Abstract
Introduction
Medial Patellofemoral Ligament (MPFL) reconstruction is an accepted treatment for recurrent patellofemoral instability when patients have normal alignment and deficient proximal medial restraints. There are several reports of malpositioned femoral tunnels leading to poor outcomes. The purpose of this study was to analyze femoral tunnel placement after MPFL reconstruction and correlate this with outcomes.
Methods
We performed a retrospective review of MPFL reconstructions done at our institution from 2006-2010. We then evaluated lateral radiographs and measured the distance between the radiographic femoral MPFL isometric point and the center of the femoral tunnel. We also evaluated post-operative KOOS scores.
Results
The average distance from the femoral tunnel to the MPFL isometric point was 13.25 mm. Sixty-four percent of tunnels were placed greater than nine millimeters from our isometric point and deemed to be malpositioned. There was no statistically significant difference in outcomes scores in patients with anatomically placed MPFL tunnels when compared to those placed non-anatomically.
Conclusion
Sixty-four percent of MPFL reconstruction femoral tunnels were placed non-anatomically, but this did not correlate with a worse outcome. Graft tension, trochlear groove anatomy, patellar height, and dynamic restraints all play important roles in outcomes after MPFL reconstruction. Even though non-anatomic tunnel placement does not guarantee a poor result, we believe an anatomic tunnel placement will give the best chance to maximize graft function and outcome.
Introduction
Patellofemoral joint stability is achieved by the coordinated interaction of static, dynamic, and osseous constraints. The medial patellofemoral ligament (MPFL) has been found to be the primary soft tissue restraint to lateral patella translation and guides the patella into the groove during the first 30 degrees of knee flexion1-6. First-time patellar dislocations can be a harbinger of future instability. Recurrent instability has been reported to occur in 15-44% of patients following the initial event7, and up to 49% recurrence rate has been reported in patients with at least two prior instability events8. A deficient MPFL has been described as a necessary lesion in the setting of recurrent lateral dislocations of the patella9. MPFL reconstruction has become an accepted method of treating recurrent patellofemoral instability in the setting of normal alignment and deficient proximal medial restraints10,11,12.
Poor outcomes after MPFL reconstruction depend on many factors including graft tension, location of patella and femoral graft fixation, underlying trochlear dysplasia, unrecognized malalignment, patella alta, hyperlaxity and associated cartilage lesions. Bollier et al. reported on five cases of medial patella overload, iatrogenic medial instability, and medial arthrosis after MPFL reconstruction in which the femoral tunnel was malpositioned (Figure 1)13. Elias and Cosgarea showed that short grafts and proximal malposition led to compressive forces at the medial cartilage that were twice that of normal at low flexion angles and increased the peak medial pressure by more than 50% at low flexion angles14.
Figure 1. A & B: In top panel, note the anterior placement of the MPFL tunnel, with correct placement marked on this lateral radiograph. In bottom panel, the tunnel is dramatically anterior and proximal. Again, appropriate tunnel position is marked with blue dot and arrow.

As the importance of femoral tunnel position has been recognized, several authors have focused on defining anatomic and radiographic MPFL femoral insertion. In a cadaveric study, the medial patellofemoral ligament (MPFL) was found to insert 1.9 mm anterior and 3.8 mm distal to the adductor tubercle (Figures 2 and 3)1. Schottle et al. described the MPFL anatomic insertion on the femur as the isometric point for MPFL tunnel placement in reconstruction cases. In their study, they defined a radiographic point one millimeter anterior to a line extending from the posterior cortex and 2.5 mm distal to the posterior origin of the medial femoral condyle, and proximal to the level of the posterior point of the Blumensaat line15. Stephen et al., in a cadaveric study, investigated nonanatomic femoral attachment points. Proximal femoral attachment resulted in a 6.4 mm lengthening of the graft through a 0-110 degree flexion arc. Distal femoral attachments led to up to 9.1 mm of shortening through this same flexion arc16. Despite a focus on defining MPFL anatomy and function, there have been very few clinical studies looking at the femoral insertion of the MPFL graft. The purpose of this study was to analyze femoral tunnel placement after MPFL reconstruction and correlate with clinical outcomes scores.
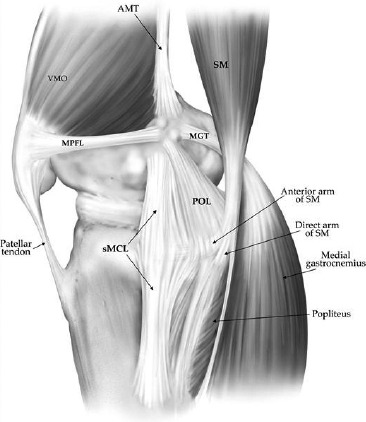
Figure 2. Illustration of the medial knee landmarks and attachments sites. Note the MPFL femoral insertion in a groove between the medial epicondyle and adductor tubercle. (Reproduced with permission from LaPrade R, Engebretsen A, Ly T, Johansen S, Wentorf F, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000–2010.).

Figure 3. Illustration of medial knee structures. Note the course and soft tissue attachements of the MPFL. (Reproduced with permission from LaPrade R, Engebretsen A, Ly T, Johansen S, Wentorf F, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000–2010).
Methods
A retrospective review of MPFL reconstructions was performed at our institution from 2006-2010. Inclusion criteria were reconstructions that utilized a femoral tunnel, postoperative lateral knee radiographs, and recorded preoperative and postoperative KOOS scores. Patients with an associated tibial tubercle transfer were also included. Fifteen isolated MPFL and 35 combined MPFL and tibial tubercle transfers for a total of 50 patients meeting inclusion criteria were identified (Table 1).
Table 1.
Data on demographics, KOOS scores, radiographic tunnel placement and correlation
| Age: Average: 31.3, Range: 14-54 | Sex: 10 males, 40 females |
| Tunnels within 9 mm isometric point (accurate placement): 16 | Tunnel greater than 9 mm from isometric point (inaccurate placement): 34 |
| Accurate tunnel placement: 36% Inaccurate tunnel placement: 64% | Average distance tunnel placement from isometric point: 13.25 mm (range: 4-28.4) |
| Average pre-operative KOOS scores: 42.0 | Average post-operative KOOS scores: 47.65 |
| Pearson correlation coefficient: 0.23-Indicative of no correlation between femoral tunnel placement and post-operative KOOS scores. |
MPFL femoral tunnel location was evaluated on lateral radiographs using a variation of Schottle’s technique15. First, we drew a vertical line extending from the inferior aspect of the posterior femoral cortex. A line perpendicular to this vertical line was drawn, extending posterior to anterior, from the intersection point of the posterior femoral cortex and metaphyseal flare. A second horizontal line was drawn, posterior to anterior, from the posterior most aspect of Blumensaat line. Finally, we defined our femoral isometric point by utilizing a point along the vertical line at the mid-point between the two horizontal lines. We measured the distance from the center of the MPFL femoral tunnel to the defined isometric point (Figure 4).
Figure 4. Determining femoral MPFL isometric point: Small circle represent point on vertical line from posterior femoral cortex, midway between horizontal line extending from cortex-metaphyseal flare junction and posterior-most aspect of Blumensaat line. Large circle represent femoral tunnel. Tunnel deemed accurately placed if within 9 mm of our isometric MPFL point. (Reproduced and modified with permission from Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801-804.).
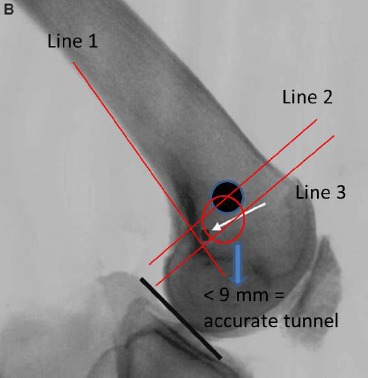
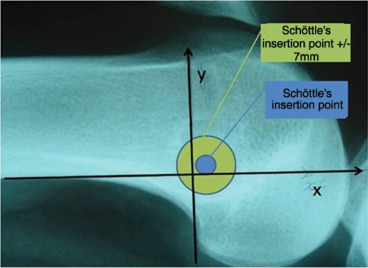
We defined anatomic position of the MPFL femoral tunnel to be within 9 mm of our defined isometric point. In a variation in a previous study on MPFL tunnel placement accuracy by Servian et al.17 (Figure 5), we increased their 7-mm diameter zone described to 9-mm, given the typical 7 mm tunnel and a more posterior defined attachment point on the femur. Tunnels were accurately placed if they fell within this 9-mm diameter and considered malpositioned if the center of the tunnel fell outside. We also evaluated preand post-operative KOOS scores and performed a statistical analysis to see if outcomes were affected by tunnel position. We performed Pearson correlation coefficient analysis to assess for significant differences.
Figure 5. Servian, et al. tunnel placement, modified from Schottle’s work. Note the 5-mm Schottle’s insertion point was expanded in Servian, et al, work to accommodate the typical 7-mm tunnel used in MPFL reconstruction. (Reproduced with permission from Servien E, Fritsch B, Lustig S, Demey G, Debarge R, Lapra C, et al. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med 2011;39(1):134-139.).
Results
Fifty patients were evaluated, 40 female and 10 male, with an average age of 31.3 years (range: 14-54). Of the 50 patients evaluated, 36 of them (64%) had tunnels placed outside of the defined 9-mm diameter. The average tunnel distance from the defined femoral isometric point was 13.25 mm (range: 4-28.4 mm).
The average preoperative KOOS score was 42.0. The average postoperative score was 47.65. Pearson correlation coefficient was 0.23 indicating negligible correlation between a change in KOOS score and femoral tunnel placement of the MPFL graft. There was no statistically significant difference in KOOS scores in patients who had a malpositioned tunnel compared to anatomic placement.
Discussion
Anatomic placement of the MPFL femoral tunnel is ideal to maximize outcomes18. Proximally placed tunnels have been shown to increase stress and contact pressure on the medial patella facet cartilage14. This can lead to medial overload, arthritis, pain and significant disability13. In addition, malpositioned femoral tunnels can increase stress on the non-isometric MPFL graft14. This can lead to failure of the reconstruction and recurrent lateral patellofemoral instability or iatrogenic medial patella subluxation13,19. Medial patella subluxation is commonly seen after prior patellar instability surgery (lateral release, tubercle transfer, or MPFL reconstruction) and involves a dramatic medial to lateral shift of the patella into the trochlear groove during knee flexion. Patients describe a sharp catching pain and clunk that can be quite disabling. Of note, they often report a lateral shift of the patella and this entity can easily be mistaken for lateral patellofemoral instability.
There are many MPFL reconstruction techniques with different methods to secure the graft to the patella and femur. There are several ways to determine the appropriate anatomic insertion site of the MPFL when performing the reconstruction. Medial knee anatomy and the femoral MPFL insertion have been studied extensively in recent years1,3,15,17,20. The MPFL inserts in the saddle between the medial epicondyle and the adductor tubercle1. This can be palpated intra-operatively. One can palpate the adductor magnus tendon insertion to help with orientation during surgery as the MPFL insertion is anterior and distal. In addition, graft isometry can be checked during surgery to determine the appropriate position of the femoral tunnel. Ideally, graft isometry should be maintained during the first 50-70 degrees of flexion and loosen in deep knee flexion. A suture can be used to connect the proposed femoral insertion site to the patella and isometry can be determined. If the suture tightens in flexion, the proposed femoral attachment site is too anterior or proximal. Based on our experience, it is easy to be fooled when only using palpation or graft isometry to determine the appropriate position of the femoral tunnel. While it is important to use several ways to check the adequacy of femoral tunnel position, we believe intra-operative fluoroscopy is the most reliable way to assess femoral tunnel position. Schottle et al. has greatly added to the understanding of radiographic MPFL insertion anatomy11. Anatomic MPFL femoral guide pin location is just anterior to the intersection of the posterior femoral cortical line and Blumensaat’s line on the lateral radiograph.
Servian et al. described a method to evaluate tunnel placement17. They made a line tangent to the posterior condyle and a perpendicular line to this at the posterior-most aspect of Blumensaat’s line, and then marked out a +/-7mm zone to accommodate a typical MPFL tunnel diameter (Figure 4). They reported accurate tunnel placement in 20 of 29 MPFL reconstructions (69%), but noted no correlation between tunnel placement and clinical outcomes, as measured by IKDC scores reported by patients17. Our results are similar to those of Servien et al. in that there was no correlation between tunnel position and outcome scores. It does not appear to be necessary to have an anatomic MPFL tunnel position to prevent further patellar instability episodes and achieve a good result. Both studies only report short-term outcomes and we suspect that longer follow-up may reveal an increased incidence of patellofemoral arthritic changes in patients with malpositioned grafts. In addition, we feel that anatomic graft position gives the best chance to achieve a successful short-term and long-term outcome with no recurrent instability, ability to return to sports, and prevention of medial overload and iatrogenic medial subluxation.
Regardless of the tunnel position, a key factor in MPFL reconstruction is to set the correct graft length or tension. Thaunat and Erasmus reported on two patients with pain and stiffness after over-tightened MPFL reconstructions19. Beck and colleagues showed that 2N of graft tension restored normal patellar translation21. Higher loads (10N and 40N) significantly restricted motion and increased medial patellofemoral contact pressure. It is likely that malpositioned grafts with good subjective outcomes were not over-tensioned. We believe medial patellofemoral overload and medial patella sub-luxation can occur when an MPFL graft has a proximal/ anterior femoral insertion and is over-tensioned. When performing MPFL reconstruction, setting appropriate graft tension or length is a key part of the procedure. There are several ways to do this. One option is to flex the knee to 60 degrees so the patella centers in the trochlea and then secure final MPFL fixation. A second method involves holding the lateral patella flush with the lateral trochlea at 30 degrees of knee flexion when securing final fixation. The MPFL is a checkrein to guide the patella into the trochlear groove during the first 30 degrees of knee flexion and is not meant to be a tight restraining ligament like others in the body. After MPFL reconstruction is finished, there should be some lateral patella translation when the knee is extended with a good endpoint. The patella should be pulled into the groove when the knee is flexed.
Several factors could have been responsible for the lack of correlation between malpositioned tunnels and poorer outcomes scores. First, our follow-up may be too short to allow the long-term effects, such as early osteoarthritic changes, to be shown. Next, while we expanded on the distance to accept a tunnel as deemed accurate, this degree of distance from the MPFL isometric point may not be far enough to reveal a significant difference. Finally, the accuracy of assessing intraoperative landmarks has not been elucidated, and it may be challenging to reliably reproduce their location despite careful surgical dissection and the use of intraoperative fluoroscopy.
Few studies have evaluated clinical outcomes in relation to femoral tunnel position. While our study showed a high rate of malpositioned tunnels, this did not correlate with outcomes scores. We propose that other factors may play a role in achieving good outcomes after this procedure including graft tension, trochlear groove anatomy, patella height, and dynamic restraints. Although results of our study suggest that it is not necessary to achieve a good result, we suggest that anatomic femoral tunnel position provides the best chance to maximize the function of the graft.
References
- 1.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89(9):2000–10. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 2.Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am, 1993;75(5):682–93. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–20. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 4.Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med. 2007;35(3):484–92. doi: 10.1177/0363546507299237. [DOI] [PubMed] [Google Scholar]
- 5.Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21(3):499–519. doi: 10.1016/s0278-5919(02)00031-5. [DOI] [PubMed] [Google Scholar]
- 6.Redziniak DE, Diduch DR, Mihalko WM, Fulkerson JP, Novicoff WM, Sheibani-Rad S, Saleh KJ. Patellar instability. J Bone Joint Surg Am. 2009;91(9):2264–75. [PubMed] [Google Scholar]
- 7.Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–62. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 8.Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–21. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 9.Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9(2):139–43. doi: 10.1016/s0968-0160(02)00002-9. [DOI] [PubMed] [Google Scholar]
- 10.Howells NR, Eldridge JD. Medial patellofemoral ligament reconstruction for patellar instability in patients with hypermobility: A case control study. J Bone Joint Surg Br. 2012;94(12):1655–9. doi: 10.1302/0301-620X.94B12.29562. [DOI] [PubMed] [Google Scholar]
- 11.Schottle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):516–21. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 12.Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M. A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):522–8. doi: 10.1007/s00167-005-0641-x. [DOI] [PubMed] [Google Scholar]
- 13.Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27(8):1153–9. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 14.Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–85. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 15.Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–4. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 16.Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA. The medial patellofemoral ligament: location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med. 2012;40(8):1871–9. doi: 10.1177/0363546512449998. [DOI] [PubMed] [Google Scholar]
- 17.Servien E, Fritsch B, Lustig S, Demey G, Debarge R, Lapra C, Neyret P. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39(1):134–9. doi: 10.1177/0363546510381362. [DOI] [PubMed] [Google Scholar]
- 18.Schottle P, Schmeling A, Romero J, Weiler A. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009;129(3):305–9. doi: 10.1007/s00402-008-0712-9. [DOI] [PubMed] [Google Scholar]
- 19.Thaunat M, Erasmus PJ. Management of overtight medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17(5):480–3. doi: 10.1007/s00167-008-0702-z. [DOI] [PubMed] [Google Scholar]
- 20.Redfern J, Kamath G, Burks R. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction. Am J Sports Med. 2010;38(2):293–7. doi: 10.1177/0363546509347602. [DOI] [PubMed] [Google Scholar]
- 21.Beck P., Brown NA, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(9):1557–63. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]


