Abstract
Background
While demographic shifts project an increased need for long-term care for an aging population, hundreds of nursing homes close each year. We examine whether nursing home closures are geographically concentrated and related to local community characteristics such as the racial and ethnic population mix and poverty.
Methods
National Online Survey Certification and Reporting data were used to document cumulative nursing facility closures over a decade, 1999 through 2008. Census 2000 zip code level demographics and poverty rates were matched to study facilities. The weighted Gini coefficient was used to measure geographic concentration of closures, and geographic information system maps to illustrate spatial clustering patterns of closures. Changes in bed supply due to closures were examined at various geographic levels.
Results
Between 1999 and 2008, a national total of 1776 freestanding nursing homes closed (11%), compared with 1126 closures of hospital-based facilities (nearly 50%). Combined, there was a net loss of over 5% of beds. The relative risk of closure was significantly higher in zip code areas with a higher proportion of blacks or Hispanics or a higher poverty rate. The weighted Gini coefficient for closures was 0.55 across all metropolitan statistical areas and 0.71 across zip codes. Closures tended to be spatially clustered in minority-concentrated zip codes around the urban core, often in pockets of concentrated poverty.
Conclusions
Nursing home closures are geographically concentrated in minority and poor communities. Since nursing home use among the minority elderly population is growing while it is declining among whites, these findings suggest that disparities in access will increase.
Regulatory oversight, reinforced by market forces and an increased focus on transparency and public reporting, is designed to eliminate poorly performing nursing homes.1–3 A small fraction of US nursing homes closes each year (not more than 2%). Perhaps this is a desired outcome, since closure is the ultimate indicator of performance failure.4 However, the operation of regulatory efforts and market forces are not likely to result in random distribution of closures. Rather, some facility types will be affected more than others.3–10 Equally important is whether closures are geographically concentrated such that their impact will not be uniform but instead will disproportionately affect certain communities and population subgroups more than others.
Within any particular community, the closure of just a few facilities could escalate anxiety among concerned family members (as well as state and local officials) owing to the negative effects of transfer trauma on frail elderly residents.11–14 Nursing home closures have been portrayed as “smoke without fire,” in that efforts are often taken to avoid public panic or a media frenzy over their potentially adverse consequences.8 Not surprisingly, federal and state regulators tend to be reluctant to close poorly performing facilities.15
A number of previous studies have examined risk factors associated with nursing home closures, focusing on structural and organizational characteristics of the facility.3–10 These studies have generally identified poor financial and quality performance as the most important and consistent antecedents of nursing home closure. In particular, closed facilities were more likely to have experienced financial troubles, lower occupancy, and a less profitable payer mix than non-closed facilities (eg, more Medicaid-supported and fewer private-paying or Medicare-supported residents); they were also likely to have received more inspection deficiency citations prior to closure. These attributes are typical of facilities ranked in the lower tier of all nursing home providers based on available resources and quality-of-care problems.16
Market factors and major policy shifts appear to have influenced nursing home closure as well. Facilities located in more competitive markets (as indicated by a greater number of nursing homes or more vacant beds) are more likely to close,3,6,8,9 and those with insufficient management and strategic planning expertise are less able to respond to exogenous policy shocks. For example, following the introduction of the federal Medicare prospective payment system (PPS) for nursing homes in 1998, there was an increase in closures.4,7 The shift to state-based Medicaid case-mix reimbursement for nursing homes has also precipitated closure.4 In addition, closures were more likely to occur among facilities in states providing lower Medicaid nursing home reimbursement rates.4,9
Herein, we document nursing home closures reported over the decade between 1999 and 2008 to better understand the geography of nursing home closures. Specifically, we address 2 questions: (1) Are nursing home closures geographically patterned or concentrated? (2) Are closures related to local community characteristics such as the racial and ethnic population mix or the level of concentrated poverty?
METHODS
DATA SOURCES
We used the Online Survey Certification and Reporting (OSCAR) database, covering the period 1999 through 2008. The OSCAR database contains facility-level aggregate information, including measures of nursing home performance, staffing, organizational characteristics, and resident characteristics for all Medicare/Medicaid–certified nursing homes in the United States. The OSCAR data are facility self-reported and reviewed under a Centers for Medicare and Medicaid Services (CMS) protocol stipulated for annual inspection and certification. Since this is a federally mandated data source, except for a few nonparticipating, exclusively private-pay facilities, virtually all licensed nursing homes in the United States are included in the OSCAR database, with ascertainment approaching 100% per year.
Of primary interest to this analysis is the information recorded in OSCAR surveys concerning facility terminations from the Medicare/Medicaid programs, which is used herein to identify closures. We identified a total of 18 259 unique nursing homes over the period 1999 through 2008 from all 50 US states and the District of Columbia. Of these, 15 998 were freestanding facilities (88%), and 2261 were hospital based (12%); 12 635 were located in urban counties (69%) and 5624 in rural counties (31%).
We used the 2000 US census data to define geographic boundaries and map nursing home closures at the state, metropolitan statistical area (MSA), and zip code levels. Zip code level population data on racial and ethnic composition and poverty (from Census 2000) were matched to study facilities to determine whether nursing home closures were related to zip code level minority and poverty concentrations. This study was exempt from institutional review board review because no individual-level information was involved, and all data analyzed were from public sources.
IDENTIFICATION OF NURSING HOME CLOSURES
We defined nursing home closure as termination from the Medicare/Medicaid programs (either voluntarily or involuntarily), based on termination codes recorded in OSCAR over the period 1999 through 2008. Although these codes were not detailed enough to differentiate more specific reasons for closure, previous research found that most terminations were voluntary, with little difference between voluntary and involuntary closures with respect to occupancy, staffing levels, or deficiency citations identified during inspection.3 Though rare, a facility might be terminated from and later reinstated in the OSCAR system. To avoid such “nonclosures,” we calculated the number of months that elapsed from the date of the last survey for that facility appearing in the OSCAR database through December 31, 2008—the end point of our observation period. If this gap exceeded 18 months, then the facility was classified as permanently closed; otherwise, the facility was deemed closed with no additional information available to ascertain permanency of the closure (n=356 or 1.95% of total facilities). There were also cases where a facility’s OSCAR records indicated no termination, but the gap between the date of its last survey and December 31, 2008, was at least 18 months; such facilities were classified as closures in this analysis (n=172 or 0.94%). The 18-month follow-up window is 3 months beyond the maximum 15-month interval between 2 successive standard surveys, as mandated by CMS in the current nursing home inspection process.
STATISTICAL ANALYSIS
We created an indicator for whether a facility was closed over the 10-year period 1999 through 2008 and tabulated freestanding and hospital-based facilities separately. Closures are presented as total counts and as the percentage of all nursing homes; the percentage measure is referred to as the cumulative rate of closures. Results were first summarized at the national level, then by region, state, MSA, and 5-digit zip code.
We calculated the Gini coefficient, weighted by the total number of ever-existing nursing homes in an area, to measure the extent of geographic concentration (or inequality in distribution) of closures across all MSAs and zip codes containing at least 1 nursing home during the study period. The weighted Gini coefficient ranges from 0 to 1; a value closer to 0 indicates a more equal distribution (ie, less concentration), and a value closer to 1 indicates a more unequal distribution (ie, higher degree of concentration). Furthermore, we used geographic information system mapping tools to visualize the geographic patterns of nursing home closures at the state level as well as spatial clustering of closures across zip codes within selected MSAs. In addition, we calculated the relative risk (RR) of closure among facilities located in zip codes with a higher proportion of minority populations or poverty rate compared with those in zip codes with the lowest proportion (bottom quartile) of minorities or poverty rate. Finally, we tallied the number of beds lost due to closures, beds added by new openings, and the resulting net change in bed supply at various geographic levels over the study period.
RESULTS
NURSING HOME CLOSURES AT THE NATIONAL LEVEL
Figure 1 illustrates the broad national trends in nursing home closures and new openings since 1993, setting the stage for a detailed analysis of closures in the decade from 1999 through 2008. The annual rate of nursing home closures increased during the pre-PPS years (before 1999), peaked during the PPS shakeout period (1999–2002), and declined gradually in subsequent years. This trend is most evident among hospital-based facilities. Between 1993 and 1999, the annual rate of new openings of hospital-based nursing homes exceeded the rate of closures by a large margin. However, in 1999, this trend reversed. In fact, from 1999 through 2008, there has been a net decline in the number of nursing homes (both hospital-based and free-standing) due to more closures than new openings. The cumulative total number of beds lost due to facility closure was estimated at 184 264 (or 10.1% of all ever-existing beds) over this 10-year period, most of which were in closed freestanding rather than hospital-based facilities. In contrast, only 87 362 beds (or 4.8%) were added due to new facility openings over the same period, resulting in a cumulative net loss of 96 902 (or over 5%) beds (eTable [http://www.archinternmed.com]).
Figure 1.
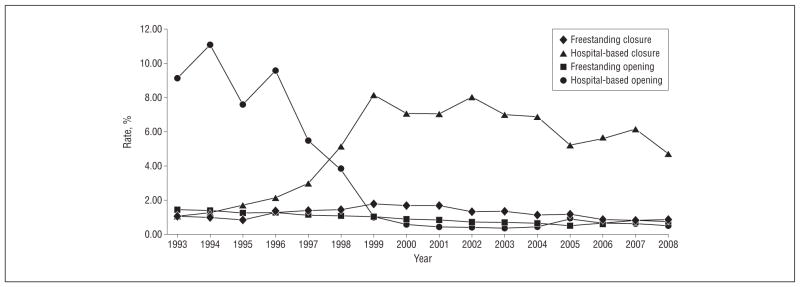
Annual rates of nursing home closures and openings from 1993 through 2008.
Between 1999 and 2008, a total of 2902 nursing homes closed, or nearly 16% of all Medicare/Medicaid–certified facilities (Table 1). The cumulative closure rate was substantially higher in hospital-based facilities than in freestanding ones (50% vs 11%). Urban hospital-based facilities had the highest cumulative closure rate (60%). The closure rate among freestanding facilities was roughly the same in urban (11%) and rural (10%) areas.
Table 1.
Cumulative Rate of Nursing Home Closures, 1999–2008, at National, Regional, and MSA Levelsa
| Geographical Unit | All Facilities
|
Freestanding
|
Hospital Based
|
|||
|---|---|---|---|---|---|---|
| Closures | Total No. | Closures | Total No. | Closures | Total No. | |
| National | 2902 (15.9) | 18 259 | 1776 (11.1) | 15 998 | 1126 (49.8) | 2261 |
| Rural | 766 (13.6) | 5624 | 502 (10.4) | 4804 | 264 (32.2) | 820 |
| Urban | 2136 (16.9) | 12 635 | 1274 (11.4) | 11 194 | 862 (59.8) | 1441 |
| Northeast | 440 (14.1) | 3122 | 301 (10.7) | 2822 | 139 (46.3) | 300 |
| Boston, MA-NH PMSA | 87 (24.6) | 354 | 60 (18.7) | 321 | 27 (81.8) | 33 |
| Philadelphia, PA-NJ PMSA | 54 (18.8) | 288 | 30 (11.8) | 255 | 24 (72.7) | 33 |
| Pittsburgh, PA MSA | 30 (19.5) | 154 | 8 (6.6) | 122 | 22 (68.8) | 32 |
| Providence-Fall River-Warwick, RI-MA MSA | 21 (14.3) | 147 | 17 (12.1) | 141 | 4 (66.7) | 6 |
| Worcester, MA-CT PMSA | 17 (23.0) | 74 | 15 (21.1) | 71 | 2 (66.7) | 3 |
| Midwest | 858 (14.4) | 5968 | 582 (10.9) | 5319 | 276 (42.5) | 649 |
| Chicago, IL PMSA | 49 (12.5) | 391 | 21 (6.1) | 346 | 28 (62.2) | 45 |
| St Louis, MO-IL MSA | 47 (21.6) | 218 | 29 (15.1) | 192 | 18 (69.2) | 26 |
| Indianapolis, IN MSA | 39 (27.7) | 141 | 30 (23.3) | 129 | 9 (75.0) | 12 |
| Cleveland-Lorain-Elyria, OH PMSA | 35 (17.5) | 200 | 22 (12.6) | 175 | 13 (52.0) | 25 |
| Kansas City, MO-KS MSA | 35 (23.3) | 150 | 15 (11.9) | 126 | 20 (83.3) | 24 |
| South | 1122 (17.9) | 6284 | 636 (11.6) | 5474 | 486 (60.0) | 810 |
| Dallas, TX PMSA | 48 (29.3) | 164 | 24 (17.4) | 138 | 24 (92.3) | 26 |
| Houston, TX PMSA | 41 (28.3) | 145 | 17 (14.9) | 114 | 24 (77.4) | 31 |
| New Orleans, LA MSA | 35 (45.5) | 77 | 18 (31.6) | 57 | 17 (85.0) | 20 |
| Oklahoma City, OK MSA | 34 (36.2) | 94 | 22 (27.2) | 81 | 12 (92.3) | 13 |
| Tampa-St Petersburg-Clearwater, FL MSA | 33 (21.0) | 157 | 16 (11.8) | 136 | 17 (81.0) | 21 |
| West | 482 (16.7) | 2885 | 257 (10.8) | 2383 | 225 (44.8) | 502 |
| Los Angeles-Long Beach, CA PMSA | 62 (13.9) | 446 | 29 (7.6) | 382 | 33 (51.6) | 64 |
| Phoenix-Mesa, AZ MSA | 29 (27.6) | 105 | 12 (14.0) | 86 | 17 (89.5) | 19 |
| Oakland, CA PMSA | 23 (18.9) | 122 | 17 (15.5) | 110 | 6 (50.0) | 12 |
| Seattle-Bellevue-Everett, WA PMSA | 23 (22.5) | 102 | 18 (18.8) | 96 | 5 (83.3) | 6 |
| San Francisco, CA PMSA | 21 (31.3) | 67 | 15 (29.4) | 51 | 6 (37.5) | 16 |
| Across all MSAs, mean (SD) (n=323) | 6 (10) (15.4 [10.9]) | 38 (54) | 4 (6) (10.0 [9.4]) | 33 (48) | 3 (5) (54.2 [38.6]) | 4 (7) |
Abbreviations: MSA, metropolitan statistical area; PMSA, primary MSA.
Unless otherwise indicated, data are number (percentage) of closures.
REGIONAL AND INTERSTATE VARIATIONS
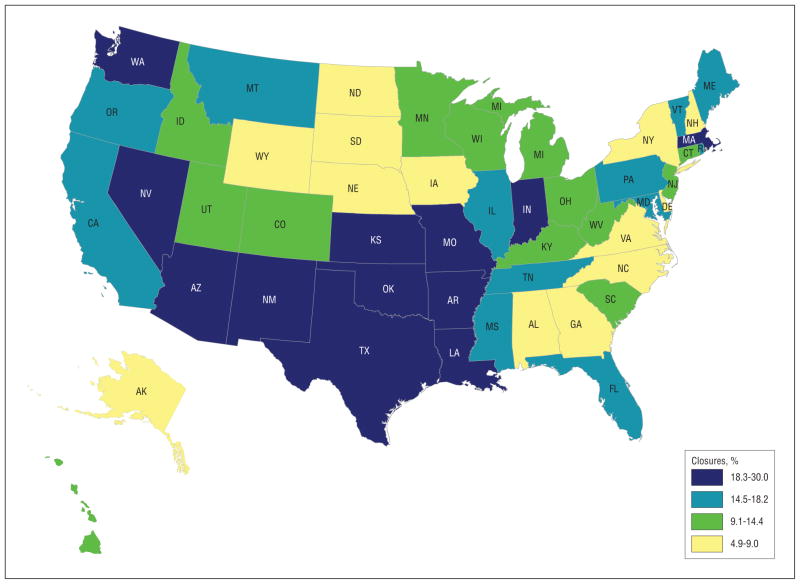
The overall cumulative closure rate was highest in the South (18%) and West (17%) and lowest in the Northeast and Midwest (14% for both) (Table 1). At the state level, the overall rate of closures varied more widely, ranging from roughly 5% in both Wyoming and South Dakota to 28% in Nevada and 30% in Oklahoma (Figure 2). There was a similar pattern with respect to the percentage of beds closed, with all 4 regions and most states within each region sustaining a cumulative net loss of nursing home beds due to facility closure over the study period (eTable).
Figure 2.
Cumulative rate of nursing home closures by state, 1999 through 2008.
CONCENTRATION OF NURSING HOME CLOSURES ACROSS MSAs
The weighted Gini coefficient for overall nursing home closures was 0.55 across all MSAs, suggesting an uneven geographic distribution of closures. Table 1 lists the 5 MSAs with the greatest number of cumulative total closures within each region. Boston ranked the highest in the cumulative total number of closures (87 closures or 25% of all facilities) among all MSAs in the Northeast and nationally as well. Within the regional list, the highest number of closures occurred in Chicago in the Midwest (49 closures or 13%), Dallas in the South (48 closures or 29%), and Los Angeles–Long Beach in the West (62 closures or 14%). In relative terms, all but a few of those 20 MSAs listed in Table 1 had their percentage of closures well above the regional or all-MSA average percentage of closures.
A ZIP CODE VIEW OF NURSING HOME CLOSURES
Since MSAs vary a great deal in size and socioeconomic characteristics, significant variations in nursing home closures might be hidden within the boundaries of each MSA. To reveal local community-level dynamics of nursing home closures, we focused the analysis on zip codes. A total of 9762 unique zip codes were identified, each containing at least 1 nursing home. The weighted Gini coefficient for the distribution of closures across all zip codes was 0.71, revealing a much more uneven distribution of closures at the community level than at the MSA level.
In Table 2, we summarize the association between nursing home closure and zip code level racial and ethnic population mix and poverty as well as the estimated net loss of beds due to closures, tabulated separately for freestanding and hospital-based facilities. Among free-standing facilities, the RR of closure in zip codes with the highest percentage of blacks (top quartile) was 1.38 (95% confidence interval [CI], 1.21–1.58) times greater than in zip codes with the lowest percentage of blacks (bottom quartile). Similarly, freestanding facilities in the top quartile of Hispanic zip codes were 1.37 (95% CI, 1.20–1.56) times as likely to close as those in the bottom quartile. The RR of closure in zip codes with the highest level of poverty (top quartile) was more than double that in zip codes with the lowest (bottom quartile) poverty rate (RR, 2.01; 95% CI, 1.76–2.29). Similar patterns of association were observed in hospital-based facilities.
Table 2.
Cumulative Rate of Nursing Home Closures and Beds Closed, 1999–2008, by Zip Code Level Concentration of Minority Populations and Poverty
| Zip Code Percentage Quartilesa | Facilities Closed
|
Net Loss of Beds, No. (%)b | Total Facilities, No. | |
|---|---|---|---|---|
| No. (%) | Relative Risk (95% CI) | |||
| Freestanding | ||||
| Blacks | ||||
| 1 | 283 (9.9) | 1 [Reference] | −9458 (−4.1) | 2845 |
| 2 | 337 (8.4) | 0.84 (0.72–0.98) | −5255 (−1.2) | 4027 |
| 3 | 539 (11.6) | 1.17 (1.02–1.34) | −17 026 (−3.2) | 4650 |
| 4 | 613 (13.7) | 1.38 (1.21–1.58) | −36 962 (−6.9) | 4460 |
| Hispanics | ||||
| 1 | 314 (9.4) | 1 [Reference] | −11 684 (−3.7) | 3346 |
| 2 | 385 (9.8) | 1.05 (0.91–1.21) | −13 876 (−3.4) | 3913 |
| 3 | 494 (11.9) | 1.27 (1.11–1.45) | −20 769 (−4.4) | 4137 |
| 4 | 560 (12.8) | 1.37 (1.20–1.56) | −21 634 (−4.3) | 4367 |
| Poverty rate | ||||
| 1 | 300 (7.8) | 1 [Reference] | 4747 (1.1) | 3866 |
| 2 | 386 (9.7) | 1.26 (1.09–1.45) | −10 682 (−2.6) | 3961 |
| 3 | 457 (11.1) | 1.43 (1.24–1.64) | −17 025 (−4.0) | 4117 |
| 4 | 627 (15.6) | 2.01 (1.76–2.29) | −45 683 (−10.3) | 4025 |
|
| ||||
| Hospital-Based | ||||
| Blacks | ||||
| 1 | 109 (26.0) | 1 [Reference] | −2600 (−14.7) | 419 |
| 2 | 224 (43.9) | 1.69 (1.40–2.04) | −5176 (−21.3) | 510 |
| 3 | 387 (60.7) | 2.33 (1.96–2.77) | −10 350 (−41.6) | 638 |
| 4 | 390 (57.8) | 2.22 (1.87–2.64) | −9438 (−28.6) | 675 |
| Hispanics | ||||
| 1 | 168 (35.4) | 1 [Reference] | −3438 (−16.8) | 474 |
| 2 | 245 (46.9) | 1.32 (1.14–1.54) | −5776 (−25.5) | 522 |
| 3 | 279 (50.8) | 1.43 (1.24–1.66) | −7395 (−28.7) | 549 |
| 4 | 412 (60.8) | 1.71 (1.50–1.96) | −10 797 (−35.8) | 678 |
| Poverty rate | ||||
| 1 | 165 (51.2) | 1 [Reference] | −5139 (−28.5) | 322 |
| 2 | 248 (45.2) | 0.88 (0.77–1.01) | −5256 (−24.3) | 549 |
| 3 | 305 (46.3) | 0.90 (0.79–1.03) | −7389 (−25.2) | 659 |
| 4 | 391 (55.1) | 1.07 (0.95–1.22) | −9762 (−31.6) | 710 |
Abbreviation: CI, confidence interval.
As quartile number increases, percentage of minority population or poverty rate increases.
Net number of lost beds is estimated by newly added beds minus closed beds cumulatively over the 10-year period 1999 through 2008. The denominator for the percentage of net lost beds includes all ever-existing beds over the period within each stratum.
Table 2 also lists both a greater number and percentage of net lost beds due to facility closures in zip codes with a higher proportion of minorities or higher poverty rates. Although hospital-based nursing homes lost a much greater percentage of both facilities and beds than freestanding homes over the study period, a great majority of both closed facilities and closed beds came from freestanding nursing homes. (Also see the eTable for hospital-based to freestanding ratios in facility closures and lost beds.)
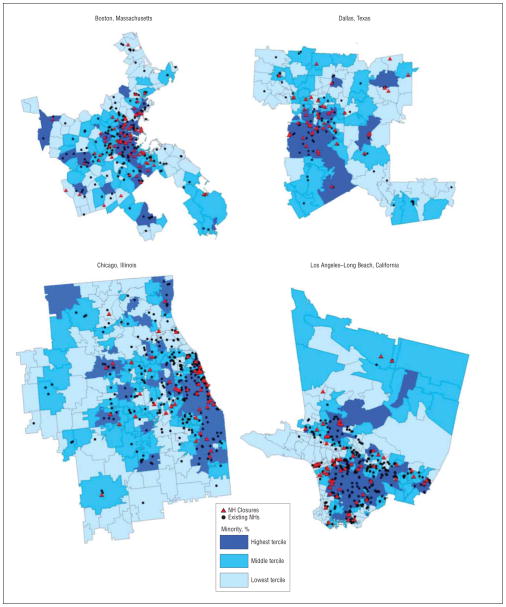
In Figure 3, we present maps to depict the spatial pattern of nursing home closures associated with selected zip code characteristics. Nursing home closures were largely clustered in zip codes with higher proportions of minority populations. Furthermore, these zip codes were typically clustered around neighborhoods close to the urban core, most often in pockets of concentrated poverty.
Figure 3.
Spatial clustering of nursing home (NH) closures from 1999 through 2008 across zip codes in 4 selected metropolitan statistical areas.
We conducted an analysis at the zip code level to calculate the distance from the centroid of each zip code to the nearest operating nursing home with Medicare/Medicaid–certified beds, separately for 1999 and 2008. We used this distance as a proximate measure of access barrier, since most older people (and their families) prefer a convenient location when searching for and selecting a long-term care facility.17 Results reveal that in zip codes in which at least 1 nursing home closed from 1999 through 2008, the nearest distance to an operating facility increased from 2.73 (95% CI, 2.59–2.87) miles in 1999 to 3.81 (95% CI, 3.58–4.04) miles in 2008, on average, by an additional 1.08 (95% CI, 0.91–1.25) miles or 39.6%. In contrast, this distance was shortened slightly in zip codes without any nursing home closure, by −2.8%, from 3.20 (95% CI, 3.11–3.29) to 3.11 (95% CI, 3.02–3.19) miles. Similarly, in the poorest quartile of zip codes (ranked by poverty rate), this nearest distance increased by 10.4%, from 3.45 (95% CI, 3.26–3.64) to 3.81 (95% CI, 3.59–4.03) miles, in contrast to a much smaller increase in the remaining zip codes of 4.7%, from 2.97 (95% CI, 2.89–3.04) to 3.11 (95% CI, 3.02–3.20) miles. Finally, in zip codes with the highest percentage of minorities (top quartile), this distance increased by 6.7%, from 2.98 (95% CI, 2.79–3.18) miles to 3.18 (95% CI, 2.97–3.39) miles, which was roughly the same as in the remaining zip codes, by 6.4%, from 3.12 (95% CI, 3.05–3.20) to 3.32 (95% CI, 3.23–3.41) miles.
COMMENT
UNEQUAL HIT: GEOGRAPHIC DISPARITIES IN NURSING HOME CLOSURE
Our analysis reveals that between 1999 and 2008, nearly 16% of all certified nursing home facilities in the United States closed, accompanied by a cumulative net loss of more than 5% of beds. Importantly, we find compelling evidence that closures are unevenly distributed geographically. The hardest hit communities with multiple closures were often those with the greatest concentration of racial and ethnic minority populations and poverty. Previous studies have found that lower-tier nursing homes, characterized by limited resources, reliance on Medicaid, poor performance, and lower-quality care,16 are most likely to serve poor and nonwhite populations, both African Americans and Hispanics,18,19 and are at greatest risk of closure.4,6,20 In addition, our results suggest that over the 10 years of the study period, the distance to the nearest operating nursing home has increased significantly for those living in zip codes where there was a closure compared with those without any closure. More importantly, this distance increased more substantially in poor and minority zip codes than in nonpoor and nonminority zip codes. It should be noted that our distance measure used mileage “as the crow flies,” which could be quite different from real distance by car or public transit lines. Combined, these patterns raise concerns that nursing home closures disproportionately affect the access that minority older populations residing in poor neighborhoods have to any nursing home care, much less high-quality care.
Since most failed nursing homes experience a downward spiral in financial and quality performance before their eventual closure, one might argue that the demise of such facilities is not necessarily a concern. In support of this argument, nursing home occupancy rates have dropped in most long-term care markets in recent years (http://LTCFocUS.org). However, in the broader context of structural and socioeconomic disparities and persistent racial residential segregation, the clustering of nursing home closures in poor and minority-concentrated urban neighborhoods is troubling. This phenomenon, arguably, resembles similar dynamics of inequalities in public schools, housing, environmental decline, and other sectors. It is likely that better-performing nursing homes located in more prosperous suburban neighborhoods will increasingly “skim the cream” (ie, private pay and problem-free patients) from the underresourced urban facilities, thereby accelerating their death spiral and the decline of inner-city areas in which these troubled facilities are located.
POLICY IMPLICATIONS
The current analysis reinforces previous work16,21 that has identified the considerable risk residents of lower-tier facilities face in terms of disparities in access and quality of care that would eventually place them in “triple jeopardy.” That is, those in need of long-term care in this tier are more likely (1) to be placed in substandard facilities, (2) to live in areas of increased closures, thereby limiting their access to nursing home care; and (3) to live in areas with limited home- and community-based alternatives to nursing home care.22
In addition, recent research has documented the increasing use of nursing homes among minority elderly people.19 The demand for long-term care is likely to rise as the minority older population continues to grow rapidly in the near term. Combined, all these forces are likely to exacerbate the problem of nursing home access for those in greatest need who reside in disadvantaged neighborhoods. Superimposed on these disparities is the ongoing effort of most state Medicaid programs to control their costs by shifting Medicaid recipients who qualify for nursing home care to home- and community-based alternatives. As these “rebalancing” efforts continue to grow and competition with noninstitutional health care providers intensifies, it is likely that more nursing homes will close in the years to come.
A similar shift to community mental health services was to have occurred with the closure of state psychiatric hospital systems concurrent with the implementation of the Medicare and Medicaid programs.23 Medicare and Medicaid offered the opportunity to shift states’ costs for psychiatric care onto the federal government if provided outside state institutions. These efforts were often hastily planned, and the supply of community-based care options did not meet the demand created by deinstitutionalization. This resulted in unintended adverse consequences for the recipients of care, their families, and communities. There is reason for concern that we may face a similar problem in long-term care.
Ultimately, a fuller picture of the impact of nursing home closures must include information on all nursing home alternatives. Of particular concern is the lack of a national database, comparable to the OSCAR database, on nursing home alternatives. We cannot fully map long-term care markets at either the MSA or zip code level without national historical and locational data on assisted living facilities, home health services, or adult day care services. Without a complete appreciation of the impact of nursing home closures on residents and local long-term care markets, our ability to select among these and other options will be short-sighted and ineffective.
LIMITATIONS
The OSCAR data we relied on to identify closures may contain reporting errors. Thus, it is possible that our accounting of closed facilities is incomplete. However, no definitive records of closures currently exist from either government or industry.8,12 We should also note that our definition of closures is based on termination from the Medicare/Medicaid programs, and in some relatively rare cases, facilities may continue to operate by converting to assisted-living facilities or simple board and care homes. With relatively few exceptions, these facilities rely solely on private payments and often have restrictions as to the maximum level of impairment of their residents. The net result is that access for impaired people who reside in nursing homes is reduced when a facility is decertified. Although beyond the scope of the current analysis, the potential impact of nursing home closures on both the displaced residents and local communities warrants close monitoring. Additional research and policy discussions are necessary to fully gauge and mediate this impact.
In conclusion, nursing home closures tend to be geographically concentrated in minority and poor communities. The cumulative loss of nursing facility beds in the aftermath of closures, combined with the lack of alternative long-term care services in these disadvantaged communities and increasing use of nursing homes among minority elderly people, suggests that disparities in access will increase.
Supplementary Material
Acknowledgments
Funding/Support: This work was supported in part by National Institute on Aging grant P01AG027296.
Role of the Sponsor: The National Institute on Aging had no role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Footnotes
Financial Disclosure: None reported.
Previous Presentations: Results from an earlier version of this article were presented at the Academy Health Annual Research Meeting (podium presentation); June 29, 2010; Boston, Massachusetts; and at the International Conference on Aging in the Americas (poster presentation); September 16, 2010; Austin, Texas.
Online-Only Material: The eTable is available at http://www.archinternmed.com.
Additional Contributions: Md Momotazur Rahman, PhD, helped calculate the nearest distance measures reported in this article. Dr Rahman did not receive any external compensation for his contribution.
Author Contributions: Drs Feng and Lepore had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Feng, Lepore, Clark, Tyler, Smith, Mor, and Fennell. Acquisition of data: Feng, Lepore, and Mor. Analysis and interpretation of data: Feng, Lepore, Clark, Smith, Mor, and Fennell. Drafting of the manuscript: Feng and Fennell. Critical revision of the manuscript for important intellectual content: Feng, Lepore, Clark, Tyler, Smith, Mor, and Fennell. Statistical analysis: Feng, Lepore, and Mor. Obtained funding: Mor and Fennell. Administrative, technical, and material support: Lepore, Clark, Tyler, Mor, and Fennell. Study supervision: Mor and Fennell.
References
- 1.Harrington C. Regulating nursing homes: residential nursing facilities in the United States. BMJ. 2001;323(7311):507–510. doi: 10.1136/bmj.323.7311.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walshe K. Regulating U.S. nursing homes: are we learning from experience? Health Aff (Millwood) 2001;20(6):128–144. doi: 10.1377/hlthaff.20.6.128. [DOI] [PubMed] [Google Scholar]
- 3.Angelelli J, Mor V, Intrator O, Feng Z, Zinn J. Oversight of nursing homes: pruning the tree or just spotting bad apples? Gerontologist. 2003;43(spec No 2):67–75. doi: 10.1093/geront/43.suppl_2.67. [DOI] [PubMed] [Google Scholar]
- 4.Zinn J, Mor V, Feng Z, Intrator O. Determinants of performance failure in the nursing home industry. Soc Sci Med. 2009;68(5):933–940. doi: 10.1016/j.socscimed.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Castle NG. Nursing home closures and quality of care. Med Care Res Rev. 2005;62(1):111–132. doi: 10.1177/1077558704271728. [DOI] [PubMed] [Google Scholar]
- 6.Castle NG, Engberg J, Lave J, Fisher A. Factors associated with increasing nursing home closures. Health Serv Res. 2009;44(3):1088–1109. doi: 10.1111/j.1475-6773.2009.00954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dalton K, Howard HA. Market entry and exit in long-term care: 1985–2000. Health Care Financ Rev. 2002;24(2):17–32. [PMC free article] [PubMed] [Google Scholar]
- 8.Kitchener M, Bostrom A, Harrington C. Smoke without fire: nursing facility closures in California, 1997–2001. Inquiry. 2004;41(2):189–202. doi: 10.5034/inquiryjrnl_41.2.189. [DOI] [PubMed] [Google Scholar]
- 9.Castle NG. Nursing home closures, changes in ownership, and competition. Inquiry. 2005;42(3):281–292. doi: 10.5034/inquiryjrnl_42.3.281. [DOI] [PubMed] [Google Scholar]
- 10.Castle NG. Characteristics of nursing homes that close. Health Care Manage Rev. 2006;31(1):78–88. doi: 10.1097/00004010-200601000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Castle NG. Replaced by fish: when a nursing home closes, what happens to the residents? Balance. 1997;1(4):12–13. 28–29. [PubMed] [Google Scholar]
- 12.Wood EF. Termination and Closure of Poor Quality Nursing Homes: What Are the Options? Washington, DC: AARP Public Policy Institute; 2002. [Google Scholar]
- 13.Castle NG. Relocation of the elderly. Med Care Res Rev. 2001;58(3):291–333. doi: 10.1177/107755870105800302. [DOI] [PubMed] [Google Scholar]
- 14.Mirotznik J, Kamp LL. Cognitive status and relocation stress: a test of the vulnerability hypothesis. Gerontologist. 2000;40(5):531–539. doi: 10.1093/geront/40.5.531. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health and Human Services. [Accessed October 3, 2010.];Nursing home enforcement: application of mandatory remedies (OEI-06-03-00410; May 2006) http://oig.hhs.gov/oei/reports/oei-06-03-00410.pdf.
- 16.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castle NG. Searching for and selecting a nursing facility. Med Care Res Rev. 2003;60(2):223–252. doi: 10.1177/1077558703060002005. [DOI] [PubMed] [Google Scholar]
- 18.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff (Millwood) 2007;26(5):1448–1458. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- 19.Fennell ML, Feng Z, Clark MA, Mor V. Elderly Hispanics more likely to reside in poor-quality nursing homes. Health Aff (Millwood) 2010;29(1):65–73. doi: 10.1377/hlthaff.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Massachusetts Senate Post Audit and Oversight Committee. Crisis at Home: the Impact of Massachusetts’ Nursing Home Closures: Senate Bill 2050. Boston: Massachusetts Senate; 2003. [Google Scholar]
- 21.Smith DB, Feng Z. The accumulated challenges of long-term care. Health Aff (Millwood) 2010;29(1):29–34. doi: 10.1377/hlthaff.2009.0507. [DOI] [PubMed] [Google Scholar]
- 22.Stevenson DG, Grabowski DC. Sizing up the market for assisted living. Health Aff (Millwood) 2010;29(1):35–43. doi: 10.1377/hlthaff.2009.0527. [DOI] [PubMed] [Google Scholar]
- 23.Koyanagi C. Learning From History: Deinstitutionalization of People With Mental Illness as Precursor to Long-Term Care Reform. Washington, DC: Bazelon Center for Mental Health Law; 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.