Abstract
Background:
There is little research on the long-term outcomes of open carpal tunnel release. The purpose of this retrospective study was to determine the functional and symptomatic outcomes of patients at a minimum of ten years postoperatively.
Methods:
Two hundred and eleven patients underwent open carpal tunnel release from 1996 to 2000 performed by the same hand fellowship-trained surgeon. Follow-up with validated self-administered questionnaire instruments was conducted an average of thirteen years after surgery. The principal outcomes included the Levine-Katz symptom and function scores, ranging from 1 point (best) to 5 points (worst), and satisfaction with the results of surgery. The patients self-reported current comorbidities.
Results:
After a mean follow-up of thirteen years (range, eleven to seventeen years), 92% (194) of 211 patients were located. They included 140 who were still living and fifty-four who had died. Seventy-two percent (113) of the 157 located, surviving patients responded to the questionnaire. The mean Levine-Katz symptom score (and standard deviation) was 1.3 ± 0.5 points, and 13% of patients had a poor symptom score (≥2 points). The mean Levine-Katz function score was 1.6 ± 0.8 points, and 26% had a poor function score (≥2 points). The most common symptom-related complaint was weakness in the hand, followed by diurnal pain, numbness, and tingling. The least common symptoms were nocturnal pain and tenderness at the incision. Eighty-eight percent of the patients were either completely satisfied or very satisfied with the surgery. Seventy-four percent reported their symptoms to be completely resolved. Thirty-three percent of men were classified as having poor function compared with 23% of women. Two (1.8%) of 113 patients underwent repeat surgery.
Conclusions:
At an average of thirteen years after open carpal tunnel release, the majority of patients are satisfied and free of symptoms of carpal tunnel syndrome.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Open carpal tunnel release is a common surgical treatment for carpal tunnel syndrome. However, few long-term outcomes studies on open carpal tunnel release have been reported. Prior studies investigating outcomes longer than two years have not always used validated instruments1,2, or achieved high participation rates3. We are unaware of any studies describing outcomes of open carpal tunnel release assessed with validated outcomes instruments at a minimum of ten years following surgery.
A prospective study of open carpal tunnel release outcomes performed in the mid-1990s determined that, although some symptoms improve immediately postoperatively, strength and function often take months to reach preoperative levels4. Recurrence of symptoms has also been documented in some studies4-7, with as many as 57% of patients reporting a return of symptoms after a period of two years7. Additionally, nerve conduction studies have demonstrated that median nerve electrodiagnostic parameters commonly do not fully recover, even after clinically successful surgery8-11. These findings suggest that carpal tunnel release may not fully restore nerve function to normal levels.
The purpose of this retrospective investigation was to use validated measures of pain and functional status to evaluate the long-term outcomes of patients assessed a minimum of ten years following open carpal tunnel release. We hypothesized that nocturnal pain, which is strongly associated with carpal tunnel syndrome, will be present in a small minority of patients on long-term follow-up.
Materials and Methods
Sample
The study was completed at Brigham and Women’s Hospital, an academic medical center. Using an interdepartmental database for International Classification of Diseases, Ninth Revision (ICD-9) billing code 354.0 and Current Procedural Terminology code 64721, we identified all patients who underwent open carpal tunnel release from 1996 to 2000 by a single hand-fellowship trained surgeon (B.P.S.). A modified version of the standard open carpal tunnel release, involving a slightly smaller (1.5-cm) incision, was used for all patients in this series (Fig. 1). Patients were excluded if, at the time of the index surgery, they underwent any other upper extremity procedure, such as a distal radial fracture repair, with the exception of concomitant release of a trigger finger or a de Quervain tenosynovitis. Non-English speakers were excluded. For patients undergoing bilateral procedures within the 1996 to 2000 time period, only the first hand to be operatively treated was included.
Fig. 1.
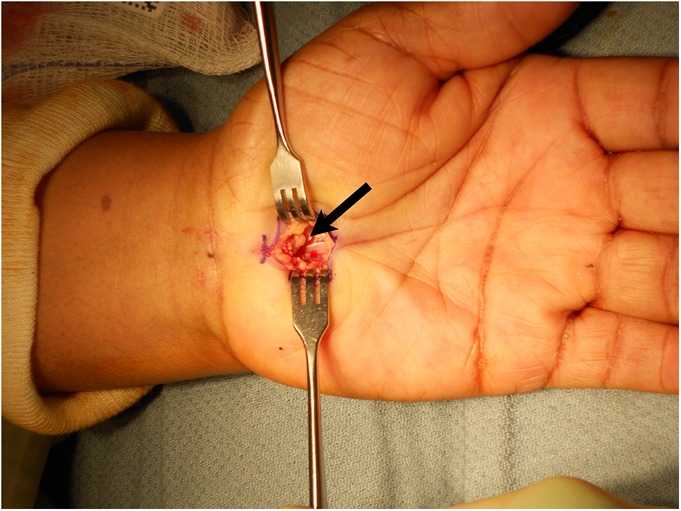
Open carpal tunnel release incision as performed by the one of the authors (B.P.S.). This image displays the carpal tunnel ligament prior to surgical division. The arrow points to the cut radial leaf of the transverse carpal ligament.
This retrospective study received approval from the institutional review board. Patients were first contacted by mail, and subsequently by telephone. No compensation was given. We attempted to contact patients by searching medical records and online web sites, such as telephone books and person-searching services, in a fashion similar to that described in prior orthopaedic investigations12,13. We utilized the Social Security Death Index to identify patients who had died during the follow-up period. Once contacted, patients were mailed a questionnaire (Fig. 2). Patients were not asked to attend a follow-up examination or interview. The human subjects research board did not permit the patient’s next-of-kin listed either in the medical record, or found through other methods, to be contacted.
Fig. 2.
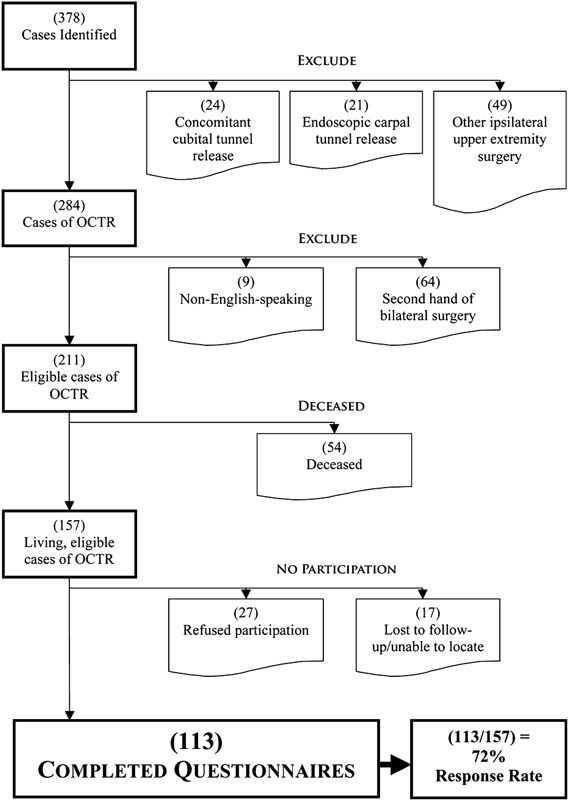
Chart showing the CONSORT (Consolidated Standards of Reporting Trials) cohort divided into relevant categories. OCTR = open carpal tunnel release.
Data Elements
Carpal tunnel symptoms and functional status were evaluated by the Levine-Katz carpal tunnel instrument14, which includes an eleven-item symptom severity scale and a nine-item functional status scale. Patients were also asked two additional questions regarding (1) symptom resolution in the first year after surgery and (2) their perception of the effect of the surgery on their carpal tunnel symptoms. The Levine-Katz scales are reliable, internally consistent, valid, and responsive15. Each item has five ordinal response categories, ranging from 1 point (no pain or symptoms and no difficulty with activity) to 5 points (severe pain or symptoms and cannot do activity). The items within each category are averaged to create an overall score. We defined poor symptom and function scores as an overall score of ≥2 points. In prior research, a score of 2 points was the mean postoperative score14,16. Sensitivity analyses that used other cutoff scores had similar results and are not presented.
Satisfaction with surgery was assessed in eight areas on an ordinal scale of 1 (completely satisfied) to 5 (very dissatisfied) (Table I). We averaged the satisfaction rating over all eight items to create an overall satisfaction measure. In addition, patients rated their overall satisfaction with the results of the surgery and the change in their quality of life, using satisfaction scales previously determined to be valid17.
TABLE I.
Satisfaction Items for the 113 Patients*
| Question | Score |
||||
| “How satisfied are you with …?” | 1 (Completely Satisfied) | 2 (Very Satisfied) | 3 (Somewhat Satisfied) | 4 (Somewhat Dissatisfied) | 5 (Very Dissatisfied) |
| Relief of night pain | 86 (78.9%) | 15 (13.8%) | 4 (3.7%) | 3 (2.8%) | 1 (0.9%) |
| Relief of daytime pain | 81 (73.6%) | 17 (15.5%) | 4 (3.6%) | 5 (4.5%) | 3 (2.7%) |
| Relief of tingling | 76 (69.1%) | 21 (19.1%) | 8 (7.3%) | 3 (2.7%) | 2 (1.8%) |
| Relief of numbness | 78 (70.3%) | 17 (15.3%) | 12 (10.8%) | 3 (2.7%) | 1 (0.9%) |
| Strength in hand | 61 (55.0%) | 23 (20.7%) | 16 (14.4%) | 7 (6.3%) | 4 (3.6%) |
| Performance at work | 75 (72.8%) | 17 (16.5%) | 6 (5.8%) | 3 (2.9%) | 2 (1.9%) |
| Performance at household tasks | 73 (66.4%) | 21 (19.1%) | 9 (8.2%) | 4 (3.6%) | 3 (2.7%) |
| Performance at recreational activities | 71 (65.7%) | 19 (17.6%) | 10 (9.3%) | 3 (2.8%) | 5 (4.6%) |
Totals may not equal 113 in all instances because of incomplete responses.
The Sangha self-administered comorbidities instrument18 assessed current comorbidities. Patients were grouped into three categories on the basis of the number of comorbidities reported: zero, one or two, or more than two. We created a dichotomous category (present or absent) for comorbidities that may cause hand symptoms and functional deficits similar to carpal tunnel syndrome (carpal tunnel syndrome-confounding comorbidities). Diabetes mellitus, rheumatoid arthritis, neuropathy, and osteoarthritis were included. Determination of the comorbid conditions in this category was based on our clinical experience. The questionnaire additionally included questions on the index hand, age, sex, employment status, and status regarding Workers’ Compensation for carpal tunnel syndrome. The time since surgery was calculated as the time from the index surgery to questionnaire completion. Age at the time of surgery was grouped into three categories: under fifty years, fifty to fifty-nine years, and sixty years or older. The categories were based in part on distribution (permitting three groups with adequate representation) and in part on clinical considerations. The younger group is enriched for workers and premenopausal women, the older group has more retirees and postmenopausal women with a greater likelihood of comorbidities, and the middle group (fifty to fifty-nine) has a mix of these characteristics.
Statistical Analysis
Study data were collected and managed using REDCap (Research Electronic Data Capture) a secure, web-based application designed to support data capture for research studies19. Data were entered into a REDCap database and exported to SAS version 9.2 (SAS Institute, Cary, North Carolina) for statistical analysis.
To describe the symptoms and functional status of patients, we present means and standard deviations for continuous variables, and frequencies and percentages for categorical variables. We examined factors associated with poor outcome for symptoms and function separately. In bivariate analysis, we considered age at the time of surgery, sex, whether the surgery was on the dominant hand, and years since surgery. Multivariable logistic regression models were used to estimate the likelihood of a poor outcome adjusted for other covariates. To determine which factors to include in multivariate models, we used clinical judgment and the results of the bivariate analysis. Our final models included age at the time of surgery, sex, and whether surgery was performed on the dominant hand. We used interaction terms in our multivariate logistic regression models to formally test for an interaction between age and sex, with a p value of <0.05 considered significant. To gain insight into the factors that contribute to current levels of pain and function, we examined these outcomes in relation to current comorbidities and current neuromuscular comorbidities. We examined whether outcomes were different by comorbidity group using chi-square and Fisher exact tests, where appropriate.
Source of Funding
This research was supported by grants K24AR057827 and T32AR055885 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health and by the Pilot Research Incubation and Development Program (PRIDE), Department of Orthopedic Surgery, Brigham and Women’s Hospital.
Results
Sample
Three hundred and seventy-eight open carpal tunnel releases were identified via billing codes, and 211 of them were eligible after exclusions. Patients were excluded for the following reasons: endoscopic carpal tunnel release (twenty-one patients), concomitant cubital tunnel release (twenty-four patients), any other ipsilateral upper-extremity procedure at the time of surgery aside from trigger finger release or de Quervain tenosynovitis (forty-nine patients), and non-English speakers (nine patients). In addition, sixty-four subjects underwent staged bilateral carpal tunnel release, with only the initial carpal tunnel release analyzed. Of the 211 patients, 92% (194) were located. There were fifty-four deceased patients identified. Of the 157 surviving patients, twenty-seven declined to participate and seventeen were lost to follow-up, leaving 113 who participated for a final response rate of 72% (113 participants of 157 surviving eligible subjects) (Fig. 2). Of those who declined, the majority did not respond to communication attempts, so no reason could be ascertained. Nine patients were too busy to participate. One patient declined because of a poor outcome. The forty-four eligible patients who refused participation or were lost to follow-up were similar to enrolled patients with respect to age. Men were more likely to participate than women (83% versus 68%) although this difference was not significant (p = 0.09). The twenty-seven eligible patients who refused participation were similar to enrolled patients with respect to age (average, forty-nine years versus fifty-two years; p > 0.05) and sex (81% female versus 71% male; p > 0.05).
The average time to follow-up after surgery was thirteen years (range, eleven to seventeen years). Seventy-six patients underwent open carpal tunnel release on their dominant hand, and thirty-four, on their nondominant hand. (One patient had incomplete responses.) Seventy-one percent of the patients were female, and 29% were male. The mean age (and standard deviation) at the time of surgery was 52 ± 14 years. Forty-five percent of the patients were under fifty years old at the time of surgery, 20% were fifty to fifty-nine years of age, and 35% were sixty years of age or older. Men were older than women at the time of surgery, with a mean age of 58 ± 12.6 years compared with 50 ± 13.7 years for women. Fifty-two percent of men were sixty years of age or older at the time of surgery compared with 28% of women. Five percent of all patients had received Workers’ Compensation because of their carpal tunnel syndrome (see Appendix).
Fifty-two percent of patients reported a carpal tunnel syndrome-confounding comorbidity on the Self-Administered Comorbidity Questionnaire (see Appendix). Ten percent of patients reported no comorbidities, 38% reported one or two, and 52% reported three or more.
Outcomes: Symptoms and Function
The mean Levine-Katz symptom score was 1.3 ± 0.5 points, and 13% of patients had a poor symptom score (≥2 points) (Table II). Thirty-three percent of patients rated at least one of the eleven symptom items as >2 points, indicating at least one symptom of moderate severity. The mean Levine-Katz function score was 1.6 ± 0.8 points, and 26% had a poor function score (≥2 points). Thirty-nine percent of patients rated at least one of the nine function items as >2 points. The Pearson correlation coefficient demonstrated a moderately strong association between symptom and function scores (r = 0.70). Of the 110 patients reporting both pain and function scores, forty-six (42%) had both scores equal to 1 point (no symptoms and no functional impairment).
TABLE II.
Outcomes of Carpal Tunnel Release at Ten to Fifteen-Year Follow-up of 113 Patients
| Outcome Measure | Finding |
| Symptom, function, and satisfaction scores* (scale of 1 to 5) (points) | |
| Levine-Katz symptom score | 1.3 (0.5) |
| Levine-Katz function score | 1.6 (0.8) |
| Overall satisfaction | 1.5 (0.8) |
| Specific outcomes† (no. of patients) | |
| Poor Levine-Katz symptom score (≥2 points) | |
| No | 97 (87%) |
| Yes | 15 (13%) |
| Poor Levine-Katz function score (≥2 points) | |
| No | 82 (74%) |
| Yes | 29 (26%) |
| Revision carpal tunnel syndrome surgery on index hand | |
| No | 111 (98%) |
| Yes | 2 (2%) |
| Symptoms within first year of surgery | |
| Disappear entirely | 81 (72%) |
| Get partially better | 25 (22%) |
| Stay the same | 5 (5%) |
| Worsen a lot | 1 (1%) |
| Symptoms overall (at the time of the survey) | |
| Completely better | 83 (74%) |
| Somewhat better | 22 (20%) |
| Stayed the same | 4 (4%) |
| Significantly worse | 3 (3%) |
| Satisfaction with surgery | |
| Completely or very satisfied | 97 (88%) |
| Somewhat satisfied | 4 (4%) |
| Somewhat or very dissatisfied | 9 (8%) |
The scores are given as the mean and the standard deviation.
Totals may not equal 113 in all instances because of incomplete responses.
Overall, 72% of patients reported that their symptoms disappeared entirely within the first year of surgery, and 74% reported that, at a minimum of ten years, the surgery made their symptoms completely better. Eighty-eight percent of patients were either completely satisfied or very satisfied with the surgery. Quality of life also showed “great” improvement or “more improvement than I dreamed possible” in 81% of patients. Two patients eventually underwent revision carpal tunnel release on the index hand.
The most common symptom-related complaint was weakness in the hand (39%) (see Appendix). Twenty-three percent reported tingling, 25% reported numbness, and 25% reported diurnal pain. However, the classic carpal tunnel syndrome-related symptom of nocturnal pain was less frequent, reported by 12% of patients. Pain or tenderness at the incision and being woken up by pain at night were the least problematic (reported by 5% and 6%, respectively). In terms of function, opening of jars was the most problematic task, with 45% reporting at least mild difficulty (see Appendix). Grasping small objects (32%), grasping grocery bags (30%), and holding a book (30%) followed.
Factors Related to Outcomes: Sex, Comorbidities, and Age
Thirty-three percent of men were classified as having poor function compared with 23% of women. Men were also less likely to report being asymptomatic (symptoms “disappeared entirely”) in the first year after surgery (50% of men versus 81% of women), or at the time of the survey (59% of men versus 80% of women). However, the Levine-Katz symptom scores were similar between men and women: 13% of women had a poor symptom score compared with 16% of men. Women were more likely than men to be completely satisfied with the surgery (68% versus 56%).
There was a difference in outcomes between age groups. The fifty to fifty-nine-year-old age group reported worse function, symptoms, and satisfaction compared with the group under fifty and the group over fifty-nine years old. Twenty percent of the group under fifty and 21% of the group over fifty-nine years had a poor function score, compared with 48% of the fifty to fifty-nine-year-old group (p = 0.0289). Seventy-six percent of the group under fifty and 79% of the group over fifty-nine years old reported that they were currently asymptomatic compared with 61% of the fifty to fifty-nine-year-old group.
Of the eleven patients with no comorbidities, none had a poor symptom score or poor function score; 14% of patients with one or two comorbidities had a poor symptom score and 20% had a poor function score; 16% of patients with more than two comorbidities had a poor symptom score and 36% had a poor function score (p = 0.3723 for pain and p = 0.0200 for function). Eighty-two percent of the group without comorbidities was completely satisfied with the surgery compared with 72% in the group with one or two comorbidities and 59% in the group with more than two comorbidities (p = 0.0589).
Those with a carpal tunnel syndrome-confounding comorbidity (diabetes mellitus, polyneuropathy, rheumatoid arthritis, or osteoarthritis) generally had worse symptoms, worse function, and worse satisfaction compared with those without (Table III): 16% of patients with one or more carpal tunnel syndrome-confounding comorbidities had a poor symptom score and 33% had a poor function score, whereas 11% of those without a carpal tunnel syndrome-confounding comorbidity had a poor symptom score and 19% had a poor function score. Eighty-nine percent of the patients with a carpal tunnel syndrome-confounding comorbidity were completely satisfied with the surgery compared with 87% of the patients without one.
TABLE III.
Outcomes by Carpal Tunnel Syndrome-Confounding Comorbidity Status
| CTS-Confounding Comorbidity*
(no. of patients) |
||
| Outcomes | No | Yes |
| Poor Levine-Katz symptom score† | ||
| No | 48 (89%) | 48 (84%) |
| Yes | 6 (11%) | 9 (16%) |
| Poor Levine-Katz function score‡ | ||
| No | 43 (81%) | 38 (67%) |
| Yes | 10 (19%) | 19 (33%) |
| Satisfaction | ||
| Completely or very satisfied | 46 (87%) | 50 (89%) |
| Somewhat satisfied | 1 (2%) | 3 (5%) |
| Somewhat or very dissatisfied | 6 (11%) | 3 (5%) |
Totals may not equal 113 in all instances because of incomplete responses. Carpal tunnel syndrome (CTS)-confounding comorbidities included diabetes mellitus, polyneuropathy, rheumatoid arthritis, and osteoarthritis.
A poor score was defined as a symptom score of ≥2 points on an ordinal scale of 1 (best) to 5 (worst).
A poor score was defined as a function score of ≥2 points on an ordinal scale of 1 (best) to 5 (worst).
Multivariable Models
We used multivariable logistic regression models to estimate the independent associations between various demographic and clinical factors and surgical outcome. Neither sex nor surgery on the dominant hand was significantly associated with poor symptoms or poor function. Age group was not significantly associated with symptoms, but was associated with function (p = 0.0353). The association was not monotonic (ordered). Rather, function was worst in the middle age group and better in the oldest and youngest age groups. Specifically, those in the fifty to fifty-nine-year age group had 3.5 (95% confidence interval [CI]: 1.1, 10.6) times the odds of poor function relative to those in the group under fifty and 4.0 (95% CI: 1.2, 12.9) times the odds of poor function relative to the group over fifty-nine years old.
We added an interaction term to the multivariable models to test whether the association between outcome and age varied by sex, and we did not find significant interaction for either outcome.
Discussion
While numerous studies have noted the excellent early results of open carpal tunnel release20-23, the durability of clinical results has remained uncertain. A recent study24 has claimed that surgical outcomes after five years were only marginally better than nonsurgical outcomes. Other studies have described noticeable returns of at least some preoperative symptoms, on the order of 57%7 and 25%5.
The results of the present study show that long-term results of open carpal tunnel release are favorable. Eighty-seven percent of patients reported good symptom scores (<2 points) and 74% reported good function scores (<2 points). Eighty-eight percent of the patients were completely or very satisfied. We hypothesized that nocturnal pain, which is characteristic of nerve irritation due to carpal tunnel syndrome, will be present in a small minority of patients. The problems reported more frequently, such as daytime pain, weakness, and trouble opening jars, are less specific to carpal tunnel syndrome and may be attributable to other comorbidities such as osteoarthritis or rheumatoid arthritis. Our finding that carpal tunnel syndrome-confounding comorbidities, such as rheumatoid arthritis, diabetes mellitus, polyneuropathy, and osteoarthritis, are associated with pain and function scores supports this hypothesis.
Only two (1.8%; 95% CI: 0%, 4.2%) of 113 hands underwent repeat surgery. Because our study is cross-sectional, we were not able to determine if there was any significant deterioration in the Levine-Katz scores after the first year of surgery; however, 74% of patients reported their symptoms were completely better at the time of final follow-up. This is comparable with results from both short-term studies25,26 and mid-range studies with follow-up periods of two to seven years4,5,27,28.
The function scores for the fifty to fifty-nine-year age group were worse than those for other age groups, and these differences were significant (p = 0.035). These findings are not intuitive, given that the potential for nerve recovery tends to decline somewhat with age28. We conjecture that older patients may be more accepting of residual functional limitations and may have fewer physical demands. The main limitations to this retrospective study are the lack of preoperative data and the lack of controls. The lack of preoperative electrophysiologic data resulted in our being unable to determine if the amount of nerve damage varied widely among patients. Additionally, since we were not able to determine the reason why some patients declined to participate, it is possible that our method may have unintentionally led to the exclusion of patients who required repeat surgery. Long-term prospective studies would be useful to build on these findings. Another methodological limitation is that most data were self-reported. Finally, our human subjects research board did not permit a patient’s next-of-kin found either in the medical record or through other methods of searching to be contacted for this study, limiting our ability to locate a higher percentage of patients.
Our results suggest that the long-term results of open carpal tunnel release are excellent, with patients experiencing consistent pain relief over ten to fifteen years. The rate of reoperation was very low, at 1.8%. A high percentage of patients reported excellent results, high levels of satisfaction, and improvements in their quality of life.
Appendix
Tables showing patient characteristics and the distribution of responses to items on the Levine-Katz symptom and function scales are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Tables showing patient characteristics and the distribution of responses to items on the Levine-Katz symptom and function scales
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Hankins CL, Brown MG, Lopez RA, Lee AK, Dang J, Harper RD. A 12-year experience using the Brown two-portal endoscopic procedure of transverse carpal ligament release in 14,722 patients: defining a new paradigm in the treatment of carpal tunnel syndrome. Plast Reconstr Surg. 2007 Dec;120(7):1911-21 [DOI] [PubMed] [Google Scholar]
- 2.DeStefano F, Nordstrom DL, Vierkant RA. Long-term symptom outcomes of carpal tunnel syndrome and its treatment. J Hand Surg Am. 1997 Mar;22(2):200-10 [DOI] [PubMed] [Google Scholar]
- 3.Kouyoumdjian JA, Morita MP, Molina AF, Zanetta DM, Sato AK, Rocha CE, Fasanella CC. Long-term outcomes of symptomatic electrodiagnosed carpal tunnel syndrome. Arq Neuropsiquiatr. 2003 Jun;61(2A):194-8 [DOI] [PubMed] [Google Scholar]
- 4.Katz JN, Fossel KK, Simmons BP, Swartz RA, Fossel AH, Koris MJ. Symptoms, functional status, and neuromuscular impairment following carpal tunnel release. J Hand Surg Am. 1995 Jul;20(4):549-55 [DOI] [PubMed] [Google Scholar]
- 5.Semple JC, Cargill AO. Carpal-tunnel syndrome. Results of surgical decompression. Lancet. 1969 May 3;1(7601):918-9 [DOI] [PubMed] [Google Scholar]
- 6.Haupt WF, Wintzer G, Schop A, Löttgen J, Pawlik G. Long-term results of carpal tunnel decompression. Assessment of 60 cases. J Hand Surg Br. 1993 Aug;18(4):471-4 [DOI] [PubMed] [Google Scholar]
- 7.Nancollas MP, Peimer CA, Wheeler DR, Sherwin FS. Long-term results of carpal tunnel release. J Hand Surg Br. 1995 Aug;20(4):470-4 [DOI] [PubMed] [Google Scholar]
- 8.Kabuto Y, Senda M, Hashizume H, Kinoshita A, Inoue H. Time course changes of nerve conduction velocity in idiopathic carpal tunnel syndrome after endoscopic surgery. Acta Med Okayama. 2001 Jun;55(3):185-91 [PubMed] [Google Scholar]
- 9.Schlagenhauff RE, Glasauer FE. Pre- and postoperative electromyographic evaluations in the carpal tunnel syndrome. J Neurosurg. 1971 Sep;35(3):314-9 [DOI] [PubMed] [Google Scholar]
- 10.Nolan WB, 3rd, Alkaitis D, Glickel SZ, Snow S. Results of treatment of severe carpal tunnel syndrome. J Hand Surg Am. 1992 Nov;17(6):1020-3 [DOI] [PubMed] [Google Scholar]
- 11.Finestone HM, Woodbury GM, Collavini T, Marchuk Y, Maryniak O. Severe carpal tunnel syndrome: clinical and electrodiagnostic outcome of surgical and conservative treatment. Muscle Nerve. 1996 Feb;19(2):237-9 [DOI] [PubMed] [Google Scholar]
- 12.King PJ, Malin AS, Scott RD, Thornhill TS. The fate of patients not returning for follow-up five years after total knee arthroplasty. J Bone Joint Surg Am. 2004 May;86-A(5):897-901 [DOI] [PubMed] [Google Scholar]
- 13.Lovell ME, Morcuende JA. Patient location strategies for pediatric long-term follow-up studies. Iowa Orthop J. 2006;26:91-5 [PMC free article] [PubMed] [Google Scholar]
- 14.Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, Katz JN. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993 Nov;75(11):1585-92 [DOI] [PubMed] [Google Scholar]
- 15.Katz JN, Gelberman RH, Wright EA, Lew RA, Liang MH. Responsiveness of self-reported and objective measures of disease severity in carpal tunnel syndrome. Med Care. 1994 Nov;32(11):1127-33 [DOI] [PubMed] [Google Scholar]
- 16.Katz JN, Keller RB, Simmons BP, Rogers WD, Bessette L, Fossel AH, Mooney NA. Maine Carpal Tunnel Study: outcomes of operative and nonoperative therapy for carpal tunnel syndrome in a community-based cohort. J Hand Surg Am. 1998 Jul;23(4):697-710 [DOI] [PubMed] [Google Scholar]
- 17.Katz JN, Punnett L, Simmons BP, Fossel AH, Mooney N, Keller RB. Workers’ compensation recipients with carpal tunnel syndrome: the validity of self-reported health measures. Am J Public Health. 1996 Jan;86(1):52-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003 Apr 15;49(2):156-63 [DOI] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atroshi I, Hofer M, Larsson GU, Ornstein E, Johnsson R, Ranstam J. Open compared with 2-portal endoscopic carpal tunnel release: a 5-year follow-up of a randomized controlled trial. J Hand Surg Am. 2009 Feb;34(2):266-72 [DOI] [PubMed] [Google Scholar]
- 21.Trumble TE, Diao E, Abrams RA, Gilbert-Anderson MM. Single-portal endoscopic carpal tunnel release compared with open release: a prospective, randomized trial. J Bone Joint Surg Am. 2002 Jul;84(7):1107-15 [DOI] [PubMed] [Google Scholar]
- 22.Ferdinand RD, MacLean JG. Endoscopic versus open carpal tunnel release in bilateral carpal tunnel syndrome. A prospective, randomised, blinded assessment. J Bone Joint Surg Br. 2002 Apr;84(3):375-9 [DOI] [PubMed] [Google Scholar]
- 23.Jacobsen MB, Rahme H. A prospective, randomized study with an independent observer comparing open carpal tunnel release with endoscopic carpal tunnel release. J Hand Surg Br. 1996 Apr;21(2):202-4 [DOI] [PubMed] [Google Scholar]
- 24.Pensy RA, Burke FD, Bradley MJ, Dubin NH, Wilgis EF. A 6-year outcome of patients who cancelled carpal tunnel surgery. J Hand Surg Eur Vol. 2011 Oct;36(8):642-7 [DOI] [PubMed] [Google Scholar]
- 25.Brown RA, Gelberman RH, Seiler JG, 3rd, Abrahamsson SO, Weiland AJ, Urbaniak JR, Schoenfeld DA, Furcolo D. Carpal tunnel release. A prospective, randomized assessment of open and endoscopic methods. J Bone Joint Surg Am. 1993 Sep;75(9):1265-75 [DOI] [PubMed] [Google Scholar]
- 26.Kluge W, Simpson RG, Nicol AC. Late complications after open carpal tunnel decompression. J Hand Surg Br. 1996 Apr;21(2):205-7 [DOI] [PubMed] [Google Scholar]
- 27.Kulick MI, Gordillo G, Javidi T, Kilgore ES, Jr, Newmayer WL., 3rd Long-term analysis of patients having surgical treatment for carpal tunnel syndrome. J Hand Surg Am. 1986 Jan;11(1):59-66 [DOI] [PubMed] [Google Scholar]
- 28.Rotman MB, Enkvetchakul BV, Megerian JT, Gozani SN. Time course and predictors of median nerve conduction after carpal tunnel release. J Hand Surg Am. 2004 May;29(3):367-72 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
Tables showing patient characteristics and the distribution of responses to items on the Levine-Katz symptom and function scales


