Abstract
Aim
We examined the implications of using the Full Scale Intelligence Quotient (FSIQ) versus the General Abilities Index (GAI) for determination of intellectual disability using the Wechsler Intelligence Scales for Children, fourth edition (WISC-IV).
Method
Children referred for neuropsychological assessment (543 males, 290 females; mean age 10y 5mo, SD 2y 9mo, range 6–16y) were administered the WISC-IV and the Adaptive Behavior Assessment System, Second Edition (ABAS-II).
Results
GAI and FSIQ were highly correlated; however, fewer children were identified as having intellectual disability using GAI (n=159) than when using FSIQ (n=196). Although the 44 children classified as having intellectual disability based upon FSIQ (but not GAI) had significantly higher adaptive functioning scores than those meeting intellectual disability criteria based upon both FSIQ and GAI, mean adaptive scores still fell within the impaired range. FSIQ and GAI were comparable in predicting impairments in adaptive functioning.
Interpretation
Using GAI rather than FSIQ in intellectual disability diagnostic decision making resulted in fewer individuals being diagnosed with intellectual disability; however, the mean GAI of the disqualified individuals was at the upper end of criteria for intellectual impairment (standard score 75), and these individuals remained adaptively impaired. As GAI and FSIQ were similarly predictive of overall adaptive functioning, the use of GAI for intellectual disability diagnostic decision making may be of limited value.
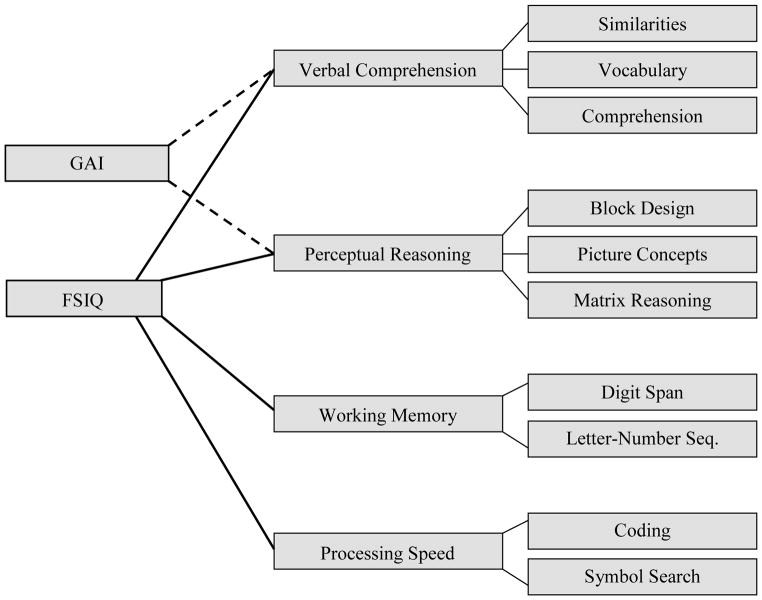
Intellectual disability is defined within the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, fourth edition, Text Revision (DSM-IV), as a standard score of approximately 70 on an individually administered measure of cognitive ability and ‘concurrent deficits or impairments in adaptive functioning’.1 Diagnostic criteria for intellectual disability in DSM-5 will continue to include requirements for both intellectual and adaptive impairment. In assessing intelligence, clinicians may choose between many standardized measures, some of which estimate overall intellectual ability by measuring two core domains – verbal and non-verbal reasoning skills – while others include additional domains (e.g. efficiency of information processing). One of the most commonly used IQ tests, the Wechsler Intelligence Scale for Children, fourth edition (WISC-IV),2 offers both a Full Scale Intelligence Quotient (FSIQ) – which is comprised of scores from four domains, including verbal comprehension, perceptual reasoning, processing speed, and working memory – and a General Abilities Index (GAI), which is calculated using only the verbal comprehension and perceptual reasoning scores (see Fig. 1).
Figure 1.
Wechsler Intelligence Scales for Children (fourth edition; WISC-IV) Full Scale Intelligence Quotient (FSIQ) and General Abilities Index (GAI) subscale composition.
Note. WISC-IV = Wechsler Intelligence Scale for Children – Fourth Edition; FSIQ = Full Scale IQ; GAI = General Abilities Index.
The use of more comprehensive measures of intellectual ability versus briefer, more targeted measures may have important implications for assessment of ‘intellectual impairment’. Thus, the distinction between GAI and FSIQ is important because the latter broadens its definition of intelligence to include measures of cognitive efficiency, such as working memory and processing speed. Use of the FSIQ potentially increases the occurrence of false positives when identifying intellectual disability, i.e. children may achieve lower FSIQ scores because of the speed and attentional or working memory demands that are part of this summary score, even though their broad reasoning skills may be largely intact. In non-clinical populations, the GAI is considered to provide an estimate of intellectual functioning comparable to that offered by the FSIQ.3 However, slowed processing speed is a common characteristic of a variety of neurocognitive disorders. For example, processing speed impairments have been found in reading disabilities,4,5 traumatic brain injury,6,7 and attention-deficit–hyperactivity disorder4,5,8 (ADHD). In addition, working memory weaknesses are commonly found in ADHD,5,9 traumatic brain injury,10,11 hydrocephalus,12,13 myelomenigocele,14,15 and reading disabilities,5,16 and in some individuals with intellectual disability.17
Because working memory and processing speed deficits may lower overall intellectual functioning but are not specific to the intellectual disability diagnostic criteria, the GAI may provide a more accurate estimate of reasoning ability in clinically referred children when low processing speed or working memory scores are suspected of reducing the FSIQ.18 The GAI may, therefore, better represent intellectual ability in these clinical groups, as their deficits may influence the speed of their output but not their ability to analyze and comprehend input.19 Harrison et al.19 compared FSIQ with GAI scores for the Wechsler Adult Intelligence Scale (third edition) among individuals with neurocognitive disorders (e.g. learning disabilities, ADHD), psychiatric diagnoses (e.g. depression, anxiety), and those with no diagnosis. They found a significant discrepancy between FSIQ and GAI scores in the neurocognitive group (with GAI greater than FSIQ), but not among the psychiatric disorders or no diagnosis groups. In addition, Bremmer et al.20 analyzed WISC-IV scores in a sample of clinically referred Canadian children, finding that in children diagnosed with either ADHD (inattentive subtype) or learning disabilities, GAI scores were significantly higher than a composite made up of the total of processing speed and working memory scores.
The purpose of the present study was to investigate the utility of the GAI, compared with the FSIQ, in identifying children with intellectual disability. Few existing studies compare FSIQ and GAI scores or examine the implication of potential GAI or FSIQ discrepancies in clinical groups. Appropriate identification of intellectual disability is essential for the determination of educational support and services, allocation of social services and funding, and even criminal proceedings.21 Given previously demonstrated differences between FSIQ and GAI scores for children and adults with various neurocognitive impairments, we hypothesized that FSIQ scores would be significantly higher than GAI scores in our sample. Furthermore, we expected that fewer children would meet criteria for intellectual impairment when using GAI as a measure of intellectual functioning compared with when using FSIQ. Given the positive correlation between adaptive functioning and IQ scores,22 we further hypothesized that low FSIQ and GAI scores would predict whether individuals would fall below the impairment threshold on adaptive functioning scores with acceptable sensitivity, specificity, and positive or negative predictive values. In addition, we anticipated that individuals in our sample with a GAI score greater than 70 but an FSIQ score of 70 or less would have higher adaptive functioning scores than those individuals with both FSIQ and GAI in the impaired range.
METHOD
Participants
Data were extracted from the clinical database of a neuropsychology outpatient clinic at a developmental disabilities center. Clinicians routinely enter assessment data into the clinical database via the secure electronic health record. Upon approval by the institutional review board, a de-identified dataset was extracted from the clinical database, consisting of individuals for whom scores on both cognitive (e.g. WISC-IV)2 and adaptive (Adaptive Behavior Assessment System, Second Edition, ABAS-II)22 measures, administered at the same assessment between 2006 and 2010, were available. The present sample, therefore, comprised a group of children presenting with diverse neurodevelopmental disorders and demonstrating a wide range of intellectual ability and adaptive functioning. Initially, the sample included 1135 children; however, 302 participants were excluded from the analysis because they had a verbal comprehension or a perceptual reasoning discrepancy of 1SD or more (thereby invalidating the use of the GAI as an estimate of global intellectual functioning).23 The remaining 833 participants were between the ages of 6 and 16 years (590 males, 209 females: mean age10y 5mo, SD 2y 9mo); 48% Caucasian 28% African-American.
Measures
Adaptive Behavior Assessment System-second edition22
The ABAS-II is a caregiver rating of adaptive behavior comprising 10 skill areas. Nine primary subscales fall into three theoretical domains. The conceptual domain consists of communication, functional academics, and self-direction scales; the social domain comprises the leisure and social skill scales; and the practical domain contains the community use, home living, health and safety, and self-care skill scales. A General Adaptive Composite (GAC) score is calculated by summing the nine subscales and then converting this into a norm-referenced standard score, with higher scores indicating better adaptive functioning. An additional work-skills subscale is included in the measure but was not applicable for the majority of the present sample and was not included in these analyses The ABAS-II is a stable and reliable measure of adaptive functioning with strong corrected test–retest reliabilities, good internal consistency, and adequate construct validity.22
Wechsler Intelligence Scale for Children, fourth edition
The WISC-IV is a well-recognized measure of cognitive ability. The WISC-IV subscales are used to generate four composite scores: verbal comprehension, perceptual reasoning, working memory, and processing speed (see Fig. 1). The FSIQ uses the four composite scores to generate an estimate of overall intellectual ability while the GAI is comprised of only the verbal comprehension and perceptual reasoning subscales to provide an estimate of overall reasoning ability that is less influenced by working memory and processing speed. Both the FSIQ and the GAI have demonstrated strong reliability for diagnosis of intellectual disability.2,23
Data analysis
After calculating both the FSIQ and GAI score for each member of the sample, we determined how many participants would be classified with intellectual impairment using the WISC-IV based upon the traditional cut-off scores for intellectual disability (i.e. ≥2 SD below the mean, or a standard score of ≤70) for each of the IQ estimates (i.e. FSIQ and GAI). Based on this information, we created two groups: participants for whom both FSIQ and GAI scores were 70 or less (the ‘both impaired’ group), and participants who had an FSIQ 70 or less but a GAI greater than 70 (the ‘discrepant’ group). These two groups differentiate between individuals who are impaired in both reasoning and working memory and/or processing speed (‘both impaired’ group) versus individuals with impairments in working memory and/or processing speed but less impaired reasoning skills (‘discrepant’ group). For the ‘discrepant’ group, it was presumed that their FSIQ may be brought down by their deficits in working memory and/or processing speed. There were eight participants with a discrepancy in the opposite direction (FSIQ >70 but GAI ≤70); however, owing to the low frequency of this pattern of scores, these participants were not included in the ‘discrepant’ group or in their own separate group.
SPSS software version 20 (IBM Corporation, New York, NY, USA) was used to calculate paired samples t-tests to compare GAI and FSIQ scores, as well as to compare GAC scores within the total sample, the ‘both impaired’ group, and the ‘discrepant’ group. Effect sizes were calculated using Cohen’s d. In order to compare the classification accuracy of FSIQ and GAI in making a diagnosis of intellectual disability, we calculated the sensitivity, specificity, and positive and negative predictive values using a receiver operating characteristic (ROC) curve for both indices of intelligence. The STATA software version 12 (Stata Corporation, College Station, TX, USA) ‘roctab’ syntax was used for sensitivity and specificity as well as ROC analyses.
RESULTS
Participants comprised 543 males, 290 females, mean age 10y 5mo, SD2y 9mo, range 6–16y) Full details regarding sample demographics and key variables, by group (‘both impaired’ vs ‘discrepant’) as well as for the total sample are shown in Table I. All participants included in the sample had complete WISC-IV and ABAS-II data. The mean FSIQ score for the total sample was in the low–average range. Within the entire sample, FSIQ and GAI were significantly correlated (r=0.957, p<0.001). ABAS-II GAC scores were also significantly correlated with both FSIQ (r=0.398) and GAI (r=0.367) at the 0.001 level. No significant differences in age or sex between the ‘both impaired’ and ‘discrepant’ groups were observed (Table I). There were significant differences between FSIQ and GAI (GAI>FSIQ) in the total sample (t[832]=−19.14, p<0.001, Cohen’s d=−0.20), and in the ‘discrepant’ group (t[43]=−12.62, p<0.001, Cohen’s d=−0.255], but not in the ‘both impaired’ group (t[151]=−1.68, p=0.095, Cohen’s d=−0.08).
Table I.
Mean FSIQ, GAI, and GAC scores for the total sample, ‘both impaired’, and ‘discrepant’ groups
| Total sample (SD) | ‘Both impaired’ group (SD) | ‘Discrepant’ group (SD) | t | p | Cohen’s d | |
|---|---|---|---|---|---|---|
| n | 833 | 152 | 44 | – | – | – |
| Males/Females | 543/209 | 63.83 | 68.85 | – | – | – |
| Age (y) | 10.4 (2.74) | 11.42 (2.72) | 11.17 (2.85) | 0.518 | 0.605 | 0.09 |
| FSIQ | 84.08 (18.07) | 57.23 (7.59) | 67.00 (3.33) | −8.30 | <0.001 | −1.67 |
| GAI | 87.77 (19.14) | 57.88 (8.97) | 75.75 (3.54) | −12.91 | <0.001 | −2.62 |
| ABAS GAC | 74.63 (17.17) | 63.61 (14.82) | 70.32 (15.55) | −2.61 | 0.01 | −0.44 |
| ABAS conceptual | 77.87 (14.46) | 66.97 (13.61) | 72.75 (13.54) | −2.49 | 0.014 | −0.43 |
| ABAS social | 81.52 (17.45) | 72.55 (15.04) | 80.23 (16.0) | −2.94 | 0.004 | −0.50 |
| ABAS practical | 75.11 (19.11) | 63.95 (18.55) | 72.07 (19.36) | −2.53 | 0.012 | −0.43 |
t, p, and Cohen’s d values are for comparisons between the ‘both impaired’ and ‘discrepant’ groups only. FSIQ, WISC-IV Full Scale Intelligence Quotient; GAI, WISC-IV General Abilities Index; ABAS, Adaptive Behavior Assessment System; GAC, General Adaptive Composite.
Table II presents the number of participants meeting the criteria for intellectual disability based on different adaptive and intellectual criteria. More participants met criteria for intellectual impairment using the FSIQ than the GAI. Approximately one-quarter of our sample met the criteria for adaptive impairment with GAC scores of 70 or less. In accordance with DSM-IV criteria for intellectual disability, all children in the present sample with GAC scores of 70 or less exhibited at least two skill areas of adaptive impairment. Of those with adaptive impairment, more participants met criteria for intellectual disability using FSIQ (FSIQ ≤ 70 and GAC ≤ 70), compared with those with adaptive impairment who met criteria for intellectual disability using GAI. A total of 118 children (14%) met intellectual disability criteria with both IQ scores (both FSIQ and GAI ≤ 70, and GAC ≤ 70), while 26 children (3%) did not meet criteria for intellectual disability diagnosis when assessed with GAI rather than FSIQ.
Table II.
Participants meeting criteria for intellectual and/or adaptive impairment
| Total sample (%) | FSIQ ≤ 70 (%) | GAI ≤ 70 (%) | |
|---|---|---|---|
| n | 833 | 196 (24) | 159 (19) |
| GAC ≤ 70 | 406 (49) | 144 (17) | 152 (14) |
| One ABAS domain ≤ 70 | 460 (55) | 152 (18) | 127 (15) |
The ABAS consists of three domains: conceptual, practical, and social. FSIQ, WISC-IV Full Scale Intelligence Quotient; GAI, WISC-IV General Abilities Index; ABAS, Adaptive Behavior Assessment System; GAC, General Adaptive Composite.
Descriptive data regarding adaptive functioning for the sample as a whole, the ‘both impaired’ group, and the ‘discrepant’ group are presented in Table I. An independent samples t-test showed that the GAC scores were significantly higher in the ‘discrepant’ group relative to the ‘both impaired’ group. Similarly, each of the ABAS domain scores was significantly higher in the ‘discrepant’ group than the ‘both impaired’ group. The proposed DSM-5 criterion for adaptive impairment (requiring impairment in at least one domain rather than at least two impaired skill areas) was comparable to using the GAC criterion score of 70 or less (see Table II). Classification of adaptive impairment using one impaired domain score increased rates only slightly among the entire sample.
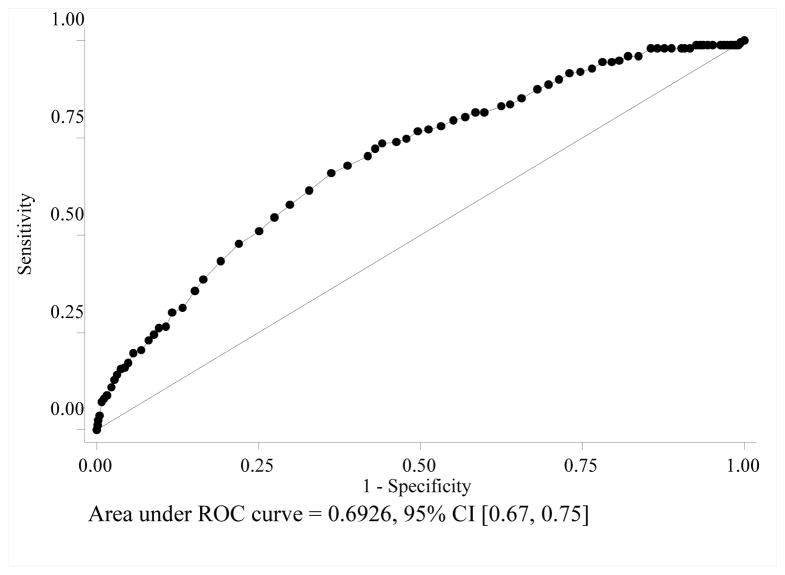
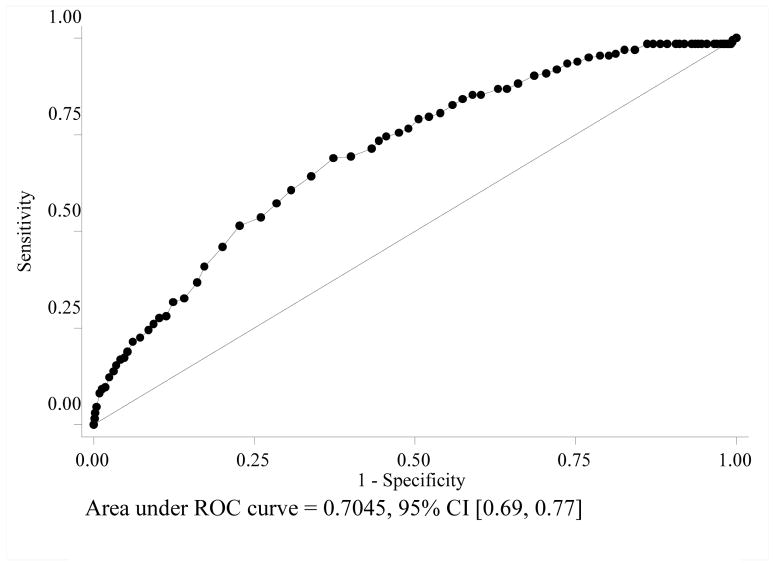
When using IQ scores in the impaired range (≤70) to predict impaired adaptive functioning (GAC ≤ 70), FSIQ and GAI were comparable (p ≥ 0.10 for all comparisons) in terms of sensitivity (GAI=0.30, FSIQ=0.35) and specificity (GAI=0.91, FSIQ=0.88). The same was true for the positive (GAI=0.75, FSIQ=0.73) and negative (GAI=0.58, FSIQ=0.59) predictive values. Using STATA 12 to conduct roctab ROC analysis, we found both measures of intellectual functioning demonstrated comparable performance in detecting intellectual disability (Figs 2 and 3). The area under the curve was fairly consistent between FSIQ (0.69) and GAI (0.70) in terms of predicting adaptive impairment. For reference, an area under the curve approaching 1.0 suggests more accurate detection of intellectual disability, whereas an area under the curve closer to 0.5 is analogous to chance.
Figure 2.
Receiver operating characteristic (ROC) curve examining Full Scale Intelligence Quotient relative to adaptive impairment, as determined by the Adaptive Behavior Assessment System, second edition, General Adaptive Composite scores.
Note. FSIQ = WISC-IV Full Scale Intelligence Quotient; ABAS = Adaptive Behavior Assessment System; GAC = General Adaptive Composite
Figure 3.
Receiver operating characteristic (ROC) curve examining General Abilities Index relative to adaptive impairment, as determined by Adaptive Behavior Assessment System, second edition, General Adaptive Composite scores.
Note. GAI = WISC-IV General Abilities Index; ABAS = Adaptive Behavior Assessment System; GAC = General Adaptive Composite
DISCUSSION
This study examined the use of WISC-IV GAI and FSIQ scores in identifying intellectual disability within a clinically referred sample. FSIQ and GAI scores were highly correlated in this clinical sample. It is not surprising that the correlation between FSIQ and GAI is greater than either of the correlations between the IQ estimates and the GAC, given the method variance among the IQ and GAC scores (performance-based testing vs parent report) and the fact that they represent two different constructs (intellectual functioning vs adaptive functioning). In contrast, FSIQ and GAI are representative of the same construct, share the same measurement methodology, and are calculated from many of the same scales.
In spite of accumulating evidence that processing speed and working memory may be differentially affected in clinical groups, little diagnostic value was added by the use of a more reasoning-based measure of intellectual functioning (i.e. the GAI) in quantifying intellectual disability. Moreover, data suggest that this practice may not be in the best interest of the individual with intellectual and adaptive skill concerns.
Use of GAI resulted in fewer children meeting criteria for intellectual disability. Examining the sample as whole, we found that GAI scores were significantly higher than FSIQ scores in this clinically referred sample of school-aged children. This finding is consistent with previous studies demonstrating that working memory and processing speed deficits are more common within clinically referred samples.24 While the clinical significance of this statistically significant difference in our sample is questionable (i.e. the average difference between the two scores was slightly more than three standard score points), the diagnostic implications of the GAI–FSIQ discrepancy were considerable, as fewer children met criteria using the GAI as opposed to FSIQ. When considering concurrent adaptive impairment (GAC ≤ 70) with intellectual functioning scores, again, a greater percentage of the sample met diagnostic criteria for intellectual disability when assessed with FSIQ as opposed to GAI. When tracking individuals for consistency of classification across intellectual indices used, we found that 26 children (3%) who would meet diagnostic criteria for intellectual disability using FSIQ and GAC no longer met the intellectual impairment criterion when using GAI and GAC.
Individuals who ‘fell out’ of a diagnosis of intellectual impairment by use of GAI (i.e. the ‘discrepant’ group) had significantly higher adaptive composite scores on average; however, as a group they still fell within the impaired range (mean GAC standard score=70.32). Moreover, the mean GAI score of the ‘discrepant’ group was a standard score of 75.75 (SD 3.54), which is typically considered the upper end of the margin of error for the intellectual impairment criteria of intellectual disability. As such, there is little evidence to suggest that this group’s relative strength in reasoning abilities constituted ‘intact’ intelligence, nor did it appear to afford much in the way of support for the application of functional daily skills. Despite their relatively stronger reasoning skills, children in the ‘discrepant’ group are still likely to be vulnerable to functional impairment in adaptive skills without supports and/or accommodations. Furthermore, sensitivity, specificity, and predictive values were comparable for the two methods when examined against adaptive functioning, suggesting that a GAI score of above 70 is not more likely to be associated with higher adaptive scores. However, it is noteworthy that the low sensitivity for both GAI and FSIQ, individually, in predicting adaptive dysfunction is consistent with previous research showing a high incidence of adaptive dysfunction in clinically referred young people without intellectual deficits, potentially owing to dysfunction in a variety of other clinical domains.25 As such, referred young people with low intelligence are likely to demonstrate adaptive dysfunction, but similar levels of adaptive dysfunction are also common in young people with ADHD, affective disorders, and medically complex conditions.
The evidence here indicates that the use of GAI for intellectual disability diagnostic decision making disqualifies a subgroup of children with significant intellectual and adaptive deficits. It calls into question the practice of relying on GAI scores in formulating a comprehensive clinical impression of a child’s overall functioning, particularly within a clinically referred group. A more accurate and representative picture might be obtained from examining each index score independently to assess a child’s particular strengths and weaknesses and integrating this information to guide rehabilitation and/or interventions. Demonstration of a GAI score greater than 70 does not necessarily translate to intact adaptive abilities. Many children with neurocognitive deficits who demonstrate generally intact reasoning abilities still require a great deal of assistance in daily functioning. Thus, it may be the case that working memory and processing speed, rather than being considered separate from ‘intelligence’, are actually vital components of the efficiency of overall intellectual functioning.
One limitation of the present study is that patient diagnosis was not available for analysis. Given preliminary evidence that there are indeed unique GAI–FSIQ relationships in various clinical groups,20 future research in this area could investigate the association between these indices and adaptive functioning within various diagnostic populations. Furthermore, it is important to note that the use of a standard score cut-off score of 70 or less means that some individuals with low measured intellectual ability (i.e. those with scores in the low 70s) were placed into the ‘not impaired’ group. Considering the standard error of measurement, those with scores in the low 70s may actually be better conceptualized as intellectually impaired.
In conclusion, the use of GAI rather than FSIQ in quantifying intellectual functioning for this clinical population only slightly reduced the incidence of intellectual disability, by placing less weight on deficit skill areas and subsequently raising intellectual functioning scores across the board. Children who demonstrate impaired intellectual functioning based on FSIQ but show relatively more intact GAI scores may not necessarily display intact adaptive abilities. Based on this information, we conclude that the GAI provides little additional value in terms of diagnostic accuracy for intellectual disability, predicting adaptive functioning, or determining more appropriate services for children who are neurocognitively compromised. While this proxy of intellectual ability is thought of as being less stringent, it does not appear to drastically alter the rates of disability against a general composite score in our sample.
What this paper adds.
Removing processing demands from IQ composite scores results in fewer children classified as having an intellectual disability.
Children disqualified from intellectual disability diagnoses using the WISC-IV GAI still present with significant deficits.
Where component reasoning indices are comparably developed, FSIQ is recommended for diagnostic decision making.
Acknowledgments
This work was supported by P30 HD-24061 (Intellectual and Developmental Disabilities Research Center) and the Johns Hopkins University School of Medicine Institute for Clinical and Translational Research, an NIH/NCRR CTSA Program.
ABBREVIATIONS
- ABAS-II
Adaptive Behavior Assessment System, second edition
- FSIQ
Full Scale Intelligence Quotient
- GAI
General Abilities Index
- GAC
General Adaptive Composite
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Text Revision. 4. Washington, DC, USA: American Psychiatric Association; 2000. [Google Scholar]
- 2.Wechsler D. WISC-IV Technical and Interpretive Manual. San Antonio, TX, USA: The Psychological Association; 2003. [Google Scholar]
- 3.Raiford SE, Weiss LG, Rolfhus E, Coalson D. Wechsler Intelligence Scale for Children: 4th Edition—General Ability Index; Report no 4. San Antonio, TX, USA: Pearson Education; 2009. [Google Scholar]
- 4.Shanahan MA, Pennington BF, Yerys BE, et al. Processing speed deficits in attention-deficit–hyperactivity disorder and reading disability. J Abnorm Child Psych. 2006;34:584–601. doi: 10.1007/s10802-006-9037-8. [DOI] [PubMed] [Google Scholar]
- 5.Willcutt EG, Pennington BF, Olson RK, Chhabildas N, Hulslander J. Neuropsychological analyses of comorbidity between reading disability and attention-deficit–hyperactivity disorder: in search of the common deficit. Dev Neuropsychol. 2005;27:35–78. doi: 10.1207/s15326942dn2701_3. [DOI] [PubMed] [Google Scholar]
- 6.Prigatano GP, Gray JA, Gale SD. Individual case analysis of processing speed difficulties in children with and without traumatic brain injury. Clin Neuropsychol. 2008;22:603–19. doi: 10.1080/13854040701440501. [DOI] [PubMed] [Google Scholar]
- 7.Thaler NS, Bello DT, Randall C, Goldstein G, Mayfield J, Allen DN. IQ profiles are associated with differences in behavioral functioning following pediatric traumatic brain injury. Arch Clin Neuropsych. 2010;25:781–90. doi: 10.1093/arclin/acq073. [DOI] [PubMed] [Google Scholar]
- 8.Jacobson LA, Ryan M, Martin RB, et al. Working memory influences processing speed and reading fluency in ADHD. Child Neuropsychol. 2011;17:209–24. doi: 10.1080/09297049.2010.532204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinussen R, Hayden J, Hogg-Johnson S, Tannock R. A meta-analysis of working memory impairments in children with attention-deficit–hyperactivity disorder. J Am Acad Child Psy. 2005;44:377–84. doi: 10.1097/01.chi.0000153228.72591.73. [DOI] [PubMed] [Google Scholar]
- 10.Levin HS, Hanten G, Chang CC, et al. Working memory after traumatic brain injury in children. Ann Neurol. 2002;52:82–8. doi: 10.1002/ana.10252. [DOI] [PubMed] [Google Scholar]
- 11.Roncadin C, Guger S, Archibald J, Barnes M, Dennis M. Working memory after mild, moderate, or severe childhood closed head injury. Dev Neuropsychol. 2004;25:21–36. doi: 10.1080/87565641.2004.9651920. [DOI] [PubMed] [Google Scholar]
- 12.Boyer KM, Yeates KO, Enrile BG. Working memory and information processing speed in children with myelomeningocele and shunted hydrocephalus: analysis of the children’s paced auditory serial addition test. J Int Neuropsych Soc. 2006;12:305–13. doi: 10.1017/s1355617706060425. [DOI] [PubMed] [Google Scholar]
- 13.Iddon JL, Morgan DJR, Loveday C, Sahakian BJ, Pickard JD. Neuropsychological profile of young adults with spina bifida with or without hydrocephalus. J Neurol Neurosurg Psy. 2004;75:1112–8. doi: 10.1136/jnnp.2003.029058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dennis M, Landry SH, Barnes M, Fletcher JM. A model of neurocognitive function in spina bifida over the life span. J Int Neuropsych Soc. 2006;12:285–96. doi: 10.1017/S1355617706060371. [DOI] [PubMed] [Google Scholar]
- 15.Yeates KO, Enrile BG, Loss N, Blumenstein E, Delis DC. Verbal learning and memory in children with myelomeningocele. J Pediatr Psychol. 1995;20:801–15. doi: 10.1093/jpepsy/20.6.801. [DOI] [PubMed] [Google Scholar]
- 16.de Jong PF. Working memory deficits of reading disabled children. J Exp Child Psychol. 1998;70:75–96. doi: 10.1006/jecp.1998.2451. [DOI] [PubMed] [Google Scholar]
- 17.Van der Molen MJ, Van Luit JEH, Jongmans MJ, Van der Molen MW. Verbal working memory in children with mild intellectual disabilities. J Intelligence Disabil Res. 2007;51:162–9. doi: 10.1111/j.1365-2788.2006.00863.x. [DOI] [PubMed] [Google Scholar]
- 18.Tulsky DS, Saklofske DH, Wilkins C, Weiss LG. Development of a General Ability Index for the Wechsler Adult Intelligence Scale-Third Edition. Psychol Assess. 2001;13:566–71. doi: 10.1037//1040-3590.13.4.566. [DOI] [PubMed] [Google Scholar]
- 19.Harrison AG, DeLisle MM, Parker KCH. An investigation of the General Abilities Index in a group of diagnostically mixed patients. J Psychoeduc Assess. 2008;26:247–59. [Google Scholar]
- 20.Bremner D, McTaggart B, Saklofske DH, Janzen T. WISC-IV GAI and CPI in psychoeducational assessment. Can J Sch Psychol. 2011;26:209–19. [Google Scholar]
- 21.Hayes SC. Early intervention or early incarceration? Using a screening test for intellectual disability in the criminal justice system. J Appl Res Intellect. 2002;15:120–8. [Google Scholar]
- 22.Harrison P, Oakland T. Adaptive behavior assessment system. 2. San Antonio: The Psychological Corporation; 2003. [Google Scholar]
- 23.Prifitera A, Saklofski DH, Weiss L. WISC-IV Clinical Use and Interpretation: Scientist-Practitioner Perspectives. Burlington, MA, USA: Elsevier Academic Press; 2005. [Google Scholar]
- 24.Schuchardt K, Gebhardt M, Maehler C. Working memory functions in children with different degrees of intellectual disability. J Intell Disabil Res. 2010;54:346–53. doi: 10.1111/j.1365-2788.2010.01265.x. [DOI] [PubMed] [Google Scholar]
- 25.Papazoglou A, Jacobson LA, Zabel TA. More than intelligence: distinct neuropsychological clusters linked to adaptive dysfunction in children. J Int Neuropsych Soc. 2013;19:189–97. doi: 10.1017/S1355617712001191. [DOI] [PubMed] [Google Scholar]