Abstract
Orthopaedic surgery requires a high degree of technical skill. Current orthopaedic surgical education is based largely on an apprenticeship model. In addition to mounting evidence of the value of simulation, recent mandated requirements will undoubtedly lead to increased emphasis on surgical skills and simulation training. The University of Iowa’s Department of Orthopaedic Surgery has created and implemented a month long surgical skills training program for PGY-1 residents. The goal of the program was to improve the basic surgical skills of six PGY-1 orthopaedic surgery residents and prepare them for future operative experiences. A modular curriculum was created by members of the orthopaedic faculty which encompassed basic skills felt to be important to the general orthopaedic surgeon. For each module multiple assessment techniques were utilized to provide constructive critique, identify errors and enhance the performance intensity of trainees. Based on feedback and debriefing surveys, the resident trainees were unanimously satisfied with the content of the surgical skills month, and felt it should remain a permanent part of our educational program. This manuscript will describe the development of the curriculum, the execution of the actual skills sessions and analysis of feedback from the residents and share valuable lessons learned and insights for future skills programs.
Background
Acquiring procedural skills is a critically important area in surgical residency training. Currently, the progress of orthopaedic residents in acquiring surgical skills is assessed through faculty evaluations and case logs. Despite the imminent addition of trainee surgical skills assessment in the form of patient care milestones1, skills training predominantly occurs in a live operating room by virtue of an apprenticeship method.
There is growing momentum to incorporate structured surgical skill education, including surgical simulation, into surgical residency training4. Often cited reasons include resident work hours restricting surgical experience, an increased demand for surgical efficiency in the setting of busy academic faculty practice, an elevated concern for patient safety2, and the availability of better surgical simulations. Studies have shown that structured surgical skill programs which include surgical simulation, can be used to train, assess, and improve operative performance5.
The results of a recent survey indicate strong agreement amongst both orthopaedic residency program directors and residents that a surgical skills curriculum, skills training and simulation technology should be a component of an orthopaedic resident’s training. Orthopaedic resident educators cite the lack of a formalized curriculum as one of the most substantial barriers to wide spread adoption of surgical skills training4. The Residency Review Committee (RRC) for Orthopaedic Surgery, a review committee of the Accreditation Council for Graduate Medical Education (ACGME), and the American Board of Orthopaedic Surgery (ABOS), have for the first time mandated a laboratory- and curriculum- based training for orthopedic residents at the PGY-1 level. These new requirements will be in effect as of July 2013.
In anticipation of these new requirements, The University of Iowa orthopedic residency program received special consideration from the ABOS to develop and pilot a month-long laboratory based skills rotation aimed at teaching basic surgical skills to PGY-1 residents. This article will describe the experience of this month, from creation of the curriculum to execution of the actual skills sessions, while sharing lessons learned and the potential for future years.
Goals and Objectives
The overall goal of the surgical skills program was to improve the basic skills of PGY-1 residents in areas fundamental to the practice of orthopedic surgery and to prepare them for actual operating room experiences.
This goal was achieved by a) designing a modular curriculum, b) incorporating background cognitive knowledge, c) allowing protected time for practice of basic skills, d) providing expert instruction, and e) incorporating assessment metrics with pre and post testing. The comprehensive curriculum was designed specifically for a single month where all six PGY-1s were together and free of other clinical responsibilities.
Overview of Format
The curriculum was designed to be a series of skills modules that followed a logical and sequential progression of difficulty level. Phase 1 of the American College of Surgeons and the Association of Program Directors in Surgery (ACS/APDS) basic surgical skills program template, which consists of an online syllabus and video tutorials, was incorporated into several modules, and served as a guideline for the curriculum design6. The template that was used (Table 1) for each individual module was based on the ACS/APDS template and was similar to a template accepted by an ABOS skills task- force to develop a national orthopedic PGY-1 curriculum
Table 1.
Template format for individual modules
| I. | Objectives |
| II. | Assumptions |
| III. | Background Info and Knowledge |
| IV. | Suggested Reading |
| V. | Description of Laboratory Module |
| VI. | Description of Techniques and Procedure(s) |
| VII. | Common Errors and Prevention Stratagies |
| VIII. | Expert Performance and Video |
| IX. | Recommendations for Practice |
| X. | Supplies and Station Setup |
| XI. | Assessment Metric |
| XII. | Estimated Costs |
| XIII. | Suggested Time Length |
The development of the curriculum and its individual modules required effort and engagement from multiple faculty members in various orthopaedic subspecialties. The central focus of the month-long course was surgical skill development. Carefully chosen supplementary didactic materials were provided as needed to support each surgical skill. The curriculum focused on those skills that were felt to be appropriate for entry level orthopaedic residents. The plan allotted time for dedicated practice of the specific surgical skills to promote retention of basic skills and improve subsequent operating room performance.
Repeated assessment of resident skills played an important role in the curriculum. Assessment started with basic tests of aptitude in spatial reasoning and dexterity that were administered at the beginning of the month.
A variety of assessment metrics and approaches were utilized throughout the month in the various modules, allowing learners to demonstrate improvement, while enhancing performance intensity.
Module Development
Once the department committed to a protected, month-long orthopaedic surgical skills rotation for PGY- 1s, a core group of contributing faculty were identified. At an initial meeting, approximately nine months prior to the surgical skills month, faculty began the process of selecting skills modules that were felt to be relevant to the entry-level orthopaedic surgery resident. As modules were selected and agreed upon by the group, individual or pairs of faculty with particular interests took ownership in the development of the content for individual modules. The module template provided a development plan. During this development period, some faculty chose to use existing media for instruction, while others chose to create new written and video content. In parallel with the development of module content, the anticipated required equipment and potential budgetary considerations were catalogued and incorporated into the planning process. Faculty engagement and interest in this process was high.
Modules
During the six months leading up to the designated month long rotation, consensus was obtained between the participating faculty members regarding the specific modules that would be included. The titles of the modules that were chosen are presented in Table 2.
Table 2.
Modules utilized in the 2013 PGY1 surgical skills curriculum at the University of Iowa
|
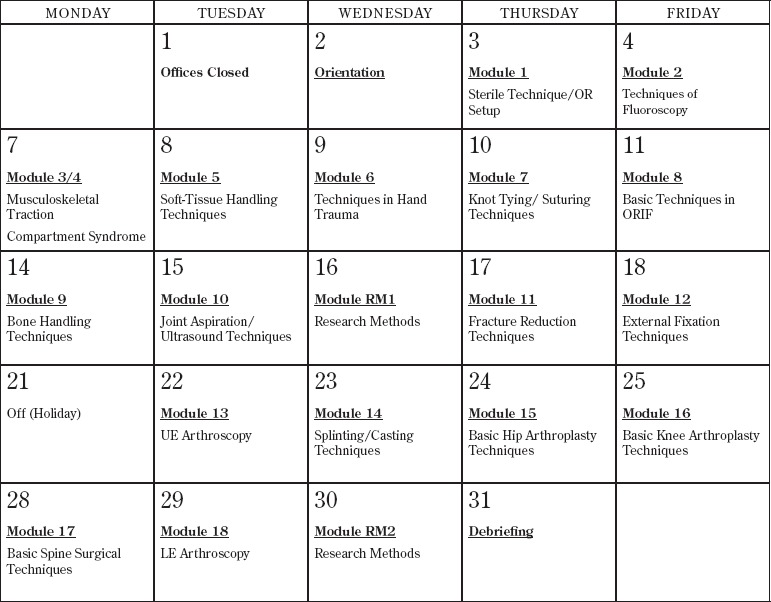
Within the constraints of a busy academic and clinical practice, individual dates were scheduled during the skills month for each module with some flexibility (to meet faculty needs) and to promote a sequential learning process. Days during the month were typically filled with one, and at most two, individual modules (Figure 1). The course syllabus and supporting background materials and reading (including video examples) were provided to the residents prior to the commencement of the month. The month began with an orientation on the objectives, goals, and context of the month. The final schedule was agreed upon three months prior to the skills month, and faculty members responsible for individual modules set aside time to participate and instruct residents on the day of their module (average three hours per day).
Figure 1. University of Iowa surgical skills month.
Description of a Representative Module – Basic Techniques in Open Reduction and Internal Fixation (ORIF)
Most modules occupied the residents for around six hours. Residents spent additional time reading or, when cadavers were available, performing dissections relevant to surgical approaches and anatomy. A detailed description of the entire curriculum is beyond the scope of this paper. Instead, the description of a single illustrative module (Module 8: Basic Techniques of Internal Fixation) is briefly presented here to convey the basic approach incorporated in each of the individual modules (Figure 2).
Figure 2. Description of the basic techniques in ORIF module.
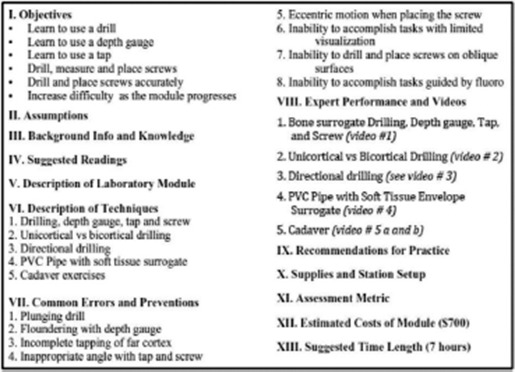
In this module, residents read background material and watched educational videos (Figure 2 VIII) that had been produced prior to beginning the day’s activities. Trainees were then individually assessed by an experienced surgeon as a reviewer using an Objective Structured Assessment of Technical Skill (OSATS) while they performed a fluoroscopy guided exposure, drill, tap, and screw placement on a cadaveric ankle. Video recordings with multiple cameras for instructional purposes were also captured. Residents then performed skills exercises on PVC pipe both with and without a foam covering. They practiced basic techniques of drilling, depth gauging and placing screws and achieved proficiency on each of these skills. In the afternoon, the residents had a final assessment while performing the same screw placement task (described above) on a different cadaver ankle, again recorded and assessed via an OSATS. The eight hour module was designed to run with limited faculty involvement other than assessments and periodic instruction.
Facilities
The majority of the skills sessions took place in the Joseph Buckwalter Surgical Skills Laboratory (Figure 3) within the orthopaedics department. This laboratory is 500 square feet in size, and it is equipped with multiple arthroscopy towers, deep freezers for cadaveric specimen storage, a radio-opaque and radiolucent table, sinks, and miscellaneous surgical instruments. Dedicated fluoroscopy was not available, and when utilized as part of a module, it had to be scheduled well in advance with hospital radiology. The PGY-1 residents spent one half day in a vacant operating room learning sterile technique, patient positioning, operating room table set up, and techniques of prepping and draping. Didactic portions of modules were held in the Arthur Steindler Orthopedic Library adjacent to the skills lab.
Figure 3. Faculty instruction in the Joseph Buckwalter Surgical Skills Laboratory.

Faculty/Staff Time Commitment
The coordination of planning and execution of the surgical skills month required dedicated faculty and support personnel time. The planning of the surgical skills month required five 45-minute meetings, at increasing frequency as the month approached. Each meeting was attended by 5-7 faculty members. While variable, individual faculty effort for module development required between 6-8 hours. This preparation time was greater for faculty choosing to create supporting media. On the day of their module faculty spent between one and four hours assisting and teaching during the module.
Support staff members were critical to the success of the month. One laboratory and one research assistant played an integral role in the preparation and execution of the month. They were tasked with assuring the required supplies and materials were available on each designated day. They worked closely with individual faculty members in the coordination of this effort. In addition, they were invaluable during the inevitable occasions of trouble-shooting. The laboratory assistant worked in the lab full time during the month, and the research assistant was involved with the project about one third time.
Materials Planned and Utilized
The provision of essential materials required careful planning. Each individual faculty member responsible for a specified module was tasked with providing a detailed and itemized checklist of desired equipment and materials. This equipment database required continuous modification with foresight as to the timing of modules and the most efficient use of materials and equipment. The most commonly requested items were cadaveric specimens, surrogate bone models (Sawbones Inc.), suture materials, surgical instruments, and C-arm fluoroscopy.
Research/Assessment Projects
Two research projects were incorporated into the skills month, laying the foundation for future refinement of intervention strategies aimed at improving skills acquisition. Through careful planning, grant funding from a variety of sources was obtained to support this research. [The research results will be reported later elsewhere.] The two specific modules that incorporated research objectives involved (1) the use of fluoroscopy to navigate guide wire placement and (2) articular fracture reduction through a limited incision. Prior to and after the use of alternative radiation-free simulations for basic skills training, a fluoroscopy guided bone surrogate simulation of a surgical procedure was accomplished in the skills lab for both modules.
The first research project focused on the fact that fluoroscopy guided wire navigation is fundamental to a number of orthopedic procedures. Directing and advancing the wire in the correct plane relies on both visual-spatial and psychomotor dexterity skills. In order to reduce radiation exposure in training, an augmented reality wire-navigation simulator was used, combining a real drill, wires, and surrogate bone models with virtually generated, radiation-free fluoroscopic images. During this simulation, trainees navigated a wire from the lateral femoral cortex, through the femoral neck, attempting placement within 5mm of the femoral head articular surface. The simulator promoted drilling dexterity, interpreting fluoroscopy images, and visual-spatial wire navigation skills.
The second research project used simulation of the surgical reduction of a three-fragment tibial plafond fracture that has previously been described3, 7 to compare the performance of the first-year orthopaedic residents before and after the use of a box skills trainer. This task simulator gives residents a 15 minute window to reduce and fix fracture fragments using a standard set of surgical tools and K-wires. The residents also made use of a fluoroscopy unit to help determine the current position of the fragments. The fracture fragments are housed in a surrogate soft tissue foot and ankle model (Sawbones Inc.). Data collected and analyzed following the fracture reduction simulation include: the number of discrete hand motions and cumulative hand distance traveled, average final articular step-off measured by CT, the number of fluoroscopy images taken(radiation exposure), and an OSATS from an expert surgeon. Multiple angles of video were recorded, including a head-mounted camera (Go Pro Hero3 silver edition) to better assess the process of thought of the trainees from their point of view.
The box skills trainer consisted of two video cameras mounted on an aluminum frame. The cameras view the workspace from orthogonal positions: one from 1.5 feet above, while the second is directed towards the participant from approximately 1.5 feet behind the workspace. In order to obstruct the view of hand motions in the workspace, a screen between the workspace and the participant is present. Thus the box skills trainer requires the participant to rely solely on the two camera views visible on a monitor placed conveniently nearby to navigate the 3D environment. Several tasks performed in the workspace were used to exercise the trainees’ skills, developing the learners’ three dimensional spatial navigation using only two dimensional images.
Costs
A recent survey reported that one of the most substantial barriers to the adoption of dedicated orthopedic surgical skills programs is the lack of available funding4. The cost of the one month simulation course is a complex variable which requires careful assessment both for the month as a whole, as well as for each of the individual modules. We categorized expenses into the following classes: Consumables, Rental, Personnel, and Donated. Consumables including cadaveric specimens, surrogate bone models and miscellaneous equipment accounted for the majority of the tangible expenses. Cadaver specimens, including shipping charges, were the largest single expense at approximately 8500 USD. Surrogate bone models represented the second largest expense at approximately 5000 USD. Other consumable supplies (e.g. suture material, PVC pipe, foam insulation) were significantly less expensive, totalling approximately 1000 USD altogether. The largest rental expense during the month was the use of C-Arm Fluoroscopy, at 12 USD/hour this accounted for between 200-300 USD for the month. At our institution, securing use of a C-Arm required substantial coordination which created difficulty with some of the modules.
Throughout the month, two laboratory personnel were available to assist in the logistics of lab set-up and take-down. In addition, these two individuals were critical to the success of photo and video archival of the month. An undergraduate student who services our laboratory on an hourly rate during the year worked full time for this month. Additional support was provided by a research-assistant who was funded by grants. The estimated cost of their time was 2500 USD. The total cost for the month was approximately 22,500 USD. By virtue of including research as a part of the program, the work was able to be funded (in part) by grants from the OMeGA Medical Grants Association, the National Board of Medical Examiners® (NBME®) Edward J. Stemmler grant, MD Medical Education Research Fund, the Orthopaedic Trauma Association, the Orthopaedic Research and Education Foundation, a private donor and a Medtronic Resident Education Grant. The remaining costs were assumed by the department.
In addition to the tangible costs enumerated, significant time, effort, energy and equipment were donated by local industry representatives. They were involved in the planning and execution of several modules, primarily adult reconstruction, trauma, and spine. Perhaps the largest cost, although not explicitly accounted for in the budget, was that of faculty time and effort. Each of the 15 faculty members that participated in various levels of planning and execution of the modules, contributed on average about 8 hours of their time between the planning and preparation of the month, as well as the planning and execution of their individual module(s).
Survey of Resident’s Experience
Upon completion of the month, the resident participants were given an inclusive questionnaire to survey their experience. The residents reported 100% satisfaction with the format of our modules, as well as the month as a whole (Figure 4a). While they ranked their skill set as similar to that of their peers at other institutions, the residents acknowledged that the program improved their surgical skill set (83%). There was an 83% consensus among the residents that they felt prepared for the month, and that the experience would enhance their operating room safety (83%). The residents unanimously agreed that this curriculum enhanced their orthopaedic training, and that it should become a permanent part of the resident education program.
Figure 4. Results from resident surveys. 4a) results of surgical skills month curriculum survey 4b) results of resident satisfaction survey.
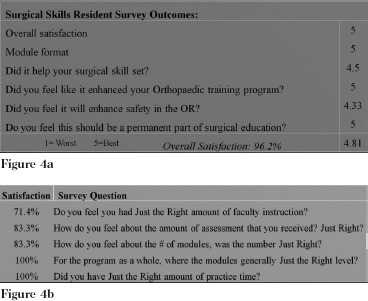
All of the residents agreed that a dedicated month of skills training was preferred to a longitudinal course during the year. One resident noted that it was helpful to have had some experience in rotations prior to the curriculum. While only half of the residents thought the amount of cognitive knowledge supporting the exercises was ideal, they unanimously felt that the modules were at exactly the right level, and that they were given adequate practice time. 71% of participants believed they had the ideal amount of faculty instruction and 83% thought that the course had the ideal number of modules and amount of assessment (Figure 4b).
Summary, Conclusions and Future Plans
This novel one month laboratory-based surgical skills curriculum for orthopedic PGY-1 residents was developed de novo and executed by the faculty of the Department of Orthopaedics at the University of Iowa. The curriculum’s modules were directed to provide PGY-1 residents with the basic surgical skills needed for future operative experiences. Despite considerable time invested in the planning and execution of the month, the faculty members were very engaged and eager to contribute to the process. Other than this faculty time commitment, the single greatest expense was for cadaveric specimens. With better planning and with different and more cost effective simulations, this expense could be reduced. The video content produced from this year’s course will be beneficial, as it should allow residents to learn more independently, and decrease the faculty time commitment in the future.
Resident satisfaction after participating in the curriculum was high. We plan to repeat this rotation again next year, with distinct goals to develop better assessment metrics as well as an assessment of the relative value of each of the modules. As we move forward, alternative sources of funding will be sought. This experience demonstrates that a dedicated one month rotation of surgical skill training aimed at educating residents at the PGY-1 level is both a viable and beneficial tool for developing the technically competent orthopaedic surgeons of the future.
References
- 1.Education TACfGM, and, Surgery TABoO. The orthopaedic surgery milestone project. ACGME and ABOS [PDF]. 2013. Available at: http://www.acgme-nas.org/assets/pdf/Milestones/OrthopaedicSurgeryMilestones.pdf. Accessed 4/1/2013.
- 2.Immerman I, Kubiak EN, Zuckerman JD. Resident work-hour rules: a survey of residents’ and program directors’ opinions and attitudes. Am J Orthop (Belle Mead NJ). 2007;36(12):E172–179. discussion E179. [PubMed] [Google Scholar]
- 3.Karam MD KJ, Yehyawi TM, Ohrt GT, Thomas GW, Jonard B, Anderson DD, Marsh JL. Application of surgical skills simulation training and assessment in orthopaedic trauma. Iowa Orthopaedic Journal. 2012;32:76–82. [PMC free article] [PubMed] [Google Scholar]
- 4.karam MD PR, Natividad H, Murray J, Marsh J.L. Current and future use of surgical skills training laboratories in orthopaedic resident education: a national survey. J Bone Joint Surg Am. 2013;95(1):e4. doi: 10.2106/JBJS.L.00177. [DOI] [PubMed] [Google Scholar]
- 5.seymour NE, Gallagher AG, roman SA, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg. 2002;236(4):458–463. doi: 10.1097/00000658-200210000-00008. discussion 463-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Surgery tACoSatAoPDi. ACS/APDS surgical skills curriculum for residents. American College of Surgeons. August 12, 2012. Accessed April 1st, 2013. [Google Scholar]
- 7.Yehyawi TM, Ohrt GT, Marsh JL, karam MD, Brown TD, Anderson DD. A simulation trainer for complex articular fracture surgery. Journal of Bone and Joint Surgery. 2013 doi: 10.2106/JBJS.L.00554. [DOI] [PMC free article] [PubMed] [Google Scholar]


