Among patients with type 2 diabetes, bariatric surgery has been the subject of considerable interest because of its favorable effects on glucose metabolism. Indeed, various procedures have been associated with high rates of diabetes remission (1), although the outcomes of these studies have been assessed in a heterogeneous manner (2). Despite the favorable results overall, there has been divergence among procedures regarding improvement of diabetes (1). This observation raises the possibility of identifying underlying mechanisms leading to improved glucose metabolism as a means to identify new diabetes treatments. The pathophysiology underlying development of type 2 diabetes includes defects in insulin secretion, disordered postprandial suppression of glucagon secretion, and defects in insulin action and glucose effectiveness (the ability of insulin and glucose to stimulate glucose uptake and suppress glucose release) (3). The heterogeneous effects of various forms of bariatric surgery on these parameters remain a topic of intense interest.
Roux-en-Y gastric bypass (RYGB) is currently the most common bariatric procedure. This surgical approach results in both gastric restriction and malabsorption. Increased delivery of calories to the jejunum/ileum increases enteroendocrine secretion, most notably that of glucagon-like peptide-1 (GLP-1) (4). Whether the increase in postprandial concentrations of GLP-1 is relevant to insulin secretion or gastrointestinal motility in ways that benefit glucose metabolism after gastric bypass is uncertain. GLP-1 increases insulin secretion and suppresses glucagon secretion. In an intact upper gastrointestinal tract, GLP-1 also delays gastric emptying (5) and increases gastric accommodation (6). However, it is uncertain if these actions are present after RYGB due to the alterations in upper gastrointestinal tract anatomy. Some studies have suggested that increased GLP-1 concentrations after RYGB contribute to insulin secretion, although the experimental conditions do not relate directly to actual postprandial conditions (7).
Bariatric surgery is associated with a rapid improvement in fasting glucose concentrations and insulin action (8). These changes occur early in the postoperative course and are independent of a significant change in weight (8). The same improvements are also observed in response to significant caloric restriction (600–800 kcal daily), suggesting that these benefits are not unique to bariatric surgery (9,10). Therefore, caloric restriction per se likely plays an important role in the favorable metabolic changes observed after bariatric surgery.
In this issue, Jackness et al. (11) compare the effect of a very low–calorie diet (VLCD) (500 kcal/day) and RYGB on β-cell function in type 2 diabetic patients during the first 3 weeks after intervention. Previously, the same group demonstrated that an 800 kcal/day diet produced less improvement in β-cell function compared with a matched cohort of subjects post-RYGB with equivalent weight reduction (12). The new study was undertaken to better control for differences in caloric consumption between the surgically treated and calorically restricted groups. Subjects with a history of type 2 diabetes scheduled to undergo RYGB and control subjects willing to maintain a VLCD were studied before and approximately 21 days after intervention using an insulin-modified, frequently sampled intravenous glucose tolerance test (fsIVGTT). The investigators reported that both groups achieved similar degrees of weight loss and that there were no significant differences in β-cell function between the groups. The authors concluded that caloric restriction was primarily responsible for the early effects of RYGB on glucose metabolism.
The investigators acknowledge that a significant limitation of their study was the use of an fsIVGTT to measure β-cell function. This approach does not account for potential influences of the incretin system on glucose metabolism (13). This is a significant weakness given the known effects of RYGB on incretin hormone concentrations. Another weakness is the potential carryover effects associated with glucose-lowering medications, which were stopped 2–3 days prior to the study. Furthermore, there is a dearth of information regarding how medication dosing changed over the duration of the study and whether any differences in treatment between the groups might have accounted for the end result.
Despite these limitations, there is some important information to be gleaned from this study as it creates conditions of controlled caloric intake and activity that mimic those in the immediate RYGB postoperative period. The authors suggest that none of the baseline function testing predicted the response to intervention as measured by changes in disposition indices and weight. This may be because the population under study had type 2 diabetes for a relatively short period of time (<6 years, self-reported) and their diabetes was controlled by relatively few agents and <60 units of insulin daily. While this limits generalizing the study’s conclusions to a broader population, the data imply that it is reasonable to expect improvement in β-cell function after a similar intervention in subjects with similar characteristics as those studied here. The study also reinforces the clinical suspicion that caloric restriction is a significant contributor to the rapid improvement in glucose metabolism observed after RYGB.
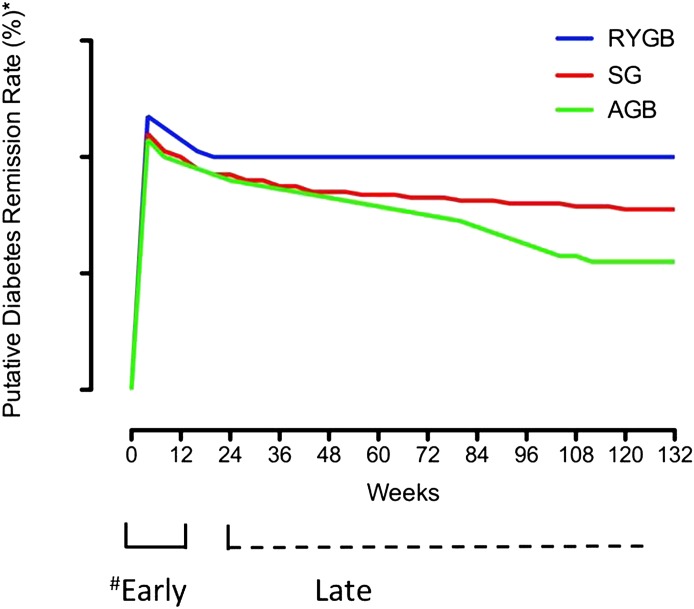
While two recent prospective, randomized, non-blinded studies concluded that bariatric surgery was superior to medical therapy alone in achieving glycemic control (14,15), there was significant heterogeneity in response. In the study by Schauer et al. (14), 12% of patients receiving medical therapy achieved an HbA1c <6% in contrast to 42% undergoing RYGB. While this is a significant difference in favor of RYGB compared with intensive therapy, less than half of the RYGB group achieved the (admittedly arbitrary) definition of remission from type 2 diabetes. The reasons for this heterogeneity in response to surgery and how to better predict an optimal response to bariatric procedures remain elusive. Intriguingly, while sleeve gastrectomy had similar rates of resolution to RYGB 1 year after intervention, at 24 months subjects with RYGB exhibited greater reduction in truncal fat and improvement in β-cell function compared with sleeve gastrectomy or medical therapy (16). Whether these differences are attributable to intestinal factors or merely reflect differing degrees and durability of restriction remain to be determined and warrant further study (Fig. 1).
FIG. 1.
Schematic representation of the time course for putative diabetes remission after various types of bariatric surgery. While it is probable that most of the “early” effects of bariatric surgery are produced by caloric restriction, it is possible/likely that other intestinal factors such as altered incretin secretion, bile acid malabsorption, and the degree of and durability of the surgically induced restriction may explain the durability of diabetes remission after surgery. *The definition of remission after surgery is arbitrary, and it is important to emphasize that the data represented here are partially gleaned from the literature and partly from clinical experience. They are intended to illustrate the suggestion that differing surgeries may have differing success in maintaining a durable diabetes remission. #Arbitrarily defined as 12 weeks. SG, sleeve gastrectomy; AGB, adjustable gastric banding.
ACKNOWLEDGMENTS
A.V. has received support from the Mayo Clinic CTSA (RR24150), and DK-78646 and DK-82396 grants.
A.V. has been the recipient of investigator-initiated grants from Merck, Novartis, and Daiichi Sankyo in the past 5 years, and has consulted for XOMA, Sanofi, Merck, Bristol-Myers Squibb, and Novartis. No other potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 3027.
REFERENCES
- 1.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724–1737 [DOI] [PubMed] [Google Scholar]
- 2.Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care 2009;32:2133–2135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vella A, Camilleri M, Rizza RA. The gastrointestinal tract and glucose tolerance. Curr Opin Clin Nutr Metab Care 2004;7:479–484 [DOI] [PubMed] [Google Scholar]
- 4.Laferrère B, Teixeira J, McGinty J, et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab 2008;93:2479–2485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salehi M, Vahl TP, D’Alessio DA. Regulation of islet hormone release and gastric emptying by endogenous glucagon-like peptide 1 after glucose ingestion. J Clin Endocrinol Metab 2008;93:4909–4916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delgado-Aros S, Kim DY, Burton DD, et al. Effect of GLP-1 on gastric volume, emptying, maximum volume ingested, and postprandial symptoms in humans. Am J Physiol Gastrointest Liver Physiol 2002;282:G424–G431 [DOI] [PubMed] [Google Scholar]
- 7.Salehi M, Prigeon RL, D’Alessio DA. Gastric bypass surgery enhances glucagon-like peptide 1-stimulated postprandial insulin secretion in humans. Diabetes 2011;60:2308–2314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wickremesekera K, Miller G, Naotunne TD, Knowles G, Stubbs RS. Loss of insulin resistance after Roux-en-Y gastric bypass surgery: a time course study. Obes Surg 2005;15:474–481 [DOI] [PubMed] [Google Scholar]
- 9.Kelley DE, Wing R, Buonocore C, Sturis J, Polonsky K, Fitzsimmons M. Relative effects of calorie restriction and weight loss in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 1993;77:1287–1293 [DOI] [PubMed] [Google Scholar]
- 10.Wadden TA, Foster GD, Letizia KA, Stunkard AJ. A multicenter evaluation of a proprietary weight reduction program for the treatment of marked obesity. Arch Intern Med 1992;152:961–966 [PubMed] [Google Scholar]
- 11.Jackness C, Karmally W, Febres G, et al. Very low–calorie diet mimics the early beneficial effect of Roux-en-Y gastric bypass on insulin sensitivity and β-cell function in type 2 diabetic patients. Diabetes 2013;. 62:3027–3032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plum L, Ahmed L, Febres G, et al. Comparison of glucostatic parameters after hypocaloric diet or bariatric surgery and equivalent weight loss. Obesity (Silver Spring) 2011;19:2149–2157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campioni M, Toffolo G, Shuster LT, Service FJ, Rizza RA, Cobelli C. Incretin effect potentiates beta-cell responsivity to glucose as well as to its rate of change: OGTT and matched intravenous study. Am J Physiol Endocrinol Metab 2007;292:E54–E60 [DOI] [PubMed] [Google Scholar]
- 14.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012;366:1567–1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med 2012;366:1577–1585 [DOI] [PubMed] [Google Scholar]
- 16.Kashyap SR, Bhatt DL, Wolski K, et al. Metabolic effects of bariatric surgery in patients with moderate obesity and type 2 diabetes: analysis of a randomized control trial comparing surgery with intensive medical treatment. Diabetes Care 2013;36:2175–2182 [DOI] [PMC free article] [PubMed] [Google Scholar]