Abstract
Background:
After radiofrequency catheter ablation of arrhythmias, patients have to bed rest for 4-6 h to prevent bleeding and hematoma. However, such a rest may cause back pain in the patients. The aim of this study was to determine the effects of continuous change in body position during and after the radiofrequency ablation on the back pain.
Materials and Methods:
In a quasi-experimental design 75 patients referring to university-affiliated hospitals were randomly assigned to a control group, receiving no change in body position, group A subjected to changes in body position during and after ablation, and group B subjected to changes in body position during ablation. The intensity of pain, blood pressure, heart rate, and extent of bleeding and hematoma were measured.
Results:
The groups were not significantly different in terms of demographic characteristics, blood pressure, heart rate, overall bleeding, or hematoma at the entry into the coronary care unit. While not significantly different from each other, the intensity of back pain between group A and B were significantly lower than that of group C. Compared to group C, group A and B had a significantly lower pain score up to 6 and 4 h after the procedure, respectively. Group B had a significantly higher pain score at 2, 4, and 6 h post ablation than group A.
Conclusions:
The findings show that changing the body position during and after the ablation procedure would reduce or prevent the back pain without increasing the chance of bleeding and hematoma.
Keywords: Back pain, bleeding, hematoma, Iran, patient positioning, radiofrequency catheter ablation
INTRODUCTION
Dysrhythmia caused or contributed to 479,000 of more than 2,400,000 deaths in the United States in 2003.[1] Atrioventricular node reentry tachycardia is the most common supraventricular tachycardia.[2] Atrial fibrillation is the most common sustained clinical arrhythmia.[3]
In case the drugs are not effective in decreasing or elimination of dysrhythmia, non-medical treatments such as ablation would be applied.[4] Radiofrequency catheter ablation is the standard therapy for treatment of different types of dysrhythmias[5] such as supraventricular dysrhythmia in patients with Wolfss–Parkinson–White syndrome and atrioventricular node reentry tachycardia.[6] The success of catheter ablation to eliminate accessory pathways is almost 95%.[7] Catheter ablation destroys specific cells, which are the reason or the center of dysrhythmia.[4] The duration of the procedure differs from 1 to 6 h based on the type of arrhythmia and other factors.[8]
Back pain is quite common after cardiac catheterization, and is caused by the position of the body, which is surrounded by the bed.[9,10,11,12,13] To avoid bleeding and hematoma, patients are instructed to rest in bed with their foot in a straight position for 4-6 h after the procedure.[14] Such a position, while reducing the vascular complications of the procedure, often leads to back pain and other adverse effects such as hemodynamic status instability.[1,15] Through the activation of autonomic nervous system and the release of epinephrine,[16] pain leads to many harmful effects including increased heart rate,[17,18] blood pressure,[19,20,21] and myocardial work load[22] and also dysrhythmia.[4] Lying on the back for a long time imposes pressure, and causes cellular ischemia and pain in the lumbar and the back.[23] Therefore, patients intend to change their position so as to reduce the pain and discomfort.[9,11]
Considering the possible incongruence of the patients’ views with the care providers perspectives[24] , the most important factor in comforting the patients is the relief of pain and a suitable position from the patient's attitude.[25] Patients’ positioning is based on experience and thought, and there is no scientific basis for that.[2,26] Inner-muscle pressure in lumbar muscles has a direct relation with the patients’ position and the imposed load on the muscles.[27] Changes in patients’ position following angiography could result in a stable hemodynamic status by reducing their pain without increasing vascular complications.[15] The present study was designed to examine the effects of a combination of reducing or preventing techniques, such as adjusting the angle of the bed with the horizontal level, changing the body position, and supportive pillow under the body and knees, on back pain following radiofrequency catheter ablation in patients with cardiac dysrhythmia.
MATERIALS AND METHODS
This is a quasi-experimental study performed at Shahid Faghihi and Kowsar hospitals in Shiraz, Iran, in 2010-2011. The inclusion criteria were eligibility for treatment by radiofrequency catheter ablation, a systolic blood pressure less than 190 mmHg, a diastolic blood pressure less than 110 mmHg, and consent to participate in the study. The exclusion criteria were spinal cord disorders, inter-vertebral disk disorders, bleeding disorders, the use of anticoagulant and analgesic drugs 24 h prior to the procedure, advanced heart failure, a procedure duration less than 1½ h and longer than 3½ h, increased bleeding or any other disorders during the procedure, severe decrease of consciousness level, performing ablation procedure through artery, and tranquilizers’ use during the procedure.
Using data from a previous study,[15] an alpha value of 0.05, power of 0.80, and effect size of 2 for pain score, the sample size was calculated to be 16 patients in each group. The samples were increased to 25 in each group (total 75 patients) to account for missing data due to any reason. The positioning protocol of the study was designed based on Rezaei-Adaryani and colleagues’protocol.[15] We also used pillow for knee positioning. The study protocol was approved by the research team and then Ethics Committee, Shiraz University of Medical Sciences. The patients (N = 75) were selected using purposive sampling. After obtaining written consent, the participants were randomly allocated to two case groups (A and B) and a control group (25 each).
Patients in the control group received routine care (with no change in position) including lying on their back for 6-8 h, which comprised of duration of the procedure.
Patients in group A did lie on their back during the procedure with the head of their bed tilted up for 15°, using a small mattress (3 × 30 × 80 cm) under their body and their knee bent for 30° using a small cylindrical pillow. In the first and second hours after the procedure, they continued lying on their back with the head of the bed tilted up for 30° and 45°, respectively. During the 2 hours post procedure, a small pillow was placed alternatively every 30 min under right and left sides of the body from shoulder to gluteal. Moreover, they continued to use the small cylindrical pillow under their knees. During the third hour, head of the bed was tilted up to 30° and the patients did lie on right and left sides for 30 min each. Within the fourth hour, the patients lied on their side (right or left) for 30 min with the head of the bed tilted up for 15°, followed by sitting for the next 30 min. In case of group B, the samples were positioned precisely like patients in group A during the procedure, and they were in the routine position after the procedure (without any alteration). The intensity of the back pain, blood pressure, heart rate, and the amount of bleeding and hematoma were measured right after the patients entered the coronary care unit (CCU) and 2, 4, 6, and 24 h after ablation in the three groups.
The data were collected using a questionnaire containing questions regarding patients’ demographic characteristics including age, gender, body mass index, marital status, education level, type of arrhythmia, previous history of ablation, angiography, open-heart surgery and changing the heart valves, the duration of ablation procedure, blood pressure, heart rate, prothrombin time, and the international normalized ratio, as well as a numeric rating scale, a standard mercury sphygmomanometer (ALPK2, Japan), a two-dimensional ruler, a scale, and a goniometer.
The numerical scale used for the evaluation of pain intensity scored pain from 0 (least severe) to 10 (most severe), and its validity and reliability had been established. Different forms of pain evaluation numeric scale have provided acceptable data with coefficients more than 99%.[28,29] Blood pressure was measured using a standard mercury sphygmomanometer. The amount of bleeding and hematoma was measured using two-dimensional ruler with the precision of 1 cm2. The ruler was reported to be highly consistent with a correlation coefficient of 0.96.[15] The goniometer was used to measure the angle of head of the bed and the patients’ knee angles.
The findings were analyzed using Chi-square and Kruskal-Wallis test. Where a significant difference was found with Kruskal-Wallis, pairwise comparisons were performed using Mann-Whitney U-test with Bonferroni adjustment. Statistical Package for Social Sciences (SPSS version 11.5) was used for data analysis at a P ≤ 0.05.
RESULTS
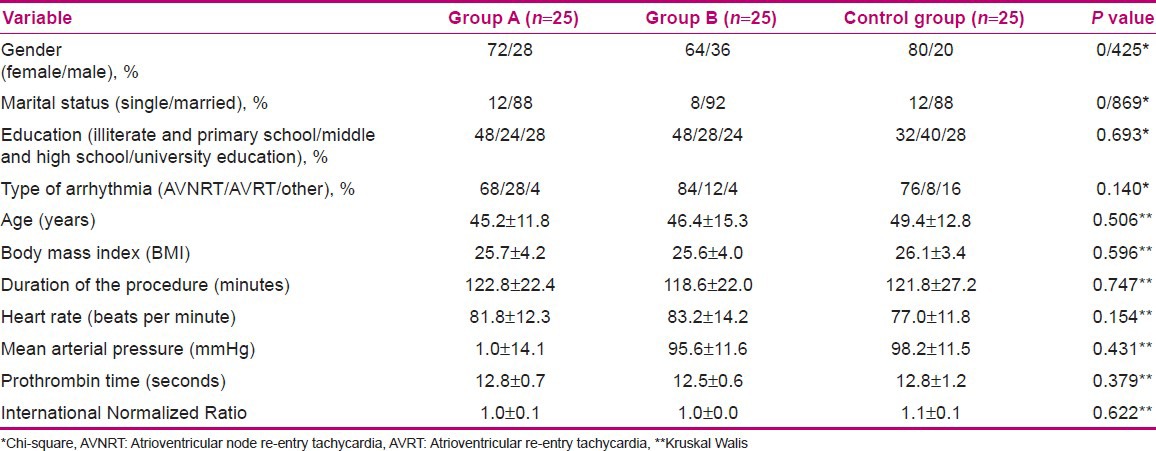
Seventy-five patients did participate in the study, and all of them did finish it. The patients’ baseline characteristics are shown in Table 1. There was no significant difference among the three groups in terms of gender, marital status, education level, type of arrhythmia, age, and body mass index, duration of ablation procedure, heart rate, mean arterial pressure, prothrombin time, or international normalized ratio. Also, the groups were not significantly different in terms of previous use of radiofrequency catheter ablation or coronary angiography.
Table 1.
Patients' baseline characteristics and group matching (the results of Kruskal-Wallis and Chi-square test)
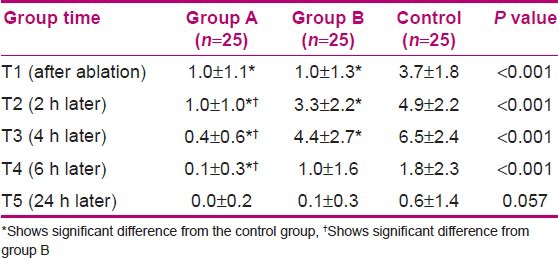
The pain intensity was significantly (P < 0.001) different among the three groups at immediately, 2, 4, or 6 h after ablation. However, it was not significantly different at 24 h after ablation among the three groups.
There was a significant difference (P < 0.001) between the control group and groups A and B in terms of pain intensity immediately after ablation. However, there was no significant difference between groups A and B. At 2 h after ablation, there was significant difference between the control group and groups A and B, as well as between groups A and B. At 4 h after ablation, there was a significant difference between groups A and B, group A and control group (P > 0.001), and group B and control group (P = 0.010) in terms of pain intensity. At 6 h after ablation, there was a significant difference in pain intensity between groups A and B (P < 0.005) and group A and control group (P < 0.001). However, it was not significantly different between group B and control group (P = 0.144). There was no significant difference in the pain intensity among the three groups at 24 h after ablation. Table 2 shows the comparison of the pain intensity among the three groups at different times after ablation.
Table 2.
Comparison of the pain intensity (mean±SD) among the three groups at different times after cardiac radiofrequency ablation
There was no significant difference in the arterial blood pressure or heart rate of the three groups at immediately, 2, 4, 6, or 24 h after ablation.
There was no significant difference among the three groups regarding the amounts of overall bleeding and overall hematoma formation.
DISCUSSION
The findings of this study indicate that patients in the control group experienced more pain compared to those in group A or B. It could be due to the prolonged rest without any change in the patients’ position. This shows that the more the patients’ rest in a flat position after ablation, the more intense back pain they would experience. No significant difference between groups A and B immediately after ablation could be due to similar body position in the two groups. Compared to patients in groups A, those in group B experienced more pain after ablation at 2, 4, and 6 h after ablation. Previous studies showed that changes in body position resulted in significant decrease of pain intensity at various times after angiography.[9,15,30,31] Also, no significant difference was observed in the mean arterial pressure or heart rate among participants at various times after ablation. However, such a finding is in contrast to that of Adaryani et al. who showed that mean arterial pressure and heart rate at 6 and 8 h after catheterization were significantly higher in the control group than those in the intervention groups.[15] Pain could lead to high blood pressure and heart rate.[17,18,20,21] The lack of significant difference in mean arterial pressure or heart rates among the three groups could be due to small number of the patients enrolled. In other words, compared to pains related to back and muscle spasms, pains with higher intensities may result in hemodynamic changes. Our study did not show significant difference in the amounts of overall bleeding or hematoma formation at femoral puncture site of the three groups at the measurement time points.
The findings of this study should be interpreted in the light of a number of limitations including variable pain threshold among patients, and the observation and reporting of outcomes was not blinded. Other studies involving varied changes in body position would be helpful to come up with a better nursing guideline for managing patients’ pain and discomfort after cardiac radiofrequency catheter ablation.
ACKNOWLEDGMENT
The authors would like to thank all patients who have participated in this study. We would also like to thank the directors of Kowsar and Faghihi hospitals, nurses of cardiac catheterization, CCU, and post-angiography wards of Kowsar Hospital, and cardiac catheterization and CCU wards of Faghihi Hospital in Shiraz. In addition, we truly appreciate the helpful corporation of all professors. We would also like to thank Vice-Chancellor of Research and Technology, Shiraz University of Medical Sciences for financial support of the study. This paper is an extract from Ms. Hajar Haghshenas MSc thesis. The study was registered at Iran's Clinical Trial Registry Center as IRCT201101095578N1.
Footnotes
Source of Support: This study was funded by Vice-Chancellor of Research Technology, Shiraz University of Medical Sciences
Conflict of Interest: None
REFERENCES
- 1.Black JM, Hawks JH. 8th ed. Missouri: Saunders Company; 2009. Medical-Surgical Nursing Clinical Management for Positive Outcomes; p. 1450. [Google Scholar]
- 2.Rostock T, Risius T, Ventura R, Klemm H, Weiss C, Keitel A. Efficacy and Safety of Radiofrequency Catheter Ablation of Atrioventricular Nodal Reentrant Tachycardia in the Elderly. J Cardiovasc Electrophysiol. 2005;16:608–10. doi: 10.1111/j.1540-8167.2005.40717.x. [DOI] [PubMed] [Google Scholar]
- 3.Terasawa T, Balk EM, Chung M, Garlitski AC, Alsheikh-Ali AA, Lau J. Systematic Review: Comparative Effectiveness of Radiofrequency Catheter Ablation for Atrial Fibrillation. Ann Intern Med. 2009;151:191–202. doi: 10.7326/0003-4819-151-3-200908040-00131. [DOI] [PubMed] [Google Scholar]
- 4.Smeltzer SC, Bare BG, Hinkle JL, Cheever KH. 12th ed. Philadelphia: Lippincott Williams and Wilkins; 2010. Brunner and Suddarth's textbook of medical surgical nursing; p. 721. 741,752. [Google Scholar]
- 5.Gaiser J. Catheter design for interventional electrophysiology. In: Singer I, editor. Interventional electrophysiology. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2001. p. 103. [Google Scholar]
- 6.Nakagawa H, Jackman WM. Catheter Ablation of Paroxysmal Supraventricular Tachycardia. Circulation. 2007;116:2465–78. doi: 10.1161/CIRCULATIONAHA.106.655746. [DOI] [PubMed] [Google Scholar]
- 7.Haung SS, Wood MA. Philadelphia: Saunders Elsevier; 2006. Catheter Ablation of Cardiac Arrhythmias; p. 448. [Google Scholar]
- 8.Craney JM. Radiofrequency catheter ablation of supraventricular tachycardias: Clinical consideration and nursing care. J Cardiovasc Nurs. 1993;7:26–39. doi: 10.1097/00005082-199304000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Chair SY, Taylor-Pilia R, Lam G, Chan S. Effect of positioning on back pain after coronary angiography. J Adv nurs. 2003;42:470–8. doi: 10.1046/j.1365-2648.2003.02646.x. [DOI] [PubMed] [Google Scholar]
- 10.Chair SY, Thompson DR, Li SK. Effect of ambulation after cardiac catheterization on patient outcomes. J Clin Nurs. 2007;16:212–4. doi: 10.1111/j.1365-2702.2006.01599.x. [DOI] [PubMed] [Google Scholar]
- 11.Fowlow B, Price P, Fung T. Ambulation after sheath removal: A comparison of 6 and 8 hours of bedrest after sheath removal in patients following a PTCA procedure. Heart Lung. 1995;24:28–37. doi: 10.1016/s0147-9563(05)80092-5. [DOI] [PubMed] [Google Scholar]
- 12.Lunde´n MH, Bengtson A, Lundgren SM. Hours During and After Coronary Intervention and Angiography. Clin Nurs Res. 2006;15:274–89. doi: 10.1177/1054773806291855. [DOI] [PubMed] [Google Scholar]
- 13.Pooler-lunse C, Barkman A, Bock BF. Effects of modified positioning and mobilization on back pain and delayed bleeding in patients who had received heparin and undergone angiography: A pilot study. Heart Lung. 1996;25:117–23. doi: 10.1016/s0147-9563(96)80113-0. [DOI] [PubMed] [Google Scholar]
- 14.Keegan B. Caring for women undergoing cardiac ablation. Crit Care Nurs Clin North Am. 2008;20:315–9. doi: 10.1016/j.ccell.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Rezaei-Adaryani M, Ahmadi F, Mohamadi E, Asghari-Jafarabadi M. The effect of three positioning methods on patient outcomes after cardiac catheterization. J Adv Nurs. 2009;65:417–24. doi: 10.1111/j.1365-2648.2008.04889.x. [DOI] [PubMed] [Google Scholar]
- 16.Urden LD, Stacy KM, Lough ME. 6th ed. Missouri: Mosby; 2010. Critical Care Nursing: Diagnosis and Management; p. 138. [Google Scholar]
- 17.Drummond P. The effect of pain on changes in heart rate during the valsalva maneuver. Clin Auton Res. 2003;13:316–20. doi: 10.1007/s10286-003-0127-1. [DOI] [PubMed] [Google Scholar]
- 18.Lu Q, Zeltzer LK, Tsao GC, Kim SC, Turk N, Nalibof BD. Heart rate mediation of sex differences in pain tolerance in children. Pain. 2005;118:185–93. doi: 10.1016/j.pain.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 19.al’Absi M, Petersen KL. Blood pressure but not cortisol mediates stress effects on subsequent pain perception in healthy men and women. Pain. 2003;106:285–95. doi: 10.1016/S0304-3959(03)00300-2. [DOI] [PubMed] [Google Scholar]
- 20.Bruehl S, Chung OY, Ward P, Johnson B, McCubbin JA. The relationship between resting blood pressure and acute pain sensitivity in healthy normotensives and chronic back pain sufferers: The effects of opioid blockade. Pain. 2002;100:191–201. doi: 10.1016/s0304-3959(02)00295-6. [DOI] [PubMed] [Google Scholar]
- 21.Pickering TG. Pain and blood pressure. J Clin Hypertens. 2003;5:359–61. doi: 10.1111/j.1524-6175.2003.02830.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Briggs E. The nursing management of pain in older people. Nurs Older People. 2002;14:23–9. doi: 10.7748/nop2002.10.14.7.23.c2224. [DOI] [PubMed] [Google Scholar]
- 23.Gould D. Wound management and pain control. Nurs Stand. 1999;14:47–54. doi: 10.7748/ns1999.10.14.6.47.c2701. [DOI] [PubMed] [Google Scholar]
- 24.Moattari, et al. The effect of empowerment on the self-efficacy, quality of life and clinical and laboratory indicators of patients treated with hemodialysis: a randomized controlled trial. Health and Quality of Life Outcomes. 2012;10:115. doi: 10.1186/1477-7525-10-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tomey MA, Alligood MR. 5th ed. Missouri: Mosby; 2002. Nursing theorists and their work. [Google Scholar]
- 26.McCabe PJ, McPherson LA, Lohse CM, Weaver AL. Evaluation of nursing care after diagnostic coronary angiography. Am J Crit Care. 2001;10:330–40. [PubMed] [Google Scholar]
- 27.Farasyn A, Meeusen R. The influence of non-specific low back pain on pressure pain thresholds and disability. Eur J Pain. 2005;9:375–81. doi: 10.1016/j.ejpain.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 28.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–92. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 29.Louville AB, Legroux-Gerot I, Cortet B, Devillers D, Blond S, Duquesnoy B, et al. Pain management in a rheumatology department: A satisfaction survey. Joint Bone Spine. 2003;70:362–6. doi: 10.1016/s1297-319x(03)00045-9. [DOI] [PubMed] [Google Scholar]
- 30.Benson G. Changing patients’ position in bed after non-emergency coronary angiography reduced back pain. Evid Based Nurs. 2004;7:19. doi: 10.1136/ebn.7.1.19. [DOI] [PubMed] [Google Scholar]
- 31.Coyne C, Baier W, Perra B, Sherer BK. Controlled trial of backrest elevation after coronary angiography. Am J Crit Care. 1994;3:282–8. [PubMed] [Google Scholar]


