Abstract
Prior research has documented a link between perceived neighborhood safety and functional limitations including incident mobility limitation, yet no research has explored the association between perceived neighborhood safety and recovery from functional limitations. This study investigates whether perceived neighborhood safety independently predicts recovery. Using longitudinal data from the Health and Retirement Study (HRS) (1996–2008), discrete-time event history models with multiple competing events were estimated using multinomial logistic regression. Robust standard errors were used to adjust for clustering. In the unadjusted model, the odds ratio for recovery from mobility limitations was 1.22 (CI: 1.17, 1.27) for respondents reporting greater neighborhood safety, while, in the fully adjusted model, the odds ratio was 1.11 (CI: 1.05, 1.17). Even after controlling for sociodemographic characteristics and numerous health risk factors, perceived neighborhood safety was a robust predictor of mobility limitation recovery. This research provides further evidence that environmental factors shape functional health outcomes including recovery.
Keywords: mobility, recovery, perceived neighborhood safety
Over the last two decades the impact of neighborhood contexts on the health of their residents has become a major field of research in population health. This includes a growing interest in the role of the neighborhood environment for functional health and functional limitations. Prior research underscores the importance of the social and physical neighborhood environment for functional health declines, where positive neighborhood characteristics are negatively associated with functional health declines. This relationship is quite robust and observed for multiple measures of functional health such as mobility limitation (Clarke, Ailshire, Bader, Morenoff, & House, 2008; Clark et al., 2009; Clarke, Ailshire, & Lantz, 2009), lower-body functional limitation (Balfour & Kaplan, 2002; Schootman et al., 2006), disability (Beard et al., 2009; Freedman, Grafova, Schoeni, & Rogowski, 2008; White et al., 2010), and social participation (Clarke, Ailshire, Nieuwenhuijsen, & de Kleijn-de Vrankrijker, 2011). Yet, functional health outcomes often reflect a dynamic process, where the onset of physical limitations is followed by a recovery to independent function. For example, in a longitudinal study of 754 community-dwelling older adults, Hardy and Gill (2004) found that four out of five persons reporting disability in basic Activities of Daily Living (ADL) recovered within 12 months of their initial onset. Yet, there is no research examining the association between the neighborhood environment and functional health recovery. Given the established relationship between contextual factors and functional health declines, it is important to understand how the neighborhood environment may shape functional health recovery.
Using data from a nationally-representative, longitudinal study of late-midlife adults in the United States (US), this research uniquely contributes to the extant literature by exploring recovery from a functional limitation (i.e., mobility limitation) and how that recovery is shaped by the neighborhood environment (i.e., perceived neighborhood safety). As evidence begins to surface of a potential increase in disability among US adults in late-midlife (see Martin, Freedman, Schoeni, & Andreski, 2010; Seeman, Merkin, Crimmins, & Karlamangla, 2010), interventions aimed at facilitating recovery from functional limitations may become even more salient. Modifications to the neighborhood environment may have the potential to facilitate mobility and independent function for adults who are aging in place.
Mobility Limitation and the Neighborhood Environment
There are multiple definitions and measures that attempt to operationalize functional health. Mobility limitation is often measured as difficulty walking, climbing, and/or standing. Difficulty walking, especially short distances, is often viewed as mobility disability and reflects a severe mobility limitation. Other common measures of disability include Activities of Daily Living (ADL) (e.g., difficulty bathing, dressing, or eating) and Instrumental Activities of Daily Living (IADL) (e.g., difficulty shopping, cooking, or managing money). There is theoretical and empirical evidence linking mobility limitation to subsequent ADL and IADL disability. For example, the Disablement Process (Verbrugge and Jette, 1994), describes a pathway from underlying health conditions to disability onset; the main pathway illustrates a connection between functional limitations such as mobility limitation and disability onset. Furthermore, prior research has demonstrated that mobility limitation is an important antecedent of disability (Guralnik et al., 1994; Ostir, Markides, Black, & Goodwin, 1998; Guralnik et al., 2000). In community samples of older adults, difficulty with mobility has been shown to predict subsequent disability in activities of daily living, as well as institutionalization and mortality up to 4 years later (Fried, Bandeen-Roche, Chaves, & Johnson, 2000; Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995). Compared to ADL and IADL disability, mobility limitation is viewed as an early stage in the disabling process, and therefore, a more reversible functional health outcome (Simonsick et al., 2008). As a result, interventions designed to prevent or minimize mobility limitations are considered important steps in the sequence to prevent subsequent disability.
The extant literature focusing on functional health and the neighborhood environment has underscored the importance of contextual environmental factors for numerous functional health outcomes including mobility limitation and ADL/IADL disability. For example, living in neighborhoods with poor street conditions, heavy traffic, and excessive noise have been shown to be associated with the onset of difficulty with movement related activities (e.g. standing in place, lifting heavy objects, climbing stairs) (Balfour & Kaplan 2002; Schootman et al. 2006) and disability, net of individual characteristics (Freedman et al., 2008; Beard et al., 2009). Data from the city of Chicago indicate that poor street conditions are associated with four-fold higher odds of walking difficulty among adults with underlying lower extremity weakness (Clarke et al. 2008). Results from nationally representative panel data in the United States have shown that living in neighborhoods characterized by more motorized travel is associated with 50% higher odds of reporting mobility limitations over time (Clarke et al., 2009).
Social environmental factors (e.g., neighborhood safety, social cohesion, or collective efficacy) have also been linked to functional health declines. Martin, Shreffler, Schoster, and Callahan (2010) showed that perceived aesthetics, walkability, safety, and social cohesion were significant predictors of disability, even after adjusting for numerous individual characteristics. Similarly,Clark et al. (2009) demonstrated a robust association with perceived neighborhood safety and incident mobility limitation. A recent study conducted byClarke et al. (2011) found lower rates of interpersonal interaction among individuals with mobility impairment living in neighborhoods perceived as unsafe. As the neighborhood environment and functional health literature continues to grow, there is mounting evidence highlighting the significance of both the physical and social environment for functional health outcomes. We extend this literature by examining the role of the neighborhood environment for functional health recovery.
Mobility Limitation and Recovery
There is a limited body of literature exploring predictors of recovery from functional health declines. Most research exploring recovery focuses on disability and utilizes clinical data, yet these studies provide evidence of recovery facilitators at the individual level. Among sociodemographic characteristics, prior research suggests that being female or older is associated with a lower likelihood of recovery from disability or mobility limitation (Peres, Verret, Alioum, & Barberger-Gateau, 2005; Gill, Allore, Hardy, & Guo, 2006). Additionally, lower levels of educational attainment have been linked to less recovery (Jagger, Matthews, Melzer, Matthews, & Brayne 2007) as well as being unmarried (Peres et al., 2005). Other predictors of recovery are health related. For example, the severity of impairment and the number of comorbid chronic health conditions are inversely associated with recovery from disability and mobility limitation (Clark, Stump, & Wollnsky, 1998; Hardy & Gill, 2004). Health risk behaviors (Gill, Robison, & Tinetti, 1997) and frailty (Hardy & Gill, 2004) are associated with a lower likelihood of disability recovery. Mental health status (i.e., cognitive impairment and depressive symptoms) is related to recovery, where more cognitive impairment or depressive symptoms have been shown to prevent recovery (Gill et al., 1997; Cronin-Stubbs et al., 2000; Hardy & Gill, 2004).
Research exploring the link between recovery and social support provides evidence that social environmental factors influence functional health recovery above and beyond individual characteristics. For example, using data from a community-based sample of older adults, Mendes de Leon et al. (1999) found that being embedded in a social network of relatives and friends enhanced the odds of recovery from ADL disability over a period of 9 years. Yet, in general, there are very few studies examining recovery from functional health declines—and even fewer exploring the influence of neighborhood environmental factors on recovery.
Perceived Neighborhood Safety
Perceived neighborhood safety is a multifaceted measure of the neighborhood environment. Neighborhood safety ratings are influenced by many social and physical environmental factors and individual characteristics. Previous research suggests that an individual’s neighborhood satisfaction and neighborhood property crime rates predict safety ratings (Baba & Austin, 1989). Similarly, a recent study conducted by De Jesus, Puleo, Shelton and Emmons (2010) demonstrates a link between social cohesion and neighborhood safety ratings. De Jesus and colleagues’ (2010) research also highlights the importance of educational attainment for an individual’s neighborhood rating. Other social environmental predictors of perceived neighborhood safety include an individual’s victimization status and whether an individual has been approached by a drug dealer (Payne & Gainey, 2007) as well as neighborhood attachment (Delisi & Regoli, 2000). Austin, Furr and Spine (2002) provide research linking physical environmental factors to perceived neighborhood safety using measures of housing quality and perceptions of the physical environment (i.e., appearance, noise, litter, and space).
Although objective measures are typically preferred by researchers, perceived neighborhood safety is a valuable measure because perception may be more powerful for functional health and mobility, especially among older adults. To illustrate, there is some evidence that perceived neighborhood deterioration is a stronger predictor of fear of crime than objective measures of neighborhood deterioration (Perkins and Taylor, 1996). Within the context of mobility, poor ratings of neighborhood safety may be a more salient barrier because they prevent physical activity, including walking outdoors (Mendes de Leon et al., 2009; Wang & Lee, 2010). Since regular physical activity has been shown to be important for the prevention or delay of mobility-related disability (Alexander & Goldberg, 2005; Rejeski et al., 2009), we extend this line of thinking to suggest that perceptions of neighborhood safety may have positive consequences for recovery from mobility limitations if residents are motivated to be mobile in their neighborhoods. The purpose of this research was to investigate perceived neighborhood safety in relation to mobility limitation recovery. Because of the strong and consistent findings relating perceived neighborhood safety to mobility limitation onset (incidence), we expect perceived neighborhood safety to be independently associated with mobility limitation recovery.
Methods
Data
Data for this research come from 7 waves of data (1996–2008) from the Health and Retirement Study (HRS), which is an ongoing, nationally-representative, panel study of American adults. The HRS is sponsored by the National Institute of Aging (grant number NIA U01AG009740) and is conducted by the Institute for Social Research at the University of Michigan (HRS, 2011). This research utilizes the HRS public release data, which has been stripped of any identifying information to ensure confidentiality. All procedures in the HRS are reviewed and approved on an annual basis by the University of Michigan’s Institutional Review Board (IRB), and all study subjects are provided written informed consent.
The initial goal of the HRS was to describe in detail the lives of a late-midlife US cohort (born 1931–1941) including collecting in-depth information about their health, finances, family structure, and employment history. Baseline face-to-face interviews were conducted in 1992, when respondents were age 51–61 years. Since baseline, two year follow-up telephone surveys have been conducted. The initial sample size was approximately 12,654 people (including age-eligible respondents and their spouses). The HRS employs a multi-stage, clustered probability frame and oversamples key groups (i.e., Blacks/African Americans, Hispanics, and Florida residents). The response rate for the original HRS baseline sample was 81.4%; response rates for subsequent waves have varied from 84.0% to 89.1%. In 2004, it was estimated that 15.9% of the original HRS baseline sample had died (HRS, 2011).
To assist in the data management and analysis of this project, the most recent RAND HRS Data file (version K) was used. The RAND HRS Data file is a user friendly, longitudinal data set created from original HRS data by the National Institute on Aging and the Social Security Administration (RAND, 2011). The RAND data file pays special attention to the cross-wave concordance of variables to maximize the longitudinal potential of HRS, including the careful imputation of missing data (RAND, 2011). The sample (N=7,122) for this study includes HRS respondents and their age-eligible spouses who were between the ages of 55–65 years at Wave 3 (1996) and excludes respondents with proxy information. Respondents with proxy information were omitted from the analysis, so that mental health could be evaluated. Proxies did not provide information for depressive symptoms or cognition. Moreover, the use of proxy information would have introduced greater reliability issues in relation to mobility limitations. This research investigated recovery from mobility limitation based on self-reported difficulty—it is necessary to have consistent assessments of difficulty throughout the observational period.
Measures
Mobility limitation recovery was measured using self-reports of difficulty completing five acts: 1) walking across the room; 2) walking one block; 3) walking several blocks; 4) climbing up one flight of stairs without resting; and 5) climbing up several flights of stairs without resting. The specific wording for each question was: “Because of a health problem do you have any difficulty with ________.” Mobility limitation recovery was defined as having any limitation (any difficulty) in a previous wave and then reporting no limitation (no difficulty) in the subsequent wave. Respondents may have reported difficulty with more than one act; however, recovery was defined as completely regaining mobility (i.e., no difficulty with all five acts).
The independent variable of interest, perceived neighborhood safety, was measured using the question: “Would you say the safety of your neighborhood is excellent, very good, good, fair or poor?” Perceived neighborhood safety was assessed starting at Wave 3 (1996); therefore, the analysis was restricted to Waves 3–9 (1996–2008). An ordinal scale of perceived neighborhood safety was created where excellent=5 and poor=1. We compared models using linear coding and non-parametric coding (i.e., a series of dummy variables) of perceived neighborhood safety to ascertain the appropriate parameterization of the measure. The non-parametric coding of perceived neighborhood safety did not significantly improve model fit; therefore, we elected to use the more parsimonious linear version of this variable. Perceived neighbor safety was treated as a time-varying variable. Sociodemographic characteristics and health risk factors were included in the analyses as control variables. There were both time-fixed and time-varying sociodemographic characteristics; time-fixed measures included gender, race/ethnicity, educational attainment, and age (i.e., relative age within sample), while marital status, income, and wealth were treated as time-varying measures. A dichotomous dummy variable was created for gender, where female=1. Three dummy variables capture race/ethnicity comparing White (reference), with Black/African American, Latino/Hispanic, and Other Race. A three category measure of education was created based on credential achievement: less than high school (i.e., respondents without a high school diploma or equivalent such as a GED), high school (i.e., respondents with a high school diploma or equivalent) (reference), and more than high school (i.e., respondents with an Associate degree or higher). Age was measured at Wave 3 (1996) in years at time of interview. Among the time-varying sociodemographic characteristics, marital status was measured using a four-category dummy variable with married/partnered (reference), divorced/separated, widowed, and never married as the categories. Both household income and wealth were measured using quartiles with the upper quartile used as the reference. Household income and wealth quartiles were generated using the original HRS sample.
All health risk factors were treated as time-varying and included measures of health behaviors, healthcare access, and morbidity status. Three health behaviors were included in the analysis: physical activity, smoking status, and body mass index (BMI). Physical activity was measured using a single question, which asks respondents if they participate in vigorous exercise or sports 3 or more times a week. The physical activity measure was as a dichotomous variable, where participating in vigorous exercise or sports was assigned a value of 1. Smoking status was measured as a three-category variable with never smoked, former smoker, and current smoker as the categories. A categorical measure of BMI was constructed from self-reported weight and height measures (height in meters/weight in kilograms squared); the categories were based established guidelines (CDC, 2011) and included underweight (BMI below 18.5), healthy weight (normal) (BMI = 18.5–24.9), overweight (BMI=25–29.9), and obese (BMI above 30).
A dichotomous measure for health insurance was created, where respondents with either individual or spousal private insurance=1. Health insurance coverage was measured as a time-varying variable. Four measures of morbidity status were employed including the number of chronic conditions, depressive symptoms, cognition impairment, and number of mobility limitations. An index of chronic conditions (i.e., arthritis, cancer, diabetes, heart problems, high blood pressure, lung disease, stroke, and psychiatric problems) was used. The chronic conditions were based on physician-diagnosed self-reports. Cognitive impairment was measured using the respondent’s serial 7s score. A respondent was asked to subtract seven from the previous number starting with 100 up to five attempts. An index ranging from 0 (i.e., no correct subtractions) to 5 (i.e., five correct subtractions) was created. This index was reversed so that cognitive impairment reflected the higher end of the scale. Depressive symptoms were measured using the Center for Epidemiology Studies Depression (CES-D 8) inventory, which ranged from 0 to 8 with higher scores representing more feelings associated with depression. Number of mobility limitations was also included in the analysis as a measure of mobility limitation severity.
Analytic Strategy
Discrete-time event history modeling with multiple competing events was estimated using multinomial logistic regression. With seven waves of data collected biennially, we have up to six 2-year intervals for each respondent. The risk group at the beginning of each interval included respondents with any mobility limitation, and possible outcomes included: any limitation (stable), no limitation (recovery), death, and attrition (i.e., lost to follow-up). Although death and attrition are explicitly modeled as competing events, the results are not presented, but are available upon request from the authors. Approximately 4–6% of the risk group experienced death per interval (contingent on the interval), whereas approximately 3–6% of the risk group attrited per interval. Odds ratios for recovery were then ascertained for each independent variable. Robust standard errors were employed to adjust for clustering within persons. The analyses were left unweighted because the attributes (e.g., gender, race/ethnicity, and marital status) for which the weights are calculated are included in the analysis and prior research has suggested that the unweighted data is less biased (see Botoseneanu & Liang, 2010; Winship & Radbill, 1994). However, analyses using weighted data (i.e., individual HRS respondent sampling weight and strata tracker file stratum weight) yielded a similar pattern of results. Because this research is interested in whether perceived neighborhood safety is an independent predictor of mobility limitation recovery, a series of models was created to examine the unadjusted and adjusted risk associated with perceived neighborhood safety. In Model 1, only perceived neighborhood safety was included. Model 2 introduced sociodemographic characteristics. Finally, in Model 3 (full model), health risk factors were included. This modeling strategy was utilized to examine the unadjusted effects of neighborhood safety for mobility limitation recovery as well as the effects after adjusting for common factors that could both select people into unsafe neighborhoods who are also less likely to recover.
Results
Distribution of Mobility Limitation and Perceived Neighborhood Safety
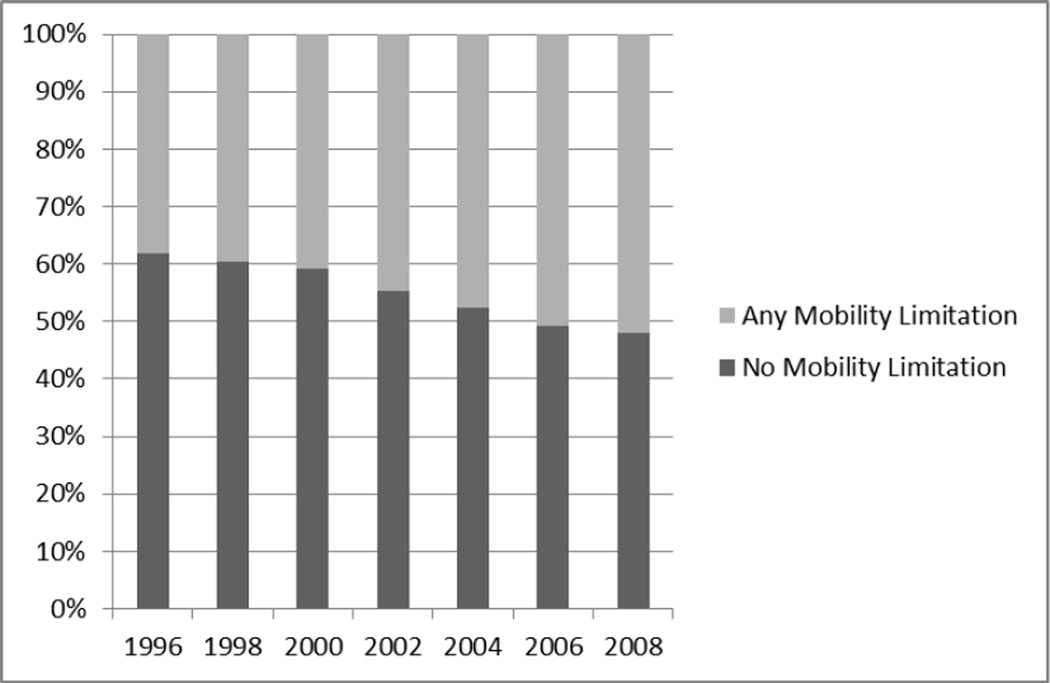
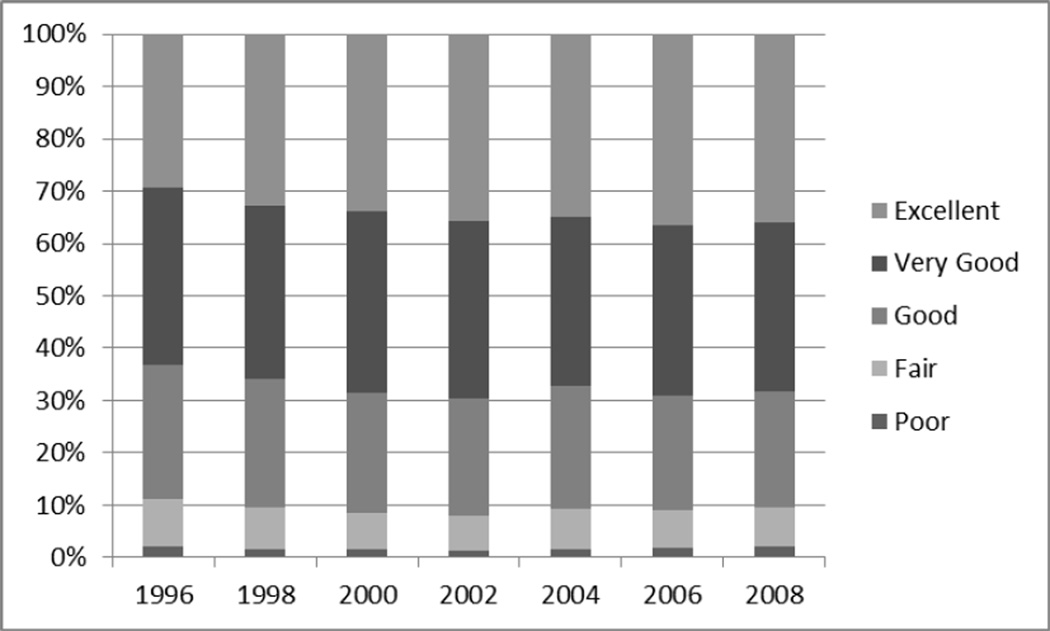
Figure 1 displays the distribution of mobility limitation by time for the entire sample. In 1996, approximately 38% of the sample reported some mobility limitation. Over the course of the study period, the amount of respondents reporting mobility limitation increased. By 2008, the majority (52%) of respondents reported having mobility limitation. Figure 2 presents the distribution of neighborhood safety rating across time. Generally, the vast majority of respondents rated their neighborhood safety as being good, very good, or excellent. For example, in 1996, only about 11% of respondents rated their neighborhood as fair or poor. Unlike mobility limitation, there is not a clear trend regarding perceived neighborhood safety over the course of the study; however, it appears that the number of respondents rating their neighborhood below good (i.e., fair or poor) remained relatively stable over time.
Figure 1. Distribution of Mobility Limitation by Time.
Figure 2. Distribution of Neighborhood Safety Rating by Time.
Descriptive Statistics for Initial Risk Group
The descriptive statistics for the initial risk group (i.e., respondents with mobility limitation at Wave 3) (N=2,709) are displayed in Table 1. Among respondents with mobility limitation in 1996, the mean perceived neighborhood safety score was 3.6, which corresponds to a rating of good/very good. The majority (67.5%) of the initial risk group was women, and the average age was about 60 years. The racial and ethnic composition of the initial risk group was disproportionately minorities compared to the original sample, while most (69.5%) respondents were White. Among the socioeconomic status (SES) measures (i.e., education, income, and wealth), there was an overrepresentation of lower SES respondents with approximately a third of the risk group having no high school degree. Over 36% of the initial risk group fell into the bottom household income and wealth quartile. The majority (66.3%) of respondents were married; however, compared to the original sample fewer respondents were married in the initial risk group.
Table 1.
Descriptive Statistics of Initial Risk Group (N=2,709)
| Distribution Informationa | |
|---|---|
| Perceived Neighborhood Safety (Range: 1–5) | 3.6 (1.1) |
| Sociodemographic Characteristics: | |
| Gender (Female=1) | 67.5% |
| Race/Ethnicity: | |
| White | 69.5% |
| Black/African American | 19.7% |
| Latino/Hispanic | 9.2% |
| Other Race | 1.6% |
| Age (Range: 55–65) | 59.8 (3.1) |
| Socioeconomic Status: | |
| Education: | |
| Less than High School | 32.8% |
| High School Degree/GED | 53.4% |
| More than High School | 13.8% |
| Income: | |
| Bottom Quartile | 36.9% |
| Bottom-Middle Quartile | 26.5% |
| Upper-Middle Quartile | 21.5% |
| Upper Quartile | 15.1% |
| Wealth: | |
| Bottom Quartile | 36.4% |
| Bottom-Middle Quartile | 26.2% |
| Upper-Middle Quartile | 21.0% |
| Upper Quartile | 16.4% |
| Marital Status: | |
| Married/Partnered | 66.3% |
| Separated/Divorced | 17.6% |
| Widowed | 11.7% |
| Never Married | 4.4% |
| Health Risk Factors: | |
| Health Behaviors: | |
| Physical Activity (yes=1) | 34.6% |
| Smoking Status: | |
| Never Smoked | 35.0% |
| Former Smoker | 38.3% |
| Current Smoker | 26.7% |
| Body Mass Index (BMI) | |
| Underweight | 3.2% |
| Healthy Weight | 24.3% |
| Overweight | 35.3% |
| Obese | 37.2% |
| Healthcare Access: | |
| Private Insurance (yes=1) | 54.5% |
| Morbidity Status: | |
| Number of Chronic Conditions (Range: 0–7) | 2.0 (1.3) |
| Cognition Impairment (Serial 7s Score) (Range: 0–5) | 2.3 (1.7) |
| Depressive Symptoms (CES-D 8 Score) (Range: 0–8) | 2.0 (2.3) |
| Number of Mobility Limitations (Range: 1–5) | 2.0 (1.2) |
Source: Health and Retirement Study (HRS) Data (1998)
Notes:
Percentage distributions are shown for categorical variables; means and (standard deviations) are shown for continuous variables.
Among the health risk behaviors, over a third (34.6%) of respondents reported that they participate in vigorous physical activity despite having mobility limitation. Current smokers represented 26.7% of the risk group, while former smokers represented 38.3%, and 35.0% the risk group had never smoked. Only 3.2% of the risk group was considered underweight. Among the BMI categories, obese (37.2%) represented the largest percentage of respondents. More than half (54.5%) of the risk group had private insurance in 1996. The average number of chronic conditions and number of mobility limitations was 2. Compared to the original sample, the respondents in the risk group reported more depressive symptoms and greater cognitive impairment. In general, the initial risk group (those with mobility limitations at the start of each interval) had fewer socioeconomic resources (e.g., lower income, education, and wealth) and poorer health compared to the original sample.
Odds Ratio Estimates for Mobility Limitation Recovery
Table 2 presents the odds ratio (OR) and 95% confidence intervals (CI) for mobility limitation recovery versus persistent mobility limitation by perceived neighborhood safety, sociodemographic characteristics, and health risk factors. For all models, the Likelihood Ratio was statistically significant at an alpha level of less than 0.001. In the unadjusted model (Model 1) the odds of recovery from mobility limitation increased by 22% for each unit increase in the neighborhood safety scale (OR=1.22). Model 2 introduced sociodemographic characteristics, and after adjusting for gender, race/ethnicity, age, SES, and marital status, the odds ratio for perceived neighborhood safety was attenuated to 1.12. For every additional positive rating of neighborhood safety, a respondent was about 12% more likely to recover from mobility limitation, net of sociodemographic characteristics. In Model 2, many of the sociodemographic characteristics were significantly associated with mobility limitation recovery. Women were less likely to recover (OR=0.77), while Black/African American (OR=1.25) and Latino/Hispanic (OR=1.51) respondents were more likely to recover. For both household income and wealth, compared to the upper quartiles, the lower three quartiles were all associated with lower likelihood of mobility limitation recovery.
Table 2.
Odds Ratio Estimates of Mobility Limitation Recovery by Perceived Neighborhood Safety, Sociodemographic Characteristics, and Health Risk Factorsa,b (Initial Risk Group: N= 2,709c)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | 95% C.I. | OR | 95% C.I. | OR | 95% C.I. | |
| Perceived Neighborhood Safety | 1.22*** | (1.17, 1.27) | 1.12*** | (1.07, 1.18) | 1.11*** | (1.05, 1.17) |
| Sociodemographic Characteristics: | ||||||
| Gender (Female=1) | 0.77*** | (0.69, 0.85) | 0.71*** | (0.63, 0.80) | ||
| Race/Ethnicity: | ||||||
| White (ref.) | ||||||
| Black/African American | 1.25* | (1.08, 1.46) | 1.27** | (1.08, 1.48) | ||
| Latino/Hispanic | 1.51*** | (1.25, 1.84) | 1.28* | (1.06, 1.56) | ||
| Other Race | 1.18 | (0.81, 1.71) | 0.96 | (0.65, 1.41) | ||
| Age | 1.01 | (0.99, 1.02) | 1.01 | (0.99, 1.03) | ||
| Socioeconomic Status: | ||||||
| Education: | ||||||
| Less than High School | 0.91 | (0.80, 1.04) | 1.07 | (0.93, 1.23) | ||
| High School Degree/GED (ref.) | ||||||
| More than High School | 1.14 | (0.99, 1.31) | 1.12 | (0.97, 1.29) | ||
| Income: | ||||||
| Bottom Quartile | 0.63*** | (0.53, 0.75) | 0.86 | (0.71, 1.04) | ||
| Bottom-Middle Quartile | 0.81** | (0.70, 0.94) | 0.92 | (0.79, 1.07) | ||
| Upper-Middle Quartile | 0.87* | (0.76, 0.99) | 0.90 | (0.78, 1.04) | ||
| Upper Quartile (ref.) | ||||||
| Wealth: | ||||||
| Bottom Quartile | 0.60*** | (0.51, 0.72) | 0.89 | (0.74, 1.06) | ||
| Bottom-Middle Quartile | 0.72*** | (0.61, 0.83) | 0.91 | (0.77, 1.06) | ||
| Upper-Middle Quartile | 0.85* | (0.74, 0.98) | 0.94 | (0.81, 1.09) | ||
| Upper Quartile (ref.) | ||||||
| Marital Status: | ||||||
| Married/Partnered (ref.) | ||||||
| Separated/Divorced | 0.97 | (0.83, 1.14) | 1.00 | (0.85, 1.18) | ||
| Widowed | 1.04 | (0.89, 1.21) | 1.03 | (0.85, 1.20) | ||
| Never Married | 1.05 | (0.80, 1.40) | 1.00 | (0.88, 1.32) | ||
| Health Risk Factors: | ||||||
| Health Behaviors: | ||||||
| Physical Activity (yes=1) | 1.30*** | (1.18, 1.44) | ||||
| Smoking Status: | ||||||
| Never Smoked (ref.) | ||||||
| Former Smoker | 0.92 | (0.82, 1.03) | ||||
| Current Smoker | 0.75*** | (0.64, 0.87) | ||||
| Body Mass Index (BMI) | ||||||
| Underweight | 0.89 | (0.65, 1.23) | ||||
| Healthy Weight (ref.) | ||||||
| Overweight | 0.94 | (0.83, 1.06) | ||||
| Obese | 0.69*** | (0.60, 0.79) | ||||
| Healthcare Access: | ||||||
| Private Insurance (yes=1) | 1.07 | (0.96, 1.19) | ||||
| Morbidity Status: | ||||||
| Number of Chronic Conditions | 0.76*** | (0.72, 0.79) | ||||
| Cognition Impairment (Serial 7s Score) | 0.97* | (0.94, 1.00) | ||||
| Depressive Symptoms (CES-D 8 Score) | 0.97* | (0.94, 0.99) | ||||
| Number of Mobility Limitations | 0.47*** | (0.44, 0.50) | ||||
| Observational Intervals: | ||||||
| Interval 1 (ref.) | ||||||
| Interval 2 | 0.96 | (0.71, 1.17) | 0.96 | (0.84, 1.10) | 1.03 | (0.89, 1.19) |
| Interval 3 | 0.85* | (0.75, 0.96) | 0.84* | (0.74, 0.96) | 0.91 | (0.79, 1.06) |
| Interval 4 | 0.79*** | (0.70, 0.90) | 0.78*** | (0.68, 0.89) | 0.90 | (0.78, 1.05) |
| Interval 5 | 0.69*** | (0.60, 0.78) | 0.66*** | (0.58, 0.76) | 0.85* | (0.73, 0.99) |
| Interval 6 | 0.70*** | (0.62, 0.80) | 0.69*** | (0.60, 0.79) | 0.96 | (0.81, 1.21) |
| Intercept | −1.90*** | −1.40** | 0.33 | |||
| Likelihood Ratio | 225.65*** | 766.50*** | 2823.02*** | |||
| Degrees of Freedom | 6 | 22 | 33 | |||
Source: Health and Retirement Study (HRS) (1996–2008)
Notes:
Risk group = respondents with mobility limitation;
Compared to respondents with persistent mobility limitation;
N= 15,486 Person-Intervals;
0.05 ≤p < 0.01;
0.01 ≤p < 0.001;
p ≤0.001.
Model 3 presents the fully adjusted model, which included health risk factors. The odds ratio in the full model for perceived neighborhood safety was 1.11. From Model 2 to Model 3, perceived neighborhood safety remained relatively stable. Positive ratings of neighborhood safety continued to be associated with greater likelihood of recovery from mobility limitation, controlling for sociodemographic characteristics and health risk factors. Women (OR=0.71) remained at lower risk of recovery, while Black/African American (OR=1.27) and Latino/Hispanic (OR=1.28) respondents continued to have a greater likelihood of recovery. In Model 3, the household income and wealth measures were no longer significant, suggesting that their effects on recovery may operate through health risk factors. Several health risk factors were linked to mobility limitation recovery including health behaviors and morbidity status. Among the health behaviors, physical activity (OR=1.30) was positively associated with increased likelihood of mobility limitation recovery, while being a current smoker (OR=0.75) or obese (OR=0.69) were associated with decreased likelihood. All four measures of morbidity status were negatively associated with mobility limitation recovery. More chronic conditions (OR=0.76) or mobility limitations (OR=0.47) were associated with reduced likelihood of recovery. Similarly, cognitive impairment (OR=0.97) or depressive symptoms (OR=0.97) were linked to lower risk of recovery.
The observation intervals in Models 1 and 2 exhibited a general trend of lower likelihood of mobility limitation recovery over the study period. For example, in Model 1, compared to interval 1, respondents in interval 6 (OR=0.70) were less likely to recover. However, in Model 3, the fully adjusted model, a general trend was no longer observed. Only interval 5 (OR=0.85) was significantly associated with mobility limitation recovery. Net of sociodemographic characteristics and health risk factors, there does not appear to be a clear trend for likelihood of mobility limitation recovery over the duration of the study.
We also tested whether the effects of neighborhood safety were particularly salient for specific high-risk sub groups of older adults by testing statistical interaction terms between perceived neighborhood safety and all sociodemographic characteristics. Additionally, interaction terms were tested incorporating each health risk behavior (including physical activity). No interaction terms were significantly associated with mobility limitation recovery, and therefore, were not included in the results. The effect of perceived neighborhood safety on mobility limitation recovery was robust across all models and was not moderated by other predictors.
Discussion
The disablement process is complex, with dynamic transitions into and out of disability states depending on both interpersonal and environmental factors (Hardy & Gill, 2004; Verbrugge & Jette, 1994). While numerous studies have examined the role of individual-level factors for both onset and recovery from disability and mobility limitation (Hardy & Gill, 2004; Peres et al., 2005; Gill et al., 2006; Jagger et al., 2007; Clark et al., 1998; Gill et al., 1997), to our knowledge this is the first study to examine the role of the surrounding neighborhood context for functional health recovery. Using a nationally representative sample of older Americans followed prospectively across a 12 year period, we investigated the role of neighborhood safety for recovery from mobility limitations. Our findings suggest that perceptions of a safe neighborhood environment are significantly associated with recovery from a mobility limitation over a two-year time interval, net of sociodemographic characteristics and health risk factors. These results provide further evidence that the neighborhood environment shapes functional health—including recovery from prior functional health declines.
Our findings may speak to future functional health interventions at the neighborhood level. Efforts to promote neighborhood safety, through better street lighting, better street conditions (walkability), or fewer indicators of crime, may encourage more physical activity and mobility among residents, which could then facilitate recovery from mobility limitations (Balfour & Kaplan, 2002; Schootman et al., 2006; Stathi et al. 2011). Furthermore, research examining barriers to physical activity among older adults with and without mobility limitation suggests that environmental barriers may be even more critical for older adults with severe to moderate mobility limitations compared to those without mobility limitation (Rasinaho, Hirvensalo, Leinonen, Lintunen, & Rantanen 2006). Preventing subsequent disability is a top priority for policy makers because of the immense financial burden of formal (and informal) care through healthcare expenditures. The neighborhood environment may hold unique potential as an area for health and aging policy makers because of the extreme relevance of aging in place. As older adults spend more time in their neighborhoods, the characteristics of these neighborhoods may provide facilitators or barriers for positive functional health outcomes.
Although the results of this research provide evidence of neighborhood effects on functional health recovery, they must be viewed in light of several limitations. A major limitation of this research is the two-year interval between observations; we cannot establish at what point during the study respondents recovered from their mobility limitation. It is also possible for respondents to have recovered multiple times, thus contributing to the study multiple observations of recovery. For example, racial and ethnic minorities were more likely to experience recovery; given the SES disadvantages and discrimination experienced by these groups, this is an unexpected finding. It is possible that racial and ethnic minorities experience intermittent onset/recovery episodes more often than Whites, which would not be indicative of better functional health, but they would contribute more recovery observations to the analysis. Additionally, attrition due to lost to follow-up and death is another limitation; however, both mortality and attrition (i.e., lost to follow-up) were included in the analyses as competing events. The omission of proxy information enabled the inclusion of mental health and increased confidence about the reliability of self-reported mobility limitation; however, it also introduced potential bias, where the at-risk group included respondents with less severe mobility limitation and a greater likelihood of recovery. Finally, this project only examines perceived neighborhood safety using a global assessment. Other more nuanced measures of perceived neighborhood safety may contribute to our understanding of which facets of neighborhood safety (e.g., perceived crime, appearance, or social cohesion) are most important for recovery. In the future, we plan to explore other neighborhood environment factors as predictors of functional health recovery.
Acknowledgements
Latham was supported by an NIA training grant from the University of Michigan (T32 AG000221). Additionally, the authors gratefully acknowledge use of the services and facilities of the Population Studies Center at the University of Michigan, funded by NICHD Center Grant (R24 HD041028).
Biographies
Kenzie Latham is currently an NIA Postdoctoral Fellow at Population Studies Center at the University of Michigan’s Institute for Social Research. Dr. Latham received her Ph.D. from the University of Florida in 2011, and her research interests include health and aging with an emphasis on functional health as well as chronic disease epidemiology. Much of Latham’s research focuses on identifying and understanding health disparities among older adults.
Philippa J. Clarke is a Research Associate Professor at the University of Michigan’s Institute for Social Research. Dr. Clarke received her Ph.D. in Public Health from the University of Toronto in 2000. Her research interests are in social epidemiology, social gerontology, life course perspectives, models of disability, and population health. She is primarily interested in the social determinants of health at both the micro and macro levels of social reality and at the intersection of these levels as well.
References
- Alexander NA, Goldberg A. Common gait disturbances: A clinical overview. In: Hausdorff JM, Alexander NB, editors. Gait Disorders: Evaluation and Management. Boca Raton, FL: Taylor & Francis Group; 2005. pp. 1–18. [Google Scholar]
- Austin DM, Furr LA, Spine M. The effects of neighborhood conditions on perceptions of safety. Journal of Criminal Justice. 2002;30:417–427. [Google Scholar]
- Baba Y, Austin DM. Neighborhood environmental satisfaction, victimization, and social participation as determinants of perceived neighborhood safety. Environment and Behavior. 1989;21:763. [Google Scholar]
- Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. American Journal of Epidemiology. 2002;155:507. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- Beard JR, Blaney S, Cerda M, Frye V, Lovasi GS, Ompad D, Vlahov D. Neighborhood characteristics and disability in older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64:252. doi: 10.1093/geronb/gbn018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botoseneanu A, Liang J. Social stratification of body weight trajectory in middle-age and older Americans: Results from a 14-Year Longitudinal Study. Journal of Aging and Health. 2011;23(3):454–480. doi: 10.1177/0898264310385930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) About BMI for Adults. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Retrieved August 10th, 2011. ( http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html). [Google Scholar]
- Clark C, Kawachi I, Ryan L, Ertel K, Fay M, Berkman L. Perceived neighborhood safety and incident mobility disability among elders: the hazards of poverty. BMC Public Health. 2009;9:162. doi: 10.1186/1471-2458-9-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DO, Stump TE, Wollnsky FD. Predictors of onset of and recovery from mobility difficulty among adults aged 51–61 years. American Journal of Epidemiology. 1998;148:63. doi: 10.1093/oxfordjournals.aje.a009561. [DOI] [PubMed] [Google Scholar]
- Clarke P, Ailshire JA, Bader M, Morenoff JD, House JS. Mobility disability and the urban built environment. American Journal of Epidemiology. 2008;168:506. doi: 10.1093/aje/kwn185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, Ailshire JA, Lantz P. Urban built environments and trajectories of mobility disability: Findings from a national sample of community-dwelling American adults (1986–2001) Social Science & Medicine. 2009;69:964–970. doi: 10.1016/j.socscimed.2009.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke PJ, Ailshire JA, Nieuwenhuijsen ER, De Kleijn-De Vrankrijker MW. Participation among adults with disability: The role of the urban environment. Social Science & Medicine. 2011;1 doi: 10.1016/j.socscimed.2011.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronin-Stubbs D, Mendes De Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Archives of Internal Medicine. 2000;160:3074. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- De Jesus M, Puleo E, Shelton RC, Emmons KM. Associations between perceived social environment and neighborhood safety: Health implications. Health & Place. 2010;16:1007–1013. doi: 10.1016/j.healthplace.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delisi M, Regoli B. Individual neighborhood attachment and perceptions of neighborhood safety. American Journal of Criminal Justice. 2000;24:181–188. [Google Scholar]
- Freedman VA, Grafova IB, Schoeni RF, Rogowski J. Neighborhoods and disability in later life. Social Science & Medicine. 2008;66:2253–2267. doi: 10.1016/j.socscimed.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried LP, Bandeen-Roche K, Chaves PHM, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 2000;55:1, M43–M52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- Gill TM, Allore HG, Hardy SE, Guo Z. The dynamic nature of mobility disability in older persons. Journal of the American Geriatrics Society. 2006;54:248–254. doi: 10.1111/j.1532-5415.2005.00586.x. [DOI] [PubMed] [Google Scholar]
- Gill TM, Robison JT, Tinetti ME. Predictors of Recovery in Activities of Daily Living Among Disabled Older Persons Living in the Community. Journal of General Internal Medicine. 1997;12:757–762. doi: 10.1046/j.1525-1497.1997.07161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, Studenski S, Wallace RB. Lower extremity function and subsequent disability. The Journals of Gerontology Series A: Medical Sciences, 2000;55:M221. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology Series A: Medical Sciences. 1994;49:M85. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. The New England Journal of Medicine. 1995;33:2, 9, 556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA: The Journal of the American Medical Association. 2004;291:1596. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study (HRS), public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740) Ann Arbor, MI: 2011. [Google Scholar]
- Jagger C, Matthews R, Melzer D, Matthews F, Brayne C. Educational differences in the dynamics of disability incidence, recovery and mortality: Findings from the MRC Cognitive Function and Ageing Study (MRC CFAS) International Journal of Epidemiology. 2007;36:358. doi: 10.1093/ije/dyl307. [DOI] [PubMed] [Google Scholar]
- Martin KR, Shreffler J, Schoster B, Callahan LF. Associations of perceived neighborhood environment on health status outcomes in persons with arthritis. Arthritis Care & Research. 2010;62:1602–1611. doi: 10.1002/acr.20267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, Freedman VA, Schoeni RF, Andreski PM. Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Affairs. 2010;29:725. doi: 10.1377/hlthaff.2008.0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes De Leon CF, Cagney KA, Bienias JL, Barnes LL, Skarupski KA, Scherr PA, Evans DA. Neighborhood Social Cohesion and Disorder in Relation to Walking in Community-Dwelling Older Adults. Journal of Aging and Health. 2009;21:155–171. doi: 10.1177/0898264308328650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes De Leon CF, Glass TA, Beckett LA, Seeman TE, Evans DA, Berkman LF. Social networks and disability transitions across eight intervals of yearly data in the New Haven EPESE. The Journals of Gerontology Series B: Social Sciences, 1999;54:S162. doi: 10.1093/geronb/54b.3.s162. [DOI] [PubMed] [Google Scholar]
- Ostir GV, Markides KS, Black SA, Goodwin JS. Lower body functioning as a predictor of subsequent disability among older Mexican Americans. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 1998;53:M491. doi: 10.1093/gerona/53a.6.m491. [DOI] [PubMed] [Google Scholar]
- Payne BK, Gainey RR. Attitudes about the police and neighborhood safety in disadvantaged neighborhoods. Criminal Justice Review. 2007;32:142. [Google Scholar]
- Peres K, Verret C, Alioum A, Barberger-Gateau P. The disablement process: factors associated with progression of disability and recovery in French elderly people. Disability & Rehabilitation. 2005;27:263–276. doi: 10.1080/09638280400006515. [DOI] [PubMed] [Google Scholar]
- Perkins DD, Taylor RB. Ecological assessments of community disorder: Their relationship to fear of crime and theoretical implications. American Journal of Community Psychology. 1996;24:63–107. doi: 10.1007/BF02511883. [DOI] [PubMed] [Google Scholar]
- RAND HRS Data, Version K. Produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. Santa Monica, CA: 2011. [Google Scholar]
- Rasinaho M, Hirvensalo M, Leinonen R, Lintunen T, Rantanen T. Motives for and barriers to physical activity among older adults with mobility limitations. Journal of Aging and Physical Activity. 2007;1 doi: 10.1123/japa.15.1.90. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Marsh AP, Chmelo E, Prescott AJ, Dobrosielski M, Walkup M, Kritchevsy S. The lifestyle interventions and independence for elders pilot (LIFE-P):2-year follow-up. Journal of Gerontology: Biologic Sciences Medical Sciences. 2009;64A:4, 462–467. doi: 10.1093/gerona/gln041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schootman M, Andresen EM, Wolinsky FD, Malmstrom TK, Miller JP, Miller DK. Neighborhood conditions and risk of incident lower-body functional limitations among middle-aged African Americans. American Journal of Epidemiology. 2006;163:450. doi: 10.1093/aje/kwj054. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: National health and nutrition examination surveys 1988–1994 and 1999–2004. American Journal of Public Health. 2010;100:100. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonsick EM, Newman AB, Visser M, Goodpaster B, Kritchevsky SB, Rubin S, Harris TB. Mobility limitation in self-described well-functioning older adults: importance of endurance walk testing. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2008;63:841. doi: 10.1093/gerona/63.8.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stathi A, Gilbert H, Fox KR, Coulson J, Davis M, Thompson JL. Determinants of neighborhood activity of adults aged 70 and over: A mixed methods study. Journal of Aging and Physical Activity, 2012;20:148–170. doi: 10.1123/japa.20.2.148. [DOI] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Wang Z, Lee C. Site and neighborhood environments for walking among older adults. Health & Place. 2010;16:1268–1279. doi: 10.1016/j.healthplace.2010.08.015. [DOI] [PubMed] [Google Scholar]
- White DK, Jette AM, Felson DT, Lavalley MP, Lewis CE, Torner JC, Keysor JJ. Are features of the neighborhood environment associated with disability in older adults? Disability & Rehabilitation. 2010;32:639–645. doi: 10.3109/09638280903254547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winship C, Radbill L. Sampling weights and regression analysis. Sociological Methods & Research. 1994;23(2):230–257. [Google Scholar]