Abstract
Background:
Some of the poor functional outcomes of knee arthroplasty may be due to pain in the contralateral, unreplaced knee. We investigated the relationship between the preoperative pain status of the contralateral knee and the risk of a poor postoperative functional outcome in patients who underwent knee arthroplasty.
Methods:
We analyzed data on 271 patients in the Multicenter Osteoarthritis Study who had undergone knee arthroplasty since the time of enrollment. Eighty-six percent of these patients were white, 72% were female, and the mean age was sixty-seven years. The severity of pain in the knee contralateral to the one that was replaced was measured before the knee arthroplasty with use of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain scale, with the scores being grouped into four categories (0, 1 to 4, 5 to 9, and 10 to 20). Poor post-arthroplasty function six months or more after surgery was determined with use of the Patient Acceptable Symptom State (PASS) outcome tool and a clinical performance measure of walking speed. We evaluated the relationship between contralateral pain severity and the functional outcomes with use of Poisson regression.
Results:
Seventy-two (27%) of 264 patients demonstrated poor post-arthroplasty function by failing to attain the threshold PASS score, and seventy-six (30%) of 250 subjects had a slow walking speed. As the pre-arthroplasty pain in the contralateral knee increased, there was a steady increase in the proportion with poor post-arthroplasty function (p < 0.0001 for PASS and p = 0.04 for slow walking speed). Compared with patients who had no pre-arthroplasty pain in the contralateral knee, those in the highest category of contralateral pain severity had 4.1 times the risk (95% confidence interval, 1.5 to 11.5) of having poor self-reported post-arthroplasty function. Patients in whom both knees had been replaced at the time of outcome collection were less likely to have poor self-reported function than those in whom only one knee had been replaced.
Conclusions:
Preoperative pain in the contralateral knee is strongly associated with self-reported post-arthroplasty functional outcome and may therefore be a useful indicator of prognosis or a potential target of perioperative intervention.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
Knee arthroplasty is a widely accepted surgical intervention for the treatment of end-stage knee osteoarthritis, with an increasing incidence1. Although most patients have improvements in terms of pain and function following knee arthroplasty2,3, a substantial number do not. Studies generally have indicated that between 10% and 30% of patients continue to have functional limitations following knee arthroplasty4,5. However, the risk factors for a lack of improvement are not fully understood.
As a large proportion of patients who undergo knee arthroplasty for the treatment of end-stage osteoarthritis have concurrent osteoarthritis in the other knee6, the pre-arthroplasty status of the contralateral knee may be related to a patient’s function after knee arthroplasty. Studies of pre-arthroplasty predictors of post-arthroplasty function have not examined the impact of contralateral knee symptoms, although a few recent studies have demonstrated that post-arthroplasty factors in the contralateral knee, such as strength7 and pain8, are associated with post-arthroplasty function. As some of the effects of post-arthroplasty contralateral knee symptoms on function may be due to contralateral impairments that developed as a consequence of surgery, increasing the demand on the contralateral knee, it is important to study both the pre-arthroplasty status and the post-arthroplasty status of the contralateral knee. This may inform both pre-arthroplasty decision-making and prognosis and also allow for an understanding of the effects of the contralateral knee on post-arthroplasty function, aside from those induced by the surgery itself.
The purposes of the present study were to determine the prevalence of poor post-arthroplasty function among patients managed with unilateral and/or bilateral knee arthroplasty and to investigate the relationship between preoperative pain in the contralateral knee, whether previously replaced or not, and the postoperative functional status. We conducted our analyses on participants in a large multicenter prospective study of patients who had, or were at risk for, knee osteoarthritis; this prospective study involves the collection of clinical and performance-based data and has followed subjects for over five years.
Materials and Methods
Study Population
The Multicenter Osteoarthritis Study (MOST) is a prospective cohort study of 3026 individuals with an age of fifty to seventy-nine years at the time of enrollment who had, or were at risk for, knee osteoarthritis. Participants in the MOST study were recruited with direct methods from Birmingham, Alabama, and Iowa City, Iowa. Details on the study population have been published elsewhere9. Individuals who had symptomatic osteoarthritis of the knee or who were considered to be at high risk for the development of osteoarthritis (those who were overweight or obese and those with knee pain, aching, or stiffness on most of the previous thirty days; a history of knee injury that made it difficult to walk for at least one week; or previous knee surgery) were included. The MOST study excluded individuals with bilateral knee arthroplasty at the time of enrollment, a history of cancer other than non-melanoma skin cancer, several rheumatological conditions (rheumatoid arthritis, psoriatic arthritis, anklyosing spondylitis, and reactive arthritis), an inability to walk without the assistance of a walker or another person, or plans to move out of the study area in the next three years. We analyzed the subset of subjects who had at least one knee arthroplasty between the time of enrollment and the sixty-month clinic visit. Knee arthroplasties included primary unicompartmental or total joint arthroplasties. We only included subjects who had had a clinic visit at least six months after the knee arthroplasty in order to allow for recovery from surgery prior to outcome collection. There were 271 subjects in the MOST study who met our inclusion criteria (Fig. 1).
Fig. 1.
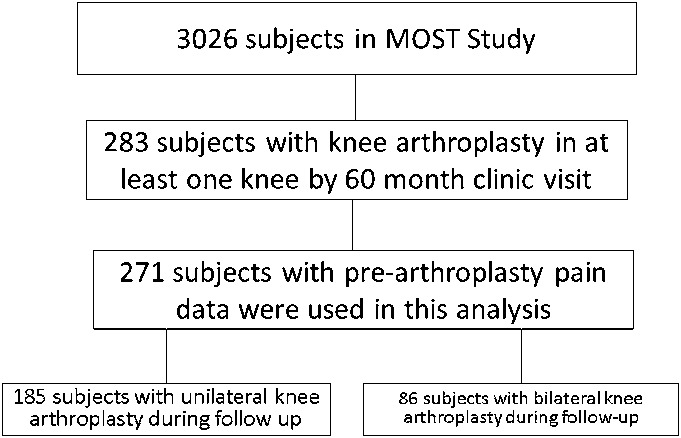
Flow chart showing the study sample origination.
Assessment of Poor Function
Post-arthroplasty function was assessed at the thirty-month and sixty-month follow-up visits with use of both a measure of clinical performance and a modified self-reported measure.
Performance Measure
The clinical performance measure of walking speed was calculated from the time it took the participants to walk 20 m at their usual pace. Speeds of <1 meter per second (m/s) were considered to be definitive of poor function on the basis of previous literature on the association of walking speed with morbidity and mortality10,11.
Self-Reported Measure
We used a recently described outcome measure, the Patient Acceptable Symptom State (PASS), for the evaluation of function after knee arthroplasty12. The original PASS score was calculated with use of the reverse option of the Western Ontario and McMaster Universities Index-Physical Function subscale (WOMAC-PF)13 and was based on a 100-point scale; thus, we back-calculated to arrive at our threshold PASS score for knee arthroplasty of <22 (of 68). The WOMAC-PF is a seventeen-item patient-specific questionnaire with which each functional activity is scored on an ordinal scale from 0 (no difficulty) to 4 (severe difficulty), with a maximum score of 68 indicating the most functional impairment.
Assessment of Knee Arthroplasty Status
Unicompartmental or total joint arthroplasties that were self-reported at clinic visits at baseline, thirty months, or sixty months or by telephone fifteen months after baseline were included in the present study. More than 95% of the arthroplasties were confirmed on the basis of medical records and/or knee radiographs that were made after surgery. Only knee arthroplasties that occurred after enrollment in the study cohort were included.
Contralateral Knee Pain at Baseline
Knee pain in the contralateral knee was measured with the WOMAC pain scale13 at baseline. The WOMAC pain scale consists of five functional tasks for which the subject reports pain on a 0 to 4-point Likert scale: (1) walking, (2) going up and down stairs, (3) being in bed, (4) sitting or lying, and (5) standing. The scores for all tasks are added, for a total score ranging from 0 to 20 (with a score of 20 indicating maximum pain). We grouped the contralateral WOMAC pain level into four categories: 0, 1 to 4, 5 to 9, and ≥10.
Statistical Methods
For all analyses, we classified each participant as having unilateral or bilateral knee arthroplasty. Any participant who had only one knee replaced since baseline was classified as having unilateral knee arthroplasty. Participants with a knee arthroplasty in both knees during the follow-up period (concurrent or not) were classified as having bilateral knee arthroplasty.
Descriptive Analyses
When determining post-arthroplasty function, we used data from the first post-arthroplasty visit that had occurred at least six months following knee arthroplasty to allow for adequate surgical recovery. We analyzed the available data for the overall group, the unilateral arthroplasty group, and the bilateral arthroplasty group to determine (1) the percentage of subjects in each group who did not attain the threshold PASS score and (2) the percentage of subjects in each group who had slow walking speed. For those with bilateral knee arthroplasty, the functional status following the second knee arthroplasty was used. Differences between the unilateral and bilateral arthroplasty groups with respect to the proportion of subjects with poor function were evaluated with use of the Cochran-Mantel-Haenszel test. In the unilateral knee arthroplasty group, we tested for linear trend for the association of the pre-arthroplasty contralateral knee pain category with both definitions of poor function.
Multivariable Analysis
We performed multivariable analyses of the association between pre-arthroplasty contralateral knee pain and post-arthroplasty function for the 185 unilateral knee arthroplasties that were done after the baseline assessment. We estimated risk ratios and 95% confidence intervals for the effect of pre-arthroplasty contralateral knee pain on post-arthroplasty function with use of Poisson regression. We adjusted for the age at the time of knee arthroplasty, sex, race, educational attainment, depressive symptoms, pre-arthroplasty body mass index (BMI), a modified Charlson comorbidity index14, the presence of pain in the back and other joints (indicated on a body pain map), and the time from knee arthroplasty to outcome assessment in all longitudinal analyses. The reference group in both analyses was that with a WOMAC pain score of 0 (of 20) in the contralateral knee.
The MOST study protocol was approved by the institutional review boards at the University of Iowa; University of Alabama, Birmingham; University of California, San Francisco; and Boston University Medical Center. Statistical analyses were completed with use of SAS software (version 9.1; SAS, Cary, North Carolina).
Source of Funding
The MOST study is supported by National Institutes of Health (NIH) and National Institute on Aging (NIA) grants U01 AG18820, U01 AG18832, U01 AG18947, U01AG19069 and provided the recruitment and data collection for the subjects used in this analysis.
Results
Basic demographic and clinical data on the study sample are provided in Table I. The mean time (and standard deviation) between knee arthroplasty and all outcome assessments was 22 ± 11.5 months. One hundred and eighty-five subjects (68%) had unilateral knee arthroplasty, and eighty-six (32%) had bilateral knee arthroplasty. Of the patients who had bilateral knee arthroplasty, 27% had concurrent knee arthroplasty whereas the remainder had both knees replaced at different times during follow-up (staged knee arthroplasties). The contralateral knee for the subjects who had unilateral arthroplasty had a pre-arthroplasty mean WOMAC pain score of 4.2 ± 4.1 (of 20) and a median Kellgren-Lawrence score of 2 (with 25% having a score of ≥3 and 25% having a score of ≤1 [no radiographic evidence of osteoarthritis]).
TABLE I.
Demographic and Clinical Characteristics of Study Sample
| Female (%) | 72.1 |
| White (%) | 86.3 |
| Age at time of knee arthroplasty* (yr) | 67 ± 7.5 |
| Baseline hip pain (%) | |
| Pain in one hip | 16 |
| Pain in two hips | 18 |
| Baseline lower limb/back pain† (%) | 64 |
| Pre-arthroplasty findings* | |
| Kellgren-Lawrence grade (osteoarthritis severity) in contralateral knee‡ | 2.0 ± 1.4 |
| Walk time (s) | 19.7 ± 4.5 |
| WOMAC physical function score (points) | 27.1 ± 11.1 |
| Contralateral WOMAC pain score (points) | 4.2 ± 4.1 |
| Contralateral flexion contracture (deg) | 9.6 |
| Post-arthroplasty ipsilateral WOMAC pain score (points) | 3.6 ± 3.7 |
The values are given as the mean, with or without the standard deviation.
Pain present in at least one hip, ankle, or foot or in the upper, middle, or lower part of back. ‡Possible range, 0 to 4.
Proportion of Subjects with Poor Postoperative Function
The proportions of subjects with poor WOMAC function and slow walking speed according to the number of knees replaced are displayed in Table II. Subjects with bilateral knee arthroplasty were less likely to have poor function, defined as not attaining the threshold PASS score, than those with only one knee replaced (p = 0.0003); however, there was no difference in the likelihood of having slow walking speed (p = 0.36).
TABLE II.
Proportions with Poor Post-Arthroplasty Function According to Number of Knees Replaced
| Did Not Attain Threshold PASS Score | Slow Walking Speed | |
| Total | 27% (72 of 264*) | 30% (76 of 250*) |
| Unilateral | 34% (61 of 179) | 32% (58 of 181) |
| Bilateral | 13% (11 of 85) | 26% (18 of 69) |
The n values are different because of differences in the number of knees with available data for each outcome.
Effect of Preoperative Pain in the Contralateral Knee on Poor Function
Data on pre-arthroplasty pain in the native contralateral knee were available for the 185 knees that underwent unilateral knee replacement; of these, 179 had PASS data and 181 had walking speed data. Sixty-one (34%) of 179 knees had poor post-arthroplasty function as determined with the modified PASS score, and fifty-eight (32%) of the 181 knees had poor post-arthroplasty function as demonstrated by a slow walking speed. As the pre-arthroplasty pain in the contralateral knee increased, there was a steady increase in the proportion with poor post-arthroplasty function (p value for trend, <0.0001 for PASS and 0.04 for walking speed) among those with unilateral knee arthroplasty (Fig. 2).
Fig. 2.
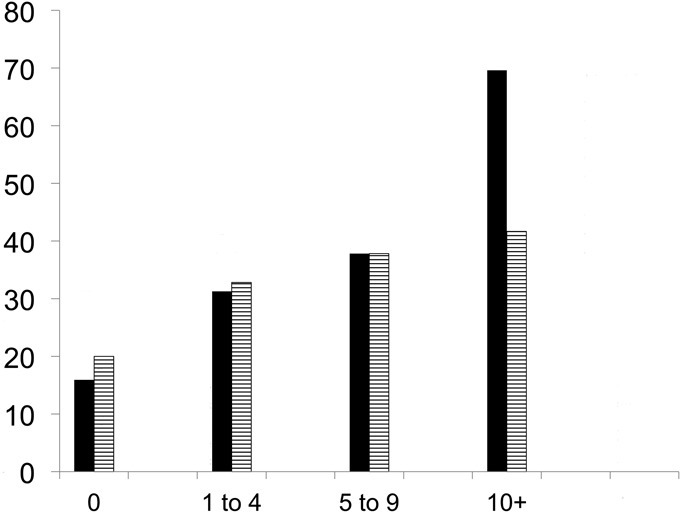
Bar graph showing the proportion of subjects with poor post-arthroplasty function according to pre-arthroplasty contralateral knee pain. The y axis shows the proportion (percentage) with poor function, and the x axis shows the pre-arthroplasty contralateral knee pain category. The black bars indicate the proportion that did not achieve the threshold PASS score (p value for trend, <0.0001), and the striped bars indicate the proportion with a slow walking speed (p value for trend, 0.04).
Multivariable Analysis
Table III presents the results of the multivariable analysis for the associations between pre-arthroplasty pain in the contralateral knee and post-arthroplasty function and walking speed. For the highest pain severity category (present in 13% [twenty-four] of 185 subjects), the relative risk of not attaining the threshold PASS score was four times that for those with no contralateral knee pain (RR [risk ratio], 4.1; 95% confidence interval [CI], 1.5 to 11.5). There was no significant multivariate association between the category of pre-arthroplasty pain in the contralateral knee and slow walking speed (RR, 1.9; 95% CI, 0.6 to 5.9). After further adjusting for the presence of back or other lower extremity joint pain (excluding knees), the risk ratio of not attaining the threshold PASS score was 3.2 (95% CI, 1.2 to 8.4).
TABLE III.
Association of Pre-Arthroplasty Contralateral Knee Pain with Poor Post-Arthroplasty Function*
| Pre-Arthroplasty Contralateral Pain Score† | Not Attaining Threshold PASS Score‡ | Slow Walking Speed‡ |
| 0 | Reference | Reference |
| 1 to 4 | 1.8 (0.7 to 4.2) | 1.3 (0.5 to 2.9) |
| 5 to 9 | 2.1 (0.8 to 5.1) | 1.3 (0.6 to 3.0) |
| 10+ | 4.1 (1.5 to 11.5) | 1.9 (0.6 to 5.9) |
Adjusted for sex, body mass index, age at the time of knee arthroplasty, educational attainment, race, depressive symptoms, number of comorbidities, and time before or after knee replacement.
Maximum score = 20.
The values are given as the risk ratio, with the 95% CI in parentheses.
Discussion
We found that moderate to severe pre-arthroplasty contralateral knee pain was associated with an increased likelihood of poor post-arthroplasty self-reported function, specifically, not attaining the threshold PASS score for function. In addition, subjects in our sample with unilateral knee arthroplasty had a higher likelihood of poor post-arthroplasty functional outcomes compared with those with bilateral knee arthroplasty. The overall proportion of subjects in our sample with poor function is consistent with other recent estimates4,5. However, our multivariate analyses demonstrated that these deficiencies in function may be due to the presence of moderate to severe pre-arthroplasty pain in the contralateral, native knee. In our subjects, we found associations between increasing levels of pre-arthroplasty contralateral knee pain and an increased prevalence of poor post-arthroplasty self-reported function and slow walking speed.
We know of no other study to date that has investigated the effects of pre-arthroplasty contralateral knee pain on self-reported and clinical performance measures of function following knee arthroplasty. One recent study7 assessed the effect of contralateral knee pain on post-arthroplasty function; however, the contralateral pain was assessed after surgery, and the sample was limited to subjects with a pre-arthroplasty contralateral pain score of <4 of 10. Instead, our study shows that moderate to severe contralateral pain also may be a factor leading to poor post-arthroplasty function. In addition, focusing on pre-arthroplasty contralateral pain as opposed to post-arthroplasty pain allowed us to exclude the potential influence of the knee arthroplasty itself on pain in the contralateral knee.
Many studies have considered demographic and clinical pre-arthroplasty predictors of post-arthroplasty function but have not included factors pertaining to the contralateral knee15-17. Factors pertaining to the ipsilateral knee presumably will be eradicated or improved following surgery. Conversely, the status of the contralateral knee may not be immediately improved by surgery or may in fact be worsened initially with increased load during surgical recovery. Studying the status of the contralateral knee prior to knee arthroplasty, rather than after knee arthroplasty, permitted us to focus on the symptoms in the contralateral knee independent of its vulnerability to loading after knee arthroplasty. The clinical data suggest that the contralateral knee pain may be due to the early osteoarthritic changes occurring in these knees. This also may be potentially informative for pre-arthroplasty intervention and prognostication.
The present study had limitations. There may be inherent affective or physical differences in patients who choose to have a second knee replaced18 (for example, such patients may be more likely to choose a second knee arthroplasty because their first one was successful), and this factor may have influenced our finding that subjects with bilateral knee arthroplasty had better self-reported functional results. Because of these potential biases, our findings cannot provide support for the effectiveness of bilateral as compared with unilateral arthroplasty with regard to functional outcomes. In addition, we acknowledge that pre-arthroplasty function is a strong predictor of post-arthroplasty function19; however, we believe that function is on the causal pathway between pre-arthroplasty pain in the contralateral knee and post-arthroplasty function and therefore should not be included in the model. A high proportion (64%) of our subjects reported baseline pain in the spine or lower extremity joints other than the knee, suggesting that other problems may have limited function in our study sample. However, even after adjusting for the presence of these other musculoskeletal problems, the effect of pain in the contralateral knee remains a critical contributor to function. Finally, Escobar et al. found that PASS scores based on tertiles of baseline function did not vary significantly, leading them to conclude that the score “can be considered independent of baseline scores.”12
In summary, our study showed that preoperative pain in the contralateral knee is strongly associated with self-reported post-arthroplasty functional outcome. While the subjects who had bilateral knee arthroplasty in our analyses were less likely to have poor post-arthroplasty function, regardless of pain in the native or previously replaced contralateral knee, as compared with those who had unilateral knee arthroplasty, our results do not necessarily support a preference for bilateral over unilateral knee arthroplasty. Future studies on intervention aimed at the contralateral knee to optimize outcomes are needed.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Acknowledgments
Note:The authors would like to thank Drs. Tuhina Neogi, Peter Grayson, and Devyani Misra for their valuable feedback in the development of this manuscript.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780-5 [DOI] [PubMed] [Google Scholar]
- 2.Cushnaghan J, Bennett J, Reading I, Croft P, Byng P, Cox K, Dieppe P, Coggon D, Cooper C. Long-term outcome following total knee arthroplasty: a controlled longitudinal study. Ann Rheum Dis. 2009 May;68(5):642-7 [DOI] [PubMed] [Google Scholar]
- 3.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2005 Aug;87(8):1719-24 [DOI] [PubMed] [Google Scholar]
- 4.Singh JA, O’Byrne M, Harmsen S, Lewallen D. Predictors of moderate-severe functional limitation after primary Total Knee Arthroplasty (TKA): 4701 TKAs at 2-years and 2935 TKAs at 5-years. Osteoarthritis Cartilage. 2010 Apr;18(4):515-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alzahrani K, Gandhi R, Debeer J, Petruccelli D, Mahomed N. Prevalence of clinically significant improvement following total knee replacement. J Rheumatol. 2011 Apr;38(4):753-9 [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y, Xu L, Nevitt MC, Aliabadi P, Yu W, Qin M, Lui LY, Felson DT. Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: The Beijing Osteoarthritis Study. Arthritis Rheum. 2001 Sep;44(9):2065-71 [DOI] [PubMed] [Google Scholar]
- 7.Zeni JA, Jr, Snyder-Mackler L. Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther. 2010 Jan;90(1):43-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farquhar S, Snyder-Mackler L. The Chitranjan Ranawat Award: The nonoperated knee predicts function 3 years after unilateral total knee arthroplasty. Clin Orthop Relat Res. 2010 Jan;468(1):37-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, Torner J, Lewis CE, Nevitt MC. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007 Sep;56(9):2986-92 [DOI] [PubMed] [Google Scholar]
- 10.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, Tylavsky FA, Brach JS, Satterfield S, Bauer DC, Visser M, Rubin SM, Harris TB, Pahor M. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005 Oct;53(10):1675-80 [DOI] [PubMed] [Google Scholar]
- 11.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, Studenski S, Berkman LF, Wallace RB. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000 Apr;55(4):M221-31 [DOI] [PubMed] [Google Scholar]
- 12.Escobar A, Gonzalez M, Quintana JM, Vrotsou K, Bilbao A, Herrera-Espiñeira C, Garcia-Perez L, Aizpuru F, Sarasqueta C. Patient acceptable symptom state and OMERACT-OARSI set of responder criteria in joint replacement. Identification of cut-off values. Osteoarthritis Cartilage. 2012 Feb;20(2):87-92 [DOI] [PubMed] [Google Scholar]
- 13.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988 Dec;15(12):1833-40 [PubMed] [Google Scholar]
- 14.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996 Jan;34(1):73-84 [DOI] [PubMed] [Google Scholar]
- 15.Parent E, Moffet H. Preoperative Predictors of Locomotor Ability Two Months After Total Knee Arthroplasty for Severe Osteoarthritis. Arthritis & Rheumatism. Arthritis Care Res. 2003;49(1):36-50 [DOI] [PubMed] [Google Scholar]
- 16.Jones CA, Voaklander DC, Suarez-Alma ME. Determinants of function after total knee arthroplasty. Phys Ther. 2003 Aug;83(8):696-706 [PubMed] [Google Scholar]
- 17.Lingard EA, Katz JN, Wright EA, Sledge CB; Kinemax Outcomes Group Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004 Oct;86(10):2179-86 [DOI] [PubMed] [Google Scholar]
- 18.Kim S, Meehan JP, White R. Operative risk of staged bilateral knee arthroplasty is underestimated in retrospective studies. J Arthroplasty. 2011 Dec;26(8):1198-204 [DOI] [PubMed] [Google Scholar]
- 19.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998 Feb;80(2):163-73 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest


