Abstract
Context:
Infectious complications of invasive procedures affect patient outcomes adversely. Choice of antiseptic solution at the time of insertion is one of the major factors affecting their incidence.
Aims:
This study was undertaken to compare efficacy of chlorhexidine 2% and povidone iodine 10% for skin disinfection prior to placement of epidural and central venous catheters (CVCs).
Settings and Design:
A prospective randomised trial in the operating rooms of a tertiary referral cancer centre.
Methods:
Sixty consecutive adult patients undergoing elective oncosurgery requiring placement of epidural and CVCs were enrolled. Paired skin swabs were collected before and after application of the antiseptic solution. The samples were incubated in McConkey's media and blood agar at 35°C for up to 24 h. Any bacterial growth was graded as: <10 colonies - poor growth, 10-50 colonies - moderate growth and >50 colonies as heavy growth. Data on demographics and antibiotic prophylaxis and costs was collected for all patients.
Statistical Analysis:
Student's t-test and Mann-Whitney tests were used to analyse data, P<0.05 was considered significant.
Results:
Demographics and antibiotic prophylaxis use was similar in both groups. Before application of antiseptic solution, a variety of micro-organisms were grown from most patients with growth ranging from none-heavy. No organism was grown after application of either antiseptic solution from any patient.
Conclusions:
We found no differences between 2% chlorhexidine and 10% povidone-iodine for skin disinfection in regard to costs, efficacy or side-effects.
Keywords: Antisepsis, chlorhexidine, povidone-iodine
INTRODUCTION
Infectious complications of indwelling devices are well-known. Central venous catheter (CVC) related bacteraemia remains an important and serious complication of CVC insertion.[1] The incidence of infectious complications with epidural catheters is very low. However, when it occurs, it can have disastrous implications for patients.[2] A variety of factors[3] affect the occurrence of catheter related blood stream infections (CRBSI). Vast majority of infections are linked to invasion of tissue by micro-organisms (mainly patient's own skin flora) via the trans-cutaneous insertion track of the device. Therefore, use of appropriate cutaneous antisepsis at the time of catheter insertion and subsequent catheter care remain important measures for preventing such infections. There are conflicting reports regarding preferred agent for cutaneous antisepsis, but among the commonly used solutions are 10% aqueous solution of povidone iodine and 2% chlorhexidene in alcohol. Our primary aim therefore was to compare the efficacy of these agents for cutaneous antisepsis. The secondary outcomes were contact time and cost difference.
METHODS
This prospective randomised controlled trial was conducted in a tertiary referral cancer centre; after obtaining waiver of informed consent from the Hospital Scientific Review Committee and Ethics Committee; over a period of three months. Sixty consecutive adult patients (a convenience sample) posted for elective surgery and in whom insertion of epidural or CVC was indicated were included. Patients with known allergy to either study drug or with coagulopathy or local infection were excluded. In our hospital, pre-operatively all patients are given bath with soap and water without antiseptic rub.
These patients were randomised in two groups according to a computer generated random numbers list prepared by our Clinical Research Secretariat-Chlorhexidine Group (CG - Chlorhexidine gluconate 2% in 80% alcohol - AHD™ 3000) and povidone iodine group (PVIG - 10% aqueous solution of povidone iodine-Wokadine™ 10%). Intravenous access was secured and the person performing the procedure took full aseptic precautions: Thorough timed scrubbing, cap, mask, sterile gown and gloves. After positioning the patient, a skin swab was obtained from the site (epidural or central venous) of catheter insertion, then skin was cleaned vigorously by applying the selected antiseptic solution over an area of approximately >500 cm2 for at least 15 s and the solution was allowed to dry. Sterile drapes were placed around the site and the area cleaned again with the same antiseptic solution. A second swab was taken after wiping the area with a sterile gauze piece. Then, the clinician proceeded with the planned procedure. Time of contact (time from application to drying) for each antiseptic solution during each procedure was noted. The paired swabs, appropriately labelled, were sent to the Microbiology Department for immediate processing. The samples were incubated on McConkey's media and blood agar at 35°C for 24 h. The microbiologist reporting the growth pattern was unaware of group assignment of the patient. If growth occurred; it was graded as follows: <10 colonies - poor growth, 10-50 colonies - moderate growth and >50 colonies as heavy growth. Any side-effects such as development of cutaneous rash, etc., were recorded. Other variables such as demographic data, haemogram values, antibiotics received were noted. The cost of cutaneous antisepsis was calculated for each patient.
Statistical analysis
Student's t-test and Mann-Whitney Test were used to analyse data after ascertaining normal distribution of data; using SPSS version 16. A P<0.05 was considered significant.
RESULTS
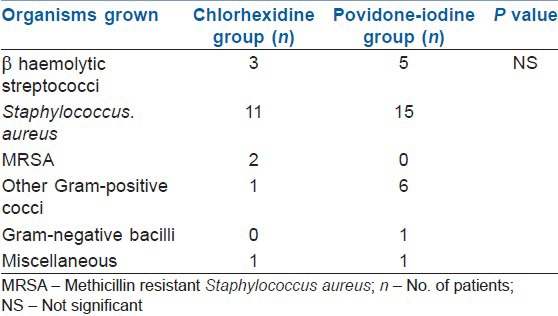
This prospective randomised observational study was conducted over a period of 3 months at a tertiary referral cancer hospital in 60 adult patients. The demographics [Table 1], antibiotic prophylaxis, sites of epidural and CVC placement [Table 2] were similar in both groups. Out of 30 patients in chlorhexidine 2% group, prior to application of antiseptic, 10 samples had heavy growth, 5 samples had moderate growth, 7 samples had poor growth, 8 samples had no growth while in povidone iodine 10% group, out of 30 patients, 6 had heavy growth, 9 had moderate growth, 3 had poor growthand 12 had swabs which had no growth [Table 3]. Table 4 lists the organisms grown from skin swabs taken before application of antiseptic solutions. After application of antiseptic, there was no growth from any of the swabs in either group. The time of contact was much longer in the Povidone-Iodine group (150.0±9.26 s vs. 60.33±9.28 s P<0.001 by Mann-Whitney test). There were no side-effects in either group.
Table 1.
Demographics
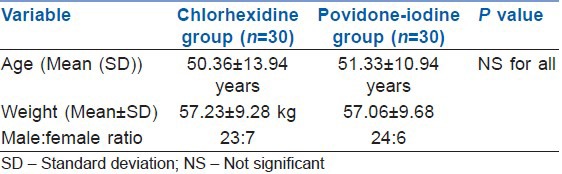
Table 2.
Antibiotic prophylaxis, sites of epidural and central venous catheters placement
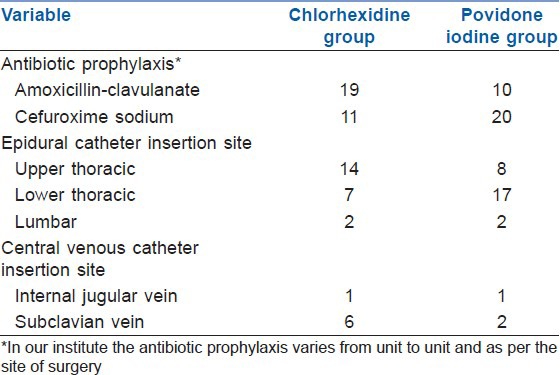
Table 3.
Magnitude of growth from swabs obtained before application of antiseptics
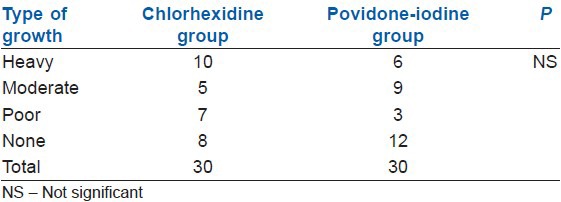
Table 4.
Micro-organisms grown from swabs before application of antiseptic solution
DISCUSSION
We compared 2% chlorhexidine in alcohol with 10% povidone-iodine aqueous solution for cutaneous antisepsis. Most patients’ swabs led to bacterial growth before but not after application of either antiseptic solution, indicating equal efficacy. Drying time was faster for 2% chlorhexidine and the costs were only marginally different.
In the PVP-Iodine complex, iodine exists as total iodine, which is a combination of negatively charged iodide and available iodine, i.e., all species, which may be titrated with sodium thiosulfate. Very little free iodine is present in the solution, which explains the low toxicity. Povidone-iodine exerts it's antiseptic properties in two ways, first it substitutes the covalently bound hydrogen groups such as-OH, -NH, -SH, or CH groups. Second povidone is an iodophor and it reacts with the oxygen containing functional groups. Free iodine determines the bactericidal activity; total iodine determines the ability to kill bacteria. Iodine solutions have rapid, broad-spectrum antimicrobial activity against bacteria, viruses, and fungi. It quickly penetrates micro-organisms and attacks neucleotides, fatty acids and thiol groups. It inhibits protein synthesis by oxidizing the thiol group.[4] Chlorhexidine is a cationic biguanide that binds to the negatively charged surface of bacterial cell wall leading to alteration in permeability, which leads to leakage of cytoplasmic contents and finally cell death.[5]
Aromaa et al.[6] reported that the incidence of bacterial infection of the central nervous system after epidural and spinal anaesthesia was 1.1 per 100,000. A recent review article[2] found that the incidence of neuraxial block associated infections is on the rise. The incidence CRBSI in ICUs is about 3%, however, it may reach as high as 16%. This translates in to 2-30 episodes of CRBSI per 1000 catheter days.[1] Many factors influence[7] the occurrence of these complications.
All our patients were immune-competent, and received pre-operative antibiotics. It is unlikely that the prophylactic antibiotics prevented bacterial growth in the second sample since we did get growth in almost all samples taken before antiseptic application and temporally the two swabs were closely related. Thus, the absence of growth from the second swab is a direct result of efficacy of the antiseptic agents, without any confounding factors.
The literature on efficacy of these agents is conflicting. Some studies[8,9,10] found alcohol based chlorhexidine (0.5-2%) to be superior to povidone-iodine 10% for cutaneous antisepsis. Mimoz et al.[8] assigned patients to skin preparation with 0.5% chlorhexidine in alcohol or povidone-iodine in an aqueous solution. The contamination rates were much lower in the chlorhexidine group ([1.4% vs. 3.3%]; odds ratio, 0.40 [95% CI, 0.21-0.75]; P=0.004). In patients undergoing clean-contaminated surgery[9] skin preparation with chlorhexidine led to lower incidence of surgical site infections (9.5% vs. 16.1%; P=0.004) compared to that with povidone-iodine. Similarly, in-patients undergoing amniocentesis 2% chlorhexidine reduced the colony count more than the povidone iodine solution.[10]
In contrast, several studies suggest that both agents are equally effective. A prospective study[11] observed the impact of povidone-iodine on residual bacteria and development of post-operative surgical site infections. Of the 1014 swabs taken, 3.6% showed positive cultures and this had no correlation with the development of post-operative surgical site infection (4.04%). Langgartner et al.[12] found that sequential application of chlorhexidine 0.5% in alcohol followed by povidone-iodine was better than either agents used alone. The catheter tip bacterial colonization rate was 4.7% with the combination as compared to 30.8% (Povidone-Iodine 10%) and 24.4% (Chlorhexidine). For cutaneous antisepsis in patients undergoing hernia surgery,[13] both chlorhexidine in alcohol and povidone iodine led to similar reductions in skin bacterial colony counts and the infection rates were similar (9.5% vs. 7.0%, P=0.364). Girard et al.[14] evaluated the effect of povidone-iodine (1 year) and chlorhexidine over the next year for CVC related infections. They found significant reduction in colonization with chlorhexidine (1.12 vs. 1.55 P=0.041), however, the reduction in CVC related infections and bacteraemia was non-significant. Another study[15] showed no difference between the two and concluded that chlorhexidine 0.5% was ‘as effective as’ povidone-iodine 10%.
Two meta-analyses have shown the superiority of chlorhexidine over povidone iodine in vascular catheter site care[16] and pre-operative abdominal wall antisepsis[17] in patients undergoing clean contaminated abdominal surgery.
There are problems in interpreting these studies - the chlorhexidine preparations used vary from 0.5 to 2 to 4%.[18] However, these different solutions provide a concentration at the effector site, which exceeds minimal inhibitory concentrations needed for the usual nosocomial bacteria and yeast. The comparators are similarly different: Povidone iodine in alcohol or in aqueous solutions. Apart from studies which looked at the bacterial growth or colony counts the studies defined catheter associated blood stream infections differently.[16] The study population and study end-points for antiseptic use were also different.[9,13]
Staphylococcus epidermidis is the most common skin commensal.[19] However, Staphylococcus aureus was the most common causative organism in epidural infections in a large systematic review on epidural abscesses.[20] In CRBSI,[21] coagulase-negative staphylococci are responsible for 37-60% of infections while staphylococcus aureus is isolated from 5-12%. This may be because Staphylococcus aureus is more resistant to cutaneous disinfectants than other skin micro-organisms, or that the bactericidal effect of some disinfectants may not be rapid enough to prevent inoculation of Staphylococcus aureus into the epidural space.[22]
In an experimental study, Zamora et al.[23] demonstrated an inhibition of bactericidal activity of povidone-iodine due to interaction with blood and other proteinaceous material in vitro. They hypothesized that organic material present in the blood may have bound to iodine leading to reduced amount of free iodine for bactericidal effect. A later study[24] clearly demonstrated that when used for hand washing; in presence of blood, both chlorhexidine and isopropyl alcohol reduced colonizing flora of the hands whereas, povidone iodine did not. They suggested that this may be of particular importance in emergency situation when proper hand washing facilities may not be available.
Another experimental study compared the activity of alcoholic solution of 2% chlorhexidine gluconate with various preparations of chlorhexidine (0.5% and 2% chlorhexidine aqueous and in alcohol) isopropyl alcohol, and 10% aqueous povidone-iodine against Staphylococcus epidermidis in the presence or absence human serum. They found that all preparations reduced the colony counts but alcoholic solution of 2% chlorhexidine gluconate was the most effective.[25]
The residual effect; defined as the long-term antimicrobial suppressive activity; of chlorhexidine gluconate, is prolonged (at least 6 h) while that of povidone-iodine is minimal. This prolonged residual effect of chlorhexidine is due to its adherence to the stratum corneum, which extends its duration of action for several hours after first application.[7] This ability of antiseptic solutions to bind to and penetrate the stratum corneum is important for effective clearance of the micro-organisms living by the side of the hair follicles or in the sebaceous glands. Up to 20% micro-organisms live deep within dermis and these may be an important source causing contamination of invasive devices and subsequent colonization.[22]
In most of our patients Staphylococcus aureus was grown (86% - 26 out of 30) in swabs collected before application of disinfectants and in another 6% patients methicillin-resistant Staphylococcus aureus (MRSA) was grown. Thus, in-patients who remain in hospital for a long time pre-operatively; the normal commensals may be replaced with Staphylococcus aureus and even with MRSA. In such patients use of 2% chlorhexidine may carry an added advantage over povidone iodine. The superiority of chlorhexidine gluconate compared with povidone iodine in reducing the colony counts of coagulase-negative staphylococci has been shown long back in a study[26] of disinfection of peritoneal dialysis catheter sites. At 24 h after peritoneal dialysis catheter site care; the incidence of patients with Staphylococcus epidermidis colony forming units was higher (54%) when povidone iodine was used than with chlorhexidine (15%) use. Because most device–related infections are caused by Gram-positive cocci, the superior bactericidal effect of chlorhexidine gluconate against these organisms is likely to be clinically important.
Cost is a consideration when choosing an antiseptic. We found a difference of 40 paise between chlorhexidine and povidone-iodine, which is very minimal. Chaiyakunapruk et al.[16] also reported that despite the higher cost of chlorhexidine gluconate, the absolute difference was relatively small (approximately $0.92 vs. $0.41) for a quantity sufficient to prepare an insertion site for a CVC. They concluded that given the extent of the benefit and the small increment in cost, chlorhexidine gluconate should be considered as a replacement for povidone-iodine, particularly in patients at high-risk for catheter related bloodstream infection. In another meta-analysis carried out by Lee et al.[18] using decision analytic cost-benefit model to compare the economic value of antiseptic solutions found that due to fewer surgical site infections and positive skin cultures, chlorhexidine resulted in net cost savings of $16-26 per surgical case and substantial costs saving for the hospital.
The contact time (application to drying) was much shorter with chlorhexidine in our study. This time taken to achieve antisepsis may be important in emergency situations like trauma or emergency caesarean section where epidural or spinal anaesthesia or CVC insertion needs to be carried out in a hurry. When time is of essence, chlorhexidine may be preferred to povidone-iodine.
Both antiseptic solutions can lead to allergic reactions, particularly cutaneous hypersensitivity. We did not observe any hypersensitivity reactions in either group.
The strength of our study was an objective end-point, i.e., bacterial growth from skin swabs. There were however, limitations. The first was small numbers and a convenience sample. The second limitation was that the operator collecting the swabs was not blinded. Blinding was not possible due to difference in the colour of the antiseptic solutions; however, the reporting microbiologist was blinded. Since, the end-point was objective in nature (growth from swabs before and after cutaneous antisepsis), we believe that the results could not have been influenced by lack of blinding of the operator, though normally this can lead to investigator bias. Third instead of incidence of device related incidence we chose bacterial growth before and after antisepsis. We feel that though use of antiseptic solution does influence this incidence, there are other confounding factor such as improper handling of the device, etc., which may confound the results. Therefore, efficacy of the antiseptic is better judged from immediate lack of growth after application. Future studies need to explore the comparative efficacy of these agents in larger number of patients with clinically relevant end-points such as CRBSI or surgical site infections.
CONCLUSION
We found that for cutaneous antisepsis, there is no difference between 2% chlorhexidine gluconate in alcohol and 10% povidone-iodine aqueous solution, in terms of efficacy, cost or side-effects. Chlorhexidine 2%, due to its significantly shorter contact time, may be of value in emergency situations. The epidemiology of device related infections, prolonged residual effect and better bactericidal effect of chlorhexidine against staphylococcus makes it a preferable agent for cutaneous antisepsis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Fletcher S. Catheter-related bloodstream infection. Contin Educ Anaesth Crit Care Pain. 2005;5:49–51. [Google Scholar]
- 2.Horlocker TT, Wedel DJ. Infectious complications of regional anesthesia. Best Pract Res Clin Anaesthesiol. 2008;22:451–75. doi: 10.1016/j.bpa.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Safdar N, Kluger DM, Maki DG. A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters: Implications for preventive strategies. Medicine (Baltimore) 2002;81:466–79. doi: 10.1097/00005792-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Fleischer W, Reimer K. Povidone-iodine in antisepsis – State of the art. Dermatology. 1997;195:3–9. doi: 10.1159/000246022. [DOI] [PubMed] [Google Scholar]
- 5.Milstone AM, Passaretti CL, Perl TM. Chlorhexidine: Expanding the armamentarium for infection control and prevention. Clin Infect Dis. 2008;46:274–81. doi: 10.1086/524736. [DOI] [PubMed] [Google Scholar]
- 6.Aromaa U, Lahdensuu M, Cozanitis DA. Severe complications associated with epidural and spinal anaesthesias in Finland 1987-1993. A study based on patient insurance claims see comment. Acta Anaesthesiol Scand. 1997;41:445–52. doi: 10.1111/j.1399-6576.1997.tb04722.x. [DOI] [PubMed] [Google Scholar]
- 7.Hebl JR. The importance and implications of aseptic techniques during regional anesthesia. Reg Anesth Pain Med. 2006;31:311–23. doi: 10.1016/j.rapm.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Mimoz O, Karim A, Mercat A, Cosseron M, Falissard B, Parker F, et al. Chlorhexidine compared with povidone-iodine as skin preparation before blood culture. A randomized, controlled trial. Ann Intern Med. 1999;131:834–7. doi: 10.7326/0003-4819-131-11-199912070-00006. [DOI] [PubMed] [Google Scholar]
- 9.Darouiche RO, Wall MJ, Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N Engl J Med. 2010;362:18–26. doi: 10.1056/NEJMoa0810988. [DOI] [PubMed] [Google Scholar]
- 10.Adler MT, Brigger KR, Bishop KD, Mastrobattista JM. Comparison of bactericidal properties of alcohol-based chlorhexidine versus povidone-iodine prior to amniocentesis. Am J Perinatol. 2012;29:455–8. doi: 10.1055/s-0032-1304827. [DOI] [PubMed] [Google Scholar]
- 11.Tschudin-Sutter S, Frei R, Egli-Gany D, Eckstein F, Valderrabano V, Dangel M, et al. No risk of surgical site infections from residual bacteria after disinfection with povidone-iodine-alcohol in 1014 cases: A prospective observational study. Ann Surg. 2012;255:565–9. doi: 10.1097/SLA.0b013e3182468b2d. [DOI] [PubMed] [Google Scholar]
- 12.Langgartner J, Linde HJ, Lehn N, Reng M, Schölmerich J, Glück T. Combined skin disinfection with chlorhexidine/propanol and aqueous povidone-iodine reduces bacterial colonisation of central venous catheters. Intensive Care Med. 2004;30:1081–8. doi: 10.1007/s00134-004-2282-9. [DOI] [PubMed] [Google Scholar]
- 13.Sistla SC, Prabhu G, Sistla S, Sadasivan J. Minimizing wound contamination in a ‘clean’ surgery: Comparison of chlorhexidine-ethanol and povidone-iodine. Chemotherapy. 2010;56:261–7. doi: 10.1159/000319901. [DOI] [PubMed] [Google Scholar]
- 14.Girard R, Comby C, Jacques D. Alcoholic povidone-iodine or chlorhexidine-based antiseptic for the prevention of central venous catheter-related infections: In-use comparison. J Infect Public Health. 2012;5:35–42. doi: 10.1016/j.jiph.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Kinirons B, Mimoz O, Lafendi L, Naas T, Meunier J, Nordmann P. Chlorhexidine versus povidone iodine in preventing colonization of continuous epidural catheters in children: A randomized, controlled trial. Anesthesiology. 2001;94:239–44. doi: 10.1097/00000542-200102000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Chaiyakunapruk N, Veenstra DL, Lipsky BA, Saint S. Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: A meta-analysis. Ann Intern Med. 2002;136:792–801. doi: 10.7326/0003-4819-136-11-200206040-00007. [DOI] [PubMed] [Google Scholar]
- 17.Noorani A, Rabey N, Walsh SR, Davies RJ. Systematic review and meta-analysis of preoperative antisepsis with chlorhexidine versus povidone-iodine in clean-contaminated surgery. Br J Surg. 2010;97:1614–20. doi: 10.1002/bjs.7214. [DOI] [PubMed] [Google Scholar]
- 18.Lee I, Agarwal RK, Lee BY, Fishman NO, Umscheid CA. Systematic review and cost analysis comparing use of chlorhexidine with use of iodine for preoperative skin antisepsis to prevent surgical site infection. Infect Control Hosp Epidemiol. 2010;31:1219–29. doi: 10.1086/657134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Widerström M, Wiström J, Sjöstedt A, Monsen T. Coagulase-negative staphylococci: Update on the molecular epidemiology and clinical presentation, with a focus on Staphylococcus epidermidis and Staphylococcus saprophyticus. Eur J Clin Microbiol Infect Dis. 2012;31:7–20. doi: 10.1007/s10096-011-1270-6. [DOI] [PubMed] [Google Scholar]
- 20.Grewal S, Hocking G, Wildsmith JA. Epidural abscesses. Br J Anaesth. 2006;96:292–302. doi: 10.1093/bja/ael006. [DOI] [PubMed] [Google Scholar]
- 21.Eggimann P, Pittet D. Overview of catheter-related infections with special emphasis on prevention based on educational programs. Clin Microbiol Infect. 2002;8:295–309. doi: 10.1046/j.1469-0691.2002.00467.x. [DOI] [PubMed] [Google Scholar]
- 22.Hebl JR, Niesen AD. Infectious complications of regional anesthesia. Curr Opin Anaesthesiol. 2011;24:573–80. doi: 10.1097/ACO.0b013e32834a9252. [DOI] [PubMed] [Google Scholar]
- 23.Zamora JL, Price MF, Chuang P, Gentry LO. Inhibition of povidone-iodine's bactericidal activity by common organic substances: An experimental study. Surgery. 1985;98:25–9. [PubMed] [Google Scholar]
- 24.Larson E, Bobo L. Effective hand degerming in the presence of blood. J Emerg Med. 1992;10:7–11. doi: 10.1016/0736-4679(92)90003-c. [DOI] [PubMed] [Google Scholar]
- 25.Adams D, Quayum M, Worthington T, Lambert P, Elliott T. Evaluation of a 2% chlorhexidine gluconate in 70% isopropyl alcohol skin disinfectant. J Hosp Infect. 2005;61:287–90. doi: 10.1016/j.jhin.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 26.Shelton DM. A comparison of the effects of two antiseptic agents on Staphylococcus epidermidis colony forming units at the peritoneal dialysis catheter exit site. Adv Perit Dial. 1991;7:120–4. [PubMed] [Google Scholar]


