli[1] on 180 infants (r = 95). The vaccination conditions were identical for all the infants in the present study. In data collection, firstly, a questionnaire containing name, age, type of vaccination, vaccination schedule, and the method of pain control was filled out for all the infants by the researchers.
Then, the necessary interventions were administrated based on the utilized method. If the infant was in breastfeeding group, vaccination was administrated after the researcher had observed continuous active sucking (infants’ intraoral form, raised cheeks, and active jaw movements) and permitted vaccination. If the infant was in vapocoolant group, the injection site was sprayed from a distance of 15 cm for 1-3 s, and after evaporation (10 s later), the injection site was disinfected by alcohol and the vaccination administered. In the control group, injection was administered with no pain control intervention.
NIPS was filled out during vaccination by a co-researcher in all three groups. The collected data were analyzed by descriptive (frequency distribution and charts) and inferential (χ2, logistic regression) statistical tests through SPSS.
RESULTS
The findings showed that the percentage of the infants in each age group (2, 4, and 6 months) and in vaccination turn of two, three, and four was 33%, and in each group of vapocoolant, breastfeeding, and control, the number of infants was 16 (33.3%). These numbers had been intentionally allocated before the research by the researcher. The percentages of the male infants in groups of vapocoolant, breastfeeding, and control were 31.25%, 35%, and 33-75%, respectively. The percentages of female infants in groups of vapocoolant, breastfeeding, and control were 35.94%, 31.25% and 33.81%, respectively.
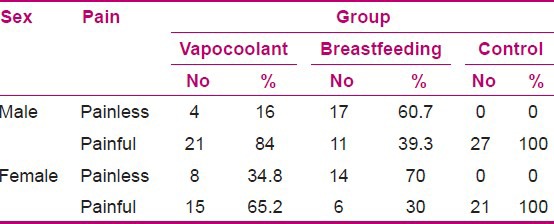
In other words, there were 80 male and 64 female infants in the present study. There were 93 injections of DTP and 51 injections of hepatitis B. The findings showed that vaccination was painless in 64.6% of the infants in the breastfeeding group, while this value was 25% for the vapocoolant group. About 100% of the infants in the control group had painful vaccination. Chi-square test showed that the frequency of pain was not the same in the three groups (P < 0.001), and frequency of painless injections in the breastfeeding group was significantly higher than in the other two groups. With regard to frequency distribution of vaccination pain in the three groups based on age group, although logistic regression test showed a significant difference in the pain frequency between the studied groups of vapocoolant and breastfeeding groups and group of no intervention and infants’ age (P = 0.01), age had no significant effect on the frequency of pain (P = 0.47) [Table 1]. With regard to frequency distribution of vaccination pain in the three groups based on sex, the findings showed that although logistic regression test showed a significant difference in the pain frequency between the studied groups and no intervention group and infants’ sex (P = 0.01), sex had no significant effect on pain frequency (P = 0.69) [Table 2].
Table 1.
Frequency distribution of vaccination-related pain in vapocoolant, breastfeeding and control groups based on infants’ age groups
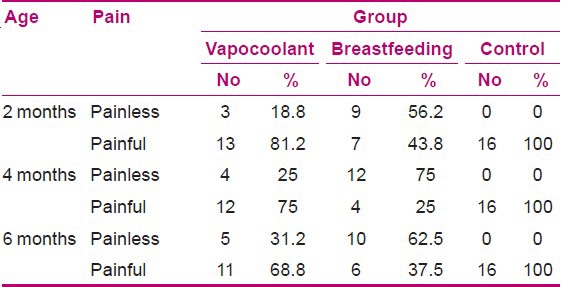
Table 2.
Frequency distribution of vaccination-related pain in vapocoolant, breastfeeding and control groups based on infants’ sex
DISCUSSION
The findings showed that frequency of painless vaccination in breastfeeding group was significantly higher than in the other two groups (vapocoolant and control).
Razak et al., in their study on the effect of breastfeeding on vaccination pain reported that breastfeeding reduced pain in 30% of the infants in the intervention group while 95% of the infants in the control group experienced painful vaccination.[19] Modares et al. (2006) in their study on the effect of breastfeeding during vaccination on vaccination pain in infants reported mean scores of pain (based on facial reaction, limb movements, and noise) to be 6.78 and 3.52, respectively, in the control and study groups, with a significant difference.[20] On the other hand, Bilgen et al. (2009) argued that there was no significant difference in the mean scores of pain while taking blood from the heel of infants during breastfeeding in the study and control groups. They claimed the inconsistency of their study result with those of other researches was because of quitting breastfeeding before taking the blood sample.[21] But in the present study and other studies, breastfeeding continued during the injection, which can be the reason for the existing inconsistency with that latter study. The former studies show that application of vapocoolant sprays before administration of painful procedures helps individuals feel less pain.[22] Farion et al. showed that on application of vapocoolant spray before catheter insertion, mean scores of pain were 3.7 and 5.6 in the intervention and control groups, respectively, with a significant difference in pain severity in both the groups.[11] These results are consistent with those of the present study since in the present study, vapocoolant spray decreased vaccination pain and χ2 test showed a significant difference between vapocoolant and control groups concerning pain severity. Cohen (2009) argue that vapocoolant spray is not effective to reduce vaccination pain. They reported that mean scores of pain in intervention and control groups were 7.46 and 5.78, respectively, with no significant difference concerning pain severity.[22]
The results of Chen's study did not support the findings of the former studies and those of the present study. As they argue, there may be some reasons for the inconsistency: Firstly, sudden feeling of cold on the skin triggers infants’ anxiety, leading to disappearance of appropriate effect of vapocoolant spray. Secondly, through spraying on infants’ skin and the sudden feel of cold, the infants focus more attention on the ongoing administration and show a more exaggerative reaction to pain, and finally, the infant is expected to feel no pain, but instead experiences anxiety and acute pain even with a minor painful procedure.[23] Other findings of the present study concerning comparison of frequency distribution of vaccination pain in intervention and control groups based on infants’ age revealed that breastfeeding during vaccination reduces pain more in 4-month-old infants compared to 6-month-old and 2-month-old infants. Application of vapocoolant before vaccination reduces pain more in the 6-month-old infants compared to 4-month-old and 2-month-old infants.
Although logistic regression showed that there was a significant difference in the frequency of pain in intervention and control groups and infants’ age, age had no effect on frequency of pain. Shah et al. reported that breastfeeding in infants of less than 2 months of age is an effective method to reduce vaccination pain, compared to other pain relief methods such as taking oral sucrose.[23]
Efe and Ozer (2007) in their study on the effect of breastfeeding on vaccination pain of the infants aged up to 4 months reported that breastfeeding significantly reduced pain in these infants, which concords with the findings of the present study.[24] Meta-analysis of Shah et al.[23] revealed that pain severity of painful procedures increases with age. Shah, quoting from Mikler, reports that application of vapocoolant spray to reduce vaccination pain in infants less than 6 months of age is not significantly effective.
Mikler remarks that further studies with higher sample size are needed to be conducted, as he had carried out his research on 30 2-6-month-old infants.[23] In the present study, although vapocoolant spray had a less effect compared to breastfeeding, it was somehow effective, possibly due to a higher number of the infants adopted in the present study compared to that by Mikler.
All in all, the results of various studies indicate that the response of the infants at lower ages to pain is more severe due to lack of development of nervous system and pain blocking neurotransmitters, compared to those at higher ages.[22,25] With regard to comparison of frequency distribution of vaccination pain in intervention and study groups based on sex, the findings showed that breastfeeding during vaccination and application of vapocoolant spray before vaccination both reduce pain more in female infants compared to males. Although logistic regression test showed a significant difference in the frequency of pain among the studied groups (vapocoolants, breastfeeding, and control) and infants’ sex, sex had no effect on frequency distribution of pain. Jenson, et al. (2001) showed that females respond more acutely to low back pain and oral surgeries, compared to males.[26]
Meanwhile, Roger (2000) states that males respond more to chest pain and facial muscles’ pain (Marcus, 2003), compared to females.[27,28] Therefore, it can be concluded that males and females respond differently to pain, based on its location. On the other hand, other studies report that sex has no effect on pain severity. Yet, the researchers believe there are many unknowns concerning the effect of sex on pain severity, and further studies are needed to reach a general conclusion. Since breastfeeding is a natural, accessible, safe, inexpensive, and complication-free method for painless vaccination, the Ministry of Health and Medical Education has suggested conducting vast studies in order to chart out a program for application of breastfeeding during infants’ vaccination in the related health care centers.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None
REFERENCES
- 1.Dilli D, Kucuk IG, Dallar Y. Interventions to reduce pain during vaccination in infancy. J Pediatr. 2009;154:385–90. doi: 10.1016/j.jpeds.2008.08.037. [DOI] [PubMed] [Google Scholar]
- 2.Cohen LL, Maclaren JE, Demore M, Fortson B, Friedman A, Lim CS, et al. A randomized controlled trial of vapocoolant for pediatric immunization distress relief. Clin J Pain. 2009;25:490–4. doi: 10.1097/AJP.0b013e3181a00414. [DOI] [PubMed] [Google Scholar]
- 3.Clifford Gevirtz MD, MPH, Anne Haddad. Topics in Pain Management Current Concepts and Treatment Strategies. Pain Management. 2008;23:1–12. [Google Scholar]
- 4.Bilgen H, Ozek E, Cebeci D, Ors R. Comparison of sucrose, expressed breast milk, and breastfeeding on the neonatal response to heal prick. J Pain. 2001;2:301–5. doi: 10.1054/jpai.2001.23140. [DOI] [PubMed] [Google Scholar]
- 5.Ramponi D. Reducing pain in pediatric procedures in the emergency department. J Emerg Dep. 2009;35:379–82. doi: 10.1016/j.jen.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Harrison D. Oral sucrose for pain management in the paediatric emergency department; A review. Australas Emerg Nurs J. 2008;11:72–9. [Google Scholar]
- 7.Boroner Stwart. Tehran, Jamehe Nagar: 1378. Medical Surgical nursing (pain, electrolytes, shock, cancer, geriatric care), translated by Abed saeidi G, Barahimi N, Parsa yekta Z, Tazacory Z, Shareify M. [Google Scholar]
- 8.Brayan R, Thomas E. Tehran: Iranian Pain Association; 2005. Management of acute pain, translated by Sharifi M, Arash Ordokanei. [Google Scholar]
- 9.Nasivanpour Shole. Tehran: Tayeb; 2004. Pain. [Google Scholar]
- 10.Namnabati M. Isfahan: Orouj; 2002. Pain in children. [Google Scholar]
- 11.Farion KJ, Splinter KL, Newhook K, Gaboury I, Splinter WM, Farion KJ, et al. The effect of vapocoolant spray on pain due to intravenous cannulation in children: A randomized controlled trial. CMAJ. 2008;179:31–6. doi: 10.1503/cmaj.070874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen LL. A multifaceted distraction intervention may reduce pain and discomfort in children 4-6 years of age receiving immunization. Evid Based Nurs. 2010;13:15–6. doi: 10.1136/ebn1014. [DOI] [PubMed] [Google Scholar]
- 13.Schechter N. Neonatal pain. J Paediatr Child Health. 2006;42:2–3. doi: 10.1111/j.1440-1754.2006.00778.x. [DOI] [PubMed] [Google Scholar]
- 14.Vannorsdall T, Dahlquist L, Shroff Pendley J. The relation between nonessentioal touch and childrens distress during lumbar puncture. Childrens Health Care. 2004;33:299–315. [Google Scholar]
- 15.American Academy of pediatrics. Committee on Psychosocial aspects of C, Family H, Task force on pain in infants C, Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108:793–7. doi: 10.1542/peds.108.3.793. [DOI] [PubMed] [Google Scholar]
- 16.Zempsky WT, Cravero JP. American Academy of Pediatrics Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine. Relief of pain and anxiety in pediatric patients in emergency medical system. Pediatrics. 2004;114:1348–56. doi: 10.1542/peds.2004-1752. [DOI] [PubMed] [Google Scholar]
- 17.Uga E, Candrilla M, Perino A, Alloni V, Angilella G, Trada M, et al. Heel lance in newborn during breastfeeding: An evaluation of analgesic effect of this procedure. Ital J Pediatr. 2008;34:1–5. doi: 10.1186/1824-7288-34-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gray PH, Trotter JA, Langbridge P, Doherty CV. Pain relief for neonates in Australian hospitals: A need to improve evidence- based practice. J Paediatr Child Health. 2006;42:10–3. doi: 10.1111/j.1440-1754.2006.00782.x. [DOI] [PubMed] [Google Scholar]
- 19.Razak AA, El N. Effect of breastfeeding on pain relief during infant immunization injections. Int J Nurs Pract. 2009;15:99–104. doi: 10.1111/j.1440-172X.2009.01728.x. [DOI] [PubMed] [Google Scholar]
- 20.Modares M, Rahimpour V, Mehran A. The effect of breast feeding during injection on injection pain in infants. J Hayat. 2006;12:31–7. [Google Scholar]
- 21.Bilgen H, Ozek E, Cebeci D, Ors R. Comparison of sucrose, expressed breast milk, and breastfeeding on the neonatal response to heal prick. J Pain. 2001;2:301–5. doi: 10.1054/jpai.2001.23140. [DOI] [PubMed] [Google Scholar]
- 22.Cohen LL. A multifaceted distraction intervention may reduce pain and discomfort in children 4-6 years of age receiving immunization. Evid Based Nurs. 2010;13:15–6. doi: 10.1136/ebn1014. [DOI] [PubMed] [Google Scholar]
- 23.Shah V, Taddio A, Rieder MJ HELPinKIDS Team. Effectiveness and tolerability of pharmacologic and combined interventions for reducing injection pain during rout in childhood immunizations: Systematic review and meta- analyses. Clin Ther. 2009;31:S104–51. doi: 10.1016/j.clinthera.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Efe E, Ozer ZC. The use of breastfeeding for pain relief during neonatal immunization injections. Appl Nurs Res. 2007;20:10–6. doi: 10.1016/j.apnr.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Henry PR, Houbold K, Dobrzykowski TM. Pain in the healthy full- term neonate: Efficacy and safety of interventions. Newborn Infant Nurse Rev. 2004;4:106–13. [Google Scholar]
- 26.Jensen IB, Bergström G, Ljungquist T, Bodin L, Nygren AL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: Are the effects depent on gender? Pain. 2001;91:65–78. doi: 10.1016/s0304-3959(00)00420-6. [DOI] [PubMed] [Google Scholar]
- 27.Roger VL, Farkouh ME, Weston SA, Reeder GS, Jacobsen SJ, Zinsmeister AR, et al. Sex differences in evaluation and outcome of unstable angina. JAMA. 2000;283:646–52. doi: 10.1001/jama.283.5.646. [DOI] [PubMed] [Google Scholar]
- 28.Marcus DA. Gender differences in chronic pain in a treatment-seeking population. J Gend Specif Med. 2003;6:19–24. [PubMed] [Google Scholar]


