Abstract
Background:
The etiology of adjacent-segment disease following cervical spine arthrodesis remains controversial. The objective of the current study was to evaluate cervical intervertebral range of motion during dynamic flexion-extension in patients who had undergone a single-level arthrodesis and in asymptomatic control subjects.
Methods:
Ten patients who had undergone a single-level (C5/C6) anterior arthrodesis and twenty asymptomatic control subjects performed continuous full range-of-motion flexion-extension while biplane radiographs were collected at thirty images per second. A previously validated tracking process determined three-dimensional vertebral position on each pair of radiographs with submillimeter accuracy. Six-degrees-of-freedom kinematics between adjacent vertebrae were calculated throughout the entire flexion-extension movement cycle over multiple trials for each participant. Cervical kinematics were also calculated from images collected during static full flexion and static full extension.
Results:
The C4/C5 motion segment moved through a larger extension range of motion and a smaller flexion range of motion in the subjects with the arthrodesis than in the controls. The extension difference between the arthrodesis and control groups was 3.8° (95% CI [confidence interval], 0.9° to 6.6°; p = 0.011) and the flexion difference was −2.9° (95% CI, −5.3° to −0.5°; p = 0.019). Adjacent-segment posterior translation was greater in the arthrodesis group than in the controls, with a C4/C5 difference of 0.8 mm (95% CI, 0.0 to 1.6 mm) and a C6/C7 difference of 0.4 mm (95% CI, 0.0 to 0.8 mm; p = 0.016). Translation range of motion and rotation range of motion were consistently larger when measured on images collected during dynamic functional movement as opposed to images collected at static full flexion or full extension. The upper 95% CI limit for anterior-posterior translation range of motion was 3.45 mm at C3/C4 and C4/C5, but only 2.3 mm at C6/C7.
Conclusions:
C5/C6 arthrodesis does not affect the total range of motion in adjacent vertebral segments, but it does alter the distribution of adjacent-segment motion toward more extension and less flexion superior to the arthrodesis and more posterior translation superior and inferior to the arthrodesis during in vivo functional loading. Range of motion measured from static full-flexion and full-extension images underestimates dynamic range of motion. Clinical evaluation of excessive anterior-posterior translation should take into account the cervical vertebral level.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Degenerative changes adjacent to fused cervical vertebrae have been well documented1-7, and may occur as early as seventeen months following surgery7. The reported prevalence of these degenerative changes has ranged from 16% (of 112 patients)6 to 25% (of 374 patients)4 within ten years after the operation, and the changes require adjacent-level surgery in 6% to 10% of patients5,8-11. In a twenty-one-year follow-up study of fifty patients who had undergone anterior cervical spine arthrodesis, 32% developed recurrent pain at an average of 7.2 years after surgery, and 16% required surgery for disc disease at an adjacent level3. The most likely location for adjacent-segment degeneration is unclear, as one study suggested that progressive degeneration occurs with equal frequency superior and inferior to the fused segment12 while another indicated that adjacent-segment degeneration is level-dependent and most prevalent at the C5/C6 and C6/C7 discs4. The degeneration may progress as a result of underlying spondylosis4,13,14, increased motion in adjacent vertebrae2,15-18, or a combination of these factors1,5.
Investigations designed to identify mechanical factors that may expedite adjacent-segment degeneration have primarily focused on excessive motion adjacent to the fused segment during flexion-extension. To identify excessive motion, the normal range of motion in asymptomatic subjects must first be defined. This has been previously accomplished by manually identifying anatomic landmarks on two-dimensional lateral radiographs16,19-25. These measurements have inherent limitations, including potential differences between ranges of motion calculated from radiographs collected in static positions compared with dynamic muscle-driven movement26, the high measurement variability associated with manual digitization24,25,27-29, and the inability to assess motion that occurs out of the film plane. Numerous authors have noted the necessity for three-dimensional16,26,30-33, in vivo23,26,30,34 measurements of the cervical spine under dynamic load16,28,34,35.
The overall objective of the current study was to evaluate cervical intervertebral range of motion during dynamic flexion-extension in patients who had undergone single-level anterior cervical discectomy and fusion and asymptomatic control subjects. The first aim was to assess differences in intervertebral range of motion, in terms of all six degrees of freedom (three translations and three rotations), between control subjects and patients who had undergone single-level anterior cervical discectomy and arthrodesis. The second aim was to compare static range-of-motion measurements with those obtained during dynamic, functional movement.
Materials and Methods
Subjects
Following institutional review board approval, subjects who were at least eighteen years of age and scheduled to undergo, or had recently undergone, single-level anterior cervical discectomy and arthrodesis were identified during clinic visits. Pregnant women, patients diagnosed with osteoporosis, and patients with any other injury or disease that interferes with spine function were excluded. Asymptomatic controls were recruited to approximately match the age and sex distribution of the subjects treated with arthrodesis. Control-subject recruitment was accomplished through an advertisement in an employee newsletter and word of mouth. Data from thirty subjects (ten patients treated with C5/C6 arthrodesis and twenty controls) who provided informed consent to participate in this study were included in the present analysis. Demographic and surgical details for the control and arthrodesis groups are summarized in the Appendix.
Data Collection and Processing
High-resolution computed tomography (CT) scans (0.29 × 0.29 × 1.25-mm voxels) (GE LightSpeed 16; GE Healthcare, Waukesha, Wisconsin) of the cervical spine (C2-C7) were acquired for each participant. Bone tissue was segmented from the CT volume with use of a combination of commercial software (Mimics software; Materialise, Leuven, Belgium) and manual segmentation36. A three-dimensional model of each vertebra was generated from the segmented bone tissue37. Markers were interactively placed on the three-dimensional bone models to define bone-specific anatomic coordinate systems.
Subjects performed continuous full-range-of-motion flexion-extension to the beat of a metronome set at a rate of forty to forty-four beats per minute to complete one full movement cycle in approximately three seconds. Biplane radiographs were collected at thirty images per second for three seconds during two or three dynamic movement trials per subject (Fig. 1-A). A total of seventy-eight dynamic flexion-extension trials were included in this analysis. Three static trials were also collected for each subject: one in the neutral position, one in full flexion, and one in full extension. For the flexion radiograph, subjects were instructed and encouraged to flex their head down as far as possible, pushing the chin into the chest if possible. For the extension radiograph, they were instructed and encouraged to look up and back as far as possible. For the neutral radiograph, they were instructed to look directly forward. A previously validated tracking process determined three-dimensional vertebral position on each pair of radiographs with submillimeter accuracy38 for all static and dynamic trials (Fig. 1-B). Details regarding the model-based tracking process, including hardware and software specifications, calibration and distortion correction procedures, and computational algorithms, have been described previously38-41. Tracked data were filtered at 1.7 Hz with use of a fourth-order, low-pass Butterworth filter with the filter frequency determined with use of residual analysis42. Six-degrees-of-freedom kinematics between adjacent vertebrae (three translations: medial-lateral, superior-inferior, and anterior-posterior; three rotations: flexion-extension, twist, and lateral bend) were calculated for every frame in each trial in accordance with established standards for reporting spine kinematics43,44 (Fig. 2). Three-dimensional motion data for C2 were not available for four subjects treated with arthrodesis, either because the CT scan did not include enough of this bone or because the subject was positioned incorrectly within the field of view of the biplane x-ray system. These oversights in data collection were corrected prior to testing of any asymptomatic control subject. Thus, C2/C3 data are presented only for the asymptomatic control group.
Biplane radiograph data collection system.
Fig. 1-A.
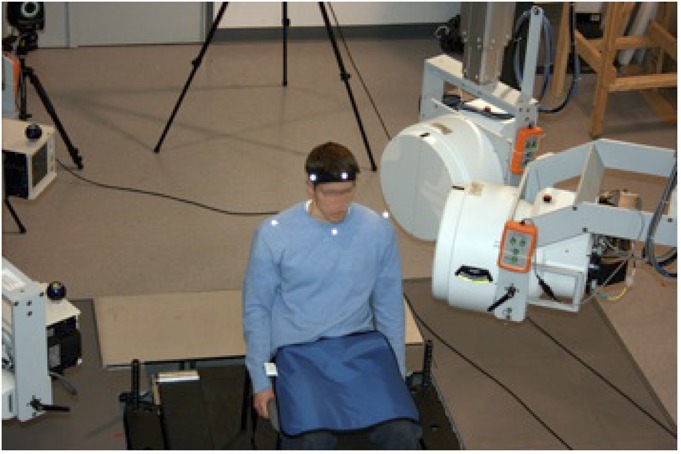
X-ray tubes (left) directed x-rays through subject-to-image intensifiers (right). 2.5-ms x-ray pulses (70 kV, 160 mA) were generated by cardiac cine-angiography generators at a rate of 30 Hz, and images were collected by high-speed cameras synchronized to the x-ray pulses. Head motion relative to the trunk was determined with use of reflective markers placed on the head and trunk (Vicon-MX, Vicon, Oxford, United Kingdom). (Reproduced, with modification, from: Anderst WJ, Baillargeon E, Donaldson WF 3rd, Lee JY, Kang JD. Validation of a noninvasive technique to precisely measure in vivo three-dimensional cervical spine movement. Spine [Phila Pa 1976]. 2011 Mar 15;36[6]:E393-400. Reproduced with permission.)
Fig. 1-B.
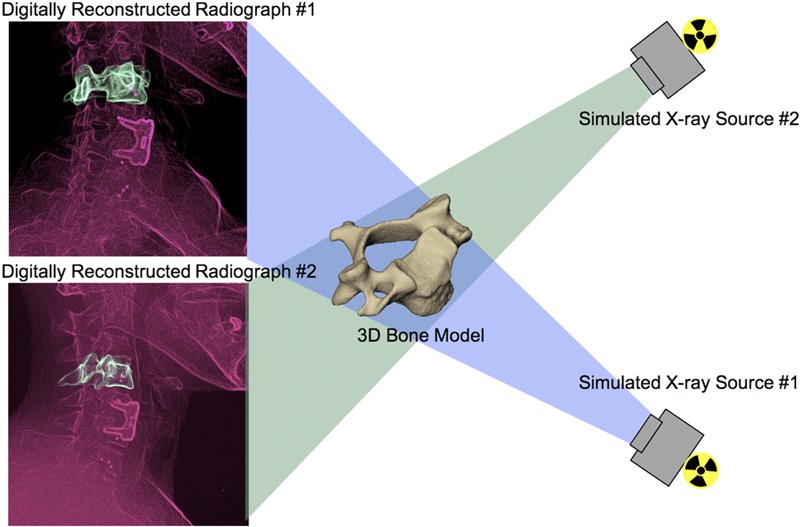
Virtual x-ray system for model-based tracking. A three-dimensional CT reconstruction of the bone was placed in a computer-generated reproduction of the x-ray system. Simulated x-rays were then passed through the three-dimensional CT reconstruction to generate digitally reconstructed radiographs. Bone position and orientation were determined by optimizing the correlation between the digitally reconstructed radiographs (green in figure) and the edge-enhanced radiographs (red in figure). (Reproduced, with permission, from: Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006 Aug;128[4]:604-9.)
Fig. 2.
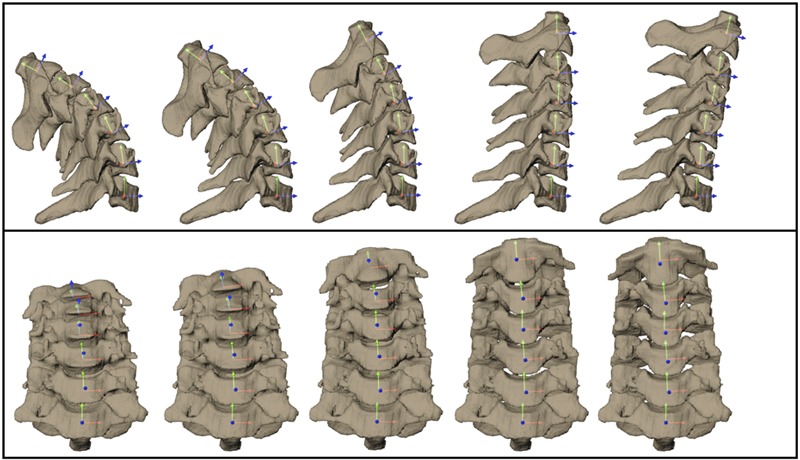
Three-dimensional bone models at five instants of the flexion cycle from a representative control subject. Sagittal views are above, and coronal views are below. Intervertebral kinematics were determined for each pair of adjacent vertebrae (superior bone motion relative to immediately inferior bone) with use of coordinate systems embedded within each vertebral body.
Analyzed Parameters
The six-degrees-of-freedom range of motion was calculated from the maximum and minimum values for each of the six kinematic parameters describing relative motion between adjacent bones (three translations and three rotations) for each motion segment for each trial (Fig. 3). The standard deviation of these range-of-motion values over all trials for a given subject defined the trial-to-trial variability. It is important to note that these maximum and minimum values may have occurred at any point of the movement cycle; they did not necessarily occur at the end of the head flexion-extension range of motion. This was especially true for parameters describing motion out of the flexion-extension plane. The maximum overall range of motion for each parameter was then calculated by finding the maximum and minimum values of each parameter over all dynamic-movement trials for a given subject (the dynamic range of motion). Intervertebral range of motion was also calculated from the static full-flexion and static full-extension images for each subject (the static range of motion). An additional measurement, termed “clinical anterior-posterior range of motion,” was calculated with use of the inferior-posterior edge of the superior vertebral body and the superior-posterior edge of the inferior vertebral body. This measurement was similar to a previous method used to quantify anterior-posterior translation as it is typically measured clinically45.
Fig. 3.
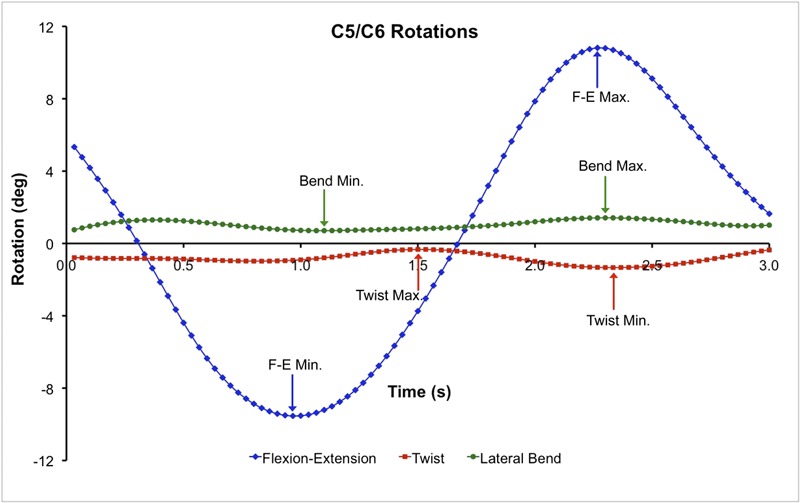
Flexion-extension (F-E), twist, and lateral bend angles between C4 and C5 for a representative subject. The arrows indicate maximum and minimum values for each curve over the entire flexion-extension trial. Maximum and minimum values for each rotation curve were determined for each cervical motion segment for each trial. The process was identical for determining translation range of motion. The symbols along the curves indicate instants when each of the ninety frames of biplane x-ray data were collected and analyzed.
Static alignment between adjacent vertebrae was determined from the static neutral trial from each subject. The maximum amount of flexion and anterior translation as well as the maximum amount of extension and posterior translation were determined relative to this static neutral position for the dynamic flexion-extension trials.
Disc height in the anterior anulus, nucleus, and posterior anulus regions was determined for each subject to assess disc degeneration. The methods used to determine disc height are provided in the Appendix.
Statistical Design and Analysis
Sample size was determined by using variability estimates from previous studies that employed CT model-based tracking and kinematic measurement techniques similar to those utilized in the current study39,41, and power was set at 0.80, so that differences between groups as small as 1.0° in rotation could be detected46. Analysis of variance was used to assess all differences between the control and arthrodesis groups. Paired t tests were performed to identify differences between static and dynamic six-degrees-of-freedom range of motion within all subjects. Significance was set at p < 0.05 for all tests, and significance levels were adjusted for multiple comparisons with use of the false discovery rate47. The p values listed in all tables were significant after adjustment for multiple comparisons.
Source of Funding
This project was funded by National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIH/NIAMS) Grant R03-AR056265 and a 21st Century Development Grant from the Cervical Spine Research Society.
Results
Specific Aim 1
Rotation Range of Motion
The dynamic range of motion in the asymptomatic controls during the flexion-extension movement was largest in the flexion-extension direction, followed by the lateral bend direction, and smallest in the twist direction at every motion segment (Table I). Significant differences between the control group and C5/C6 arthrodesis group were identified at the operatively treated motion segment, with flexion-extension range of motion significantly less in the arthrodesis group (average difference: −11.8°; 95% confidence interval [CI], −14.9° to −8.7°; p < 0.001). Twist rotation inferior to the operatively treated segment was also significantly larger (p < 0.001) in comparison with the value in the controls. The total range of motion in the flexion-extension direction did not differ significantly between the control and arthrodesis groups at any motion segment that had not been included in the operation (all p > 0.370).
TABLE I.
Rotation Range of Motion (in Degrees) During Dynamic Flexion-Extension*
| C2/C3 |
C3/C4 |
C4/C5 |
C5/C6 |
C6/C7 |
|||||||||||
| Group | Flex-Ext | Twist | Lat Bend | Flex-Ext | Twist | Lat Bend | Flex-Ext | Twist | Lat Bend | Flex-Ext | Twist | Lat Bend | Flex-Ext | Twist | Lat Bend |
| Control† | 10.2 ± 2.4 | 1.9 ± 0.8 | 2.8 ± 1.2 | 14.2 ± 2.6 | 1.9 ± 0.8 | 2.6 ± 1.4 | 15.9 ± 2.1 | 1.9 ± 0.7 | 2.8 ± 1.6 | 14.6 ± 4.7 | 1.6 ± 0.7 | 2.0 ± 0.8 | 12.5 ± 4.6 | 1.5 ± 0.5 | 2.3 ± 1.0 |
| C5/C6 arthrodesis† | N/A | N/A | N/A | 13.2 ± 3.1 | 2.1 ± 0.8 | 2.5 ± 0.9 | 16.7 ± 2.9 | 2.4 ± 0.9 | 2.7 ± 1.2 | 2.9 ± 0.9* | 2.2 ± 1.1 | 2.5 ± 1.2 | 12.6 ± 4.2 | 2.6 ± 0.9* | 3.3 ± 0.9 |
| Difference | N/A | N/A | N/A | −1.0 | 0.2 | −0.2 | 0.8 | 0.5 | 0.0 | −11.8 | 0.6 | 0.5 | 0.1 | 1.1 | 1.0 |
| 95% CI‡ | N/A | N/A | N/A | −3.2 to 1.2 | −0.5 to 0.8 | −1.1 to 0.8 | −1.1 to 2.7 | −0.2 to 1.1 | −1.2 to 1.1 | −14.9 to −8.7 | −0.1 to 1.3 | −0.2 to 1.3 | −3.5 to 3.6 | 0.5 to 1.6 | 0.2 to 1.8 |
The following significant differences between the control and arthrodesis groups were identified (marked by asterisks within the table): C5/C6 (flexion-extension): control > arthrodesis (p < 0.001) and C6/C7 (twist): control > arthrodesis (p < 0.001). N/A = not available.
The values are given as the mean and standard deviation.
The 95% confidence interval of the difference between groups.
The flexion-extension range of motion was further characterized by separating the total flexion-extension range of motion into a flexion range of motion and an extension range of motion with use of the static neutral trial as a reference. In the control group, the flexion range of motion was larger than the extension range of motion at each motion segment; however, this difference did not reach significance at any level (p = 0.096) (Table II). The distribution of the flexion and extension ranges of motion in the subjects treated with C5/C6 arthrodesis was opposite that of the controls. In the subjects treated with arthrodesis, the extension range of motion was larger than the flexion range of motion at each motion segment that had not been included in the operation. In fact, the extension range of motion at the C4/C5 motion segment was significantly greater in the C5/C6 arthrodesis group than it was in the asymptomatic control subjects (average difference: 3.8°; 95% CI, 0.9° to 6.6°; p = 0.011) while the flexion range of motion was significantly less in the C5/C6 arthrodesis group in comparison with the asymptomatic control group (average difference: −2.9°; 95% CI, −5.3° to −0.5°; p = 0.019) (Table II and Fig. 4). The overall head range of motion relative to the trunk was 40.9° ± 9.7° in flexion and 45.3° ± 12.8° in extension in the control group and 35.3° ± 8.5° and 43.5° ± 11.6°, respectively, in the arthrodesis group.
TABLE II.
Flexion and Extension Rotation Range of Motion (in Degrees) During Dynamic Flexion-Extension*
| C2/C3 |
C3/C4 |
C4/C5 |
C5/C6 |
C6/C7 |
||||||
| Group | Flex | Ext | Flex | Ext | Flex | Ext | Flex | Ext | Flex | Ext |
| Control† | 5.9 ± 2.4 | 4.2 ± 2.2 | 7.9 ± 3.6 | 6.3 ± 3.3 | 8.0 ± 2.6 | 7.9 ± 3.3 | 7.4 ± 2.9 | 7.3 ± 3.8 | 7.1 ± 3.9 | 5.4 ± 2.3 |
| C5/C6 arthrodesis† | N/A | N/A | 6.1 ± 3.1 | 7.1 ± 2.2 | 5.1 ± 3.7* | 11.7 ± 4.1* | 2.2 ± 1.1* | 0.6 ± 1.4* | 5.9 ± 3.1 | 6.7 ± 3.0 |
| Difference | N/A | N/A | −1.8 | 0.8 | −2.9 | 3.8 | −5.2 | −6.7 | −1.2 | 1.3 |
| 95% CI‡ | N/A | N/A | −4.5 to 0.9 | −1.5 to 3.2 | −5.3 to −0.5 | 0.9 to 6.6 | −7.1 to −3.2 | −9.2 to −4.1 | −4.1 to 1.7 | −1.1 to 3.6 |
No significant differences between flexion and extension ranges of motion were identified in the control group or arthrodesis group at any motion segment. The following significant differences between the control and arthrodesis groups were identified (marked by asterisks within the table): C4/C5 (extension): control < arthrodesis (p = 0.011); C4/C5 (flexion): control > arthrodesis (p = 0.019); C5/C6 (flexion): control > arthrodesis (p < 0.001); and C5/C6 (extension): control > arthrodesis (p < 0.001). N/A = not available.
The values are given as the mean and standard deviation.
The 95% confidence interval of the difference between groups.
Fig. 4.
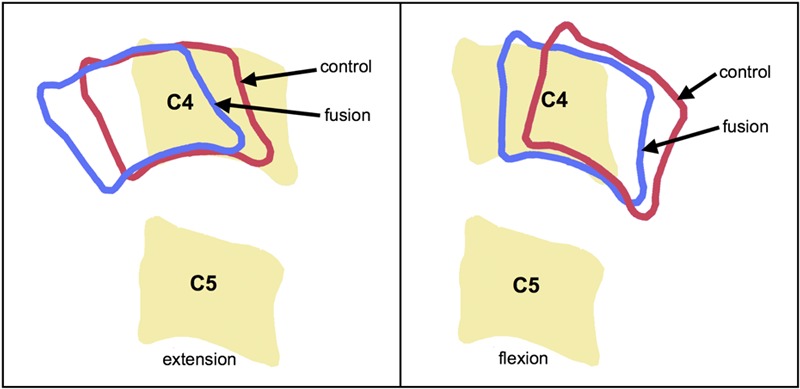
Representation of flexion-extension range of motion in the C5/C6 arthrodesis (fusion) and control groups. The neutral position of C4 and C5 are shown as solid bones, with the movement in control subjects (red) and subjects treated with arthrodesis (blue) represented by bone outlines in full extension (left) and flexion (right). The total range of motion adjacent to the arthrodesis did not differ between groups; however, the subjects treated with arthrodesis had greater extension and posterior translation range of motion at full extension and less flexion and anterior translation at full flexion.
Translation Range of Motion
The only significant difference between the control and C5/C6 arthrodesis groups in total dynamic translation range of motion was at the fused motion segment, with the anterior-posterior range of motion significantly less in the arthrodesis group (average difference: −2.6 mm; 95% CI, −3.2 to −2.0 mm; p < 0.001) (Table III). The total anterior-posterior range of motion was larger superior to the C5/C6 motion segment in comparison with the value in the controls; however, this difference did not reach significance (p = 0.063).
TABLE III.
Translation Range of Motion (in Millimeters) During Dynamic Flexion-Extension*
| C2/C3 |
C3/C4 |
C4/C5 |
C5/C6 |
C6/C7 |
|||||||||||
| Group | Med-Lat | Sup-Inf | Ant-Post | Med-Lat | Sup-Inf | Ant-Post | Med-Lat | Sup-Inf | Ant-Post | Med-Lat | Sup-Inf | Ant-Post | Med-Lat | Sup-Inf | Ant-Post |
| Control† | 0.6 ± 0.2 | 0.7 ± 0.3 | 3.8 ± 1.1 | 0.6 ± 0.4 | 0.7 ± 0.3 | 3.8 ± 0.8 | 0.6 ± 0.3 | 0.6 ± 0.3 | 3.9 ± 0.7 | 0.6 ± 0.5 | 0.6 ± 0.3 | 3.2 ± 1.3 | 0.7 ± 0.6 | 0.7 ± 0.4 | 2.4 ± 1.0 |
| C5/C6 arthrodesis† | N/A | N/A | N/A | 0.8 ± 0.3 | 0.7 ± 0.3 | 3.7 ± 0.8 | 0.7 ± 0.3 | 1.0 ± 0.5 | 4.5 ± 0.9 | 1.0 ± 0.5 | 0.7 ± 0.3 | 0.6 ± 0.3* | 1.3 ± 0.9 | 0.9 ± 0.4 | 2.9 ± 0.8 |
| Difference | N/A | N/A | N/A | 0.2 | −0.0 | −0.0 | 0.1 | 0.4 | 0.6 | 0.4 | 0.0 | −2.6 | 0.6 | 0.2 | 0.4 |
| 95% CI‡ | N/A | N/A | N/A | −0.1 to 0.5 | −0.2 to 0.2 | −0.7 to 0.6 | −0.1 to 0.4 | 0.0 to 0.8 | −0.0 to 1.2 | 0.0 to 0.8 | −0.2 to 0.3 | −3.2 to −2.0 | 0.1 to 1.1 | −0.1 to 0.5 | −0.4 to 1.2 |
The following significant difference between the control and arthrodesis groups was identified (marked by asterisk within the table): C5/C6 (anterior-posterior): control > arthrodesis (p < 0.001). N/A = not available.
The values are given as the mean and standard deviation.
The 95% confidence interval of the difference between groups.
When the total anterior-posterior range of motion was divided into an anterior range of motion and a posterior range of motion with use of the static neutral trial as a reference, trends were similar to those found in the analysis of the flexion and extension components of the total dynamic range of motion (Fig. 4 and Appendix). Specifically, anterior translation was consistently less and posterior translation was consistently greater in the C5/C6 arthrodesis group, in comparison with the controls, at each nonfused motion segment. The difference in posterior translation was significant at the C6/C7 motion segment (average difference: 0.4 mm; 95% CI, 0.0 to 0.8 mm; p = 0.016), but not at the C4/C5 motion segment after correcting for multiple comparisons (p = 0.043).
Clinical Translation Range of Motion
Intervertebral translation in the control subjects, as typically measured clinically, ranged from 1.1 to 2.3 mm, with no significant differences among levels (see Appendix). The only significant difference between the control and arthrodesis groups in terms of clinical anterior-posterior translation occurred at the fused motion segment (p < 0.001).
Trial-to-Trial Variability
Trial-to-trial variability results and discussion are provided in the Appendix.
Specific Aim 2
Static Versus Dynamic Range of Motion
The intervertebral range of motion measured during dynamic, functional movement tended to be larger than the intervertebral range of motion measured on static full-flexion and full-extension images (see Appendix). In the control subjects, the dynamic range of motion was significantly greater than the range of motion measured on static images in all three rotational and translational degrees of freedom at the C2/C3, C3/C4, and C4/C5 motion segments. The effect of measuring range of motion with images collected during active motion, as opposed to images collected with the subject stationary, was typically greater in the C5/C6 arthrodesis group than it was in the control subjects (see Appendix).
Disc Height
Disc height measurements indicated no significant differences between the control and arthrodesis groups. Details of these results are provided in the Appendix.
Discussion
No significant differences between the control and C5/C6 arthrodesis groups were identified for range of motion at the unfused cervical vertebrae in the primary directions of motion during flexion-extension (i.e., flexion-extension rotation and anterior-posterior translation). This result agrees with those of previous reports that indicated that adjacent-segment kinematics remained unchanged approximately one year after arthrodesis48,49, but they contradict those in another report that demonstrated significantly less intersegmental range of motion at “almost every level” when subjects treated with arthrodesis were compared with control subjects50. The lack of significant in vivo differences in the total range of motion between the arthrodesis and control groups contradicts in vitro studies that showed excessive motion following arthrodesis in cadaver specimens18,51-54, suggesting that in vitro test protocols may not adequately replicate in vivo loading. The small flexion-extension rotation at the C5/C6 motion segment observed in the subjects treated with C5/C6 arthrodesis consistently followed the flexion-extension patterns of adjacent vertebrae, indicating that the flexion-extension range of motion calculated in the present study represented actual motion at the operatively treated segment, and was not merely noise in the measurement system.
The results of the current study indicate that the total range of motion in secondary components of motion (i.e., twist and bend rotation as well as medial-lateral and superior-inferior translation), on average, are less than 2.8° in rotation and 0.7 mm in translation in asymptomatic subjects. Single-level anterior arthrodesis does not appear to have a clinically relevant effect on range of motion in these secondary components of total motion during the flexion-extension movement.
According to our results, single-level anterior arthrodesis appears to affect the distribution of the total flexion-extension range of motion and total anterior-posterior translation range of motion (Table II and Appendix). The absence of significant differences between the flexion and extension ranges of motion and between the anterior and posterior translation ranges of motion in the control subjects contradicts a previous study that demonstrated significant differences between anterior and posterior translation in control subjects27. The current study is the first to compare flexion and extension components of rotation and anterior and posterior components of translation in control and arthrodesis groups. The significant alteration in the balance between flexion and extension range of motion and between anterior and posterior translation range of motion adjacent to the arthrodesis revealed a kinematic difference between the arthrodesis and control groups and suggests that it may be advantageous to evaluate range of motion clinically by measuring it from neutral to full flexion and from neutral to full extension, rather than with the current standard of full extension to full flexion. It is not clear if the observed kinematic differences in the arthrodesis group modify disc stress and pressure enough to effect disc homeostasis55-58 and lead to disc degeneration.
Clinical anterior-posterior translation in the control subjects was well below the standard of 3.5 mm to indicate excessive translation or pathology59. The 3.5-mm standard, determined in experiments on cadaver specimens, agrees well with the current in vivo data that showed that the upper boundary for the 95% confidence interval for anterior-posterior translation range of motion was 3.45 mm at the motion segments with the greatest anterior-posterior translation range of motion (C3/C4 and C4/C5). However, the present data also suggest that the standard anterior-posterior translation measurement used to identify excessive translation is level-dependent, with 2.3 mm being the upper boundary for the 95% confidence interval for the anterior-posterior translation range of motion at the C6/C7 motion segment.
The results of this study indicate that range-of-motion measurements performed with use of only static end-range-of-motion images significantly underestimate the six-degrees-of-freedom range of motion in the cervical spine. The present results confirm a previous suggestion that there may be differences between static and dynamic measurements of range of motion26. Single end-range images obtained during either static positioning or dynamic movement underestimate the range of motion because of muscular and inertial force differences between static and dynamic conditions and because all motion segments do not reach their maximum range of motion simultaneously. Furthermore, as has been previously demonstrated, static cervical flexion-extension range of motion may be increased by an average of 2° to 3° per motion segment by manually applying force to the head24, suggesting a potential for additional range of motion beyond standard flexion-extension views. The clinical implication of this finding is that range of motion measured from static full-flexion and static full-extension images of patients who have undergone an arthrodesis should be interpreted with the understanding that these measurements may underestimate the functional flexion-extension range of motion by up to 3° at each vertebral level.
There were several limitations associated with this study. First, dynamic, functional movement testing was not performed on the subjects before the C5/C6 arthrodesis because they had pain and limited movement prior to the surgery. As a result, the data for the arthrodesis group were compared with those for control subjects of approximately the same age. It is important to note that the subjects in the arthrodesis group were tested approximately seven months after the surgery, earlier than adjacent-segment disease generally occurs7. Therefore, while the present results provide valuable information regarding the short-term effects of arthrodesis, they may not be representative of longer-term effects. One benefit of this short-term data, however, is that, if kinematic differences are observed after longer-term follow-up, it will be clear which kinematic changes occurred soon after surgery and which changes developed over a longer time period.
An additional limitation of the study is that the age range of the subjects treated with arthrodesis (and therefore of the age-matched controls as well) was relatively narrow for this investigation. Although this age group is highly relevant from a clinical perspective, the results presented here should be considered to be representative only for the age group included in this cohort and with consideration of the well-known changes that occur in the spine with age12,55,60,61. The percentages of smokers in the control and arthrodesis groups were slightly lower and slightly higher, respectively, than the percentage of smokers in large clinical trials involving subjects treated with anterior arthrodesis or arthroplasty (32% to 45% rates of smokers)8,12,62. Additional study involving a larger number of patients will be necessary to determine if a relationship exists between smoking and cervical kinematics following arthrodesis. Although no significant group differences in either the total flexion-extension range of motion or the total anterior-posterior translation range of motion were identified in this study, other kinematic differences such as the instant center of rotation24,26,63 and the sequencing of the intervertebral rotations64,65 may exist between controls and subjects treated with single-level arthrodesis. Furthermore, measurements of total range of motion may not even be the appropriate parameters to characterize the mechanical effects of arthrodesis on subsequent disc degeneration because end-range-of-motion positions are encountered much less frequently than mid-range-of-motion positions during activities of daily living. Thus, additional and alternative kinematic measurements may prove more effective in identifying mechanical factors that lead to disc degeneration following arthrodesis. Finally, the range-of-motion results presented here are limited to the flexion-extension movement. The effect of C5/C6 arthrodesis on range of motion during twisting and bending rotations may or may not follow the patterns described here.
Appendix
A table showing subject demographic and surgical details; tables showing anterior and posterior translation range of motion, clinical anterior-posterior translation range of motion, differences between dynamic and static ranges of motion, and trial-to-trial variability in range of motion during dynamic flexion-extension; and a table showing disc height by vertebral level and anatomic location are available with the online version of this article as a data supplement at jbjs.org. Also available with the online version of this article as a data supplement at jbjs.org are figures demonstrating disc regions and measurement of disc height. In addition, a description of disc height calculations, trial-to-trial variability results, and disc height results along with a trial-to-trial variability discussion are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
A table showing subject demographic and surgical details; tables showing anterior and posterior translation range of motion, clinical anterior-posterior translation range of motion, differences between dynamic and static ranges of motion, and trial-to-trial variability in range of motion during dynamic flexion-extension; and a table showing disc height by vertebral level and anatomic location. Also figures demonstrating disc regions and measurement of disc height. In addition, a description of disc height calculations, trial-to-trial variability results, and disc height results along with a trial-to-trial variability discussion
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Hunter LY, Braunstein EM, Bailey RW. Radiographic changes following anterior cervical fusion. Spine (Phila Pa 1976). 1980 Sep-Oct;5(5):399-401 [DOI] [PubMed] [Google Scholar]
- 2.Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976). 1993 Nov;18(15):2167-73 [DOI] [PubMed] [Google Scholar]
- 3.Gore DR, Sepic SB. Anterior discectomy and fusion for painful cervical disc disease. A report of 50 patients with an average follow-up of 21 years. Spine (Phila Pa 1976). 1998 Oct 1;23(19):2047-51 [DOI] [PubMed] [Google Scholar]
- 4.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999 Apr;81(4):519-28 [DOI] [PubMed] [Google Scholar]
- 5.Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, Van Calenbergh F, van Loon J. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004 Apr;17(2):79-85 [DOI] [PubMed] [Google Scholar]
- 6.Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004 Nov-Dec;4(6):624-8 [DOI] [PubMed] [Google Scholar]
- 7.Kulkarni V, Rajshekhar V, Raghuram L. Accelerated spondylotic changes adjacent to the fused segment following central cervical corpectomy: magnetic resonance imaging study evidence. J Neurosurg. 2004 Jan;100(1 Suppl Spine):2-6 [DOI] [PubMed] [Google Scholar]
- 8.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993 Sep;75(9):1298-307 [DOI] [PubMed] [Google Scholar]
- 9.Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine (Phila Pa 1976). 1984 Oct;9(7):667-71 [DOI] [PubMed] [Google Scholar]
- 10.Watters WC, 3rd, Levinthal R. Anterior cervical discectomy with and without fusion. Results, complications, and long-term follow-up. Spine (Phila Pa 1976). 1994 Oct 15;19(20):2343-7 [DOI] [PubMed] [Google Scholar]
- 11.Hilibrand AS, Yoo JU, Carlson GD, Bohlman HH. The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine (Phila Pa 1976). 1997 Jul 15;22(14):1574-9 [DOI] [PubMed] [Google Scholar]
- 12.Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Hashimoto T, Takahata T. Age-related changes of thoracic and cervical intervertebral discs in asymptomatic subjects. Spine (Phila Pa 1976). 2010 Jun 15;35(14):1359-64 [DOI] [PubMed] [Google Scholar]
- 13.Fuller DA, Kirkpatrick JS, Emery SE, Wilber RG, Davy DT. A kinematic study of the cervical spine before and after segmental arthrodesis. Spine (Phila Pa 1976). 1998 Aug 1;23(15):1649-56 [DOI] [PubMed] [Google Scholar]
- 14.Song KJ, Choi BW, Jeon TS, Lee KB, Chang H. Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. Eur Spine J. 2011 Nov;20(11):1940-5 Epub 2011 Jun 8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fielding JW. Normal and selected abnormal motion of the cervical spine from the second cervical vertebra to the seventh cervical vertebra based on cineroentgenography. J Bone Joint Surg Am. 1964 Dec;46:1779-81 [PubMed] [Google Scholar]
- 16.Dunsker SB, Colley DP, Mayfield FH. Kinematics of the cervical spine. Clin Neurosurg. 1978;25:174-83 [DOI] [PubMed] [Google Scholar]
- 17.Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976). 1999 Apr 1;24(7):670-5 [DOI] [PubMed] [Google Scholar]
- 18.Schwab JS, Diangelo DJ, Foley KT. Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine (Phila Pa 1976). 2006 Oct 1;31(21):2439-48 [DOI] [PubMed] [Google Scholar]
- 19.Bakke S. Röntgenologische beobachtungen über die bewegungen der halswirbelsaule. Acta Radiol [Suppl] (Stockh). 1931;13 [Google Scholar]
- 20.Buetti-Bäuml C. Funktionelle Röntgendiagnostik der Halswirbelsaule. Fortschritte auf dem Gebiete der Röentgenstrahlen vereinigt mit Röentgenpraxis. Ergänzungsband. Stuttgart: Georg Thieme;1954. p 70.
- 21.de Sèze C, Djian A, Abdelmaola M. Etude radiologique de la dynamique cervicale dans le plain sagittal. (Une contribution radiophysiologique a l’étude pathogenique des artheoses cervicales). Revue du Rhumatisme. 1951;18:37-46 [PubMed] [Google Scholar]
- 22.Penning L, Functioneel rontgenonderzoek Bij degenerative en traumatische afwijkingen der laag-cervicale bewegingssegmenten. Gronigen, The Netherlands: University of Groningen; 1960
- 23.White AA, 3rd, Panjabi MM. The basic kinematics of the human spine. A review of past and current knowledge. Spine (Phila Pa 1976). 1978 Mar;3(1):12-20 [DOI] [PubMed] [Google Scholar]
- 24.Dvorak J, Froehlich D, Penning L, Baumgartner H, Panjabi MM. Functional radiographic diagnosis of the cervical spine: flexion/extension. Spine (Phila Pa 1976). 1988 Jul;13(7):748-55 [DOI] [PubMed] [Google Scholar]
- 25.Frobin W, Leivseth G, Biggemann M, Brinckmann P. Sagittal plane segmental motion of the cervical spine. A new precision measurement protocol and normal motion data of healthy adults. Clin Biomech (Bristol, Avon). 2002 Jan;17(1):21-31 [DOI] [PubMed] [Google Scholar]
- 26.Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon). 2000 Nov;15(9):633-48 [DOI] [PubMed] [Google Scholar]
- 27.Wu SK, Kuo LC, Lan HC, Tsai SW, Chen CL, Su FC. The quantitative measurements of the intervertebral angulation and translation during cervical flexion and extension. Eur Spine J. 2007 Sep;16(9):1435-44 Epub 2007 Apr 27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reitman CA, Mauro KM, Nguyen L, Ziegler JM, Hipp JA. Intervertebral motion between flexion and extension in asymptomatic individuals. Spine (Phila Pa 1976). 2004 Dec 15;29(24):2832-43 [DOI] [PubMed] [Google Scholar]
- 29.Simpson AK, Biswas D, Emerson JW, Lawrence BD, Grauer JN. Quantifying the effects of age, gender, degeneration, and adjacent level degeneration on cervical spine range of motion using multivariate analyses. Spine (Phila Pa 1976). 2008 Jan 15;33(2):183-6 [DOI] [PubMed] [Google Scholar]
- 30.Mimura M, Moriya H, Watanabe T, Takahashi K, Yamagata M, Tamaki T. Three-dimensional motion analysis of the cervical spine with special reference to the axial rotation. Spine (Phila Pa 1976). 1989 Nov;14(11):1135-9 [DOI] [PubMed] [Google Scholar]
- 31.Iai H, Moriya H, Goto S, Takahashi K, Yamagata M, Tamaki T. Three-dimensional motion analysis of the upper cervical spine during axial rotation. Spine (Phila Pa 1976). 1993 Dec;18(16):2388-92 [DOI] [PubMed] [Google Scholar]
- 32.Ishii T, Mukai Y, Hosono N, Sakaura H, Fujii R, Nakajima Y, Tamura S, Sugamoto K, Yoshikawa H. Kinematics of the subaxial cervical spine in rotation in vivo three-dimensional analysis. Spine (Phila Pa 1976). 2004 Dec 15;29(24):2826-31 [DOI] [PubMed] [Google Scholar]
- 33.Ishii T, Mukai Y, Hosono N, Sakaura H, Fujii R, Nakajima Y, Tamura S, Iwasaki M, Yoshikawa H, Sugamoto K. Kinematics of the cervical spine in lateral bending: in vivo three-dimensional analysis. Spine (Phila Pa 1976). 2006 Jan 15;31(2):155-60 [DOI] [PubMed] [Google Scholar]
- 34.Goel VK, Pope MH. Biomechanics of fusion and stabilization. Spine (Phila Pa 1976). 1995 Dec 15;20(24 Suppl):85S-99S [PubMed] [Google Scholar]
- 35.Van Mameren H, Drukker J, Sanches H, Beursgens J. Cervical spine motion in the sagittal plane (I) range of motion of actually performed movements, an X-ray cinematographic study. Eur J Morphol. 1990;28(1):47-68 [PubMed] [Google Scholar]
- 36.Thorhauer E, Miyawaki M, Illingworth K, Holmes A, Anderst B. Accuracy of bone and cartilage models obtained from CT and MRI. Poster presented at the 34th Annual Meeting of the American Society of Biomechanics; 2010 Aug 18-21; Providence, RI. Poster no. 68.
- 37.Treece G, Prager RW, Gee AH. Regularized marching tetrahedra: improved iso-surface extraction. Computers and Graphics. 1999;23: 583-598 [Google Scholar]
- 38.Anderst WJ, Baillargeon E, Donaldson WF, 3rd, Lee JY, Kang JD. Validation of a noninvasive technique to precisely measure in vivo three-dimensional cervical spine movement. Spine (Phila Pa 1976). 2011 Mar 15;36(6):E393-400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006 Aug;128(4):604-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martin DE, Greco NJ, Klatt BA, Wright VJ, Anderst WJ, Tashman S. Model-based tracking of the hip: implications for novel analyses of hip pathology. J Arthroplasty. 2011 Jan;26(1):88-97 Epub 2010 Mar 26 [DOI] [PubMed] [Google Scholar]
- 41.Anderst W, Zauel R, Bishop J, Demps E, Tashman S. Validation of three-dimensional model-based tibio-femoral tracking during running. Med Eng Phys. 2009 Jan;31(1):10-6 Epub 2008 Apr 23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Winter DA. Biomechanics and motor control of human movement. 4th ed. Hoboken, NJ: Wiley; 2009 [Google Scholar]
- 43.Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D'Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I; Standardization and Terminology Committee of the International Society of Biomechanics ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion–part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech. 2002 Apr;35(4):543-8 [DOI] [PubMed] [Google Scholar]
- 44.Kane T, Likins P, Leivseth G. Spacecraft dynamics. New York: McGraw-Hill; 1983 [Google Scholar]
- 45.Park DK, Lin EL, Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion: in vivo quantitative radiographic analysis. Spine (Phila Pa 1976). 2011 Apr 20;36(9):721-30 [DOI] [PubMed] [Google Scholar]
- 46.Pagano R. Understanding statistics in the behavioral sciences. 3rd ed. New York: West Publishing Co; 1990 [Google Scholar]
- 47.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc Series B. 1995;57(1):289-300 [Google Scholar]
- 48.Kolstad F, Nygaard ØP, Leivseth G. Segmental motion adjacent to anterior cervical arthrodesis: a prospective study. Spine (Phila Pa 1976). 2007 Mar 1;32(5):512-7 [DOI] [PubMed] [Google Scholar]
- 49.Reitman CA, Hipp JA, Nguyen L, Esses SI. Changes in segmental intervertebral motion adjacent to cervical arthrodesis: a prospective study. Spine (Phila Pa 1976). 2004 Jun 1;29(11):E221-6 [DOI] [PubMed] [Google Scholar]
- 50.Liu F, Cheng J, Komistek RD, Mahfouz MR, Sharma A. In vivo evaluation of dynamic characteristics of the normal, fused, and disc replacement cervical spines. Spine (Phila Pa 1976). 2007 Nov 1;32(23):2578-84 [DOI] [PubMed] [Google Scholar]
- 51.Finn MA, Brodke DS, Daubs M, Patel A, Bachus KN. Local and global subaxial cervical spine biomechanics after single-level fusion or cervical arthroplasty. Eur Spine J. 2009 Oct;18(10):1520-7 Epub 2009 Jul 8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976). 2002 Nov 15;27(22):2431-4 [DOI] [PubMed] [Google Scholar]
- 53.Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine (Phila Pa 1976). 2005 May 15;30(10):1165-72 [DOI] [PubMed] [Google Scholar]
- 54.DiAngelo DJ, Roberston JT, Metcalf NH, McVay BJ, Davis RC. Biomechanical testing of an artificial cervical joint and an anterior cervical plate. J Spinal Disord Tech. 2003 Aug;16(4):314-23 [DOI] [PubMed] [Google Scholar]
- 55.Benoist M. Natural history of the aging spine. Eur Spine J. 2003 Oct;12 Suppl 2:S86-9 Epub 2003 Sep 5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Adams MA, Dolan P, McNally DS. The internal mechanical functioning of intervertebral discs and articular cartilage, and its relevance to matrix biology. Matrix Biol. 2009 Sep;28(7):384-9 Epub 2009 Jul 5 [DOI] [PubMed] [Google Scholar]
- 57.Urban JP, Holm S, Maroudas A, Nachemson A. Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res. 1977 Nov-Dec;(129):101-14 [PubMed] [Google Scholar]
- 58.Urban JP, Holm S, Maroudas A, Nachemson A. Nutrition of the intervertebral disc: effect of fluid flow on solute transport. Clin Orthop Relat Res. 1982 Oct;(170):296-302 [PubMed] [Google Scholar]
- 59.White AA, 3rd, Johnson RM, Panjabi MM, Southwick WO. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res. 1975;(109):85-96 [DOI] [PubMed] [Google Scholar]
- 60.Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990 Sep;72(8):1178-84 [PubMed] [Google Scholar]
- 61.Ferguson SJ, Steffen T. Biomechanics of the aging spine. Eur Spine J. 2003 Oct;12 Suppl 2:S97-S103 Epub 2003 Sep 9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nunley PD, Jawahar A, Kerr EJ, 3rd, Gordon CJ, Cavanaugh DA, Birdsong EM, Stocks M, Danielson G. Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2-to 4-year follow-up of 3 prospective randomized trials. Spine (Phila Pa 1976). 2012 Mar 15;37(6):445-51 [DOI] [PubMed] [Google Scholar]
- 63.Amevo B, Aprill C, Bogduk N. Abnormal instantaneous axes of rotation in patients with neck pain. Spine (Phila Pa 1976). 1992 Jul;17(7):748-56 [DOI] [PubMed] [Google Scholar]
- 64.Wu SK, Kuo LC, Lan HC, Tsai SW, Su FC. Segmental percentage contributions of cervical spine during different motion ranges of flexion and extension. J Spinal Disord Tech. 2010 Jun;23(4):278-84 [DOI] [PubMed] [Google Scholar]
- 65.Hino H, Abumi K, Kanayama M, Kaneda K. Dynamic motion analysis of normal and unstable cervical spines using cineradiography. An in vivo study. Spine (Phila Pa 1976). 1999 Jan 15;24(2):163-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
A table showing subject demographic and surgical details; tables showing anterior and posterior translation range of motion, clinical anterior-posterior translation range of motion, differences between dynamic and static ranges of motion, and trial-to-trial variability in range of motion during dynamic flexion-extension; and a table showing disc height by vertebral level and anatomic location. Also figures demonstrating disc regions and measurement of disc height. In addition, a description of disc height calculations, trial-to-trial variability results, and disc height results along with a trial-to-trial variability discussion


