I am very fortunate to be the recipient of the 2010 Bakken Institute Pioneer Award and feel especially honored to have my lifetime work recognized in this way. When informed that I was this year’s recipient, it prompted me to reflect on the meaning of the term “pioneer,” and how it related to me.
What is a pioneer?
According to Webster’s Dictionary, a pioneer is defined as (a) one who ventures into unknown or unclaimed territory to settle; and (b) one who opens up new areas of thought, research, or development. One requirement for any pioneer is that there is a frontier to explore. Thirty years ago, my colleagues and I began our investigations into cardiac rehabilitation (CR), which at the time we considered to be a new frontier for behavioral medicine (1).
Exercise-based cardiac rehabilitation
Historically, patients who suffered an acute myocardial infarction (MI) were often discouraged from engaging in physical activity; patients were initially prescribed prolonged bed rest and told to avoid strenuous exercise (2) (Figure 1). In the early 1950s, arm chair therapy was proposed (3) as an initial attempt to mobilize patients after a coronary event. Over the years, the value of physical exercise has been increasingly recognized and exercise is now considered to be the cornerstone of exercise-based CR (4–7). Today, exercise-based CR, involving aerobic exercise supplemented by resistance training, is offered by virtually all CR programs in the United States (8). Proper medical management is also emphasized, along with dietary modification and smoking cessation, but exercise is the centerpiece of treatment.
Figure 1.
In the early days, patients were discouraged from any form of physical activity after a coronary event.
Exercise has been shown to reduce traditional risk factors such as hypertension and hyperlipidemia (8), attenuate cardiovascular responses to mental stress (9), and reduce myocardial ischemia (10–12). Although no single study has demonstrated definitively that exercise reduces morbidity in patients with coronary heart disease (CHD), pooling data across clinical trials has shown that exercise may reduce risk of fatal CHD events by 25% (13). A recent, comprehensive meta analysis by Jolliffe et al. (14) reported a 27% reduction in all cause mortality and 31% reduction in cardiac mortality.
Not only is exercise considered beneficial for medical outcomes, but is also recognized as being important for improving quality of life. Indeed, there has been increased interest in the value of exercise for improving not just physical health, but also for improving mental health (15–17). The mental health benefits of exercise are especially relevant for cardiac patients, as there is a growing literature documenting the importance of mental health, and, in particular the prognostic significance of depression, in patients with CHD.
Psychosocial Risk Factors: The Role of Depression and Coronary Heart Disease
There has long been an interest in psychosocial factors that contribute to the development and progression of CHD. More than 3 decades ago, researchers identified the Type A behavior pattern as a risk factor for CHD (18). When subsequent studies failed to confirm the association of Type A and adverse health outcomes, researchers turned their attention to other possible psychosocial risk factors, including anger and hostility (19), low social support (20), and most recently, depression (21). Indeed, the most consistent and compelling evidence is that clinical depression or elevated depressive symptoms in the presence of CHD place individuals at increased risk for fatal and non-fatal cardiac events and for increased risk of all cause mortality (22).
Major depressive disorder (MDD) is a widespread and often chronic condition. Lifetime incidence estimates for MDD are approximately 12% in men and 20% in women (23). In addition, MDD is marked by high rates of relapse with 22–50% of patients suffering recurrent episodes within 6 months after recovery (24). Furthermore, MDD is under-recognized and under-treated in older adults (25), CHD patients, and especially minorities (26–28).
Cross-sectional studies have documented a higher prevalence of depression in CHD patients than in the general population. Point estimates range from 14% to as high as 47%, with higher rates recorded most often in patients with unstable angina, heart failure, and patients awaiting coronary artery bypass graft (CABG) surgery (29–36).
A number of prospective studies have found that depression is associated with increased risk for mortality or non-fatal cardiac events in a variety of CHD populations. The most compelling evidence for depression as a risk factor has come from the studies from Montreal, Canada. In an initial report, Frasure-Smith and colleagues (31) followed 222 AMI patients in which 35 patients were diagnosed with MDD at the time of hospitalization; there were 12 deaths (6 depressed and 6 non-depressed) over an initial 6 month follow-up period, resulting in greater than a 5-fold greater risk of death for depressed patients compared to non-depressed patients (Hazard Ratio = 5.7 95% CI, 4.6 – 6.9). In a subsequent report (36), in which 896 AMI patients were followed for one year, the presence of elevated depressive symptoms was associated with more than a 3-fold increased risk in cardiac mortality after controlling for other multivariate predictors of mortality (OR= 3.29 for women; 3.05 for men).
Studies of patients with stable CHD also have reported significant associations between the presence of depression and worse clinical outcomes. For example, Barefoot et al. (37) assessed 1250 patients with documented CHD using the Zung self-report depression scale at the time of diagnostic coronary angiography and followed patients for up to 19.4 years. Results showed that patients with moderate to severe depression were at 69% greater risk for cardiac death and 78% greater risk for all-cause death.
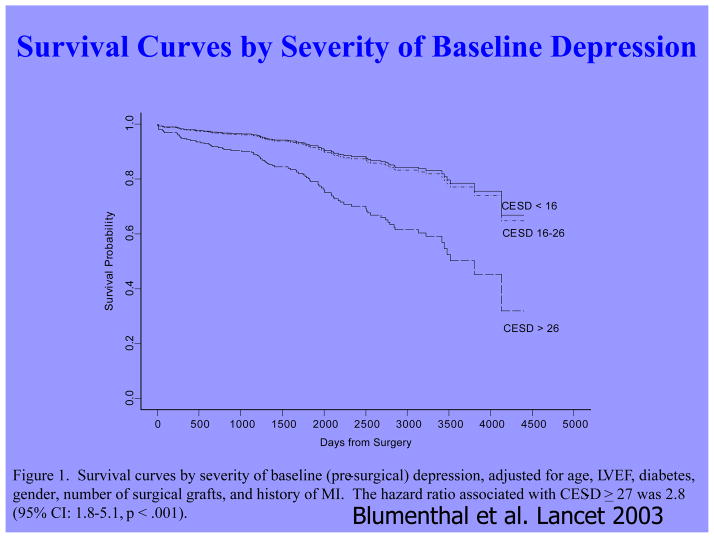
The presence of depression also has been shown to be associated with worse clinical outcomes in patients undergoing coronary bypass surgery (CABG) (33,38–40). For example, Duke researchers (39) assessed the effect of depression on mortality after CABG surgery in 817 patients followed for up to 12 years (mean=5.2 years). Patients with moderate to severe depression at the time of surgery were found to have a 2–3-fold increased risk of death, even after statistically controlling for age, gender, number of grafts, diabetes, smoking, left ventricular ejection fraction, and history of AMI (Figure 2).
Figure 2.
Patients with significant depressive symptoms assessed by the Center for Epidemiological Studies-Depression scale (CES-D) were at increased risk of dying up to 12 years after they underwent CABG surgery. From Blumenthal et al. Lancet, 2003.
Patients with HF represent a particularly vulnerable group; a meta analysis of depression in HF patients suggested that 1 in 5 patients are clinically depressed (range 9–60%) (41). Not only is depression in HF patients associated with worse outcomes (42–46), but recent evidence suggests that worsening of depressive symptoms, independent of clinical status, is related to worse outcomes. Sherwood et al. (46) demonstrated that increased symptoms of depression, as indicated by higher scores on the Beck Depression Inventory (BDI) over a 1-year interval (BDI change (1-point) Hazard Ratio=1.07; 95% CI 1.02–1.12; p=.007), were associated with higher risk of death or cardiovascular hospitalization after controlling for baseline depression (baseline BDI Hazard Ratio = 1.1; 95% CI 1.06–1.14, p<.001) and established risk factors, including HF etiology, age, EF, NT-proBNP, and prior hospitalizations. Consequently, strategies to reduce depressive symptoms and prevent the worsening of depression may have important implications for improving cardiac health as well as for enhancing quality of life.
Mechanisms Linking Depression and CHD
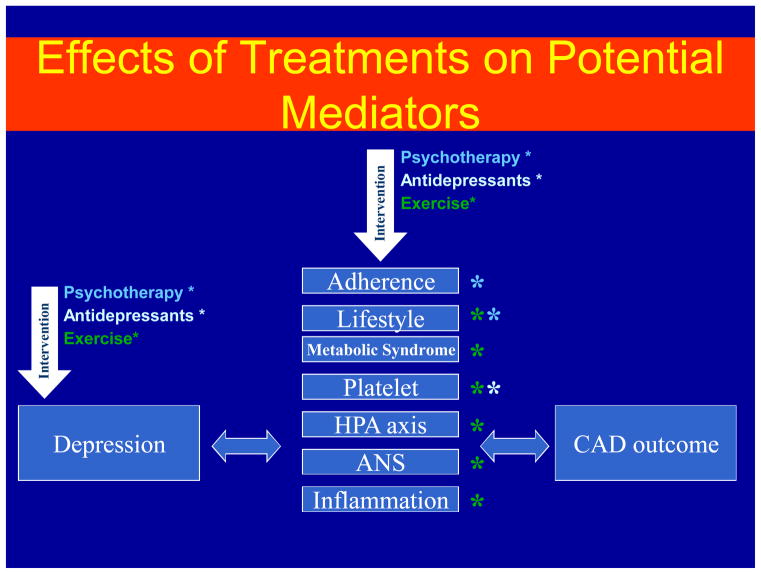
A number of biobehavioral mechanisms have been hypothesized to underlie the relationship between depression and CHD. There is evidence that depression is associated with traditional CHD risk factors such as hypertension, diabetes, and insulin resistance (47,48), as well as changes in platelet reactivity (49), dysregulation of the autonomic nervous system (50) and hypothalamic pituitary adrenal axis (51), and alterations in the immune response/inflammation (52). Depression is also associated with behavioral factors that are, in turn, associated with CHD risk, such as treatment adherence (53), smoking (54), heavy alcohol use, and physical inactivity (55). In considering strategies to maximize benefits in depressed cardiac patients, treatments that not only reduce depressive symptoms but also improve possible mediators responsible for the increased risk may hold particular promise (Figure 3).
Figure 3.
Proposed effects of different treatments for depression (Pharmacotherapy, Exercise, and Psychotherapy) on hypothesized mechanisms by which depression is associated with adverse clinical events in CHD patients.
Conventional Approaches the Treatment of Depression
Treatment of depression has focused on reduction of symptoms and restoration of functioning. Antidepressant medications are generally considered the treatment of choice (56). In particular, second-generation antidepressants such as selective serotonin reuptake inhibitors (SSRIs) are widely prescribed (57). Current treatment guidelines suggest 6–12 weeks of acute treatment followed by a continuation phase of 3–9 months to maintain therapeutic benefit (58). However, meta-analyses of antidepressant medications have reported only modest benefits over placebo treatments (59,60). In particular, drug-placebo differences in antidepressant efficacy are positively correlated with depression severity: antidepressants are often comparable to placebo in patients with low levels of depression but may be superior to placebo among patients with more severe depression. However, it has been suggested that this relationship may be due to the fact that placebo is less effective for more depressed patients rather than antidepressants being more effective for more depressed patients (59).
For acute treatment of MDD, approximately 60% of patients respond to second generation antidepressants (61), with a 40% relapse rate after 1 year (62). A recent meta analysis (60) with second generation antidepressants summarized 4 comparative trials and 23 placebo-controlled trials and found that second generation antidepressants were generally comparable to each other. Interestingly, despite the modest benefit of antidepressants, the percent of patients who have been treated for depression in the United States has increased from 0.73% in 1987 to 2.33% in 1997 while antidepressant use has increased from 37.3%in 1997 to 74.5% in 1997 (63). By 2007, however, the rates of outpatient treatment for depression have now increased to 2.88%. The percentage of treated patients who used antidepressants has remained at 73.8% since 1997, but declined from 53.% to 43.1% for psychotherapy (64). Moreover, the national expenditure for the outpatient treatment of depression increased from $10.05 billion to $12.45 billion in 2007, primarily driven by an increase in antidepressant expenditures.
Despite the compelling reasons for treating depression in cardiac patients, the clinical significance of treating depression in cardiac patients remains uncertain. To date, only the ENRICHD trial has examined the impact of treating depression in post-MI patients on “hard” clinical endpoints (65). Although more than 2400 patients were enrolled in the trial, the results were disappointing because there were only modest differences (i.e., 2-points on the HAM-D) in reductions of depressive symptoms in the group receiving cognitive behavior therapy (CBT) relative to usual care controls, and there were no treatment group differences in the primary outcome, all cause mortality and non-fatal cardiac events. It was noted that by the end of the follow-up period, 28.0% of patients in the CBT condition had received anti-depressant medication and 20.6% of patients in usual care also received antidepressants. Although a subsequent reanalysis of the ENRICHD study revealed that antidepressant use was associated with improved clinical outcomes (66), because patients were not randomized to medication treatment it could not be concluded that SSRI use was responsible for the improved outcomes.
In a randomized trial of patients with acute coronary syndrome known as the SADHART study (67), almost 400 patients were treated with an SSRI (sertraline) or placebo. Reductions in depressive symptoms were similar for patients receiving sertraline compared to placebo in the full sample, although a subgroup analysis revealed that patients with more severe depression (i.e., those patients who reported 2 or more previous episodes) benefitted more from sertraline compared to placebo. Interestingly, patients receiving sertraline tended to have more favorable cardiac outcomes, including a composite measure of both “hard” and “soft” clinical events, compared to placebo controls. These results suggested that antidepressant medication may improve underlying physiological processes, such as platelet function, independent of changes in depression (68). However, because SADHART was not powered to detect differences in clinical events, there remain unanswered questions about the clinical value of treating depression in cardiac patients with antidepressant medication.
In a second sertraline trial, SADHART-HF (69), 469 men and women with MDD and chronic systolic HF were randomized to either sertraline or placebo for 12 weeks of treatment. Participants were followed for a minimum of 6 months. Results showed that while sertraline was safe, treatment with sertraline did not result in greater reductions in depressive symptoms compared to placebo (−7.1 +0.5 v −6.8 +0.5) and there were no differences in clinical event rates between patients receiving sertraline compared to placebo controls.
It should be noted that in an observational study of patients with HF (44), medication use was associated with increased risk of mortality or hospitalization. Although the potential harmful effects of antidepressant medication could not be ruled out, a more likely interpretation is that antidepressant medication use was a marker for individuals with more severe depression, and that the underlying depression may have been responsible for their higher risk. Further, patients who are depressed, despite receiving treatment, may represent a subset of treatment-resistant patients who may be especially vulnerable to further cardiac events. Indeed, worsening depression is associated with worse outcomes in HF patients (46), which is consistent with data from the ENRICHD trial, which showed that patients receiving CBT (and, in some cases, anti-depressant medication) who failed to improve with treatment had higher mortality rates compared to patients who exhibited a positive response to treatment (70).
In a fourth randomized trial of CHD patients, the CREATE Trial (71) used a modified 2 (citalopram/placebo) by 2 (interpersonal therapy/clinical management) design in which 284 CHD patients with MDD and HAM-D rating scores ≥ 20 were randomized to 12 weeks of interpersonal therapy (IPT) plus clinical management (CM) or to CM only and 12 weeks of citalopram or matching placebo. The same interventionists delivered the CM and IPT, such that those patients assigned to IPT received IPT plus CM within the same (extended) session. Patients receiving citalopram had greater reductions in depressive symptoms compared to placebo, with a small to medium effect size of 0.33, and better remission rates compared to placebo (35.9% to 22.5% respectively). Unexpectedly, patients who received just CM tended to have greater improvements in depressive symptoms compared to patients who received IPT plus CM (p <0,07); no clinical CHD endpoints were assessed, however.
Taken together, these data illustrate that while antidepressant medications may reduce depressive symptoms for some patients, for a number of patients medication fails to adequately relieve depressive symptoms and may perform no better than placebo. Adverse effects also may affect a subgroup of patients and may be relatively more common or more problematic in older persons with CHD (72). Thus, there continues to be a need to identify alternative approaches for treating depression in cardiac patients. We believe that aerobic exercise, the cornerstone of traditional CR, may be one such approach: Exercise is safe for most cardiac patients (73,74), including patients with HF (75) and, if proven effective as a treatment for depression, exercise would hold a number of potential advantages over traditional medical therapies: it is relatively inexpensive, improves cardiovascular functioning, and avoids the side effects sometimes associated with medication use.
Exercise Therapy for Depression
Some studies of exercise treatments for CHD patients have tracked depressive symptoms and thus have provided information regarding the potential efficacy of exercise as a treatment for depression in this population (76–81). Although most of the previous studies in the area have reported significant improvements in depression after completion of an exercise program, many studies frequently had important methodological limitations, such as the absence of a control group. In one of the few controlled studies in this area Stern et al. (82) randomized 106 male patients with a recent AMI and elevated depression, anxiety, or low fitness to 12 weeks of exercise training, group therapy, or a usual care control group. At one-year follow-up, both the counseling and the exercise group showed improvements in depression relative to controls.
Cross-sectional studies of non-CHD samples have reported that active individuals obtain significantly lower depression scores on self-report measures than sedentary persons (83). Studies also have shown that aerobic exercise may reduce self-reported depressive symptoms in non-clinical populations and in patients diagnosed with MDD (83). In 2001, a meta analysis evaluating 11 randomized controlled trials of non-CHD patients with MDD (84) noted that studies were limited because of self-selection bias, absence of control groups or non-random controls, and inadequate assessment of exercise training effects, and concluded that “the effectiveness of exercise in reducing symptoms of depression cannot be determined because of a lack of good quality research on clinical populations with adequate follow up.”
A subsequent meta analysis (85) included 25 studies; for 23 trials (907 participants) comparing exercise with no treatment or a control intervention, the pooled SMD was −0.82 (95% CI-1.12, −0.51), indicating a large effect size. However, when only the three trials (216 participants) with adequate allocation concealment and intention to treat analysis and blinded outcome assessment were included, the pooled SMD was −0.43 (95% CI-0.88, 0.03), with a point estimate that was half the size of that with all trials. As a result, the authors concluded that “exercise seems to improve depressive symptoms in people with a diagnosis of depression, but when only the methodologically robust trials are included, the effect size is only moderate.”
To date, there have been no RCTs that have examined the effects of exercise on clinical outcomes in depressed cardiac patients. However, data from the ENRICHD trial suggest that exercise may reduce the rates of mortality and non-fatal reinfarction in patients with depression or socially isolated post-MI patients (86). Self-report data were used to categorize participants as exercising regularly or not exercising regularly. After controlling for medical and demographic variables, the magnitude of reduction in risk associated with regular exercise was nearly 40% for non-fatal reinfarction and 50% for mortality. The evidence that exercise improves depression, CHD risk factors, and CHD outcomes suggests that exercise may be a particularly promising intervention for depressed CHD patients.
Comparative Effectiveness of Exercise and Antidepressant Medication
In 2008, an Institute of Medicine (IOM) report called for a national initiative of research that would provide a basis for better decision making about how to best treat various medical conditions, including depression. In 2009, the American Reinvestment Recovery Act provided a major boost in funding CER. The act allotted $1.1 billion to support this form of research, which came to be known as comparative effectiveness research (CER). CER refers to the generation and synthesis of evidence that encompares the benefits and harms of altenative methods to prevent, diagnose, treat, and monitor a clinical condition, or to improve the delivery of care. The purpose of CER is to assist consumers, clinicians, purchasers, and policy makers to make informed decisions that will improve health care at both the individual and population levels (87).
Two broad categories of research have been used to inform decision making. Epidemiologic studies provide evidence linking various treatments with patient outcomes. However, these sources of data are limited because they seldom specify the basis for medical decisions and also fail to take into account patient characteristics that both affect clinical decisions and clinical outcomes. Indeed, it has been suggested that “overcoming the limitations of observational research is the most important frontier of research on study methods” p204. (88). Randomized clinical trials (RCTs) address this issue by randomly assigning patients to different treatment conditions. While this design may eliminate some of the uncertainty and potential confounders that characterize purely observational studies, most RCTs are efficacy studies in that patients are carefully selected and studies often compare one treatment against a placebo or usual care condition. While this design addresses the question of whether a given treatment is effective, it does not necessarily address questions that many physicians want to know: namely, is this treatment better than that treatment. Furthermore, physicians want to know if one treatment is more effective than another for a given patient. For example, Hlatky et al (89) showed that mortality rates for percutaneous coronary interventions (PCI) and CABG were comparable; however, mortality was significantly lower for patients >65 years while PCI was superior for patients <55 years old. Thus, examination of individual differences may also help to inform clinicians as to the optimal therapy for their particular patients.
The IOM committee sought advice from a broad range of stakeholders and prioritized areas for research. The top ranked topic was comparison of strategies to treat atrial fibrillation including surgery, catheter ablation, and pharmacologic treatment. Coming in at #98 was comparison of the effectiveness of different treatment strategies (e.g., psychotherapy, antidepressants, combination treatment with case management) for depression after MI on medication adherence, cardiovascular events, hospitalization, and death.
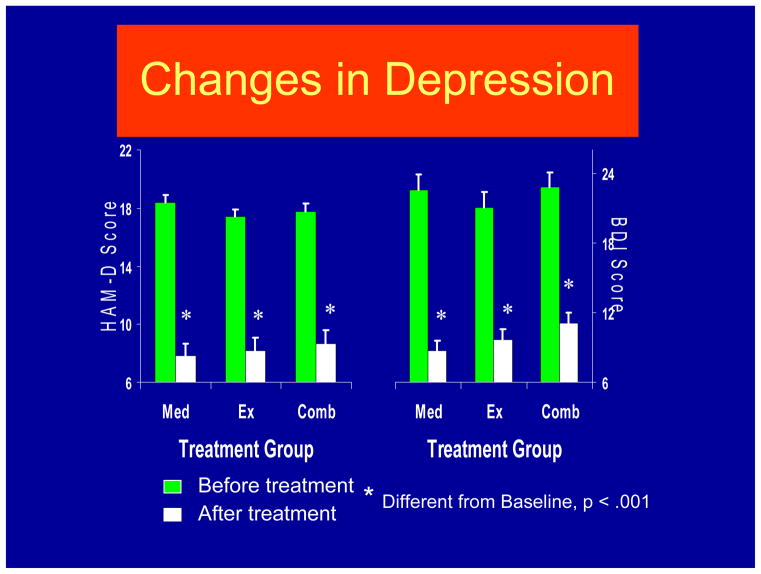
To date, there have been only two RCTs designed to compare exercise training to antidepressant medication. In an initial study, Blumenthal et al. (90) randomly assigned 156 middle-aged and older adults with DSM-IV MDD to one of three treatment conditions: 1) aerobic exercise training, 2) standard pharmacotherapy (sertraline) and 3) a combination of these treatments. After 16 weeks of treatment, groups did not differ significantly on percent remitted, self-reported depression severity (BDI), or clinician-rated depression severity (HAM-D). All treatment conditions demonstrated statistically and clinically significant reductions in depression (Figure 4). At 6-month follow-up, participants who remitted with exercise alone exhibited significantly lower relapse rates than remitted subjects in the medication or combination groups (91). Furthermore, there was an association between exercising during the follow-up period (regardless of initial treatment group) and reduced risk of depression diagnosis at 6 months post-treatment, such that 50 minutes of exercise per week was associated with a 50% reduction in risk.
Figure 4.
Changes in depressive symptoms measured by interview (HAM-D) and self-report (BDI) in patients who received sertraline (Med), exercise (Ex), or a combination of exercise and antidepressant medication (Comb). From Blumenthal et al. Arch Int Med 1999.
While the study provided encouraging results, it was limited by the absence of a no-treatment control group and by the fact that the exercise was conducted in a supervised setting, so that the effects of exercise may have been confounded by social support. A small RCT (92) also demonstrated that exercise was associated with reduced depression, independent of group support. Participants exercised alone in a secluded setting and a no-treatment control group was also included. However, only 53 out of 80 patients actually completed the 12 week trial, including only 5 of 13 no-treatment controls. Moreover, there was no active treatment comparison group, so that an estimate of comparative effectiveness could not be determined.
In a second Duke study that compared exercise and antidepressant medication (93), 202 adults (153 women; 49 men) diagnosed with MDD were randomly assigned to one of four conditions: supervised exercise in a group setting; home-based exercise; antidepressant medication (sertraline, 50–200 mg daily); or placebo pill for 16 weeks. Once again, patients underwent the Structured Clinical Interview for Depression (SCID) and completed the Hamilton Depression Rating Scale (HAM-D). After 4 months of treatment, 41% of participants achieved remission, defined as no longer meeting criteria for MDD and a HAM-D < 8. Patients receiving active treatments tended to have higher remission rates than placebo controls: Supervised exercise = 45%; Home-based exercise = 40%; Medication = 47%; Placebo = 31% (p = .057). All treatment groups had lower HAM-D scores after treatment; scores for the active treatment groups were not significantly different from the placebo group (p = .23). However, when immediate responders (i.e., those patients who reported >50% reduction in depressive symptoms after only 1 week of treatment) we excluded from the analysis, patients receiving active treatments (i.e., either the sertraline or exercise conditions) had greater reductions in depressive symptoms compared to placebo controls (p=.048). There was no difference between either exercise condition and antidepressant medications. We concluded that the efficacy of exercise appears generally comparable to antidepressant medication and both tend to be better than placebo in patients with MDD. Placebo response rates were high, suggesting that a considerable portion of the therapeutic response could be determined by patient expectations, ongoing symptom monitoring, attention, and other non-specific factors. Similar to our previous trial, participants who continued to exercise following the completion of the program were less likely to be depressed (94). While these results are preliminary and should be interpreted with caution, it would appear that exercise may be comparable to conventional antidepressant medication in reducing depressive symptoms, at least for patients who are willing to try it, and maintenance of exercise reduces the risk of relapse.
Summary
Three decades ago, we recognized that cardiac rehabilitation was a new frontier for behavioral medicine. We now know that successful rehabilitation of patients with CHD involves modification of lifestyle behaviors including smoking cessation, dietary modification and exercise. Exercise is no longer considered unsafe for most cardiac patients, and exercise is currently the key component of CR services. Research also has provided consistent evidence that depression is an important risk factor for CHD, although there is no consensus as to the optimal way to treat depression in CHD patients (95). Research on comparative effectiveness of established and alternative treatments for depressed cardiac patients is a new frontier for future pioneers in heart-brain medicine.
Acknowledgments
Supported by grants HL093374 and HL080664 from the National Heart, Lung, and Blood Institute. Based upon a presentation at the Cleveland Clinic Heart-Brain Summit, Las Vegas, NV, September 23, 2010
References
- 1.Blumenthal JA, Califf R, Williams RS, Hindman M. Cardiac rehabilitation: A new frontier for behavioral medicine. Journal of Cardiac Rehabilitation. 1983;3:637–656. [Google Scholar]
- 2.Lewis T. Diseases of the Heart. New York: Macmillan; 1933. pp. 41–49. [Google Scholar]
- 3.Levine SA, Lown B. The chair treatment of acute coronary thrombosis. Trans Assoc Am Physicians. 1951;64:316–327. [PubMed] [Google Scholar]
- 4.Cain HD, Frasher WG, Stivelman R. Graded activity program for safe return to self-care after myocardial infarction. JAMA. 1961;177:111–115. doi: 10.1001/jama.1961.03040280015005. [DOI] [PubMed] [Google Scholar]
- 5.Hellerstein HK, Ford AB. Rehabilitation of the cardiac patient. JAMA. 14:225–231. doi: 10.1001/jama.1957.02980030001001. [DOI] [PubMed] [Google Scholar]
- 6.Naughton J, Bruhn JG, Lategola MT. Effects of physical training on physiologic and behavioral characteristics of cardiac patients. Arch Phys Med Rehab. 1968;49:131–137. [PubMed] [Google Scholar]
- 7.O’Connor GT, Buring JE, Yusuf S, et al. An overview of randomized trials fo rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:234–244. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]
- 8.Wenger NK, Froelicher ES, Smith LK. Cardiac Rehabilitation: Clinical Practice Guideline No 17. Rockville, MD: US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research and the National Heart, Lung, and Blood Institute; 1995. [PubMed] [Google Scholar]
- 9.Blumenthal JA, Cox DR, Walsh MA, Emery CF, Kuhn CM, Williams RB, Williams RS. Exercise training in healthy Type A middle-aged men: Effects on behavioral and cardiovascular responses. Psychosomatic Medicine. 1988;50(4):418–433. doi: 10.1097/00006842-198807000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Schuler G, Schlierf G, Wirth A, Mautner HP, Scheurlen H, Thumm M, et al. Low-fat diet and regular, supervised physical exercise in patients with symptomatic coronary artery disease: reduction of stress-induced myocardial ischemia. Circulation. 1988;77(1):172–81. doi: 10.1161/01.cir.77.1.172. [DOI] [PubMed] [Google Scholar]
- 11.Jiang W, Trauner MA, Coleman RE, Waugh RA, Hanson MW, Frid DJ, et al. Association of physical fitness and transient myocardial ischemia in patients with coronary artery disease. J Cardiopulm Rehab. 1995;15(6):431–8. doi: 10.1097/00008483-199511000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Blumenthal JA, Jiang W, Babyak MA, Krantz DS, Frid DJ, Coleman RE, et al. Stress management and exercise training in cardiac patients with myocardial ischemia. Effects on prognosis and evaluation of mechanisms. Arch Int Med. 1997;157(19):2213–23. [PubMed] [Google Scholar]
- 13.Oldridge NB, Guyatt GH, Fisher ME, Rimm AA. Cardiac rehabilitation after myocardial infarction: Combined experience of randomized clinical trials. JAMA. 1988;260:945–950. [PubMed] [Google Scholar]
- 14.Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst. 2 [Google Scholar]
- 15.Folkins CH, Sime WE. Physical fitness training and mental health. American Psychologist. 1981;36(4):373–89. doi: 10.1037//0003-066x.36.4.373. [DOI] [PubMed] [Google Scholar]
- 16.Hughes JR. Psychological effects of habitual aerobic exercise: a critical review. Preventive Medicine. 1984;13(1):66–78. doi: 10.1016/0091-7435(84)90041-0. [DOI] [PubMed] [Google Scholar]
- 17.Plante T, Rodin J. Physical fitness and enhanced psychological health. Clin Psych: Res Rev. 1990;9:3–24. [Google Scholar]
- 18.Review Panel. Coronary-prone behavior and coronary heart disease: a critical review. The review panel on coronary-prone behavior and coronary heart disease. Circulation. 1981;63:1199–1215. doi: 10.1161/01.cir.63.6.1199. [DOI] [PubMed] [Google Scholar]
- 19.Smith TW. Hostility and health: current status of a psychosomatic hypothesis. Health Psychol. 1992;11:139–150. doi: 10.1037//0278-6133.11.3.139. [DOI] [PubMed] [Google Scholar]
- 20.Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, Sherwood A. Social support and coronary heart disease: Epidemiologic evidence and implications for treatment. Psychosom Med. 2005;67:869–878. doi: 10.1097/01.psy.0000188393.73571.0a. [DOI] [PubMed] [Google Scholar]
- 21.Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66:304–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 22.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCR-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 24.Belsher G, Costello CG. Relapse after recovery from unipolar depression: a critical review. Psychol Bull. 1988;104(1):84–96. doi: 10.1037/0033-2909.104.1.84. [DOI] [PubMed] [Google Scholar]
- 25.Strothers HS, Rust G, Minor P, et al. Disparities in antidepressant treatment in Medicaid elderly diagnosed with depression. J Am Geriatr Soc. 2005;53:456–461. doi: 10.1111/j.1532-5415.2005.53164.x. [DOI] [PubMed] [Google Scholar]
- 26.Simpson SM, Krishnan LL, Kunik ME, Ruiz P. Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatric Quarterly. 2007;78:3–14. doi: 10.1007/s11126-006-9022-y. [DOI] [PubMed] [Google Scholar]
- 27.Sclar DA, Robison LM, Skaer TL. Ethnicity/race and the diagnosis of depression and use of antidepressants by adults in the United States. Int Clin Psychopharmacol. 2008;23:106–109. doi: 10.1097/YIC.0b013e3282f2b3dd. [DOI] [PubMed] [Google Scholar]
- 28.Waldman SV, Blumenthal JA, Babyak MA, Sherwood A, Sketch M, Davidson J, Watkins LL. Ethnic differences in the psychopharmacologic treatment of depression in patients with ischemic heart disease. American Heart Journal. 2009;57:77–83. doi: 10.1016/j.ahj.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carney RM, Rich MW, Freedland KE, Saini J, Tevelde A, Simeone C, et al. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med. 1988;50(6):627–33. doi: 10.1097/00006842-198811000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Schleifer SJ, Macari-Hinson MM, Coyle DA, et al. The nature and course of depression following myocardial infarction. Arch Intern Med. 1989;149(8):1785–9. [PubMed] [Google Scholar]
- 31.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270(15):1819–25. [PubMed] [Google Scholar]
- 32.Gonzalez MB, Snyderman TB, Colket JT, Arias RM, Jiang JW, O’Connor CM, et al. Depression in patients with coronary artery disease. Depression. 1996;4(2):57–62. doi: 10.1002/(SICI)1522-7162(1996)4:2<57::AID-DEPR3>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 33.Connerney I, Shapiro PA, McLaughlin JS, Bagiella E, Sloan RP. Relation between depression after coronary artery bypass surgery and 12-month outcome: a prospective study. Lancet. 2001;358:1766–71. doi: 10.1016/S0140-6736(01)06803-9. [DOI] [PubMed] [Google Scholar]
- 34.Burker EJ, Blumenthal JA, Feldman M, Burnett R, White W, Smith LR, et al. Depression in male and female patients undergoing cardiac surgery. Br J Clin Psychol. 1995;34(Pt 1):119–28. doi: 10.1111/j.2044-8260.1995.tb01444.x. [DOI] [PubMed] [Google Scholar]
- 35.Lesperance F, Frasure-Smith N, Juneau M, Theroux P. Depression and 1-year prognosis in unstable angina. Arch Intern Med. 2000;160(9):1354–60. doi: 10.1001/archinte.160.9.1354. [DOI] [PubMed] [Google Scholar]
- 36.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 37.Barefoot JC, Helms MJ, Mark DB, Blumenthal JA, Califf RM, Haney TL, et al. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol. 1996;78:613–7. doi: 10.1016/s0002-9149(96)00380-3. [DOI] [PubMed] [Google Scholar]
- 38.Burg MM, Benedetto C, Soufer R. Depressive symptoms and mortality two years after coronary artery bypass graft surgery (CABG) in men. Psychosom Med. 2003;65:508–10. doi: 10.1097/01.psy.0000077509.39465.79. [DOI] [PubMed] [Google Scholar]
- 39.Blumenthal JA, Lett H, Babyak M, White W, Smith P, Mark D, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362:604–9. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 40.Connerney I, Sloan RP, et al. Depression is associated with increased mortality 10 years after coronary artery bypass surgery. Psychosom Med. 2010;72:874–881. doi: 10.1097/PSY.0b013e3181f65fc1. [DOI] [PubMed] [Google Scholar]
- 41.Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure: a meta analytic review of prevalence, intervention effects, and association with clinical outcomes. JACC. 2006;48:1526–37. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 42.Murberg TA, Furze G. Depressive symptoms and mortality in patients with congestive heart failure: a six-year follow-up study. Med Sci Monit. 2004;10:CR643–8. [PubMed] [Google Scholar]
- 43.Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–56. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 44.Sherwood A, Blumenthal JA, Trivedi R, Johnson KS, et al. Relationship of depression to mortality and hospitalization in patients with heart failure. Arch Int Med. 2007;167:367–373. doi: 10.1001/archinte.167.4.367. [DOI] [PubMed] [Google Scholar]
- 45.Frasure-Smith N, Lesperance F, et al. Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation. 2009;120:134–140. doi: 10.1161/CIRCULATIONAHA.109.851675. [DOI] [PubMed] [Google Scholar]
- 46.Sherwood A, Blumenthal JA, et al. Worsening depressive symptoms are associated with adverse clinical outcomes in patients with heart failure. JACC. 2011;57:418–23. doi: 10.1016/j.jacc.2010.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 48.Thakore JH, Richards PJ, Reznek RH, Martin A, Dinan TG. Increased intra-abdominal fat deposition in patients with major depressive illness as measured by computed tomography. Biological Psychiatry. 1997;41:1140–2. doi: 10.1016/S0006-3223(97)85394-2. [DOI] [PubMed] [Google Scholar]
- 49.Musselman DL, Tomer A, Manatunga AK, Knight BT, Porter MR, Kasey S, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry. 1996;153:1313–7. doi: 10.1176/ajp.153.10.1313. [DOI] [PubMed] [Google Scholar]
- 50.Delgado PL, Moreno FA. Role of norepinephrine in depression. Journal of Clinical Psychiatry. 2000;61:5–12. [PubMed] [Google Scholar]
- 51.Akil H, Haskett RF, Young EA, Grunhaus L, Kotun J, Weinberg V, et al. Multiple HPA profiles in endogenous depression: effect of age and sex on cortisol and beta-endorphin. Biol Psychiatry. 1993;33(2):73–85. doi: 10.1016/0006-3223(93)90305-w. [DOI] [PubMed] [Google Scholar]
- 52.Kop WJ, Gottdiener JS, Tangen CM, Fried LP, McBurnie MA, Walston J, et al. Inflammation and coagulation factors in persons > 65 years of age with symptoms of depression but without evidence of myocardial ischemia. Am J Cardiology. 2002;89:419–24. doi: 10.1016/s0002-9149(01)02264-0. [DOI] [PubMed] [Google Scholar]
- 53.Carney RM, Freedland KE, Eisen SA, Rich MW, Jaffe AS. Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychology. 1995;14:88–90. doi: 10.1037//0278-6133.14.1.88. [DOI] [PubMed] [Google Scholar]
- 54.Lehto S, Koukkunen H, Hintikka J, Viinamaki H, Laakso M, Pyorala K. Depression after coronary heart disease events. Scand Cardiovas J. 2000;34(6):580–3. doi: 10.1080/140174300750064512. [DOI] [PubMed] [Google Scholar]
- 55.Camacho TC, Roberts RE, Lazarus NB, Kaplan GA, Cohen RD. Physical activity and depression: evidence from the Alameda County Study. Am J Epidemiol. 1991;134(2):220–31. doi: 10.1093/oxfordjournals.aje.a116074. [DOI] [PubMed] [Google Scholar]
- 56.Depression Guideline Panel. Treatment of Depression, Clinical Practice Guideline, No 5. Vol. 2. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, HHCPR; 1993. Depression in Primary Care. [Google Scholar]
- 57.Anderson IM, Ferrier NI, Baldwin CR, et al. Evidence based guidelines for treating depressive disorders with antidepressants. J Psychopharm. 1008;22:330–332. doi: 10.1177/0269881107088441. [DOI] [PubMed] [Google Scholar]
- 58., American Psyciatric Association. Practice Guideline for the treatment of pateints with major depressive disorder (revision) Am J Psychiatr. 2000;157:1–45. [PubMed] [Google Scholar]
- 59.Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the food and drug administration. PLOS Medicine. 2008;5:260–268. doi: 10.1371/journal.pmed.0050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hansen R, Gaynes B, Thieda P, et al. Meta-analysis of major depressive disorder relapse and recurrence with second generation antidepressants. Psychiatr Serv. 2008;59:1121–1129. doi: 10.1176/appi.ps.59.10.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hansen RA, Gartlehner G, Lohr KN, et al. Efficacy and safety of second-geneartion antidepressants in the treatment of major depressive disorder. Ann Int Med. 2005;143:415–426. doi: 10.7326/0003-4819-143-6-200509200-00006. [DOI] [PubMed] [Google Scholar]
- 62.Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer term outcomes in depressed outpatients requiareing one or several treatment stepsL a STAR*D report. Am J Psychiat. 2006;163:19005–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 63.Olfson M, Marcus SC, et al. National trends in the outpatient treatment of depression. JAMA. 2002;287:203–9. doi: 10.1001/jama.287.2.203. [DOI] [PubMed] [Google Scholar]
- 64.Marcus SC, Olfson M. National trends int eh treatment of depression from 1998 to 2007. Arch Gen Psychiat. 1010;67:1265–1273. doi: 10.1001/archgenpsychiatry.2010.151. [DOI] [PubMed] [Google Scholar]
- 65.Writing committee for the ENRICHD investigators. Effects of treating depression and low social support on clinical events after myocardial infarction: The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. JAMA. 2003;289:3106–16. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 66.Taylor CB, Youngblood ME, Catellier D, Veith RC, Carney RM, Burg MM, Kaufmann PG, Shuster J, Mellman T, Blumenthal JA, Krishnan R, Jaffe AS ENRICHD Investigators. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry. 2005;62:792–798. doi: 10.1001/archpsyc.62.7.792. [DOI] [PubMed] [Google Scholar]
- 67.Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Jr, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–9. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 68.Serebruany VL, Glassman AH, Malinin AI, Nemeroff CB, Musselman DL, van Zyl LT, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the Sertraline Anti-Depressant Heart Attack Randomized Trial (SADHART) Platelet Substudy. Circulation. 2003;108:939–44. doi: 10.1161/01.CIR.0000085163.21752.0A. [DOI] [PubMed] [Google Scholar]
- 69.O’Connor CM, Jiang W, Kuchibhatla M, et al. Safety and efficacy of sertraline for depression in patients with heart failure. JACC. 2010;56:692–9. doi: 10.1016/j.jacc.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carney RM, Blumenthal JA, Freedland KE, Youngblood M, Veith RC, Burg MM, et al. Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study. Psychosom Med. 2004;66:466–74. doi: 10.1097/01.psy.0000133362.75075.a6. [DOI] [PubMed] [Google Scholar]
- 71.Lesperance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: The Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) Trial. JAMA. 2007;297:367–379. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 72.Salzman C, Schneider L, Alexopoulos GS. Pharmacological treatment of depression in late life. In: Bloon F, Kupfer D, editors. Psychopharmacology: Fourth Generation of Progress. New York: Raven Press; 1995. [Google Scholar]
- 73.Franklin BA, Bonzheim K, Gordon S, Timmis GC. Safety of medically supervised outpatient cardiac rehabilitation exercise therapy: a 16-year follow-up. Chest. 1998;114(3):902–6. doi: 10.1378/chest.114.3.902. [DOI] [PubMed] [Google Scholar]
- 74.Vongvanich P, Paul-Labrador MJ, Merz CN. Safety of medically supervised exercise in a cardiac rehabilitation center. Am J Cardiology. 1996;77:1383–5. doi: 10.1016/s0002-9149(96)00215-9. [DOI] [PubMed] [Google Scholar]
- 75.O’Connor CM, Whellan DJ, et al. Efficacy and safety of exercise training in patients with chronic heart failure. JAMA. 2010;302:1439–1540. doi: 10.1001/jama.2009.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Milani RV, Lavie CJ, Cassidy MM. Effects of cardiac rehabilitation and exercise training programs on depression in patients after major coronary events 8. Am Heart J. 1996;132(4):726–32. doi: 10.1016/s0002-8703(96)90304-x. [DOI] [PubMed] [Google Scholar]
- 77.Beniamini Y, Rubenstein JJ, Zaichkowsky LD, Crim MC. Effects of high-intensity strength training on quality-of-life parameters in cardiac rehabilitation patients. Am J Cardiol. 1997;80(7):841–6. doi: 10.1016/s0002-9149(97)00533-x. [DOI] [PubMed] [Google Scholar]
- 78.Maines TY, Lavie CJ, Milani RV, Cassidy MM, Gilliland YE, Murgo JP. Effects of cardiac rehabilitation and exercise programs on exercise capacity, coronary risk factors, behavior, and quality of life in patients with coronary artery disease 331. South Med J. 1997;90(1):43–9. doi: 10.1097/00007611-199701000-00010. [DOI] [PubMed] [Google Scholar]
- 79.Milani RV, Lavie CJ. Prevalence and effects of cardiac rehabilitation on depression in the elderly with coronary heart disease 341. Am J Cardiol. 1998;81(10):1233–6. doi: 10.1016/s0002-9149(98)00121-0. [DOI] [PubMed] [Google Scholar]
- 80.Blumenthal JA, Emery CF, Rejeski WJ. The effects of exercise training on psychosocial functioning after myocardial infarction. J Cardpulm Rehabil. 1988;8(5):183–93. [Google Scholar]
- 81.Taylor CB, Houston-Miller N, Ahn DK, Haskell W, DeBusk RF. The effects of exercise training programs on psychosocial improvement in uncomplicated postmyocardial infarction patients. J Psychosom Res. 1986;30(5):581–7. doi: 10.1016/0022-3999(86)90031-0. [DOI] [PubMed] [Google Scholar]
- 82.Stern MJ, Gorman PA, Kaslow L. The group counseling v exercise therapy study. A controlled intervention with subjects following myocardial infarction. Arch Intern Med. 1983;143(9):1719–25. [PubMed] [Google Scholar]
- 83.Brosse AL, Sheets ES, Lett HS, Blumenthal JA. Exercise and the treatment of clinical depression in adults: recent findings and future directions. Sports Med. 2002;32(12):741–60. doi: 10.2165/00007256-200232120-00001. [DOI] [PubMed] [Google Scholar]
- 84.Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomised controlled trials. BMJ. 2001;322(7289):763–7. doi: 10.1136/bmj.322.7289.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mead GE, Morley W, Campbell P, Greig CA, McMurdo M, Lawlor DA. Exercise for depression. Cochrane Database Syst Rev. 2009;(3):CD004366. doi: 10.1002/14651858.CD004366.pub4. [DOI] [PubMed] [Google Scholar]
- 86.Blumenthal JA, Babyak MA, et al. Exercise, depression, and mortality after myocardial infarction in the ENRICHD trial. Med Sci Sports Ex. 2004;36:746–755. doi: 10.1249/01.mss.0000125997.63493.13. [DOI] [PubMed] [Google Scholar]
- 87.Institute of Medicine. Knowing What Works in Health Care. In: Eden J, Wheatley B, McNeil B, Sox H, editors. A Roadmap for the Nation. Washington DC: National Academics Press; 2009. [Google Scholar]
- 88.Sox HC, Greenfield S. Comparative effectiveness research: A report from the Institute of Medicine. Ann Int Med. 2009;151:203–5. doi: 10.7326/0003-4819-151-3-200908040-00125. [DOI] [PubMed] [Google Scholar]
- 89.Hlatky MA, Boothroyd DB, Bravata DM. Coronary artery bypass compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomized trials. Lancet. 2009;373:1190–7. doi: 10.1016/S0140-6736(09)60552-3. [DOI] [PubMed] [Google Scholar]
- 90.Blumenthal JA, Babyak MA, Moore KA, et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999;159:2349–56. doi: 10.1001/archinte.159.19.2349. [DOI] [PubMed] [Google Scholar]
- 91.Babyak M, Blumenthal JA, Herman S, Khatri P, Doraiswamy M, Moore K, Craighead WE, Baldewicz TT, Krishnan KR. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62:633–8. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 92.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: Efficacy and dose response. Am J Prev Med. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 93.Blumenthal JA, Babyak MA, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69:587–96. doi: 10.1097/PSY.0b013e318148c19a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hoffman B, Babyak M, et al. Exercise and pharmacotherapy in patients with major depression: One year follow up of the SMILE study. Psychosom Med. 2010 Dec; doi: 10.1097/PSY.0b013e31820433a5. (epub) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lichtman JH, Bigger JT, Jr, Blumenthal JA, et al. Depression and coronary heart disease. Recommendations for screening, referral, and treatment. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]