ABSTRACT
Functional dyspepsia (FD) is a disorder presenting with symptoms such as postprandial fullness, early satiety or epigastric pain. Although there is a 10 to 30% reported prevalence worldwide, there is currently no clear explanation of the pathophysiology behind this condition. Motility disorders, visceral hypersensitivity, acid disorders, Helicobacter pylori infection or psychosocial factors have all been reported to play a part in the pathophysiology of FD. The diagnosis of FD is one of exclusion, based on the Rome III criteria. The main therapeutic modalities include lifestyle changes, eradicating Helicobacter pylori infection and treatment with either proton pump inhibitors, prokinetics or antidepressants.
INTRODUCTION
Dyspepsia is a clinical syndrome which comprises a series of symptoms such as postprandial fullness, early satiety, or epigastric pain, symptoms which can accompany a number of gastrointestinal disorders. Although functional dyspepsia (FD) is diagnosed in more than 60% of patients complaining of these symptoms, the diagnosis remains one of exclusion (1) after structural disease (such as peptic ulcer, esophagitis or digestive malignancy) has been ruled out.
Large studies have shown a 10-30% prevalence of FD worldwide, highlighting the importance of FD as a healthcare issue (2).
Pathophysiology
The cause of functional dyspepsia remains unknown despite a great body of work in this field in the last decades. A variety of theories have been proposed in the attempt to better understand the pathopysiological mechanisms behind FD, but none have been conclusively proven.
There are currently five main theories regarded as possible explanations for FD symptoms and, while it now seems unlikely that any one of them can account for the entire disease burden on its own, they each merit an individual discussion of pathophysiological mechanism and its implications in FD treatment.
1. Motility disorders
Altered motility of the GI tract is an apparently simple and elegant explanation for the whole spectrum of FD symptoms, from epigastric pain to early satiety, nausea and belching.
According to some researchers, delayed gastric emptying was present in 25-40% of patients with functional dyspepsia and it was associated with postprandial satiation, nausea and vomiting (3).
Ultrasound, barostat and single photon emission tomography studies demonstrated impaired accommodation, an abnormal distribution of ingested food in the stomach, with an increased proportion of the food being distributed in the antrum compared to the proximal portion of the stomach. The impaired accommodation of the stomach is caused by a vaso-vagal reflex which requires nonadrenergic and noncolinergic pathways (4).
Recent studies suggest that delayed gastric emptying leading to FD symptoms may be the result of an altered migrating motor complex (MMC) (5). There is also evidence linking the presence of HP infection to altered phase III gastric MMC (6), thus suggesting an interrelation between these two pathogenic mechanisms of FD.
Another theory which is interesting also from a therapeutic viewpoint is the possibility that 5HT 3 receptors might be involved in the abnormal distension of the stomach in response to the perfusion of a fatty solution in the duodenum (7).
A disorder of the central or autonomous nervous systems has been studied as a possible mechanism for the impaired gastric accommodation and the antral hypomotility. There is some indirect evidence of a correlation between emotional and psychological factors and dyspeptic symptoms, via diminished vagal activity (8).
Manometric studies have also shown antral hypomotility as well as numerous retrograde contractions from the duodenum towards the stomach. Unsuppressed phased contractility increase parietal tension in the stomach which is, in turn, perceived as postprandial discomfort. This abnormality has been linked by some researchers with Helicobacter pylori infection (9).
Despite the continued development of sophisticated methods allowing the minute exploration of GI tract physiology, correctly quantifying the motility patterns of normal and FD patients is still proving a major obstacle in providing adequate support for this theory.
2. Visceral hypersensitivity
Some of the earliest studies in FD suggested a role for altered visceral sensitivity as an important mechanism for dyspeptic symptoms. Increased sensitivity to lipids in the duodenum was one of the first investigated pathways in FD (10).
Other studies focused on the role of mechanic stimulation of gastric and duodenal receptors. Results of gastric barostat studies have shown that patients with functional dyspepsia have a lower sensitive threshold to the distension of the barostat inside the proximal regions of the stomach and the duodenum. This gastric hypersensitivity, defined as pain threshold 2 standard deviations below that of normal voluntaries, is associated with postprandial epigastric pain and weight loss. Whether concomitant Helicobacter pylori infection contributes to gastric hypersensitivity is a matter still open to debate (11).
3. Acid disorders
Because FD symptoms are virtually indistinguishable from those of peptic ulcer disease (PUD) and because PPI treatment is a mainstay of FD treatment, many research groups have long advocated the role of abnormal gastric and duodenal acid levels in FD. Studies have shown that acid secretion is normal in a majority of dyspeptic patients but recent evidence suggests an abnormal acid clearance from the duodenum as well as a decreased motor response of the duodenum when acid is present. pHmetry studies lasting 24 hours have shown an increased exposure to acid after a meal, but no direct link between this exposure and dyspeptic symptoms has been proven (12). These observations have been recently confirmed by radiotelemetry pH monitoring over 48 hour periods (13).
4. Helicobacter pylori infection
One of the main arguments behind the possible role of Helicobacter pylori (HP) infection in FD is derived from clinical experience, with a systematic review showing the positive impact of HP eradication on FD symptoms (14) with a NNT of 15 (15). However, there is conflicting data on this matter, with a systematic review of studies striving to prove a causal relation between Helicobacter pylori infection and functional dyspepsia were inconclusive; a modest relationship seems to exist but evidence is lacking to support an important role of HP infection in patients with functional dyspepsia (16).
5. Psychosocial factors
There has been a longstanding interest in the role of psychological factors in the onset and symptom severity in FD. Studies have established that psychosocial stressors influence FD symptoms (17) and that depressive mood and altered quality of life were more frequent among FD and FD and IBS overlap patients (18). However, antidepressant treatment in FD, the next logical step in this pathophysiological chain, has been disappointing so far, raising questions over the validity of this particular approach to FD (19).
6. Allergic disorders
Recently, the role of various allergens has been studied in both FD and IBS, with studies showing an increase in the prevalence of food allergies (e.g.: eggs, soybeans) in FD and IBS patients (20). Furthermore, pathological studies have shown eosinophilia in the mucosa of FD patients, but its relationship to food allergens still needs further evaluation (21).
Symptoms and diagnosis
The cardinal symptoms of FD are epigastric pain, postprandial discomfort often described as postprandial fullness and early satiety. Additional symptoms such as nausea and belching may be present. Patients complaining of heartburn as a main symptom will usually receive a GERD diagnosis, although there is probably an important overlap between GERD and FD (22). The lack of sensitivity and specificity of the clinical diagnosis of FD has been highlighted by a clinical trial, which showed that only endoscopy was capable of correctly differentiating between peptic ulcer disease, esophagitis and FD (23).
While the continued development of functional explorations tests has allowed for a more refined exploration of the physiology of the GI tract, no correlation has been found between impaired mechanisms and FD symptoms as had been previously suggested (24). Due to the imprecise nature of its symptoms, functional dyspepsia has been defined using a set of periodically revised diagnostic criteria. The Rome III criteria, published in 2006, are the most commonly employed. They consist of one or more of the following symptoms (25): bothersome postprandial fullness, early satiety, epigastric pain, epigastric burning and no evidence of structural disease (including at upper endoscopy) that is likely to explain the symptoms. The criteria must be fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis.
The older Rome II criteria which classified functional dyspepsia as ulcer-like, dysmotility-like and nonspecific were abandoned in favor of the more precise Rome III (22) criteria based on the four cardinal symptoms already presented. According to the dominant presenting symptom, two subtypes of FD were defined as follows (Table 1):
Table 1.
Functional dyspepsia subtypes.
| A. Postprandial Distress Syndrome |
|
Diagnostic criteria* must include one or both of the following: Bothersome postprandial fullness, occurring after ordinary-sized meals, at least several times per week Early satiety that prevents finishing a regular meal, at least several times per week |
|
Supportive criteria Upper abdominal bloating or postprandial nausea or excessive belching can be present Epigastric pain syndrome may coexist |
| B. Epigastric Pain Syndrome |
|
Diagnostic criteria* must include all of the following: Pain or burning localized to the epigastrium of at least moderate severity, at least once per week The pain is intermittent Not generalized or localized to other abdominal or chest regions Not relieved by defecation or passage of flatus Not fulfilling criteria for gallbladder and sphincter of Oddi (26) disorders |
|
Supportive criteria The pain may be of a burning quality, but without a retrosternal component The pain is commonly induced or relieved by ingestion of a meal, but may occur while fasting Postprandial distress syndrome may coexist |
* Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
Therapy of functional dyspepsia
The heterogeneous nature of the functional dyspepsia patient population makes it difficult to have a representative study group, which is one of the reasons that the results of drug trials tend to be discordant. During the past decades, many trials have addressed the problem of FD therapy, with unsatisfying and sometimes contradictory results.
Lifestyle alteration
General measures such as smaller, more frequent meals, avoiding caffeine, alcohol, NSAIDs, fatty or spicy meals, seem in order, although there is little evidence supporting their use (27).
Pump proton inhibitor
Two regimens of antisecretory therapy were proposed: "step-up" (e.g., start with antacids, then H2-blockers and then proton pump inhibitors) or "step-down". A metanalysis comparing these two strategies has showed similar success rate, but with higher costs for step-down approach at six-months (28).
Several placebo-controlled trials had the same results regarding the efficacy of PPI, a meta-analysis finding an NNT of 10 and a relative risk reduction of 13%, without difference between doses of PPIs (29). However, the relief of symptoms was greatest in patients with ulcer-like and reflux-like symptoms, but not in those with dysmotility-like symptoms or unspecified dyspepsia.
H2-receptor antagonists (H2RA)
Many trials, which probably included GERD patients, found a significant benefit and a relative risk reduction of 23% with a number to treat of 7, but better quality trials showed a low efficacy for H2RA therapy (30).
Prokinetics
Prokinetics act on three different types of receptors in order to enhance gastric motility. These drugs might help alleviate satiation, abdominal distention and nausea, but the link between symptom relief and improved gastric emptying is not yet proven (31).
Several studies have symptom relief for cisapride and domperidone, with a reduction in relative risk of 50% (32). Cisapride, however, has been withdrawn because of safety concerns and domperidone is not widely available.
Metoclopramide may also be effective, but is associated with several potential side effects, particularly with long-term use. Itopride, a dopamine D2 antagonist, was effective in a phase III multicenter trial; the suggested mechanism of action being its effect on gastric accommodation and hypersensitivity (33).
Antidepressants
If initial treatment with IPPs or prokinetics fails, antidepressants can be employed, in lower doses than required in the treatment of depression. Tricyclic antidepressants as well as selective serotonine reuptake inhibitors (SSRI) such as paroxentine, valexetine, were no more effective than placebo on improving symptoms, according to results of a randomized placebo-controlled trial (34).
The role and the mechanism of antidepressants in functional dyspepsia remain unsettled.
Management of functional dyspepsia
From the insufficient understanding of the pathogenic mechanisms of functional disorders stems, to the difficulty of setting up diagnostic and therapeutic guidelines. Furthermore, there is a logical incongruity between the diagnostic criteria for FD and its management. Although a diagnosis of FD requires the absence of any structural disease, including at endoscopy, management guidelines support empiric antisecretory or prokinetic therapy in patients with suspected FD who show no alarm symptoms (35). Endoscopy is recommended only in those cases where alarm symptoms are present or patients are non-responders to at least 4 weeks of empiric therapy. As such, a vast majority of FD patients will most likely receive treatment without undergoing endoscopy for diagnosis confirmation.
The first step in evaluating any patient is history taking and physical examination, which can help suggest either a structural or a functional disorder. Routine lab tests (e.g.: blood count) can also be helpful in an initial workup of the patient.
In addition, the physician needs to pay attention to the so-called "alarm symptoms", which increase the likelihood of a structural disease (Table 2). Any of these signs and symptoms requires an endoscopic study to assess a possible malignancy. The American Society of Gastroenterology (ASGE) guidelines emphasize the fact that the positive predictive value of these symptoms is low (11%). However, their negative predictive value in excluding gastrointestinal malignancy is very high, approximately 97% (36). This is the logical consequence of the fact that only 2% of dyspeptic syndromes are caused by esophageal or gastric cancer, 30 times fewer than functional dyspepsia (37). Conversely, the presence of alarm symptoms provides reasonable guidance, and has been included in consensus recommendations on functional dyspepsia management.
Table 2.
Alarm symptoms.
| Alarm symptoms |
|---|
| Age > 50 yrs |
| Family history of digestive malignancy |
| Involuntary weight loss |
| Unexplained anemia or iron deficiency |
| Progressive dysphagia |
| Hematemesis |
| Odinophagia |
| Recurrent vomiting |
| Palpable tumor or lymphadenopathy |
| Jaundice |
| Previous gastric surgery |
Excluding gastroesophageal reflux disease (GERD) as the cause of dyspeptic symptoms is also of paramount importance because GERD has a different treatment and prognosis and requires a particular management strategy involving long-term proton pump inhibitor therapy (IPP) and active surveillance for reflux esophagitis, Barrett's esophagus as well as esophageal cancer. Many GERD patients are diagnosed with functional dyspepsia because of the lack of structural abnormalities in endoscopic studies and the great variety of symptoms of functional dyspepsia (including heartburn) which in turn has lead to confusing results in many clinical trials (38).
A drug-induced dyspepsia must be also taken into account, especially nonsteroidal anti-inflammatory drugs (NSAIDs) commonly associated with dyspepsia. In this case, the offending agent should be discontinued, if possible, or a proton pump inhibitor can be added (PPI) (39). Patients on long term NSAID treatment can be considered at risk for peptic ulcer disease and the physician should decide whether endoscopy is warranted from the first visit.
The optimal approach for a patient with uninvestigated dyspeptic symptoms is far from being decided. Several strategies for the management of these patients have been proposed, but several systematic reviews have failed to settle the dispute.
The options taken into discussion were:
-
1.
Prompt endoscopy
-
2.
Empiric antisecretory therapy
-
3.
Noninvasive testing for Helicobacter pylori, followed by treatment or endoscopy if positive (test-and-treat strategy)
1. The role of endoscopy in FD
The most debated problem in the management of FD, as already shown above, is the role of an initial upper digestive endoscopy. Endoscopy (40-42) has the advantage of excluding peptic ulcer, esophagitis and cancer as causes of dyspepsia. A meta-analysis of nine studies with 5389 patients showed that the most common finding in patients with dyspeptic symptoms was erosive esophagitis (pooled prevalence 13%), though the prevalence was much lower when dyspepsia was defined using the Rome criteria (6 %) (43).
In addition, clinical trials show that simply being subjected to an endoscopic study increases the patient's level of satisfaction and confidence (44). Supporters of empiric therapy argue that a low incidence of cancer (less than 2% of dyspeptic patients) and the high costs incurred by endoscopy should preclude upper digestive endoscopy as a first step in investigating these patients. Accordingly, patients under 45-50 years of age without any alarm symptoms could be treated empirically with minimal risks (45), endoscopic studies being reserved for those patients who are nonresponsive to 6-8 weeks of therapy. However, given that many patients do not achieve full symptomatic relief with medical therapy, requiring further investigations, it seems more prudent to perform endoscopy in the initial workup. If this initial endoscopic study is normal, endoscopy will not be repeated unless alarm symptoms develop.
The American Gastroenterology Association's guidelines from 2005 also suggest that endoscopy should be performed in patients with dyspepsia who have alarm symptoms or those without alarm symptoms who are ≥55 years of age (46). The authors point out that in some regions where cancer incidence is higher (such as Alaska), lower age thresholds are appropriate, for example 45 years rather than 55 years of age. Patients who receive medication should be evaluated for symptomatic improvement at approximately eight weeks.
2. Empiric antisecretory therapy
The empiric antisecretory therapy has advantages and disadvantages, according to conflicting results of studies. Many patients can have a favorable symptomatic response, but this does not exclude a malignant gastric ulcer and it can delay the diagnosis. Also, the recurrence of the symptoms is common after one year (47) and the lack of H. pylori eradication increases the risk of ulcer recurrence.
3. Test and treat strategy
The relationship between Helicobacter pylori infection and peptic ulcer disease is well known but H. Pylori infection alone can account for a minority of cases of chronic dyspepsia. For this reason, the consensus of European H. Pylori Study Group (March 2005) suggested a "test-and-treat" approach for patients less than 45 years old with persistent dyspepsia (a remark is made for the age cutoff, which may vary with the prevalence of gastric cancer in different countries). Another conclusion was that, in countries with low prevalence of H. pylori infection (<20%), the empirical therapy with PPI is preferred to the test and treat strategy (48).
Among the noninvasive studies the most widely used in managing functional dyspepsia are the 13C-urea breath test and the stool antigen test for Helicobacter pylori (HP), the IgG serology being reserved for the cases where pretest probability is high, followed by a confirmation by one of the methods mentioned above. ❑
CONCLUSIONS
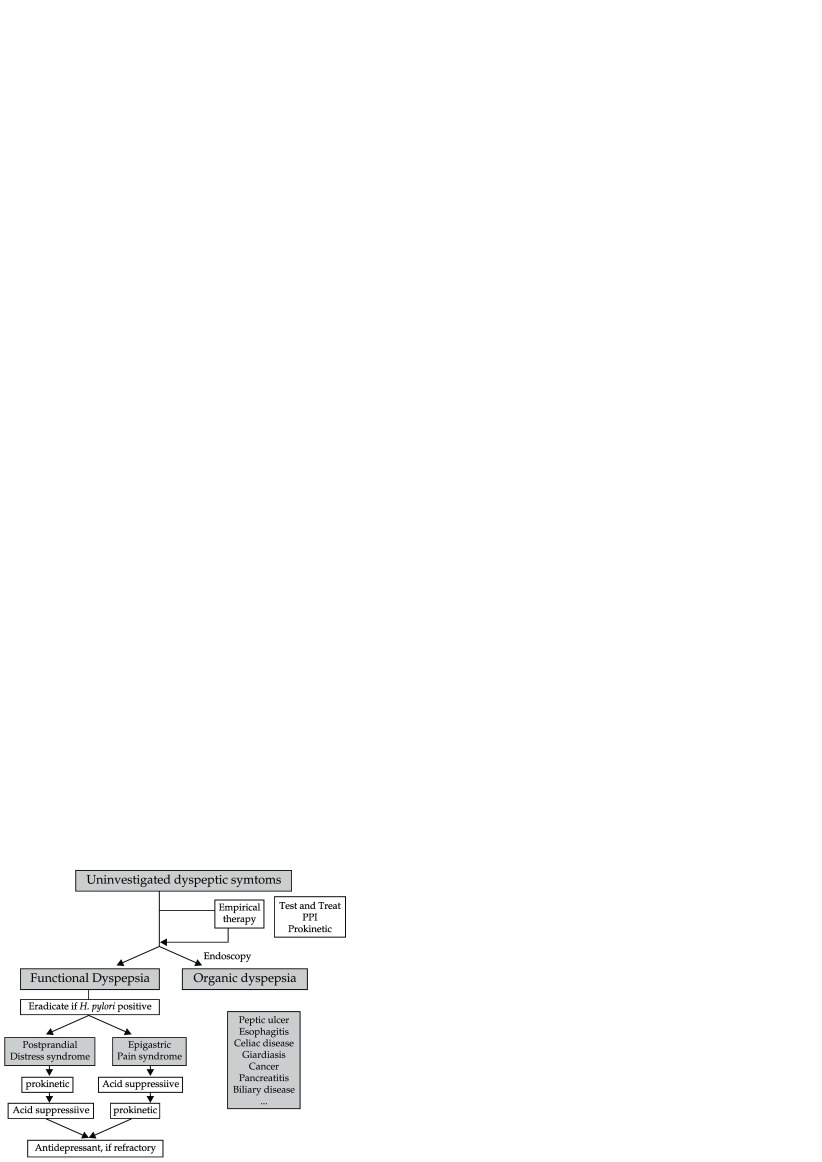
As long as the mechanisms of disease involved in functional dyspepsia are not fully understood we cannot hope for an adequate treatment for FD. Consequently, physicians must rely on empiric therapies, choosing those drugs that have a good safety profile and whose effectiveness has been validated by clinical trials. For the time being, use of a PPI or/and a prokinetic for a minimum of 4 to 8 weeks seems the best option available (Figure 1). New drugs such as antidepressants might be of use in treatment failures but further research is needed in order to provide better care for FD patients.
Figure 1. Treatment algorithm for FD.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Bazaldua OV, Schneider FD. Evaluation and Management of Dyspepsia. Am. Fam Physician. 1999;60:1774–1774. [PubMed] [Google Scholar]
- 2.Mahadeva S, Gok KL. Epidemiology of Functional Dyspepsia: a Global Perspective. 2006;12(17):2661–6. doi: 10.3748/wjg.v12.i17.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maes BD, Ghoos YF, Hiele MI, et al. Gastric Emptying Rate of Solids in Patients with Nonulcer Dyspepsia. Dig. Dis Sci. 1997;42:235–42. doi: 10.1023/a:1018881419010. [DOI] [PubMed] [Google Scholar]
- 4.Thumshirn M, Camilleri M, Saslow SB, et al. Gastric Accomodation in Non-Ulcer Dyspepsia and the Roles of Helicobacter Pylori Infection and Vagal Function. Gut. 1999;44:55–64. doi: 10.1136/gut.44.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takashi T. Mechanisms of Interdigestive Migrating Motor Complex. J Neurogastroenterol Motil. 2012;18(3):246–257. doi: 10.5056/jnm.2012.18.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Testoni PA, Bagnolo F, Bologna P, et al. Higher Prevalence of Helicobacter Pylori Infection in Dyspeptic Patients who Do Not Have Gastric Phase IIII of the Migrating Motor Complex. Scand J Gastroenterol. 1996;31(11):1063–8. doi: 10.3109/00365529609036888. [DOI] [PubMed] [Google Scholar]
- 7.Feinle C, Read NW. Ondansetron Reduces Nausea Induced by Gastroduodenal Stimulation without Changing Gastric Motility. Am J Physiol. 1996;271:G591–7. doi: 10.1152/ajpgi.1996.271.4.G591. [DOI] [PubMed] [Google Scholar]
- 8.Troncon LE, Thompson DG, Ahluwalia NK, et al. Relations between Upper Abdominal Symptoms and Distension Abnormalities in Dysmotility Like Functional Dyspepsia and after Vagotomy. Gut. 1995;36:17–22. doi: 10.1136/gut.37.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camilleri M. Functional Dyspepsia; Mechanisms of Symptom Generation and Appropriate Management of Patients. Gastroenterol Clin N Am. 2007;36:643–664. doi: 10.1016/j.gtc.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Barbera R, Feinle C, Read NW. Nutrient-specific modulation of gastric mechanosensitivity in patients with functional dyspepsia. Dig Dis Sci. 1995;40:1636–41. doi: 10.1007/BF02212683. [DOI] [PubMed] [Google Scholar]
- 11.Mearin F, de Ribot X, Balboa A, et al. Does Helicobacter Pylori Infection Increases Gastric Sensitivity in Functional Dyspepsia? Gut. 1995;37:47–51. doi: 10.1136/gut.37.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee KJ, Demarchi B, Vos R, et al. Comparison of Duodenal Acid Exposure in Functional Dyspepsia Patients and Healthy Controls Using 24-Hour Ambulatory Duodenal Ph Monitoring. Gastroenterology. 2002;122:A–102. [Google Scholar]
- 13.Bratten J, Jones MP. Prolonged Recording of Duodenal Acid Exposure Inpatients with Functional Dyspepsia and Controls Using a Radiotelemetry Ph Monitoring System. J Clin Gastroenterol. 2009;43(6):527–533. doi: 10.1097/MCG.0b013e31818e37ab. [DOI] [PubMed] [Google Scholar]
- 14.Moayyedi P, Soo S, Deeks J, et al. Eradication of Helicobacter Pylori for Non-Ulcer Dyspepsia. Cochrane Database Syst Rev. 2006;(2):CD002096–CD002096. doi: 10.1002/14651858.CD002096.pub4. [DOI] [PubMed] [Google Scholar]
- 15.Loyd RA, McClellan DA. Update on the Evaluation and Management of Functional Dyspepsia. Am Fam Physician. 2011;83(5):547–52. [PubMed] [Google Scholar]
- 16.Danesh J, Lawrence M, Murphy M, et al. Systematic Review of the Epidemiological Evidence on Helicobacter Pylori Infection and Nonulcer or Uninvestigated Dyspepsia. Arch Intern Med. 2000;160:167–80. doi: 10.1001/archinte.160.8.1192. [DOI] [PubMed] [Google Scholar]
- 17.Budavari AI, Olden KW. Psychosocial Aspects of Functional Gastrointestinal Disorders. Gastroenterol Clin North Am. 2003;32:477–506. doi: 10.1016/s0889-8553(03)00030-x. [DOI] [PubMed] [Google Scholar]
- 18.Lee HJ, Lee SY, Kim JH, et al. Depressive Mood and Quality of Life in Functional Gastrointestinal Disorders: Differences Between Functional Dyspepsia, Irritable Bowel Syndrome and Overlap Syndrome. Gen Hosp Psychiatry. 2010;32(5):499–502. doi: 10.1016/j.genhosppsych.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 19.van Kerkhoven LA, Laheij RJ, Aparicio N, et al. Effect of the Antidepressant Venlafaxine in Functional Dyspepsia: a Randomized, Double-Blind, Placebo-Controlled Trial. Clin Gastroenterol Hepatol. 2008;6(7):746–746. doi: 10.1016/j.cgh.2008.02.051. [DOI] [PubMed] [Google Scholar]
- 20.Zuo XL, Li YQ, Li WJ, et al. Alterations of Food Antigen-Specific Serum Immunoglobulins G and E Antibodies in Patients with Irritable Bowel Syndrome and Functional Dyspepsia. Clin Exp Allergy. 2007;37:823–30. doi: 10.1111/j.1365-2222.2007.02727.x. [DOI] [PubMed] [Google Scholar]
- 21.Friesen CA, Sandridge L, Andre L, et al. Mucosal Eosinophilia and Response to H1/H2 Antagonist and Cromolyn Therapy in Pediatric Dyspepsia. Clin Pediatr (Phila) 2006;45:143–7. doi: 10.1177/000992280604500205. [DOI] [PubMed] [Google Scholar]
- 22.Talley NJ, Vakil N, Lauritsen K, et al. and STARS I Study Group. Randomized Controlled Trial of Esomeprazolein Functional Dyspepsia Patients with Epigastric Pain or Burning: Does a One Week Trial of Acid Suppression Predict Symptom Response? Aliment Pharmacol Ther. 2009;26(5):673–682. doi: 10.1111/j.1365-2036.2007.03410.x. [DOI] [PubMed] [Google Scholar]
- 23.Thomson AB, Barkun AN, Armstron D et al. The Prevalence of Clinically Significant Endoscopic Findings in Primary Care Patients with Uninvestigated Dyspepsia: the Canadian Adult Dyspepsia Empiric Treatment – Prompt Endoscopy (CADET PE) study. Aliment Pharmacol Ther. 2003;17:1481–1491. doi: 10.1046/j.1365-2036.2003.01646.x. [DOI] [PubMed] [Google Scholar]
- 24.Sha W, Pasricha PJ, Chen JD. Correlations among Electrogastrogram, Gastric Dysmotility and Duodenal Dysmotility in Patients with Functional Dyspepsia. J Clin Gastroenterol. 2009;43(8):716–722. doi: 10.1097/MCG.0b013e31818b8ed9. [DOI] [PubMed] [Google Scholar]
- 25.Tack J, Tallez NJ, Camilleri M, et al. Functional Gastroduodenal Disorders. Gastroenterology. 2006;130:1466–79. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 26.Drossman DA. Rome III: the New Criteria. Chin J Dig Dis. 2006;7(4):181–5. doi: 10.1111/j.1443-9573.2006.00265.x. [DOI] [PubMed] [Google Scholar]
- 27.Simren M, Tack J. Functional Dyspepsia: Evaluation and Treatment. Gastroenterol Clin N Am. 2003;32:577–599. doi: 10.1016/s0889-8553(03)00023-2. [DOI] [PubMed] [Google Scholar]
- 28.van Marrewijk CJ, Mujakovic S, Fransen GA, et al. Effect and Cost-Effectiveness of Step-Up versus Step-Down Treatment with Antacids, H2-Receptor Antagonists and Proton Pump Inhibitors in Patients with New Onset Dyspepsia (DIAMOND study): a Primary-Care-Based Randomised Controlled Trial. Lancet. 2009;373(9659):215–215. doi: 10.1016/S0140-6736(09)60070-2. [DOI] [PubMed] [Google Scholar]
- 29.Peura DA, Kovacs TO, Metz DC, et al. Lansoprazole in the Treatment of Functional Dyspepsia: Two Double-Blind, Randomized, Placebo-Controlled Trials. Am J Med. 2004;116(11):740–740. doi: 10.1016/j.amjmed.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 30.Abraham NS, Moayyedi P, Daniels B, et al. Systematic Review: the Methodological Quality of Trials Affects Estimates of Treatment Efficacy in Functional (Non-Ulcer) Dyspepsia. Aliment Pharmacol Ther. 2004;19(6):631–631. doi: 10.1111/j.1365-2036.2004.01878.x. [DOI] [PubMed] [Google Scholar]
- 31.Tack J, Tallez NJ, Camilleri M, et al. Functional Gastroduodenal Disorders. Gastroenterology. 2006;130:1466–79. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 32.Soo S, Moayyedi P, Deeks J, et al. Pharmacological Interventions for Non-Ulcer Dyspepsia. Cochrane Database Syst Rev. 2000 doi: 10.1002/14651858.CD001960. [DOI] [PubMed] [Google Scholar]
- 33.Talley NJ, Tack J, Ptak T, et al. Itopride in Functional Dyspepsia: Results of Two Phase III Multicentre, Randomised, Double-Blind, Placebo-Controlled Trials. Gut. 2008;57(6):740–740. doi: 10.1136/gut.2007.132449. [DOI] [PubMed] [Google Scholar]
- 34.van Kerkhoven LA, Laheij RJ, Aparicio N, et al. Effect of the Antidepressant Venlafaxine in Functional Dyspepsia: a Randomized, Double-Blind, Placebo-Controlled Trial. Clin Gastroenterol Hepatol. 2008;6(7):746–746. doi: 10.1016/j.cgh.2008.02.051. [DOI] [PubMed] [Google Scholar]
- 35.Miwa H, Ghoshal UC, Gonlachanvit SJ. Asian Consensus Report on Functional Dyspepsia. Neurogastroenterol Motil. 2012;18(2):150–68. doi: 10.5056/jnm.2012.18.2.150. Epub, 2012 April 9th. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahadeva S, Gok KL. Epidemiology of Functional Dyspepsia: a Global Perspective. World J Gastroenterol. 2006;12(17):2661–6. doi: 10.3748/wjg.v12.i17.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bazaldua OV, Schneider FD. Evaluation and Management of Dyspepsia. Am. Fam Physician. 1999;60:1774–1774. [PubMed] [Google Scholar]
- 38.Talley NJ, Meineche-Scmidt V, Pare P, et al. Efficacy of Omeprazol in Functional Dyspepsia: Double-Blind, Randomized, Placebo-Controlled Trial (The Bond and Opera Studies). Aliment Pharmacol Ther. 1998;12:1055–1065. doi: 10.1046/j.1365-2036.1998.00410.x. [DOI] [PubMed] [Google Scholar]
- 39.Talley NJ. American Gastroenterological Association Medical Position Statement: Evaluation of Dyspepsia. Gastroenterology. 2005;129:1753–5. doi: 10.1053/j.gastro.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 40.ASG The Role of Endoscopy in Dyspepsia. Gastrointest Endosc. 2007;66(6):1071–5. doi: 10.1016/j.gie.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 41.Lassen AT, Pedersen FM, Bytzer P, et al. Helicobacter Pylori Test and Eradicate versus Prompt Endoscopy for Management of Dyspeptic Patients – a Randomized Trial. Lancet. 2000;356:455–60. doi: 10.1016/s0140-6736(00)02553-8. [DOI] [PubMed] [Google Scholar]
- 42.Talley N, Silverstein M, et al. AGA Technical Review: Evaluation of Dyspepsia. Gastroenterology. 1998;114(3):582–595. doi: 10.1016/s0016-5085(98)70542-6. [DOI] [PubMed] [Google Scholar]
- 43.Ford AC, Marwaha A, Lim A, et al. What Is the Prevalence of Clinically Significant Endoscopic Findings in Subjects with Dyspepsia? Systematic Review and Meta-Analysis. Clin Gastroenterol Hepatol. 2010;8(10):830–830. doi: 10.1016/j.cgh.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 44.Rabeneck L, Wristers K, Souchek J, et al. Impact of Upper Endoscopy on Satisfaction in Patients with Previously Uninvestigated Dyspepsia. Gastrointestinal Endoscopy. 2003;57(3):295–9. doi: 10.1067/mge.2003.122. [DOI] [PubMed] [Google Scholar]
- 45.Health and Public Policy Committee. Endoscopy in the Evaluation of Dyspepsia. Ann Intern Med. 1985;102:266–269. [PubMed] [Google Scholar]
- 46.Talley NJ, American Gastroenterological Association, American Gastroenterological Association. Medical Position Statement: Evaluation Of Dyspepsia. Gastroenterology. 2005;129(5):1753–1753. doi: 10.1053/j.gastro.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 47.Rabeneck L, Souchek J, Wristers K, et al. A Double Blind, Randomized, Placebo-Controlled Trial of Proton Pump Inhibitor Therapy in Patients with Uninvestigated Dyspepsia. Am J Gastroenterol. 2002;97:3045–3045. doi: 10.1111/j.1572-0241.2002.07123.x. [DOI] [PubMed] [Google Scholar]
- 48.Malfertheiner P, Megraud F, O'Morain C, et al. Current Concepts in the Management of Helicobacter Pylori Infection: the Maastricht III Consensus Report. Gut. 2007;56(6):772–772. doi: 10.1136/gut.2006.101634. [DOI] [PMC free article] [PubMed] [Google Scholar]