Abstract
STUDY QUESTION
Can reproductive life plan (RLP)-based information in contraceptive counselling before pregnancy increase women's knowledge of reproduction, and of the importance of folic acid intake in particular?
SUMMARY ANSWER
The RLP-based information increased women's knowledge of reproduction including knowledge of folic acid intake.
WHAT IS KNOWN ALREADY
Many women have insufficient knowledge of reproduction, including a health-promoting lifestyle prior to conception, and highly educated women in particular postpone childbearing until an age when their fertile capacity has started to decrease.
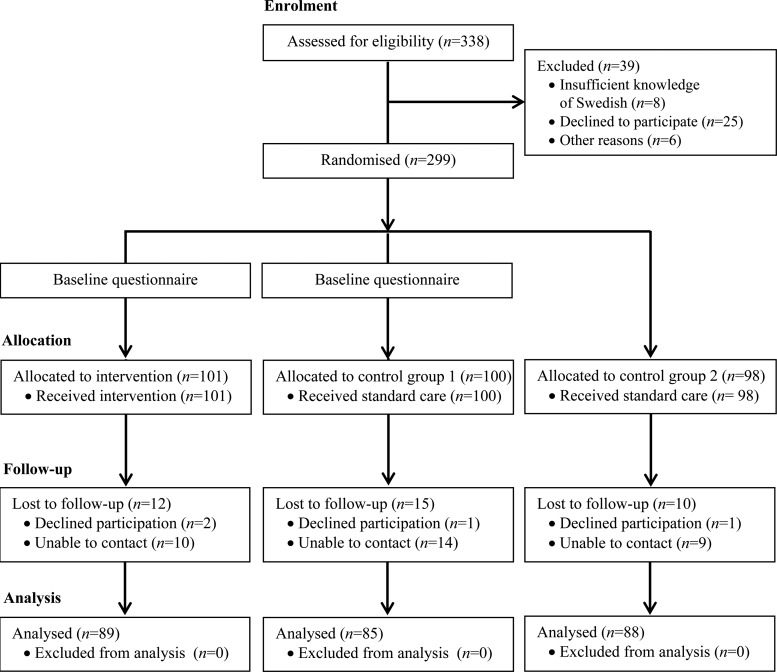
STUDY DESIGN, SIZE, DURATION
The study was an randomized controlled trial with one intervention group (IG) and two control groups (CG1, CG2). A sample size calculation indicated that 82 women per group would be adequate. Recruitment took place during 3 months in 2012 and 299 women were included. The women were randomized in blocks of three. All groups received standard care (contraceptive counselling, Chlamydia testing, cervical screening). In addition, women in the IG were given oral and written RLP-based information about reproduction.
PARTICIPANTS/MATERIALS, SETTING, METHODS
A total of 299 out of 338 (88%) Swedish-speaking women visiting a Student Health Centre were included (mean age 23 years); response rate was 88%. Before the counselling, women in the IG and the CG1 completed a baseline questionnaire, including questions about lifestyle changes in connection to pregnancy planning, family planning intentions and knowledge of reproduction (e.g. the fecundity of an ovum). At follow-up 2 months after inclusion, a structured telephone interview was performed in all groups (n = 262, 88% participation rate).
MAIN RESULTS AND THE ROLE OF CHANCE
There was no difference between the groups regarding the mean knowledge score at baseline. The IG scored higher at follow-up than at baseline (P < 0.001); the mean increased from 6.4 to 9.0 out of a maximum 20 points. The women in the CG1 scored no differently at follow-up than at baseline. The difference in the knowledge score between the IG and the two CGs was significant (P < 0.001), whereas no difference was shown between the two CGs. There was no difference between the groups at baseline regarding how many women could mention folic acid intake among the things to do when planning to get pregnant. At follow-up, 22% in the IG, 3% in CG1 and 1% in CG2 mentioned folic acid intake (P < 0.001). At follow-up, more women in the IG also wished to have their last child earlier in life (P < 0.001) than at baseline, while there was no difference in the CG1.
LIMITATIONS, REASONS FOR CAUTION
As the study sample consisted of university students, it is possible that the effect of the intervention was connected to a high level of education and conclusions for all women of reproductive age should be drawn with caution.
WIDER IMPLICATIONS OF THE FINDINGS
The provision of RLP-based information seems to be a feasible tool for promoting reproductive health.
STUDY FUNDING/COMPETING INTEREST(S)
Study funding was received from the Faculty of Medicine, Uppsala University, Sweden. There are no conflicts of interest.
TRIAL REGISTRATION NUMBER
ClinicalTrial.gov Identifier NCT01739101.
Keywords: health education, reproductive health, fertility, pregnancy
Introduction
Human reproduction is a central issue for the individual and for society. Sexual and reproductive health in Sweden is generally good compared with international data but there are some worrying trends. The use of condoms has declined and sexually transmitted infections (STIs) are increasing (The National Board of Health and Welfare, 2009). Furthermore, the abortion rate in Sweden is the highest among the Nordic countries (The Finnish National Institute for Health and Welfare, 2009) and the highest abortion rate in Sweden is found among women aged 20–29 years (The National Board of Health and Welfare, 2012a). As in other parts of Europe, women in Sweden delay childbearing until ages when reproductive capacity is decreased and the risk for age-related complications during pregnancy is increased; the mean age of first-time mothers is close to 29 years, and 13% of them are 35 years or older (The National Board of Health and Welfare, 2012b). Along with technical improvements this has led to a 4-fold increase of IVF in the last decade (The National Board of Health and Welfare, 2012b).
Attitudes to having children in the future have been investigated among the highly educated in Sweden, who tend to postpone childbearing more than those with lower education (Andersson et al., 2009; Statistics Sweden, 2011). Although it is often concluded that there will never be a perfect time for having children, many state prerequisites for parenthood, such as being of reasonable age, having a partner ready for a child, good living conditions and stable finances (Tydén et al., 2006; Eriksson et al., 2012). In studies among university students, the majority want to have on average two to three children; the first child at age 28–32 years and their last child after age 35 years (Skoog Svanberg et al., 2006; Lampic et al., 2006). Six out of 10 women would choose to have an abortion if they became pregnant during their studies (Tydén et al., 2006). Men and women are not sufficiently aware about age and fertility, and they overestimate the success rate of assisted reproduction techniques (Lampic et al., 2006; Skoog Svanberg et al., 2006). Knowledge gaps about fertility issues have also been found among US, Finnish, Italian, Israeli and Canadian university students (Bretherick et al., 2010; Rovei et al., 2010; Hashiloni-Dolev et al., 2011; Virtala et al., 2011; Peterson et al., 2012).
Sexual health education, including basic information about reproduction, has been mandatory in Swedish schools for over 50 years (Agency for School Improvement, 2005; The Swedish National Agency for Education, 2011). The national guidelines do not, however, specify how or by whom the education should be implemented, and there are consequently differences in quality and quantity of sexual health education both between and within schools (The Swedish National Agency for Education, 2000). The official responsibility for family planning in Swedish health care lies within maternity care (The National Board of Health and Welfare, 2008) but the responsibility for coordinating measures to prevent unwanted pregnancies at a governmental level is unclear (The Ministry of Health and Social Affairs, 2009). If appointments for contraceptive counselling, screening for Chlamydia and cervical screening are discounted, the majority of women will either enter the maternal health-care system once pregnant or when having trouble conceiving (The National Board of Health and Welfare, 2012a). As there are no recommendations or guidelines for pre-pregnancy counselling, i.e. preconception care, within the Swedish health-care system, many women are unaware of the recommended health-promoting lifestyle changes to increase their chances of becoming pregnant and of having a normal pregnancy and a healthy child, until it is too late. One example of these is the intake of folic acid. Daily intake of folic acid 1 month prior to pregnancy reduces the risk of fetal neural tube defects by up to 70% (Medical Research Council, 1991), and is therefore recommended by the National Food Agency (2013) for all women of reproductive age. A Swedish study shows that only 20% of pregnant women had taken folic acid in connection with pregnancy planning (Tydén et al., 2011).
The Health Belief Model (HBM) is a theoretical framework for understanding health behaviour. According to the HBM, a person will take action to prevent a health condition only if she (i) considers herself susceptible to the condition, (ii) estimates the consequences of the condition to be severe enough, (iii) believes the specific action is effective in decreasing the risk, (iv) believes that the benefit of the action outweighs the barriers to, or cost of, taking the action and (v) has enough self-efficacy. These beliefs are influenced by modifying factors, such as age, gender, ethnicity, socioeconomics and knowledge. The model also describes cues to action, which is something that activates the individual behaviour (Champion and Skinner, 2008). The HBM has been applied to different areas within sexual and reproductive health, for example knowledge of human papillomavirus (Gottvall et al., 2010), sexual risk taking (Ekstrand et al., 2011) and contraception (Brown et al., 2011). In this study, the HBM was used as a theoretical framework for understanding different aspects of family planning.
The reproductive life plan (RLP) is a tool developed in an American context for reproductive health promotion in a life cycle perspective (Moos et al., 2008) and consists of a set of non-normative questions about having or not having children (Moos, 2003). The RLP aims to encourage both women and men to reflect on their reproductive intentions and to find strategies for successful family planning, for example to have the wanted number of children and to avoid unwanted pregnancies as well as ill-health that may threaten reproduction (Centers for Disease Control and Prevention, 2006). The RLP can be used both in counselling and in a written form, as booklets or worksheet (http://www.cdc.gov/preconception/documents/ReproductiveLifePlan-Worksheet.pdf). The Centers for Disease Control and Prevention has recommended the RLP as a tool to increase preconception health and decrease both unintended pregnancies and adverse pregnancy outcomes, and emphasizes the importance of integrating reproductive health in primary health care (Centers for Disease Control and Prevention, 2006). Several descriptions of the RLP are available in the literature (Moos, 2003; Sanders, 2009; Malnory and Johnson, 2011; Barry, 2011) and one study demonstrates that assessment of RLP in primary care is appreciated by exposed patients (Dunlop et al., 2010). In spite of this, no previous study has systematically evaluated the effectiveness of using an RLP protocol in clinical practice. In the present study we evaluated the use of an RLP protocol as a starting point for providing structured information about reproduction in contraceptive counselling.
The aim of our study was to investigate if RLP-based information in contraceptive counselling increases women's knowledge of reproduction, and particularly knowledge of folic acid intake, prior to pregnancy. Secondary aims were to evaluate the influence on women's family planning and to explore different aspects of the women's overall experience of the RLP-based information. Although the RLP is developed to target both men and women, this study will focus on women only.
Materials and Methods
Setting, participants and procedure
The study had a randomized controlled design and the procedure is illustrated in Fig. 1. The study took place at a Student Health Centre from March to June 2012. Female students (n = 338) who visited midwives for contraceptive counselling (n = 287), Chlamydia testing (n = 37) or cervical screening (n = 14) were invited in consecutive order to participate in the study. Swedish midwives are licensed to prescribe hormonal contraceptives and to insert intrauterine devices and implants for women without medical problems. The midwives at the Student Health Centre have 15 min allotted for each consultation. Some appointments take 15 min or more while others (prescription of gestagen-only pills, testing for Chlamydia) take less time. Three midwives (among these the last author, T.T.) at the clinic recruited the participants. The only exclusion criterion was insufficient knowledge of Swedish. Before the study, the principal investigator (J.S.) informed the midwives about the concept of the RLP and the study procedure to ensure equivalent execution. During the study period, all visits to the midwives were scheduled for 5 extra minutes.
Figure 1.
CONSORT flow diagram for the randomized controlled trial (RCT) to study the benefit of using RLP-based information in contraceptive counselling.
The power calculation was conducted on a previous study showing that only 20% of women of reproductive age have knowledge of the recommended folic acid intake before pregnancy (The National Food Agency, 2010). The calculations assumed that the intervention would increase the knowledge of folic acid to 40% (i.e. increase by 100%). To detect a difference between the intervention and control groups with 80% power and with a significance level of P < 0.05, 82 women were needed in each group. In order to allow for possible drop-out during the study, we planned to recruit 100 women in each group.
During the study period, 338 women visited the clinic and were assessed for eligibility. The study procedure is shown in Fig. 1. The midwives informed eligible women about the study in the waiting room, ensuring that they knew that participation was voluntary and could be ended at any time without further explanation or consequences for treatment. The women received both verbal and written information before giving their written consent. The response rate was 88% (n = 299).
The women who accepted participation were randomized in blocks of three by receiving a sealed envelope containing instructions for either the intervention group (IG, n = 101) or one of two control groups (CG1, n = 100 and CG2, n = 98). The envelopes for the IG were coded so that the midwife would know whom to give the intervention to. Before the counselling the IG and CG1 completed a baseline questionnaire in the waiting room. In order to be able to analyse the effect of the questionnaire per se, the women in CG2 were not asked to complete this questionnaire.
All groups received standard care. The national guidelines for standard care in contraceptive counselling includes taking a medical history (heredity, medication, previous pregnancies and previous experiences of contraception), measuring blood pressure and weight, counselling and provision of contraceptives (Medical Products Agency, 2005). Standard care for Chlamydia testing and cervical screening is the testing procedure as such, with no extensive counselling involved. In addition to standard care the IG received the RLP-based intervention.
Two months after the visit (May to August) trained research assistants interviewed the women in all groups according to a structured questionnaire equivalent to the baseline questionnaire. The follow-up was conducted by telephone instead of mail or email to minimize the risk that the women would check the brochure or other source for information for the correct answers to the knowledge questions while answering and thereby biasing the results. Non-responders were approached repeatedly via telephone, text message and email. Of the 299 women who entered into the study, 262 (88%) participated in the follow-up interview. After the interviews the brochure used in the intervention was sent to the women in CG1 and CG2 in order to provide them with the same information about reproduction that was given to the IG.
The study was approved by the Regional Ethical Review Board in Uppsala, Sweden.
Instrument
The main outcome measure was knowledge of reproduction including knowledge of folic acid intake prior to conception. Secondary outcome measures were family planning intentions and the experience of the intervention.
The questionnaire was designed by the authors to evaluate the intervention and was developed on the basis of earlier research (Moos, 2003; Lampic et al., 2006; Tydén et al., 2006; Skoog Svanberg et al., 2006; Champion and Skinner, 2008). It was reviewed and commented on by researchers, clinicians and laypeople to ensure high face and construct validity. To test the instrument and procedure, we also conducted a pilot study with 25 women in each group. Based on feedback from the women, the phrasing of two questions was modified and a clarifying explanation was added. The final baseline questionnaire included 28 questions.
Background/demographic data (seven items)
The women were requested to state the date, their age, level of university education, own and parents' country of birth, sexual orientation and if they currently were in a stable relationship or not.
Reproductive history (five items)
The women were asked if they had experience of trying to get pregnant and, if so, any problems in achieving pregnancy. Further questions covered personal experience of pregnancy and, if so, how it ended (abortion, miscarriage, currently pregnant or childbirth); history of STI and which method(s) of contraception (if any) they had used during their last intercourse.
Family planning/RLP (six items)
The questions were based on the RLP description by Moos (2003). The first item was ‘do you want children/more children?’ (yes/no/don't know) and affirmative responses were followed by three questions about how many children and the desired age for having the first and last child. The women were also requested to state how confident they felt in having the number of children they desired on a visual analogue scale (VAS) with the extreme values ‘not confident at all’ (0) and ‘totally confident’ (10). Finally, all women were requested to state how likely it was that a pregnancy within the following 6 months would be planned, with four response alternatives ranging from ‘very likely’ to ‘totally unlikely’.
Knowledge about different aspects of reproduction (six items)
The knowledge questions were open ended to minimize the risk of an overestimation of the knowledge by listing alternatives. Three of the questions have previously been validated and used in Swedish settings (Lampic et al., 2006; Tydén et al., 2006; Skoog Svanberg et al., 2006). One question about the fecundity of an ovum was developed with the same structure. Finally, two questions with free text answers were developed covering factors that can impair female fertility and healthy lifestyle during pregnancy planning.
Attitudes towards pregnancy planning (four items)
Based on the HBM (Champion and Skinner, 2008), we developed four questions as five-step ranking scales with a neutral centre aiming to explore the woman's attitude to pregnancy planning.
Follow-up
The structured telephone interview included the same questions used at baseline, but background questions were not repeated in the IG and CG1. The IG answered seven additional questions aiming to evaluate their experience of the intervention. The questions that evaluated the intervention were designed as five-step ranking scales with a neutral centre. The questions covered: if the woman had previously thought about the topics included in the intervention (‘a lot’ to ‘not at all’), if any of the information was new to her (‘a lot’ to ‘not at all’), the overall impression of being asked about the RLP (‘very positive’ to ‘very negative’), if the intervention made her think about reproduction in a different way (‘very much’ to ‘very little’), if the intervention had made her search for more information about reproduction (‘a lot’ to ‘not at all’), the likelihood of turning to a midwife if she had further questions about reproduction (‘very likely’ to ‘very unlikely’) and finally, if midwives and/or other health-care professionals routinely should discuss RLP with their patients (yes, both midwives and other health-care professionals/yes, but only midwives/yes, but only other health-care professionals/no/don't know).
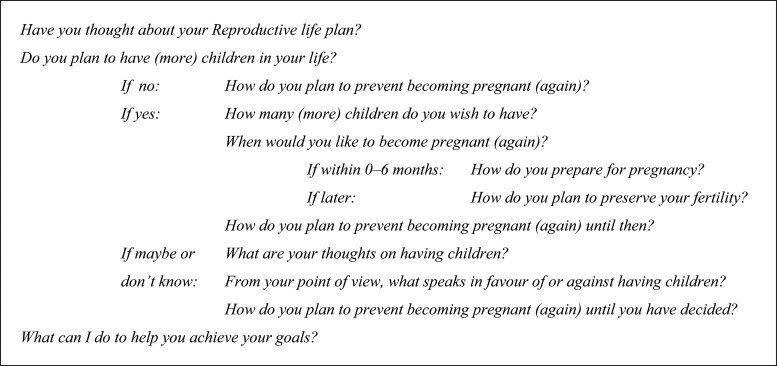
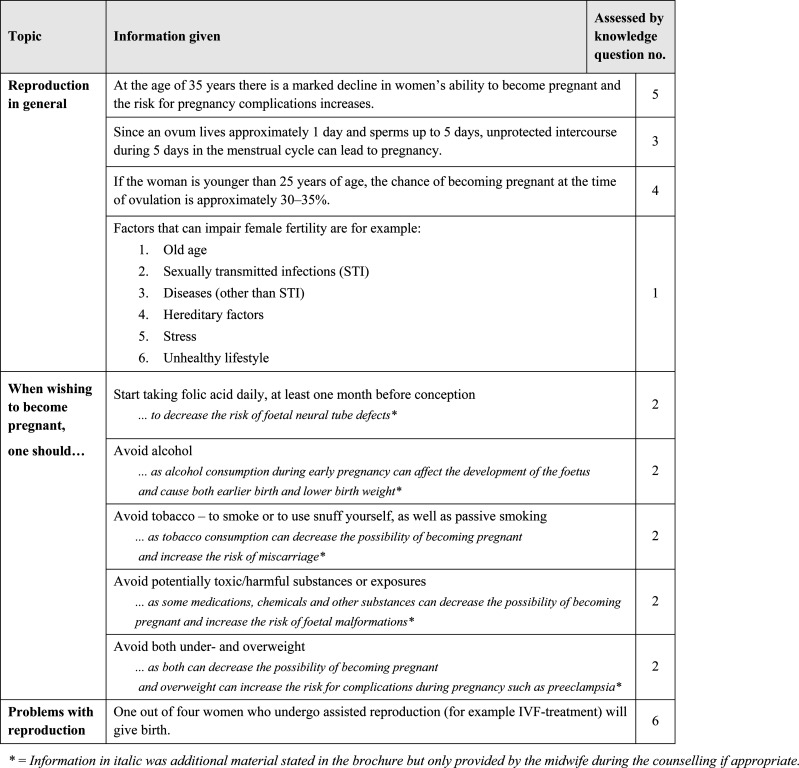
Intervention: RLP-based information
In addition to the standard care given to all women, the IG participated in a semi-structured discussion aimed to encourage the woman to reflect on her own RLP. The midwife then provided targeted information based on the woman's reproductive intentions. For guidance, the midwife used an RLP-based interview guide, as described by Moos (2003), as shown in Fig. 2, and the specific information as listed in Fig. 3. All women received the same information, but delivered in an individualized way depending on the woman's answers. For women who did not wish to have children emphasis was placed on how to avoid an unplanned pregnancy and preserve fertility. For women who intended to become pregnant in the future, emphasis was placed on information on how to preserve their fertility and what to do when they wished to become pregnant. All women were informed to start taking folic acid on the same day they discontinued their regular contraceptive method. It took ∼5–15 min to relate the RLP-based information to women. All women in the IG also received a specially designed brochure to take home. The brochure was inspired by RLP leaflets used in the USA and adapted to the Swedish context, and included both information about the RLP and the information about reproduction shown in Fig. 3.
Figure 2.
RLP-based interview guide used by the midwives during the intervention.
Figure 3.
Information given to the intervention group, both verbally by the midwives during the counselling and in written form in the brochure.
Data analysis
Data were entered and analysed using the Statistical Package for the Social Sciences (SPSS) (version 20, IBM, Armonk, NY, USA) and SAS (version 9.3, SAS Institute, Cary, NC, USA). The IG and CG1 were compared regarding background variables (age, level of university education, immigrant background, relationship status) and reproductive history (history of STI, pregnancy, abortion, miscarriage, childbirth) with independent t-test for continuous variables, Mann–Whitney U-test for ordinal variables and Pearson's χ2 test for categorical variables. Non-responders at follow-up were compared with responders using the same procedure.
In order to obtain the main outcome variable, knowledge questions were computed to form a knowledge score. The answers to the two open-ended questions could sum up to a maximum of six points each (1 point for at least one correct answer in each category) according to the intervention-specific information (Fig. 3). For the additional four questions, each entirely correct answer received two points and almost correct answers were given one point. The total score could thus range between 0 and 20. Since this score was not normally distributed, it was analysed using non-parametric methods. Correlations between the total score and background variables (age, level of education, immigrant background) and reproductive history (history of STI, relationship status, desire for having children, history of pregnancy) were analysed using Spearman's correlation coefficient. Differences in the knowledge score between groups at baseline and follow-up were analysed with Mann–Whitney U-test. Differences between baseline and follow-up within groups were analysed with Wilcoxon signed ranks test. To adjust for baseline differences between the groups a multiple linear regression analysis was conducted, using the total knowledge score as the dependent variable and baseline knowledge score and group assignment as independent variables. The relationship between knowledge of folic acid (mentioned folic acid/did not mention folic acid) and group assignment at baseline and at follow-up was analysed with Pearson's χ2 test.
Differences between groups in the secondary outcome variables (desire of having children, preferred age for having children and confidence of having the desired number of children) were analysed with Mann–Whitney U-test. Differences between baseline and follow-up within groups were analysed with Wilcoxon signed ranks test. All statistical tests were two-sided with P < 0.05 considered statistically significant.
Results
Characteristics of the women are shown in Table I. There were no differences in the studied characteristics between groups.
Table I.
Characteristics of the women in the intervention group (IG), Control group 1 (CG1) and Control group 2 (CG2) in the RCT to study the benefit of using RLP-based information in contraceptive counselling.
| IG (n = 101) (%) | CG1 (n = 100) (%) | CG2 (n = 88) (%) | P-value* | |
|---|---|---|---|---|
| Age | ||||
| Years; mean ± SD | 23 ± 2.4 | 23 ± 2.2 | 24 ± 2.8 | 0.290a |
| Level of university education | ||||
| 0–3 years/studies for bachelor's degree | 73 | 63 | 64 | 0.172b |
| 4–5 years/studies for master's degree | 21 | 35 | 32 | |
| 6–10 years/studies for doctoral degree | 4 | 0 | 2 | |
| Immigrant background | ||||
| Born outside of Sweden | 7 | 7 | 5 | 0.558c |
| One or two parents born outside of Sweden | 14 | 19 | 9 | 0.597c |
| Relationship status | ||||
| Single | 42 | 45 | 39 | 0.625c |
| Stable relationship | 58 | 55 | 61 | |
| Reproductive history | ||||
| Contraceptive method(s) used at last intercourse | ||||
| None | 6 | 7 | 5 | |
| Fertility awareness-based method/interrupted intercourse | 5 | 8 | 1 | |
| Condom | 27 | 26 | 22 | |
| Birth control pill/patch/injection etc. | 66 | 71 | 77 | |
| Intrauterine device | 3 | 2 | 5 | |
| History of STI | 17 | 26 | 19 | 0.113c |
| Tried to become pregnant | 0 | 0 | 6 | — |
| History of pregnancy | 4 | 3 | 14 | 0.731c |
| History of abortion | 3 | 3 | 9 | — |
| History of miscarriage | 1 | 0 | 0 | — |
| History of childbirth | 0 | 0 | 5 | — |
aIndependent t-test
bMann–Whitney test
cPearson's χ2 test.
*P-value from comparison between IG and CG1.
Knowledge of reproduction
An overview of the knowledge questions and distributions of answers is shown in Tables II and III. At baseline (IG and CG1), the women stated that an ovum is fecund in mean (M), 3.7 days, [median (Md) 3.0, range 0.5–30.0]. The chance that a young woman will become pregnant after having unprotected intercourse at the time of ovulation was estimated as 51% (Md 50, range 2–100). The mean age at which there is a marked decrease in women's ability to become pregnant was estimated to 33 years (Md 30, range 18–60). The chance of having a child with one treatment of IVF was estimated to be 32% (Md 25, range 1–99).
Table II.
Distribution of answers to knowledge questions 1–2 in the IG, CG1 and CG2 at baseline and follow-up at 2 months.
| Knowledge questions 1–2 | Score (no. of points) | IG |
CG1 |
CG2 | |||
|---|---|---|---|---|---|---|---|
| Baseline (n = 101) | Follow-up (n = 89) | Baseline (n = 100) | Follow-up (n = 85) | Follow-up (n = 88) | |||
| 1. Mention as many factors as possible that can impair female fertilitya | 0–6p | Mean | 2.6 | 2.6 | 2.4 | 2.6 | 2.4 |
| Median | 3 | 3 | 2 | 3 | 2 | ||
| Range | 0–5 | 0–5 | 0–5 | 0–5 | 0–5 | ||
| 2. Mention as many changes in lifestyle as possible that a woman can do when planning to become pregnant to increase her chances of a healthy pregnancy and healthy childb | 0–6p | Mean | 1.9 | 2.9 | 1.9 | 2.3 | 2.2 |
| Median | 2 | 2.5 | 2 | 2.5 | 2.5 | ||
| Range | 0–4 | 0.5–5.5 | 0–4 | 0–4.5 | 0–4.5 | ||
aCorrect answers [1point (p) for each category]: high age; STIs; diseases (other than STI); hereditary factors; stress; unhealthy lifestyle (smoking, alcohol, drugs).
bCorrect answers (1p each category): folic acid intake; avoidance of alcohol and tobacco; avoidance of under- or overweight; avoidance of potentially toxic/harmful substances.
Table III.
Distribution of answers to knowledge questions 3–6 in the IG, CG1 and CG2 at baseline and follow-up.
| Knowledge questions 3–6 | Categories | Score (no. of points) | IG |
CG1 |
CG2 | ||
|---|---|---|---|---|---|---|---|
| Baseline (n = 101) (%) | Follow-up (n = 89) (%) | Baseline (n = 100) (%) | Follow-up (n = 85) (%) | Follow-up (n = 88) (%) | |||
| 3. How long does an ovum live?a | <1 day | 0p | 0 | 0 | 1 | 0 | 0 |
| 1 day | 2p | 16 | 25 | 12 | 8 | 9 | |
| >1 day | 0p | 71 | 63 | 78 | 85 | 81 | |
| 4. How likely is it that a 25-year old woman becomes pregnant if she has unprotected intercourse with a young man at the time of ovulation?a | <25% | 0p | 12 | 9 | 16 | 8 | 8 |
| 25–29% | 1p | 10 | 11 | 6 | 9 | 4 | |
| 30–35% | 2p | 7 | 36 | 8 | 9 | 3 | |
| 36–40% | 1p | 6 | 1 | 5 | 4 | 4 | |
| >40% | 0p | 56 | 32 | 56 | 55 | 68 | |
| 5. At what age is there a marked decline in women's ability to become pregnant?a | <30 years | 0p | 22 | 20 | 22 | 19 | 21 |
| 30–34 years | 1p | 42 | 21 | 38 | 33 | 36 | |
| 35 years | 2p | 15 | 42 | 18 | 20 | 18 | |
| 36–40 years | 1p | 12 | 4 | 15 | 7 | 12 | |
| >40 years | 0p | 8 | 2 | 6 | 6 | 2 | |
| 6. What is the chance of giving birth to a child conceived through IVF?a | <20% | 0p | 18 | 26 | 22 | 27 | 15 |
| 20–24% | 1p | 21 | 26 | 11 | 9 | 13 | |
| 25% | 2p | 12 | 13 | 11 | 10 | 6 | |
| 26–30% | 1p | 8 | 13 | 13 | 6 | 11 | |
| >30% | 0p | 30 | 11 | 38 | 33 | 44 | |
aCorrect answers: marked in bold.
The total knowledge score is presented in Table IV, and was for IG and CG1 at baseline in average 6.2 out of maximum 20 points (Md 6.0, range 0.0–14.0). The total score at baseline correlated with age (P = 0.002, rs = 0.18), level of education (P = 0.007, rs = 0.16) and desire for having children (P = 0.028, rs = −0.13); those older and with a higher level of education and desire for children scored higher than those who were younger, had a lower level of education and/or had no desire to have children. The total score at baseline was not correlated to immigrant background (P = 0.569, rs = 0.03), relationship status (P = 0.644, rs = 0.03), history of pregnancy (P = 0.787, rs = −0.02) or history of STI (P = 0.970, rs = 0.00).
Table IV.
Total score for knowledge of reproduction in the IG, CG1 and CG2 at baseline and follow-up: questions 1–6.
| Total score for knowledge of reproduction | Score (no. of points) | IG |
CG1 |
CG2 | ||
|---|---|---|---|---|---|---|
| Baseline (n = 101) (%) | Follow-up (n = 89) (%) | Baseline (n = 100) (%) | Follow-up (n = 85) (%) | Follow-up (n = 88) (%) | ||
| Sum of points questions 1–2 | ||||||
| Mean ± SD | 0–12p | 4.4 ± 1.9 | 5.5 ± 1.6 | 4.2 ± 1.9 | 4.9 ± 1.7 | 4.6 ± 1.7 |
| Sum of points questions 3–6 | ||||||
| Mean ± SD | 0–8p | 2.0 ± 1.6 | 3.5 ± 1.9 | 1.9 ± 1.5 | 1.9 ± 1.5 | 1.7 ± 1.2 |
| Total score questions 1–6 | ||||||
| Mean ± SD | 0–20p | 6.4 ± 2.9 | 9.0 ± 2.8 | 6.1 ± 2.6 | 6.8 ± 2.5 | 6.3 ± 2.2 |
| 95% CI | 5.8–7.0 | 8.4–9.5 | 5.6–6.6 | 6.3–7.4 | 5.9–6.8 | |
| Adjusted mean | 8.9* | 6.8* | 6.4* | |||
CI, confidence intervals.
*Difference between IG and CG1 in the multiple regression analysis: P < 0.001; difference between IG and CG2: P < 0.001. Difference between CG1 and CG2: P = 0.114.
There was no difference between the groups at baseline (U = 4715, P = 0.416). The IG scored higher on the knowledge questions at follow-up than at baseline (Z = −6.301, P < 0.001) with a mean of 9.0 (Md 9.0, range 3.5–15.5). The women in the CG1 did not score differently at follow-up than at baseline (Z = −1.686, P = 0.092). There was a difference in the total score both between the IG and CG1 (U = 2147, P < 0.001), and between the IG and CG2 at follow-up (U = 1843, P < 0.001). No difference in the total score was found between CG1 and CG2 at follow-up (U = 3393, P = 0.291).
When taking the baseline variation into account in the multiple regression analysis, the mean total score was 8.9 in the IG; 6.8 in the CG1 and 6.4 in the CG2. The difference in the knowledge score between the IG and the two CGs was significant (P < 0.001), whereas no difference was shown between the two CGs (P = 0.114). In the adjusted model, the knowledge score at baseline and group assignment had a significant effect on the total knowledge score at follow-up.
Knowledge of folic acid
At baseline, 4% in the IG and 5% in the CG1 mentioned folic acid intake among things to do when planning to get pregnant. There was no difference between the groups (χ2 (2) = 0.25, P = 0.881) in this regard. At follow-up, 22% in the IG and 3% in the CG1 mentioned folic acid intake (χ2 (2) = 31.67, P < 0.001). In the CG2, 1 woman (1%) mentioned folic acid intake.
Family planning intentions
The results for family planning intentions are shown in Table V. There was no difference between the IG and CG1 at baseline regarding the wish to have children (U = 4608, P = 0.371). A higher proportion in both IG and CG1 wanted children at follow-up than at baseline, and fewer were unsure or unwilling to have children (Z = −2.428, P = 0.015; Z = −2.066, P = 0.039). Similar increases in confidence from baseline to follow-up were observed for both the IG and for CG1. As shown in Table VI, a higher proportion in the IG stated it to be likely that they would make lifestyle changes prior to pregnancy after the intervention (P = 0.028) but no difference over time was found in the CG1.
Table V.
Family planning in the IG, CG1 and CG2 at baseline and follow-up.
| IG |
CG1 |
CG2 | |||
|---|---|---|---|---|---|
| Baseline (n = 101) (%) | Follow-up (n = 89) (%) | Baseline (n = 100) (%) | Follow-up (n = 85) (%) | Follow-up (n = 88) (%) | |
| Do you plan to have (more) children in your life?* | |||||
| Do not want (more) children | 8 | 3 | 9 | 4 | 5 |
| Do not know/unsure | 8 | 2 | 12 | 9 | 3 |
| Want (more) children | 82 | 94 | 77 | 87 | 92 |
| If you want (more) children … | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Desired number of children | 2.5 (±0.6) | 2.5 (±0.6) | 2.4 (±0.6) | 2.4 (±0.5) | 2.5 (±0.7) |
| Preferred age at first child (years) | 29 (±2.2) | 29 (±2.1) | 29 (±1.7) | 29 (±1.8) | 29 (±1.6) |
| Years until preferred age at first child | 5.5 (±2.2) | 5.4 (±2.1) | 5.9 (±2.1) | 5.9 (±1.9) | 5.5 (±2.0) |
| Preferred age at last child (years) | 35 (±2.9) | 34 (±2.7)a | 34 (±2.7) | 34 (±2.6) | 35 (±3.5) |
| Confidence in having the desired no. of children (0 = not confident at all; 10 = totally confident) | 5.2 (±2.4) | 5.9 (±2.0)a | 5.3 (±2.5) | 5.9 (±2.1)a | 5.5 (±2.0) |
*Difference within IG over time, analysed with Wilcoxon signed ranks test: P < 0.05; difference within CG over time, analysed with Wilcoxon signed ranks test: P < 0.05.
aDifferences within groups over time, analysed with Wilcoxon signed ranks test: P < 0.05
Table VI.
Attitudes towards pregnancy planning from an HBM perspective in the IG, CG1 and CG2 at baseline and follow-up.
| Item | Response alternatives | IG |
CG1 |
CG2 | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline (n = 101) (%) | Follow-up (n = 89) (%) | P-valuea | Baseline (n = 100) (%) | Follow-up (n = 85) (%) | P-valuea | Follow-up (n = 88) (%) | ||
| Perceived susceptibility | ||||||||
| How likely is it that you would ever experience an unplanned pregnancy? | 0.021 | 0.001 | ||||||
| Very/quite likely | 13 | 5 | 6 | 1 | 11 | |||
| Neither likely nor unlikely | 31 | 24 | 32 | 20 | 17 | |||
| Very/Quite unlikely | 56 | 72 | 62 | 79 | 72 | |||
| Perceived severity of consequences | ||||||||
| How important is it to you to get pregnant at the time you have planned? | 0.181 | 0.800 | ||||||
| Very/quite important | 57 | 64 | 66 | 64 | 65 | |||
| Neither important nor unimportant | 30 | 24 | 17 | 21 | 19 | |||
| Totally/quite unimportant | 8 | 9 | 13 | 12 | 11 | |||
| Wish never to become pregnant | 5 | 3 | 4 | 4 | 3 | |||
| Pregnancy planning as cue to action | ||||||||
| Imagine that you would like to become pregnant within 6 months. How likely is it that you would make any lifestyle changes? | 0.028 | 0.556 | ||||||
| Very/quite likely | 78 | 85 | 71 | 79 | 75 | |||
| Neither likely nor unlikely | 9 | 7 | 15 | 12 | 9 | |||
| Very/quite unlikely | 13 | 8 | 14 | 9 | 14 | |||
| Perceived self-efficacy | ||||||||
| Do you feel that you can influence if and when you become pregnant? | 0.806 | 0.106 | ||||||
| Very/quite much | 75 | 83 | 86 | 84 | 81 | |||
| Neither much nor little | 18 | 9 | 11 | 14 | 15 | |||
| Very/quite little | 7 | 8 | 3 | 2 | 5 | |||
HBM, health belief model.
aP-value for difference between baseline and follow-up, analysed with Wilcoxon signed ranks test.
Experience of the intervention
Of the 89 women in the IG who participated in the follow-up, 90% rated the midwife's initiative to discuss the RLP as very or rather positive, 45% had previously reflected on the questions covered in the discussion and brochure and 82% estimated it to be very or rather likely that they would approach a midwife if they had more questions about reproduction. The intervention was regarded by 56% to have made them think about reproduction in a different way and 54% stated that some or a substantial part of the information was new to them. That midwives routinely should discuss RLP with their patients was stated by 90%.
Non-responders
Of those enrolled in the study, a total of 37 women (12%)—evenly distributed between the three groups—were lost to follow-up. There was no difference between responders and non-responders in the CG1 and the IG regarding age (P = 0.542), level of education (P = 0.482), immigrant background (P = 0.396), relationship status (P = 0.124), history of STI (P = 0.370), history of pregnancy (P = 0.293) or wish to have children in the future (P = 0.085). There was a difference in the total knowledge score between responders (6.3) and non-responders (4.4) in the CG1 (P = 0.007) but not in the IG (6.5 versus 5.3, P = 0.132).
Discussion
In this study we evaluated the effect of RLP-based information among female university students in a student health-care setting, with particular focus on knowledge of reproduction. Our study showed that with only a small period of time, ∼10 min, we succeeded in increasing both knowledge of reproduction in general and knowledge of folic acid intake. Our intervention influenced women to plan for their last child earlier in life. This is very promising, as previous studies have indicated a need for education about age and fertility (Bretherick et al., 2010; Rovei et al., 2010; Virtala et al., 2011; Hashiloni-Dolev et al., 2011; Daniluk and Koert, 2012; Peterson et al., 2012). The midwives explicitly told the women in the IG to take folic acid pills when they discontinued hormonal contraceptive pills. The advice of taking a new kind of pill instead of a contraceptive pill might be easy to remember and can explain the increased knowledge.
Increased knowledge about reproduction may enable women to make informed choices about their RLP easier, avoiding unwanted pregnancies, preserving fertility and enhancing preconception health. It is therefore important to increase accessibility to information and health education about reproduction. Although significantly higher than the control group, the knowledge of reproduction was still not particularly high after the intervention. We used the RLP-based question ‘do you plan to have (more) children in your life?’ as a starting point for our intervention. However, as the information about reproduction was initiated by the midwives and not requested by the women in the IG this might be one explanation for the limited effect on their knowledge. This may also be due to the fact that the women were young and many did not plan to start a family for several years. The intervention might have given even better results in a motivated population, with women who are planning to become pregnant soon. Regardless of this, it is important to target all women of reproductive age, since many pregnancies are unplanned.
In line with earlier studies (Skoog Svanberg et al., 2006; Tydén et al., 2006), women had planned to delay childbearing until an age when reproductive capacity decreases and age-related complications increase. It is therefore encouraging that the intervention made the women plan for their last child earlier in life. We believe that the intervention may empower women and, for example, help them to understand what aspects of reproduction they are able to control, such as lifestyle habits, and what aspects they cannot control, for example declining fertility with advancing age. The intervention increased their self-efficacy in taking health-promoting actions for their reproductive health. After the intervention the women were more confident to have the desired number of children, stated to a higher degree that it was unlikely that they would ever experience an unplanned pregnancy and responded to higher degree that it was likely that they would make lifestyle changes in connection with pregnancy planning. Conclusions about the increase in confidence need to be drawn with caution, as an increase was also seen in CG1. Responding to questions about the RLP may have stimulated reflection on their own plans and thereby increased their confidence, regardless of whether the questions were posed in a questionnaire or by health-care personnel. The increase might also reflect the difference in measurement: in writing, as a VAS, at baseline and verbally at follow-up. As a higher proportion of women in the IG stated that they wanted children after the intervention, it is possible that lack of desire to have children is related to low knowledge of reproduction. But as the difference was seen also in the CG1 it is likely that many women had not fully reflected on these questions earlier, and only by being asked about their RLP did they realize that they actually wanted to have children sometime in the future.
Our follow-up time was short (at 2 months) and it was therefore not possible to study the intervention's possible effect on behaviour, such as increased incidence of health-promoting behaviour prior to pregnancy. Still, according to HBM, changing modifying factors and targeting individual beliefs are the first steps to change individual behaviours. The intervention aimed not only to increase the knowledge of reproduction, but also to influence the women's perception of their susceptibility to and severity of the consequences of an unplanned pregnancy, the perceived benefits of lifestyle changes in connection to pregnancy planning and to increase their self-efficacy. Pregnancy planning was intended to be perceived as a cue to action for health-promoting lifestyle changes. By targeting these aspects, young women would become better equipped to make informed choices about their sexual and reproductive health. The use of the HBM to understand contraceptive behaviour has recently been reviewed by Hall (2012), who concluded that the HBM can be used as a framework to predict and explain contraceptive behaviour and to promote strategies to improve family planning outcomes. The HBM is also applicable for understanding preconception health and was used in a recent study about folate intake to demonstrate mechanisms influencing behavioural changes in women who are planning a pregnancy (Jensen et al., 2012).
Another important finding was that the majority of women appreciated the intervention and considered that midwives routinely should discuss RLP with their patients. Since the majority of our participants visited the clinic for contraceptive counselling we suggest that guidelines for contraceptive counselling should include RLP-based questions. Our results show that health-care personnel should not hesitate to pose personal questions about reproductive health, even if they feel those questions are sensitive. This correlates well with a previous study, in which it was found that young women consider it natural to be asked questions about sexual health during gynaecological encounters (Wendt et al., 2011), and they express great trust towards midwives and doctors. The women feel that questions about their situation open a dialogue and help clarify their situation (Wendt et al., 2007). Still, it must be emphasized that it is always important when discussing questions such as these, to adapt the information to the individual, to use a non-normative approach and respect the informant's autonomy. If health professionals feel unable to give RLP-based information due to time constraints, we suggest using specially designed leaflets and/or recommending reliable websites. We believe that national evidence-based guidelines for preconception care would be an important step towards promoting reproductive health and, as such, useful for both the public and for health care personnel.
The study was conducted by dedicated midwives at a small clinic. It is possible that if implemented routinely, the RLP-based information would be less standardized, and more adapted to the individual patient, which could have both advantages and disadvantages. It is also possible that the effect of the intervention was connected to the women's high level of education. Women with a university education might more easily benefit from such an intervention than women with a lower level of education, and conclusions for the general population should therefore be drawn with caution. Still, consistent with earlier research among university students in different settings (Bretherick et al., 2010; Rovei et al., 2010; Hashiloni-Dolev et al., 2011; Virtala et al., 2011; Peterson et al., 2012), these highly educated women had low levels of knowledge of reproduction at baseline. It is likely that women with a lower level of education might have more limited knowledge and therefore could benefit even more from a similar intervention.
This is the first study to evaluate the use of an RLP in clinical practice in a systematic way. By using a randomized controlled design with two control groups we are confident that our results demonstrate the effect of the RLP intervention and that they are not biased by group selection. This study presents a feasible way of introducing the concept of preconception care in the Swedish health system, where preconception has not yet been included. The intervention was conducted with a limited amount of time and resources and is easy to adapt to the current standard care. Given the moderate knowledge of reproduction at baseline, there seems to be a need for increased health education to women of reproductive age. The RLP should be considered as a useful tool for reproductive health promotion and can be used by all health-care professionals working with issues related to reproductive health, for example at youth clinics, family planning services, genitourinary medicine clinics and by general practitioners. The next step in our research will be to implement RLP in routine contraceptive counselling. The counsellors will play a key role in successful implementation and it is therefore important to capture their perceptions of this novel approach to contraceptive counselling. Further studies will be needed on how to target men and also to investigate the effect on health behaviour.
Conclusions
Our study showed that the RLP-based information increased women's knowledge both of reproduction and of folic acid intake prior to pregnancy, affected the women's RLP and was appreciated by the women. Midwife-initiated use of RLP-based information therefore seems to be a feasible tool for promoting reproductive health.
Authors' roles
J.S., M.L. and T.T. planned and designed the study and contributed to the acquisition of data. J.S. analysed the data and provided a draft manuscript. P.K. made additional statistical analyses. All authors were involved in revising the manuscript and approved the final version.
Funding
Grants were received from the Faculty of Medicine, Uppsala University, Sweden (46 500 EUR). Funding to pay the Open Access publication charges for this article was provided by the Faculty of Medicine, Uppsala University, Sweden.
Conflict of interest
None declared.
Acknowledgements
We are grateful to Hannah Johansson and Anna Ekenberg Abreu at the Student Health Centre and to research assistants Maria Olovsson and Sarah Söderström who assisted in data collection. We would also like to thank all the participating women.
Reference
- Agency for School Improvement. 2005. Hela livet: 50 år med sex- och samlevnadsundervisning http://www.skolverket.se/polopoly_fs/1.95608!Menu/article/attachment/hela%2520livet.pdf. 3 January 2013, date last accessed.
- Andersson G, Rønsen M, Knudsen LB, Lappegård T, Neyer G, Skrede K, Teschner K, Vikat A. Cohort fertility patterns in the Nordic countries. Demogr Res. 2009;20:313–352. [Google Scholar]
- Barry M. Preconception care at the edges of the reproductive lifespan. Nurs Women's Health. 2011;15:68–74. doi: 10.1111/j.1751-486X.2011.01613.x. [DOI] [PubMed] [Google Scholar]
- Bretherick K, Fairbrother N, Avila L, Harbord S, Robinson W. Fertility and aging: do reproductive-age Canadian women know what they need to know? Fertil Steril. 2010;93:2162–2168. doi: 10.1016/j.fertnstert.2009.01.064. [DOI] [PubMed] [Google Scholar]
- Brown W, Ottney A, Nguyen S. Breaking the barrier: the health belief model and patient perceptions regarding contraception. Contraception. 2011;83:453–458. doi: 10.1016/j.contraception.2010.09.010. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Recommendations to improve preconception health and health care—United States: a report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR. 2006;55:1–23. [PubMed] [Google Scholar]
- Champion V, Skinner C. The health belief model. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education—Theory, Research, and Practice. 4th edn. San Fransisco, US: Jossey-Bass; 2008. pp. 45–66. [Google Scholar]
- Daniluk JC, Koert E. Childless Canadian men's and women's childbearing intentions, attitudes towards and willingness to use assisted human reproduction. Hum Reprod. 2012;27:2405–2412. doi: 10.1093/humrep/des190. [DOI] [PubMed] [Google Scholar]
- Dunlop A, Logue K, Miranda M, Narayan D. Integrating reproductive planning with primary health care: An exploration among low-income, minority women and men. Sex Reprod Healthc. 2010;1:37–43. doi: 10.1016/j.srhc.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Ekstrand M, Tydén T, Larsson M. Exposing oneself and one's partner to seuxal risk-taking as perceived by young Swedish men who requested a Chlamydia test. Eur J Contracept Reprod Health Care. 2011;16:100–1007. doi: 10.3109/13625187.2010.549253. [DOI] [PubMed] [Google Scholar]
- Eriksson C, Larsson M, Tydén T. Reflections on having children in the future – interviews with highly educated women and men without children. Ups J Med Sci. 2012;117:328–335. doi: 10.3109/03009734.2012.654862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottvall M, Tydén T, Höglund AT, Larsson M. Knowledge of human papillomavirus among high school students can be increased by an educational intervention. Int J STD AIDS. 2010;21:558–562. doi: 10.1258/ijsa.2010.010063. [DOI] [PubMed] [Google Scholar]
- Hall KS. The Health Belief Model can guide modern contraceptive behavior research and practice. J Midwifery Womens Heal. 2012;57:74–81. doi: 10.1111/j.1542-2011.2011.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashiloni-Dolev Y, Kaplan A, Shkedi-Rafid S. The fertility myth: Israeli students' knowledge regarding age-related fertility decline and late pregnancies in an era of assisted reproductive technology. Hum Reprod. 2011;26:3045–3053. doi: 10.1093/humrep/der304. [DOI] [PubMed] [Google Scholar]
- Jensen B, Lähteenmäki L, Grunert K, Brown K, Timotijevic L, Barnett J, Shepherd R, Raats M. Changing micronutrient intake through (voluntary) behaviour change. The case of folate. Appetite. 2012;68:1014–1022. doi: 10.1016/j.appet.2012.03.004. [DOI] [PubMed] [Google Scholar]
- Lampic C, Skoog Svanberg A, Karlström P, Tydén T. Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Hum Reprod. 2006;21:558–564. doi: 10.1093/humrep/dei367. [DOI] [PubMed] [Google Scholar]
- Malnory M, Johnson T. The Reproductive Life Plan as a Strategy to Decrease Poor Birth Outcomes. J Obstet Gynecol Neonatal Nurs. 2011;40:109–121. doi: 10.1111/j.1552-6909.2010.01203.x. [DOI] [PubMed] [Google Scholar]
- Medical Products Agency. Antikonception—behandlingsrekommendation. Information från Läkemedelsverket. 2005. 7 http://www.lakemedelsverket.se/upload/halso-och-sjukvard/behandlingsrekommendationer/Rek%20antikonception%20v3.pdf. 3 January 2013, date last accessed.
- Medical Research Council. Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. MRC Vitamin Study Research Group. Lancet. 1991;338:131–137. [PubMed] [Google Scholar]
- Moos MK. Unintended pregnancies—a call for nursing action. MCN Am J Matern child Nurs. 2003;28:24–30. [PubMed] [Google Scholar]
- Moos MK, Dunlop A, Jack B, Nelson L, Coonrad D, Long R, Boggess K, Gardiner P. Healthier Women, healthier reproductive outcomes: Recommendations for the routine care of all women of reproductive age. Am J Obset Gynecol. 2008;199:S280–S289. doi: 10.1016/j.ajog.2008.08.060. [DOI] [PubMed] [Google Scholar]
- Peterson BD, Pirritano M, Tucker L, Lampic C. Fertility awareness and parenting attitudes among American male and female undergraduate university students. Hum Reprod. 2012;27:1375–1382. doi: 10.1093/humrep/des011. [DOI] [PubMed] [Google Scholar]
- Rovei V, Gennarelli G, Lantieri T, Casano S, Revelli A, Massobrio M. Family planning, fertility awareness and knowledge about Italian legislation on assisted reproduction among Italian academic students. Reprod Biomed. 2010;20:873–879. doi: 10.1016/j.rbmo.2010.03.024. [DOI] [PubMed] [Google Scholar]
- Sanders L. Reproductive Life Plans: Initiating the Dialogue with Women. MCN Am J Matern Child Nurs. 2009;34:342–347. doi: 10.1097/01.NMC.0000363681.97443.c4. [DOI] [PubMed] [Google Scholar]
- Skoog Svanberg A, Lampic C, Karlström P-O, Tydén T. Attitudes toward parenthood and awareness of fertility among postgraduate students in Sweden. Gend Med. 2006;3:187–195. doi: 10.1016/s1550-8579(06)80207-x. [DOI] [PubMed] [Google Scholar]
- Statistics Sweden. Childbearing trends of different generations. 2011. Demographic Reports 3 http://www.scb.se/statistik/_publikationer/BE0701_2011A01_BR_BE51BR1103.pdf. 4 April 2013, date last accessed.
- The Finnish National Institute for Health and Welfare. Pohjoismaiset raskaudenkeskeytykset 2009—Aborter i Norden 2009—Induced abortions in the Nordic countries 2009 Statistikrapport 9/2011, 2011 http://www.thl.fi/tilastoliite/tilastoraportit/2011/Tr09_11.pdf. 3 January 2013, date last accessed.
- The Ministry of Health and Social Affairs. The working group on prevention of unwanted pregnancies (S 2007:D). Bättre förutsättningar för det förebyggande arbetet—idépromemoria från Socialdepartementets arbetsgrupp för förebyggande av oönskade graviditeter. S 2008/3709/HS. 2009-06-15 http://www.regeringen.se/content/1/c6/12/83/30/018247a0.pdf. 3 January 2013, date last accessed.
- The National Board of Health and Welfare. Att förebygga oönskade graviditeter: kartläggning, beskrivning och analys av verksamheters arbete med unga och unga vuxna. 2008-131-26 http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/8853/2008-131-26_200813126.pdf. 11 December 2012, date last accessed.
- The National Board of Health and Welfare. The Swedish Health Care Report 2009-9-18 http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/17742/2009-9-18.pdf. 3 January 2013, date last accessed.
- The National Board of Health and Welfare. 2012a. Official Statistics of Sweden. Induced abortions 2011 http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18877/2012-11-6.pdf. 3 January 2013, date last accessed.
- The National Board of Health and Welfare. Official Statistics of Sweden. Pregnancies, deliveries and newborn infants: the Swedish Medical Birth Register 1973-2010. 2012b. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18669/2012-4-2.pdf. 3 January 2013, date last accessed.
- The National Food Agency. 2010. Kunskaper om folsyra http://www.slv.se/upload/dokument/nyheter/2010/opinionsundersokning_folsyra_jan_2010.pdf. 3 January 2013, date last accessed.
- The National Food Agency. 2013. Take folic acid before you get pregnant/Ät folsyra innan du blir gravid http://www.slv.se/en-gb/Folic-acid/ 3 January 2013, date last accessed.
- The Swedish National Agency for Education. Stockholm: Liber; 2000. Nationella kvalitetsgranskningar 1999: Skolverkets Rapport Nr 180. Dnr 99:208. ISSN 1103-2421 http://www.skolverket.se/2F%2Fwww5.skolverket.se%2Fwtpub%2Fws%2Fskolbok%2Fwpubext%2Ftrycksak%2FRecord%3Fk%3D605. 3 January 2013, date last accessed. [Google Scholar]
- The Swedish National Agency for Education. 2011. Sexualitet, genus och relationer i grundskolans styrdokument http://www.skolverket.se/polopoly_fs/1.162740!/Menu/article/attachment/Sex_och_samlevnad_grundskolans_styrdokument_2.pdf. 3 January 2013, date last accessed.
- Tydén T, Skoog Svanberg A, Karlström P-O, Lihoff L, Lampic C. Female university students' attitudes to future motherhood and their understanding about fertility. Eur J Contracept Reprod Health Care. 2006;11:181–189. doi: 10.1080/13625180600557803. [DOI] [PubMed] [Google Scholar]
- Tydén T, Stern J, Nydahl M, Berglund A, Larsson M, Rosenblad A, Aarts C. Pregnancy planning in Sweden—a pilot study among 270 women attending antenatal clinics. Acta Obstet Gynecol Scand. 2011;90:408–412. doi: 10.1111/j.1600-0412.2010.01055.x. [DOI] [PubMed] [Google Scholar]
- Virtala A, Vilska S, Huttunen T, Kunttu K. Childbearing, the desire to have children, and awareness about the impact of age on female fertility among Finnish university students. Eur J Contracept Reprod Health Care. 2011;16:108–115. doi: 10.3109/13625187.2011.553295. [DOI] [PubMed] [Google Scholar]
- Wendt E, Hildingh C, Lidell E, Westerståhl A, Baigi A, Marklund B. Young women's sexual health and their views on dialogue with health professionals. Acta Obstet Gynecol Scand. 2007;86:590–595. doi: 10.1080/00016340701214035. [DOI] [PubMed] [Google Scholar]
- Wendt E, Lidell E, Westersåhl A, Marklund B, Hidingh C. Young women's perception of being asked questions about sexuality and sexual abuse—a content analysis. Midwifery. 2011;27:250–256. doi: 10.1016/j.midw.2009.06.008. [DOI] [PubMed] [Google Scholar]