Abstract
Background:
Knot holding strength is essential to maintain wound closure and ensure tissue contact for healing. Knot unraveling can lead to severe complications, especially for high-tension closures such as tendon repairs, which have recently been reported to have knot unraveling rates as high as 86%. In the current study, a novel surgical knot, the two-strand-overhand locking (TSOL) knot, was designed and mechanically evaluated with use of different suture materials and knot configurations and in actual tendon repairs.
Methods:
The knot holding strength of the TSOL knot was compared with that of a 4-throw square knot with use of three different suture materials that are in common clinical use. With use of braided polyblend suture, the TSOL knot was also compared with five other surgical knot configurations. Finally, the strength of tendon repairs performed with use of the TSOL knot and a 4-throw square knot was studied.
Results:
Compared with the 4-throw square knot, the holding strength of the TSOL knot was 143% greater for braided polyblend, 216% greater for polydioxanone, and 118% greater for polyester suture, with a significantly lower knot unraveling rate compared with that of the 4-throw square knot regardless of suture material. The TSOL knot holding strength was also greater than that of the other surgical knot configurations. The strength and stiffness of tendon repairs with a TSOL knot were significantly increased over those of repairs with a 4-throw square knot.
Conclusions:
The TSOL knot provided superior knot holding strength compared with some commonly used surgical knots.
Clinical Relevance:
The TSOL knot has potential clinical applications, especially when knot security is important and high loads are expected, as in tendon or ligament repairs.
Sixteen surgical knot configurations were described by Heraklas in the first century AD1. Heraklas’ “Hercules” knot is recognized as the “square” or “reef” knot commonly used today. This knot and its double-loop first-throw variant, the surgeon’s knot, have been the gold standard of surgical knots for tissue repair, ligature, and wound closure for nearly a century2,3.
Despite the primacy given to the square knot and its variants, knot holding strength (i.e., the force required for the knot to unravel [untie] or for the suture to break at the knot site) has been an important research topic for many years3-7. Adequate knot holding strength is essential to maintain wound closure and ensure tissue contact for healing. Knot unraveling can lead to severe complications, especially in the setting of internal tissue repairs that cannot be directly observed or monitored before catastrophic failure. Knot holding strength is especially important for high-tension closures, such as herniorrhaphy, capsular closure, and tendon and ligament repairs8-12.
Knot holding strength is extremely important for flexor tendon repair, as these small structures can only provide purchase for one or two sutures and as the repair bears a high tensile force during postoperative rehabilitation. Recent studies have shown that, despite the best modern techniques of knot positioning and tying, knots unravel following flexor tendon repair as frequently as 71% to 86% of the time, depending on the repair technique13. The typical recommendation for circumventing this problem has been to increase the number of knot throws13,14. However, increasing the number of throws increases bulk, which can be a problem with certain repairs, especially the repair of flexor tendons, which must pass through a narrow fibro-osseous pulley. In addition, a large knot placed between cut tendon ends potentially interferes with the healing process and could decrease repair strength15,16.
Modern high-strength suture materials cannot be used to their full advantage without proper knot holding strength, and many of these newer materials have a low coefficient of friction and are thus more likely to slip when tied17-19. Silva et al. studied the frictional coefficient of several suture materials and found that braided polyblend suture had a lower frictional coefficient than polyester or nylon sutures20. Waitayawinyu et al. reported that braided polyblend suture increased flexor tendon repair strength. However, braided polyblend knots unraveled before they broke or pulled out during 79% of failure tests13.
We recently designed a 3-throw knot involving a combination of a two-strand-overhand knot plus two surgical square knots, which we have named the “TSOL” (two-strand-overhand locking) knot. The purpose of this study was (1) to measure the TSOL knot holding strength compared with that of a standard surgical 4-throw square knot with use of different suture materials, (2) to compare the TSOL knot holding strength with that of other commonly employed surgical knots, and (3) to investigate the strength of flexor tendon repairs with a TSOL knot compared with a standard square knot. We hypothesized that, compared with the square knot, the TSOL knot would have increased knot holding strength, regardless of the suture material, and would yield increased strength of repaired tendons.
Materials and Methods
Knot Holding Strength of Different Suture Materials
Three commonly used suture materials with a United States Pharmacopeia (USP) designation of 3-0 were selected for testing: braided polyblend (FiberWire; Arthrex, Naples, Florida), polyester (ETHIBOND; Ethicon, Somerville, New Jersey), and polydioxanone (PDS; Ethicon). A closed suture ring was made by looping the suture material around a 30-mm-diameter rod. One of three orthopaedic surgeons (C.Z., C.-C.H., T.M.) randomly tied either a 4-throw square knot or a TSOL knot, and a consistent load of 1 kg was maintained for three seconds to tie the final throw, as shown in Figure 1. To make a TSOL knot, a two-strand overhand knot was first made and a 2-throw square knot was then added. The technique is demonstrated in the accompanying video files. The suture was cut 3 mm from the last knot throw21,22. The suture ring was mounted on a pair of hooking rods (5 mm in diameter), with the knot located in the middle, and the rods were connected to a servohydraulic testing machine (model 312; MTS Systems, Eden Prairie, Minnesota). Therefore, the testing gauge length was 40 mm (the distance between the centers of the two hooking rods) (see Appendix).
Fig. 1.
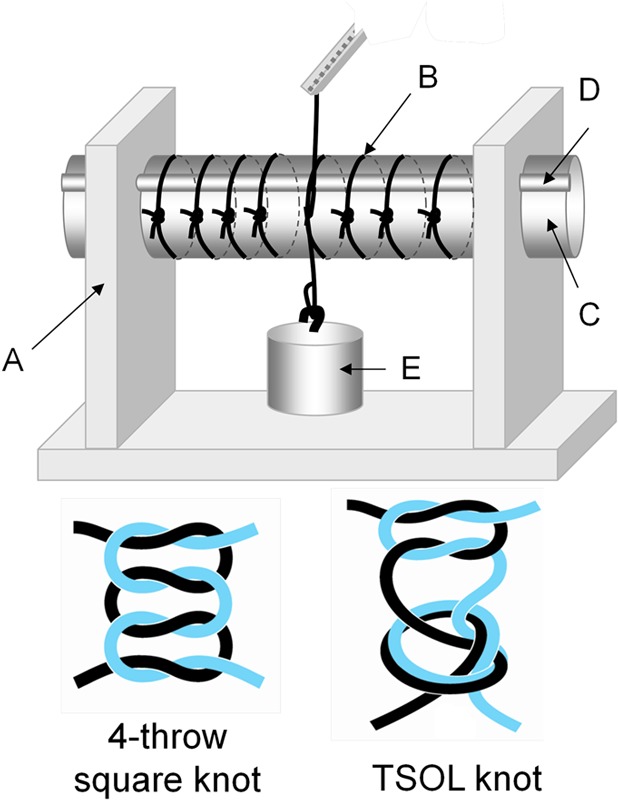
The top panel shows an apparatus (A) for making a suture loop. A single loop (B) is wrapped around a 30-mm-diameter rod (C) and an adjacent 3-mm-diameter rod (D). The purpose of adding the small rod is to permit easy removal of the suture loop from the large rod after withdrawal of the small rod. A 1-kg weight (E) is tied to the knot. The bottom panel illustrates a 4-throw square knot and a TSOL knot.
To test the strength of the suture material alone, a closed suture ring was made by looping the material around a 50-mm-diameter rod and tying it with an 8-throw square knot. The ring was then mounted on the two hooking rods in such a way that the ring wrapped around one of the rods four times, with the knot buried among these suture loops to avoid suture breakage at the knot site or knot unraveling during testing (see Appendix). Although the suture ring was necessarily larger in this group, to accommodate the multiple loops around the hooking rod, the testing gauge length was also 40 mm. For each of the three suture materials, three sets of strength tests were performed—one of the intact suture, one of the 4-throw knot, and one of the TSOL knot. Ten samples were tested in each of these nine sets. The mounted suture ring was distracted to failure at a rate of 20 mm/min. During testing, the suture material was kept moist with a saline solution mist. The force and displacement were recorded at 20 Hz, and the failure mode was also recorded.
Knot Holding Strength in Different Knot Configurations
The braided polyblend suture was selected to test the holding strength of the TSOL knot (designated as group F) compared with several other commonly used surgical knot configurations: a 3-throw square knot (group A), a 4-throw square knot (group B), a 1-throw surgeon’s knot plus a 2-throw square knot (group C), a 1-throw surgeon’s knot plus a 3-throw square knot (group D), and a 5-throw square knot (group E) (Fig. 2). The braided polyblend suture was selected on the basis of the results of the above testing, which indicated its superior suture strength compared with that of the other two materials. A closed suture ring was made by looping around a 30-mm-diameter rod, and the suture was cut 3 mm from the last throw. The mechanical testing was performed on ten samples in each group with use of the same procedures and gauge length (40 mm) used for the previous testing.
Fig. 2.
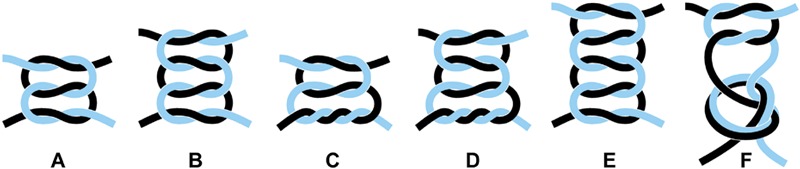
The six tested knot configurations: a 3-throw square knot (A), a 4-throw square knot (B), a 1-throw surgeon’s knot with a 2-throw square knot (C), a 1-throw surgeon’s knot with a 3-throw square knot (D), a 5-throw square knot (E), and a TSOL knot (F).
Tensile Strength of Flexor Tendon Repairs
Twenty-four flexor tendons from five human cadaver hands (from four male donors and one female donor; mean age, seventy-four years), including the flexor digitorum profundus (FDP) and flexor pollicis longus (FPL) tendons, were divided into two groups. The FDP tendons were sharply transected at the level of the proximal interphalangeal joint, and the FPL tendons were transected at the level of the metacarpophalangeal joint. The transected tendons were immediately repaired with 3-0 braided polyblend suture with use of a modified Pennington technique23. The sutures were randomly tied with use of either a 4-throw square knot or a TSOL knot and cut 2 mm from the last loop of the knot in order to bury the suture tails within the tendon ends. A peripheral epitenon suture was not used, as the goal was to strictly compare the knot holding strength of the core suture.
The repaired tendon was mounted on a servohydraulic testing machine and was instrumented with a differential variable reluctance transducer (DVRT; MicroStrain, Williston, Vermont) (Fig. 3). The DVRT displacement curve and the linear region of the force curve recorded by the testing machine were used to calculate the stiffness of the tendon repair. The specimen was distracted to failure at a rate of 20 mm/min23. During testing, the specimen was kept moist with a saline solution mist. Failure was defined as either suture loop breakage or visible complete separation of the tendon ends, with the confirmation that no force was needed to further distract the tendon. The failure mode was observed and recorded.
Fig. 3.
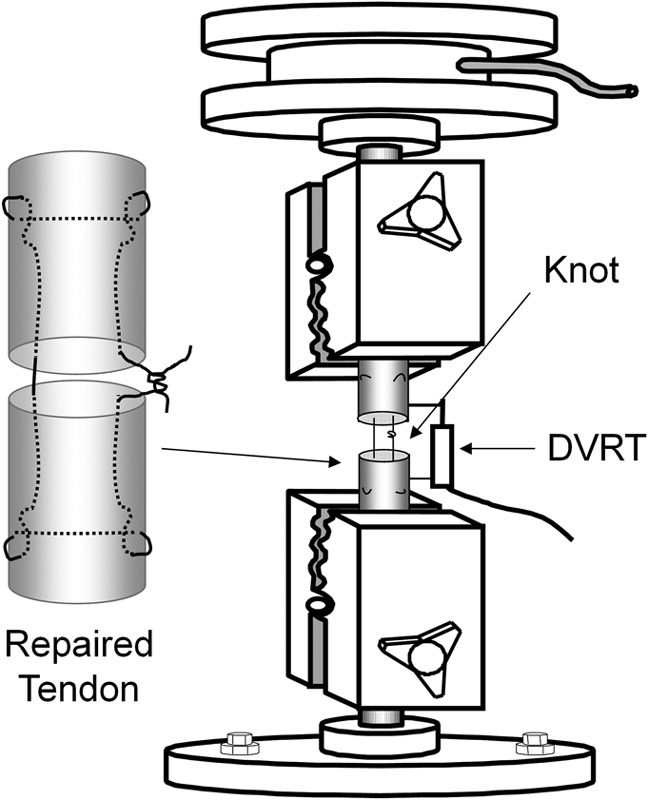
Testing of a tendon repair. A transected tendon is repaired with use of a modified Pennington technique, with the knot (either a 4-throw square knot or a TSOL knot) buried between the tendon ends. The repaired tendon is mounted on the MTS machine for mechanical testing. The DVRT is used to measure gap formation in the repaired tendon and the stiffness of the repair.
Knot Volume Measurement
The knot volume can be estimated by measuring the amount of suture material used to tie the knot. Since the amount of suture material used is directly proportional to its weight, knot weight was used as a proxy for knot volume. USP 3-0 nylon suture (ETHILON; Ethicon) was used to tie either five TSOL knots or five 4-throw square knots around a 1-mm metal rod; as in the previous testing, a constant load of 1 kg was applied to each knot with use of a weight. Following knotting, the suture was cut without leaving any tail. The suture loop with the intact knot was slid off the metal rod. Five suture loops were weighed as a group with use of an analytical balance (Mettler Toledo, Columbus, Ohio) because this balance was not sensitive enough to measure the weight of a single suture loop with a knot. Eight groups of five knots of each type (TSOL and 4-throw square) were weighed, and the mean weights of the two types were compared.
Statistical Analysis
Our pilot data indicated a failure strength and standard deviation of 21.2 ± 6.5 N for a 4-throw square knot and 13.8 ± 4.9 N for a 3-throw square knot. For a two-group t test of equal means, a sample size of ten in each group would yield 80% power at a significance level of p < 0.05 to detect a difference of 7 N, equal to approximately 30% of the failure strength of a 4-throw square knot. The mean failure strength and stiffness of the suture loops (with the various suture materials and knot configurations) and the tendon repair data were analyzed with use of one-factor analysis of variance (ANOVA) with repeated measures to assess differences among groups, followed by a Tukey-Kramer post hoc test for individual comparisons. A simple Pearson chi-square test was used to analyze differences in the knot failure mode (breakage, pullout, or unraveling). The mean knot weight was analyzed with use of a Student t test. All statistical tests were two-sided, and a p value of <0.05 was considered significant.
Source of Funding
This study was partially supported by NIAMS/NIH grant AR44391.
Results
Knot Holding Strength of Different Suture Materials
All suture loops failed within the suture midsubstance during the testing of the intact suture loop (tied with an 8-throw square knot). The failure modes for the TSOL knots and 4-throw square knots made with use of the three different suture materials are listed in the Appendix. For the TSOL knots, suture breakage occurred at the knot site in twenty-five of the thirty loops, which was a significantly greater frequency than that for the 4-throw square knots (four of thirty, p < 0.05). Conversely, the 4-throw knot unraveled (untied) significantly more often than the TSOL knot did (twenty-six compared with five loops).
In the comparison of the suture materials, the braided polyblend suture had a significantly greater potential for knot sliding (fifteen of twenty knots) than the polydioxanone (seven of twenty knots) or polyester sutures (nine of twenty knots) did (p < 0.05). For all three suture materials, the failure strength of the intact loop was significantly greater than that of the knot suture loops regardless of knot type (p < 0.05) (Fig. 4-A). The strength of the intact braided polyblend loop was significantly greater than that of the polyester (p < 0.05). Compared with the 4-throw square knot, the failure strength of the TSOL knot was 143% greater for the braided polyblend, 216% greater for the polydioxanone, and 118% greater for the polyester. The difference was significant for all three suture materials (p < 0.05). The failure strength of the polydioxanone TSOL knot was significantly greater than that of the polyester TSOL knot (p < 0.05). However, there was no significant difference in failure strength among the three different suture materials when the 4-throw square knot was used. The stiffness of the braided polyblend suture material was significantly greater than that of the polyester, which was in turn significantly greater than that of the polydioxanone (p < 0.05) (Fig. 4-B). There was no significant difference in stiffness between the intact suture loop and the TSOL knot for any of the three suture materials. Compared with the 4-throw square knot, the stiffness of the TSOL knot was 65% greater for the braided polyblend (p < 0.05) and 47% greater for the polyester (p < 0.05). However, there was no significant difference in stiffness between the TSOL knot and the 4-throw square knot for the polydioxanone suture.
Fig. 4.
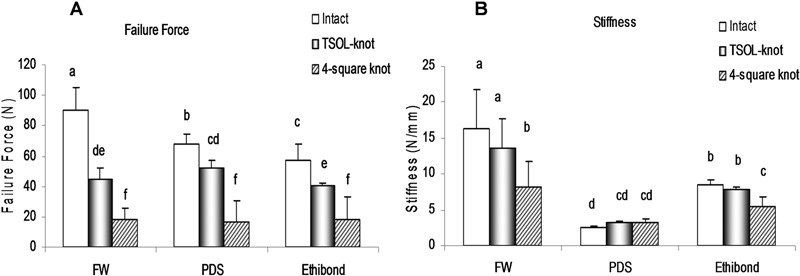
Failure strength (Fig. 4-A) and stiffness (Fig. 4-B) with three different suture materials (braided polyblend [FW], polydioxanone [PDS], and polyester [Ethibond]) and three different knot configurations (8-throw square knot [Intact], TSOL knot, and 4-throw square knot). Bars whose annotations include the same letter (e.g., “a” and “a”) were not significantly different from each other, whereas bars not including the same letter (e.g., “a” and “b”) were significantly different. The error bars represent the standard deviation.
Knot Holding Strength in Different Knot Configurations
Three 5-throw square knots failed by suture rupture at the knot site, and all of the remaining knots in groups A through E failed by unraveling. The failure strength was significantly greater for the TSOL knot than for groups A through E (p < 0.05) (Fig. 5).The failure strength was significantly greater for groups D and E than for groups A and B (p < 0.05). The stiffness was significantly greater for the TSOL knot and group E than for groups A, B, and C (p < 0.05).
Fig. 5.
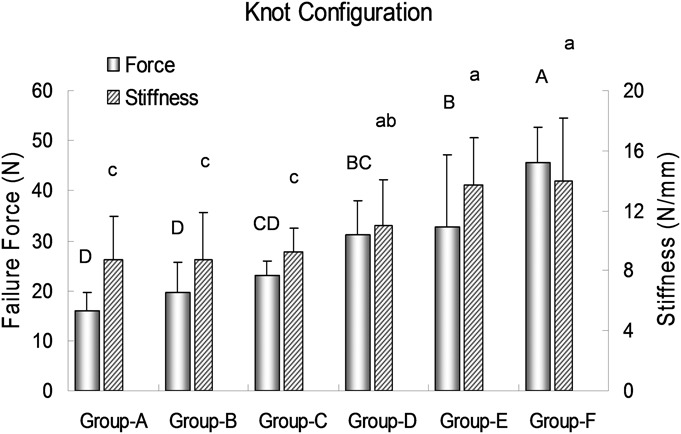
Failure strength (left y axis) and stiffness (right y axis) with six different knot configurations. Group-A = 3-throw square knot, Group-B = 4-throw square knot, Group-C = 1-throw surgeon’s knot with 2-throw square knot, Group-D = 1-throw surgeon’s knot with 3-throw square knot, Group-E = 5-throw square knot, and Group-F = TSOL knot. Bars whose annotations include the same letter were not significantly different from each other, whereas bars not including the same letter were significantly different. The capital letters refer to the failure strength, and the lowercase letters refer to the stiffness. The error bars represent the standard deviation.
Tensile Strength of Tendon Repairs
The failure mode for the 4-throw square knot was knot unraveling in all tendons. For the TSOL knot, four repairs failed by knot unraveling. The other eight failed by suture breakage at the knot. The failure strength and stiffness of the tendons repaired with the TSOL knot were significantly greater than those of the tendons repaired with the 4-throw square knot (p < 0.05) (Fig. 6).
Fig. 6.
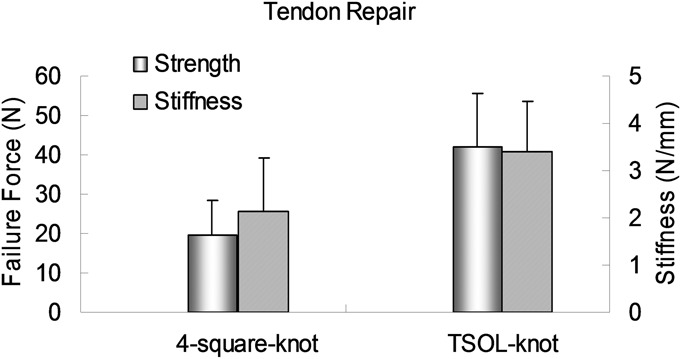
The failure strength (left y axis) and stiffness (right y axis) for tendon repairs with the TSOL knot were significantly higher than those for repairs with the 4-throw square knot. The error bars represent the standard deviation.
Knot Weight Measurement
The mean weight of the TSOL knots was 4.2 ± 0.4 mg compared with 4.1 ± 0.2 mg for the 4-throw square knot; this difference was not significant.
Discussion
The ideal surgical knot should be simple, quick to tie, strong, and secure. The ideal strength of a tied suture should be close to the strength of the suture material itself. However, this ideal is almost impossible to achieve. Knots may slip, and suture material can be weakened by knotting24,25. Square and surgeon’s knots are the most common standard knots used for surgical procedures. Nevertheless, both of these knots often experience knot slippage and unraveling5,26,27, which have been reported to occur in 30% to 100% of typical surgical knots7,27-31, depending on characteristics such as the knot configuration32, suture material26, number of knot throws14, end or “tail” length33, load applied during tying of the knot34, and tying skill35. Trimbos surveyed twenty-five experienced surgeons and discovered that, although most believed that they were using square knots, 80% percent were in fact using sliding knots, which resulted in a large variation in knot holding strength30. However, compared with a variety of commonly used surgical knots, the TSOL knot in the present study—with a base configuration quite different from that of the square knot—yielded a consistently large and significant increase in knot holding strength regardless of suture material.
For the polyester and polydioxanone sutures, the TSOL knots failed by suture rupture and reached 71% and 76%, respectively, of the breaking strength of the suture material. However, although the intact braided polyblend suture material showed a greater breaking strength compared with either the polyester or polydioxanone, use of the TSOL knot did not result in any benefit in breaking strength. This may be due to knot unraveling, which occurred in one-half of the TSOL knots in this group. This, in turn, may be due to the lower coefficient of friction of braided polyblend20. It has been shown theoretically and experimentally that the coefficient of friction of suture material directly correlates with knot holding strength3,5. Herrmann tested eighteen different suture materials and found a perfect linear relationship between the coefficient of friction of the material and the knot holding strength5. For the braided polyblend suture, the TSOL knot reached only 50% of the suture material’s breaking strength, which indicates that there is a potential opportunity for future research to further improve the knot holding strength of the braided polyblend. However, the strength of the TSOL knots that unraveled was still greater than that of the square knots that unraveled, which demonstrates that the TSOL knot configuration yielded greater knot holding strength, even with slippage, compared with the 4-throw square knot.
The number of knot throws has a large effect on knot holding strength. The 2 and 3-throw square knots failed by slippage and knot untying14,21. However, some strong but low-friction suture materials, such as polytetrafluoroethylene (Teflon), polyethylene terephthalate (Dacron), and braided polyblend sutures, have shown evidence of slippage even with six well-snugged-down squared throws on the knot5,13,14. In the present study, 70% of the braided polyblend 5-throw square knots displayed knot slippage. Even with knot slippage, however, the knot holding strength increased in proportion to the increase in the number of throws in the present study; the same effect has also been reported by Herrmann5.
Knot size is also an important parameter in wound-healing. The ideal knot should be strong yet small to reduce the size of the foreign body, especially for tendon repair, in which a large knot may affect tendon-healing since it is buried between opposed tendon ends36. This was the rationale for the assessment of knot volume in the present study. Unfortunately, we were unable to devise a method to accurately measure knot volume, so we used the amount of suture used to make the knot (as reflected by its weight) as a proxy. We found that there was no significant difference in knot weight between the TSOL knot and the 4-throw square knot.
We have found the TSOL knot to be easy to make if there is little tension on the ends to be sutured (see Appendix). If there is greater tension, the assistance of an instrument can be helpful (Fig. 7). There are several ways to tie the first throw (two-strand overhand loop), as shown in the accompanying video files. First, the overhand loop can be slid down with use of forceps within the loop. After withdrawal of the forceps, the two strands of suture are separated and pulled in different directions, bringing the overhand loop down to approximate the tissues being closed. This technique can also be performed by hand. Second, the overhand knot can be made with the help of an assistant. This may be particularly helpful if the tissue to be sutured is under tension. After the tissue ends are approximated by sliding the overhand loop down with forceps, an assistant can hold the knot in position while the forceps are withdrawn and the loop is tied with the securing square knot. Tying a TSOL knot may also become easier and faster if an assistive instrument is used. We have prototyped such an instrument by adding a sliding knot holder to regular forceps. With this instrument, the first overhand loop can be secured even under tension.
Fig. 7.
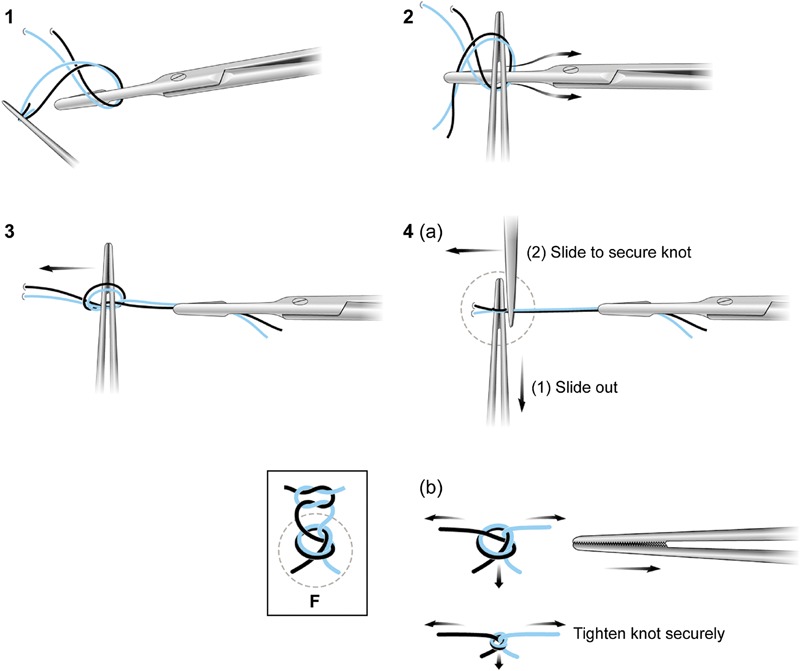
TSOL knot technique. A needle holder goes 360° around the two strands of suture, starting underneath the suture strands (1). The proximal suture is then fed to the needle holder (2). Forceps are inserted into the overhand loop of the first throw to maintain the loop open, then slid down to tie the knot (3), since the knot cannot slide down to approximate the tissue ends if the overhand loop is closed. If the knot is tied under tension, an assistant needs to hold the knot in position, and then the overhand loop can be closed to tie the knot (4[a]). Alternatively, if a strong and low-friction suture material such as braided polyblend is used, the first two-strand overhand knot can be slid by separating the two strand ends (4[b]). Following the first throw of an overhand knot, a 2-throw square knot is added to form the TSOL knot (F).
There are several limitations to this study. Only three different suture materials were evaluated, and we did not test knot holding strength with more than five square knots. As we demonstrated with the 8-throw square knots, knot unraveling can be prevented by adding more knots. However, this strategy to increase knot holding strength has limited applicability because of the bulk involved. It is impossible to use such a strategy in some situations such as flexor tendon repair, in which gliding through a fibro-osseous sheath is important37. Also, we only tested 3-0 suture. Different suture sizes may have different effects on the knot. Only tendon repair with a two-strand core suture was tested; in such testing, each knot would have borne 50% of the total load if the force was evenly distributed between the two strands. We did not assess four or six-strand tendon repair techniques, in which a single suture knot would have borne less load. However, the most common flexor tendon repair technique used clinically is the modified Kessler repair, which involves a two-strand suture with a single knot buried within the tendon ends. We did not perform an epitendinous repair, which is regularly performed clinically, in order to measure exclusively the strength of the core suture and its knot. Without epitendinous repair, our capability to reliably evaluate gap formation in the repaired tendon was limited. Furthermore, without epitendinous repair, assessment of friction following tendon repair is also not reliable. Therefore, we did not evaluate the effect of different knots on tendon friction. Finally, this was an in vitro study, and testing was performed at room temperature. Whether the TSOL knot could maintain its superior holding strength at body temperature (in vivo or in vitro in tissues) is unknown, but decreased holding strength of square knots in vivo has been reported24.
In summary, we designed and tested a new knot with three throws (one two-strand overhand knot plus two square knots, named the TSOL knot) for surgical use. Knot holding strength was assessed with use of three different suture materials and six knot configurations by means of a suture loop testing model. The TSOL knot provided superior holding strength and stiffness compared with the square knots regardless of suture material, without any increase in knot volume compared with the 4-throw square knot. Finally, in the flexor tendon repair model, the TSOL knot provided a strong knot holding capability and also increased the repair stiffness, which might be beneficial to reduce the rate of tendon rupture and gap formation. We believe that this new knot has potential clinical applications, especially for suturing soft tissue under tension, such as in tendon or ligament repairs.
Appendix
A table showing the failure modes of the suture loops, a figure illustrating the strength testing procedures, and videos demonstrating techniques for tying the first knot throw are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
A table showing the failure modes of the suture loops, a figure illustrating the strength testing procedures, and videos demonstrating techniques for tying the first knot throw
Video 1: Making the first throw of the two-strand overhand loop by using a needle holder without the help of an assistant. The overhand loop is slid down with forceps within the loop. After withdrawing the forceps, the two strands of suture are separated and pulled in different directions, bringing the overhand loop down to approximate the tissues being closed.
Video 2: Making the first throw of the two-strand overhand loop by hand without the help of an assistant.
Video 3: Making the first throw of the two-strand overhand loop by using a needle holder with the help of an assistant. This may be particularly helpful if the tissue to be sutured is under tension. After the tissue ends are approximated by sliding down the overhand loop with a forceps, an assistant can hold the knot in position, then the forceps is withdrawn and the loop is tied with the securing square knot.
Video 4: Making the first throw of the two-strand overhand loop by using a specially designed instrument without the help of an assistant. In the prototype in this video, a sliding knot holder has been added to regular forceps. With this instrument, the first overhand loop can be secured even under tension.
Acknowledgments
Note: Arthrex, Inc. provided the braided polyblend (FiberWire) suture material.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Hage JJ. Heraklas on knots: sixteen surgical nooses and knots from the first century A.D. World J Surg. 2008 Apr;32(4):648-55 [DOI] [PubMed] [Google Scholar]
- 2.Halsted WS. Ligature and suture material. J Am Med Assoc. 1913;LX(15):1119-26 [Google Scholar]
- 3.Taylor FW. Surgical knots. Ann Surg. 1938 Mar;107(3):458-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babcock WW. Metallic sutures and ligatures. Surg Clin North Am. 1947;27:1435. [DOI] [PubMed] [Google Scholar]
- 5.Herrmann JB. Tensile strength and knot security of surgical suture materials. Am Surg. 1971 Apr;37(4):209-17 [PubMed] [Google Scholar]
- 6.Fong EDM, Bartlett ASR, Malak S, Anderson IA. Tensile strength of surgical knots in abdominal wound closure. ANZ J Surg. 2008 Mar;78(3):164-6 [DOI] [PubMed] [Google Scholar]
- 7.Muffly TM, Boyce J, Kieweg SL, Bonham AJ. Tensile strength of a surgeon’s or a square knot. J Surg Educ. 2010 Jul-Aug;67(4):222-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ketchum LD. Suture materials and suture techniques used in tendon repair. Hand Clin. 1985 Feb;1(1):43-53 [PubMed] [Google Scholar]
- 9.Schaller G, Paolucci V, Gutt C, Weber B, Manegold BC. The “knot before loop” technique for the endoscopic ligation and suture-instrument set. Knot formation and application. Surg Endosc. 1997 Jul;11(7):785-8 [DOI] [PubMed] [Google Scholar]
- 10.Provencher MT, Verma N, Obopilwe E, Rincon LM, Tracy J, Romeo AA, Mazzocca A. A biomechanical analysis of capsular plication versus anchor repair of the shoulder: can the labrum be used as a suture anchor? Arthroscopy. 2008 Feb;24(2):210-6 [DOI] [PubMed] [Google Scholar]
- 11.Tera H, Aberg C. Tissue strength of structures involved in musculo-aponeurotic layer sutures in laparotomy incisions. Acta Chir Scand. 1976;142(5):349-55 [PubMed] [Google Scholar]
- 12.Becker R, Schröder M, Stärke C, Röpke M, Nebelung W. [Mechanical properties of suture materials for anchoring cruciate ligament transplants]. Unfallchirurg. 2000 May;103(5):375-9 German [DOI] [PubMed] [Google Scholar]
- 13.Waitayawinyu T, Martineau PA, Luria S, Hanel DP, Trumble TE. Comparative biomechanic study of flexor tendon repair using FiberWire. J Hand Surg Am. 2008 May-Jun;33(5):701-8 [DOI] [PubMed] [Google Scholar]
- 14.Ivy JJ, Unger JB, Hurt J, Mukherjee D. The effect of number of throws on knot security with nonidentical sliding knots. Am J Obstet Gynecol. 2004 Nov;191(5):1618-20 [DOI] [PubMed] [Google Scholar]
- 15.Papandrea R, Seitz WH, Jr, Shapiro P, Borden B. Biomechanical and clinical evaluation of the epitenon-first technique of flexor tendon repair. J Hand Surg Am. 1995 Mar;20(2):261-6 [DOI] [PubMed] [Google Scholar]
- 16.Komatsu F, Mori R, Uchio Y. Optimum surgical suture material and methods to obtain high tensile strength at knots: problems of conventional knots and the reinforcement effect of adhesive agent. J Orthop Sci. 2006 Jan;11(1):70-4 [DOI] [PubMed] [Google Scholar]
- 17.Wright PB, Budoff JE, Yeh ML, Kelm ZS, Luo ZP. Strength of damaged suture: an in vitro study. Arthroscopy. 2006 Dec;22(12):1270: e3 [DOI] [PubMed] [Google Scholar]
- 18.Bisson LJ, Manohar LM, Wilkins RD, Gurske-Deperio J, Ehrensberger MT. Influence of suture material on the biomechanical behavior of suture-tendon specimens: a controlled study in bovine rotator cuff. Am J Sports Med. 2008 May;36(5):907-12 [DOI] [PubMed] [Google Scholar]
- 19.Moriya T, Zhao C, Yamashita T, An KN, Amadio PC. Effect of core suture technique and type on the gliding resistance during cyclic motion following flexor tendon repair: a cadaveric study. J Orthop Res. 2010 Nov;28(11):1475-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silva JM, Zhao C, An KN, Zobitz ME, Amadio PC. Gliding resistance and strength of composite sutures in human flexor digitorum profundus tendon repair: an in vitro biomechanical study. J Hand Surg Am. 2009 Jan;34(1):87-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thacker JG, Rodeheaver G, Kurtz L, Edgerton MT, Edich RF. Mechanical performance of sutures in surgery. Am J Surg. 1977 Jun;133(6):713-5 [DOI] [PubMed] [Google Scholar]
- 22.Muffly T, McCormick TC, Dean J, Bonham A, Hill RFC. An evaluation of knot integrity when tied robotically and conventionally. Am J Obstet Gynecol. 2009 May;200(5):e18-20 [DOI] [PubMed] [Google Scholar]
- 23.Tanaka T, Amadio PC, Zhao C, Zobitz ME, Yang C, An KN. Gliding characteristics and gap formation for locking and grasping tendon repairs: a biomechanical study in a human cadaver model. J Hand Surg Am. 2004 Jan;29(1):6-14 [DOI] [PubMed] [Google Scholar]
- 24.Herrmann JB. Changes in tensile strength and knot security of surgical sutures in vivo. Arch Surg. 1973 May;106(5):707-10 [DOI] [PubMed] [Google Scholar]
- 25.Trail IA, Powell ES, Noble J. An evaluation of suture materials used in tendon surgery. J Hand Surg Br. 1989 Nov;14(4):422-7 [DOI] [PubMed] [Google Scholar]
- 26.Brouwers JE, Oosting H, de Haas D, Klopper PJ. Dynamic loading of surgical knots. Surg Gynecol Obstet. 1991 Dec;173(6):443-8 [PubMed] [Google Scholar]
- 27.Hurt J, Unger JB, Ivy JJ, Mukherjee D, Pizzaro A. Tying a loop-to-strand suture: is it safe? Am J Obstet Gynecol. 2005 Apr;192(4):1094-7 [DOI] [PubMed] [Google Scholar]
- 28.Tera H, Aberg C. Tensile strengths of twelve types of knot employed in surgery, using different suture materials. Acta Chir Scand. 1976;142(1):1-7 [PubMed] [Google Scholar]
- 29.Holmlund DE. Suture technic and suture-holding capacity. A model study and a theoretical analysis. Am J Surg. 1977 Nov;134(5):616-21 [DOI] [PubMed] [Google Scholar]
- 30.Trimbos JB. Security of various knots commonly used in surgical practice. Obstet Gynecol. 1984 Aug;64(2):274-80 [PubMed] [Google Scholar]
- 31.Shaw AD, Duthie GS. A simple assessment of surgical sutures and knots. J R Coll Surg Edinb. 1995 Dec;40(6):388-91 [PubMed] [Google Scholar]
- 32.Lo IKY, Ochoa E, Jr, Burkhart SS. A comparison of knot security and loop security in arthroscopic knots tied with newer high-strength suture materials. Arthroscopy. 2010 Sep;26(9)(Suppl):S120-6 [DOI] [PubMed] [Google Scholar]
- 33.Muffly TM, Cook C, Distasio J, Bonham AJ, Blandon RE. Suture end length as a function of knot integrity. J Surg Educ. 2009 Sep-Oct;66(5):276-80 [DOI] [PubMed] [Google Scholar]
- 34.Batra EK, Franz DA, Towler MA, Rodeheaver GT, Thacker JG, Zimmer CA, Edlich RF. Influence of surgeon’s tying technique on knot security. J Appl Biomater. 1993 Fall;4(3):241-7 [DOI] [PubMed] [Google Scholar]
- 35.Ind TE, Shelton JC, Shepherd JH. Influence of training on reliability of surgical knots. BJOG. 2001 Oct;108(10):1013-6 [DOI] [PubMed] [Google Scholar]
- 36.Pruitt DL, Aoki M, Manske PR. Effect of suture knot location on tensile strength after flexor tendon repair. J Hand Surg Am. 1996 Nov;21(6):969-73 [DOI] [PubMed] [Google Scholar]
- 37.Zhao C, Amadio PC, Zobitz ME, An KN. Gliding characteristics of tendon repair in canine flexor digitorum profundus tendons. J Orthop Res. 2001 Jul;19(4):580-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
A table showing the failure modes of the suture loops, a figure illustrating the strength testing procedures, and videos demonstrating techniques for tying the first knot throw
Video 1: Making the first throw of the two-strand overhand loop by using a needle holder without the help of an assistant. The overhand loop is slid down with forceps within the loop. After withdrawing the forceps, the two strands of suture are separated and pulled in different directions, bringing the overhand loop down to approximate the tissues being closed.
Video 2: Making the first throw of the two-strand overhand loop by hand without the help of an assistant.
Video 3: Making the first throw of the two-strand overhand loop by using a needle holder with the help of an assistant. This may be particularly helpful if the tissue to be sutured is under tension. After the tissue ends are approximated by sliding down the overhand loop with a forceps, an assistant can hold the knot in position, then the forceps is withdrawn and the loop is tied with the securing square knot.
Video 4: Making the first throw of the two-strand overhand loop by using a specially designed instrument without the help of an assistant. In the prototype in this video, a sliding knot holder has been added to regular forceps. With this instrument, the first overhand loop can be secured even under tension.


