Abstract
Background
Correlates of prenatal physical activity can inform interventions, but are not well-understood.
Methods
Participants in the Pregnancy, Infection, and Nutrition 3 Study were recruited before 20 weeks gestation. Women self-reported frequency, duration, and mode of moderate and vigorous physical activities. We used logistic regression to identify correlates of any physical activity (≥10 minutes/week of any mode), any recreational activity (≥10 minutes/week), and high volume recreational activity (either ≥150 minutes/week of moderate or ≥75 minutes/week of vigorous). Our analysis included 1752 women at 19-weeks gestation and 1722 at 29 weeks.
Results
Higher education, white race, and enjoyment of physical activity were positively correlated with all 3 outcomes. Any recreational activity was negatively associated with parity, body mass index, and history of miscarriage. The associations of history of miscarriage and body mass index differed at 19 weeks compared with 29 weeks. Single marital status, health professional physical activity advice, and time for activity were associated with high volume recreational activity only.
Conclusions
Correlates of physical activity differed by mode and volume of activity and by gestational age. This suggests that researchers planning physical activity interventions should consider the mode and amount of activity and the gestational age of the participants.
Keywords: leisure activity, gestational age, intervention, barriers, psychosocial
Recreational physical activity is considered beneficial for pregnant women by both the American College of Obstetrics and Gynecology (The College) and the United States (U.S.) Department of Health and Human Services.1,2 Despite these recommendations, many pregnant women are not physically active.3 Moreover, among active women, the intensity and duration of recreational activity tend to decline during pregnancy.4-17 Low levels of physical activity may lead to higher weight gain,18 and excess weight gain during pregnancy may be related to higher body mass index in the long term, even 15 years later.19 To design and target interventions for maintaining or safely increasing activity during pregnancy, it is useful to understand factors that are correlated with physical activity during pregnancy.
The factors correlated with physical activity during pregnancy are not well understood. Studies have been small (N = 25–74),5,6,12,13 limited to a comparison of all pregnant women to nonpregnant women,20-22 or measured recreational activity at one time point during pregnancy,7,10,12,20-24 which precluded assessment of whether correlates vary over the course of pregnancy. Measurements of physical activity have not always included frequency, intensity, duration, and type, nor have they allowed the women to enumerate all their physical activities. In addition, some potentially important correlates have not been investigated, including psychosocial characteristics and barriers to physical activity.
Physical activity includes recreational activity, which is elective and usually the most amenable to change, as well as more obligatory forms of activity such as occupational, household, and transportation activities. The correlates of recreational activity may differ from those of other modes of physical activity. If time and energy are limited, recreation may decrease in pregnancy, while nonrecreational physical activity may be more likely to remain constant.4,5
To understand the characteristics that are associated with physical activity we undertook an analysis of moderate and vigorous physical activity during pregnancy. Our aim was to identify characteristics that were associated with total moderate or vigorous physical activity and recreational activity at 2 different time points during pregnancy.
Methods
Study Participants and Protocol
Participants in the Pregnancy, Infection, and Nutrition 3 (PIN3) Study were recruited before 20 weeks gestation between January 2001 and June 2005 from the University of North Carolina prenatal care centers in Chapel Hill. Women were excluded if they were less than 16 years of age, did not speak English, did not plan to continue care or deliver at the study site, had multiple gestations, or did not have access to a telephone from which they could complete phone interviews. The PIN3 cohort included 2006 pregnancies, with some women contributing up to 3 pregnancies. We limited our analysis sample to the first study pregnancy for each woman, leaving 1875 pregnancies. Women who were eligible and recruited were more likely to be older, non-Hispanic white, married, and more highly educated than those eligible and not recruited. This study was approved by the Institutional Review Board at the University of North Carolina, and informed consent was provided by all participants.
Participants provided access to their medical records and completed 2 telephone interviews to assess physical activity patterns and other characteristics; 1 interview was administered between gestational weeks 17 and 22 (mean/median = 19 weeks, referred to as the “19-week interview”) and the other between weeks 27 and 30 (mean/median = 29 weeks, “29-week interview”). Women also completed 2 self-administered questionnaires between gestational weeks 15 and 20 and again between weeks 24 and 29 which provided data on psychosocial measures. Of the 1875 women, 76 indicated that their physician advised them to refrain from physical activity at some point during pregnancy,25 24 dropped out, 22 lost their pregnancy and 1 discovered she was carrying multiples, this left 1752 women in our analysis at week 19. After the 19-week interview but before the 29-week interview, 2 women discovered they were carrying multiples, 13 pregnancies ended, and 15 women dropped out of the study. This left 1722 pregnancies for analysis at 29 weeks.
Outcomes
At both phone interviews women were asked to describe their physical activities in the past week. Each woman was asked, “In the past week, did you participate in any recreational activity or exercise, such as walking for exercise, swimming, or dancing that caused at least some increase in breathing and heart rate?” If she answered “yes,” she was asked “What type of recreational activities did you do during the past week?”, “How many times in the past week did you [activity]?”, “On average, for how many minutes or hours did you usually [activity] at a time?”, and “Thinking about your breathing and heart rate, how hard did this usually feel to you (fairly light, somewhat hard, or hard/very hard)?” The same series of questions was asked for other types of activity, including occupational activity, household activity (indoor and outdoor), child or adult care activity, and transportation activity (ie, biking or walking to work).
Evidence for validity and reliability of the questionnaire were previously assessed among pregnant women.26 To assess concurrent-related validity, 177 pregnant women kept a structured diary and wore an accelerometer (ActiGraph) for 1 week. At the end of the week, they completed the physical activity questionnaire over the telephone. Comparison of the questionnaire to the structured diary was moderate to substantial (Spearman correlation coefficient 0.47–0.69) for moderate or vigorous physical activity. Comparison of moderate-to-vigorous physical activity from the questionnaire to the accelerometer ranged from 0.28 to 0.34 using perceived intensity (hours/week).
To assess evidence for test-retest reliability, 109 pregnant women completed the questionnaire twice over the telephone, within 48 hours apart, recalling the same time period.26 Test-retest reliability was moderate to almost perfect for moderate-to-vigorous physical activity, with the intraclass correlation coefficients ranging from 0.56 to 0.82.
Three outcomes were of interest in this analysis and each one was assessed at 19 weeks and again at 29 weeks of gestation. Our outcome measures included only moderate or vigorous intensity activities (we did not consider light or very light activities). First, we defined a dichotomous outcome that encompassed all modes of physical activity. Women who performed a total of at least 10 minutes of moderate (“somewhat hard”) to vigorous (“hard/very hard”) physical activity in the past week met the criteria for any physical activity. Second, women were categorized as performing any recreational activity if they reported at least 10 minutes per week of “somewhat hard” or “hard/very hard” recreational activity.
Third, we explored higher levels of recreational activity. Women were classified as performing high volume recreational activity if 1) they reported “somewhat hard” recreational activity for at least 150 minutes/week, 2) they reported “hard/very hard” recreational activity for at least 75 minutes/week, or 3) the sum of their “somewhat hard” minutes/week and twice their “hard/very hard” minutes per week was at least 150 minutes/week. We also examined correlates of the minutes of recreational activity as a continuous outcome. Associations were similar to high volume recreational activity, and thus are not presented here.
Correlates
The correlates we considered are listed in Table 1 and were grouped into the following categories: sociodemographic, behavioral, reproductive history, current pregnancy, psychosocial, and barriers/external influences. Income was expressed as a percentage of the 2001 poverty level. Prenatal care use was assessed in 2 ways, as month of initiation and as observed versus expected number of visits and categorized according to Kotelchuck.27
Table 1. Descriptive Characteristics of Women in the Analysis Sample—Pregnancy, Infection,and Nutrition 3 Study, North Carolina, 2001–2005.
| Enrolled population |
Complete case analysis |
|||
|---|---|---|---|---|
| 19 weeks gestation |
29 weeks gestation |
19 weeks gestation |
29 weeks gestation |
|
| N (%) | N (%) | N (%) | N (%) | |
| Totals | N = 1752 | N = 1722 | N = 1162 | N = 1040 |
| Physical activity | ||||
| Any physical activity† | ||||
| Yes | 1052 (65) | 943 (63) | 767 (66) | 681 (65) |
| Any recreational activity*,† | ||||
| Yes | 651 (40) | 540 (36) | 496 (43) | 408 (39) |
| High volume recreational activity*,† | ||||
| Yes | 270 (17) | 210 (14) | 204 (18) | 156 (15) |
| Sociodemographic | ||||
| Age*,* | ||||
| ≤25 | 500 (29) | 491 (29) | 254 (22) | 214(21) |
| 26–30 | 572 (33) | 564 (33) | 407 (35) | 366 (35) |
| 31–35 | 475 (27) | 469 (27) | 360 (31) | 332 (32) |
| 36–40 | 205 (12) | 198 (12) | 141 (12) | 128 (12) |
| Race*,* | ||||
| White | 1207 (69) | 1190 (69) | 887 (76) | 803 (77) |
| African-American | 380 (22) | 369 (21) | 177 (15) | 150 (14) |
| Other | 162 (9) | 160 (9) | 98 (8) | 87 (8) |
| Marital status*,* | ||||
| Single | 510 (29) | 501 (29) | 231 (20) | 195 (19) |
| Married | 1235 (71) | 1213 (71) | 931 (80) | 845 (81) |
| Education*,* | ||||
| High school graduate or less | 433 (25) | 422 (25) | 190 (16) | 157 (15) |
| Some college | 338 (19) | 330 (19) | 211 (18) | 185 (18) |
| College graduate | 465 (27) | 460 (27) | 355 (31) | 319 (31) |
| ≥ Some graduate school | 509 (29) | 503 (29) | 406 (35) | 379 (36) |
| Employed*,† | ||||
| Yes | 1126(69) | 1021 (68) | 838 (72) | 733 (70) |
| Behavioral | ||||
| Body mass index (kg/m2)*,* | ||||
| <18.5 | 75 (5) | 74 (5) | 45 (4) | 42 (4) |
| 18.6–24.9 | 881 (53) | 871 (53) | 662 (57) | 192 (18) |
| 25.0–29.9 | 327 (20) | 323 (20) | 220 (19) | 199 (19) |
| ≥30.0 | 378 (23) | 369 (23) | 235 (20) | 607 (58) |
| Prenatal care initiation index*,* | ||||
| Adequate or less | 403 (25) | 398 (25) | 262 (23) | 226 (22) |
| Adequate plus | 1230 (75) | 1213 (75) | 900 (77) | 814 (78) |
| Alcohol use†,† | ||||
| No | 790 (53) | 790 (53) | 609 (52) | 540 (52) |
| Occupational physical activity*,† | ||||
| Any | 184 (11) | 189 (13) | 125 (11) | 129 (12) |
| Child/adult care physical activity (min/week)*,† | ||||
| None | 1346 (83) | 1237 (83) | 961 (83) | 864 (83) |
| 1–250 | 189 (12) | 186 (12) | 136 (12) | 130 (13) |
| >250 | 94 (6) | 70 (5) | 65 (6) | 46 (4) |
| Outdoor physical activity at 19 weeks (min/week)*,† | ||||
| Any | 88 (5) | 109 (7) | 74 (6) | 82 (8) |
| Indoor physical activity at 19 weeks (min/week)*,† | ||||
| None | 1251 (77) | 1113 (75) | 909 (78) | 786 (76) |
| 1–100 | 237 (15) | 242 (16) | 162 (14) | 167 (16) |
| >100 | 140 (9) | 138 (9) | 91 (8) | 87 (8) |
| Transportation physical activity*,† | ||||
| Any | 141 (9) | 130 (9) | 100 (9) | 95 (9) |
| Reproductive history | ||||
| Parity*,* | ||||
| 0 | 849 (49) | 834 (49) | 595 (51) | 548 (53) |
| 1 | 571 (33) | 564 (33) | 386 (33) | 339 (33) |
| ≥2 | 326 (19) | 318 (19) | 181 (16) | 153 (15) |
| History of miscarriage**,* | ||||
| Any | 444 (27) | 431 (27) | 318 (27) | 288 (28) |
| Psychosocial | ||||
| Perceived stress score*,† | ||||
| 0–16 | 547 (34) | 516 (35) | 431 (37) | 385 (37) |
| 17–22 | 494 (30) | 513 (34) | 358 (31) | 367 (35) |
| ≥ 23 | 586 (36) | 463 (31) | 373 (32) | 288 (28) |
| CES-D score†,§ | ||||
| 0–16 | 1113 (74) | 944 (75) | 906 (78) | 794 (76) |
| 17–24 | 195 (13) | 185 (15) | 144 (12) | 153 (15) |
| ≥ 25 | 188 (13) | 132 (10) | 112 (10) | 93 (9) |
| Barriers/external influences | ||||
| Partner is supportive of activity† | ||||
| All of the time | 921 (62) | 921 (62) | 749 (64) | 673 (65) |
| Some of the time | 340 (23) | 340 (23) | 270 (23) | 242 (23) |
| None of the time | 33 (2) | 33 (2) | 25 (2) | 24 (2) |
| Refused/Don’t know/NA | 195 (13) | 195 (13) | 118 (10) | 101 (10) |
| Time for recreational activity† | ||||
| All of the time | 509 (34) | 509 (34) | 396 (34) | 357 (34) |
| Some of the time | 912 (61) | 912 (61) | 717 (62) | 642 (62) |
| None of the time | 69 (5) | 69 (5) | 49 (4) | 41 (4) |
| Advised to change activity routine† | ||||
| Yes | 293 (20) | 293 (20) | 227 (20) | 204 (20) |
| Confidence in ability to exercise more§,§,** | ||||
| Very | 269 (44) | 269 (44) | †† | †† |
| Somewhat | 232 (38) | 232 (38) | ||
| Not at all | 112 (18) | 112 (18) | ||
| Interviewed before 11/2003 | 879 | 879 | ||
| How enjoyable is physical activity§,§,** | ||||
| Very | 108 (18) | 108 (18) | †† | †† |
| Somewhat | 227 (37) | 227 (37) | ||
| A little | 154 (25) | 154 (25) | ||
| Not at all | 124 (20) | 124 (20) | ||
| Interviewed before 11/2003 | 879 | 879 | ||
| Children over age 5 in the household* | ||||
| None | 1227 (75) | 1210 (76) | 918 (79) | 833 (80) |
| One | 265 (16) | 256 (16) | 160 (14) | 134 (13) |
| ≥2 | 137 (8) | 133 (8) | 84 (7) | 73 (7) |
Missing <10%.
Missing 10 to <20%.
Categorized using Institute of Medicine cutpoints.18
Missing 20–30%.
This question was added to the first telephone interview part way through the study (11/03),thus only some of the participants have information for this question. Percentages were calculated among those interviewed after this date (N = 613).
These variables were examined in separate models because they were added to the questionnaire later. They were not involved in the model selection process,thus there was no complete case analysis for these variables.
Maternal psychosocial health was characterized by state-trait anxiety (based on the State-Trait Anxiety Inventory28), perceived stress (Cohen Perceived Stress Scale29), and depressive symptoms (Center for Epidemiologic Studies Depression (CES-D) Scale30). The 14-item perceived stress scale was administered at 19 weeks and the 10-item scale was used at 29 weeks. We assessed exercise self-efficacy and enjoyment of physical activity for women interviewed later in the study period, after these questions were added to the second phone interview (11/2003). More details on these items can be found elsewhere.31
Analysis
Characteristics associated with inclusion in the complete case analysis were assessed with chi-square statistics. We used logistic regression models to explore correlates of physical activity, estimated with generalized estimating equations32,33 and a compound symmetric correlation34 to account for the dual measurements per woman. Exposures measured at each interview were treated as time-dependent. We did not find evidence of endogeneity (correlation between 19-week outcomes and 29-week correlates). We used backward selection to obtain the most parsimonious model. Variables with a P-value of less than 0.2 were retained in the model. Interactions with time were evaluated for all predictors and retained if P < .1. A smaller P-value cutoff was chosen for interactions to avoid over-stratifying the models.
The number of women in the final models depended on which variables were in the model. To determine the sensitivity of our models to the missingness of excluded variables, we reran the final models including only women who were not missing for any of the variables in the full model, before backward selection (complete case analysis). All 3 of our models began with the same set of correlates. We considered a > 10% change in odds ratio for any exposure to be important. To avoid over-interpretation due to multiple testing we considered P ≤ .03, rather than 0.05, to be statistically significant. We used SAS software, Version 9.2 of the SAS System for Windows for all analyses.
Results
Descriptive characteristics of the study population are shown in Table 1. The characteristics of the women included in the complete case analysis are also shown. Inclusion in the complete case analysis was less likely for women who were 25 years of age or less, African-American, single, of low income, at the extremes of body mass index (BMI), multiparous, had less than a high school education, smoked, had a high perceived stress score, a higher depressive symptom score, at least 1 child over age 5 in the house, or who did not report having a partner (P < .0001 for all comparisons). Inclusion was also less likely for women who were unemployed, interviewed during the spring or fall, scored adequate or less on the prenatal care initiation index or adequate plus on the prenatal care use index, took a vitamin less than daily, did not engage in outdoor activity, had high state or trait anxiety, or had previously given birth preterm (P ≤ .01 for all comparisons). None of the other variables in Table 1 were associated with inclusion in the complete case analysis.
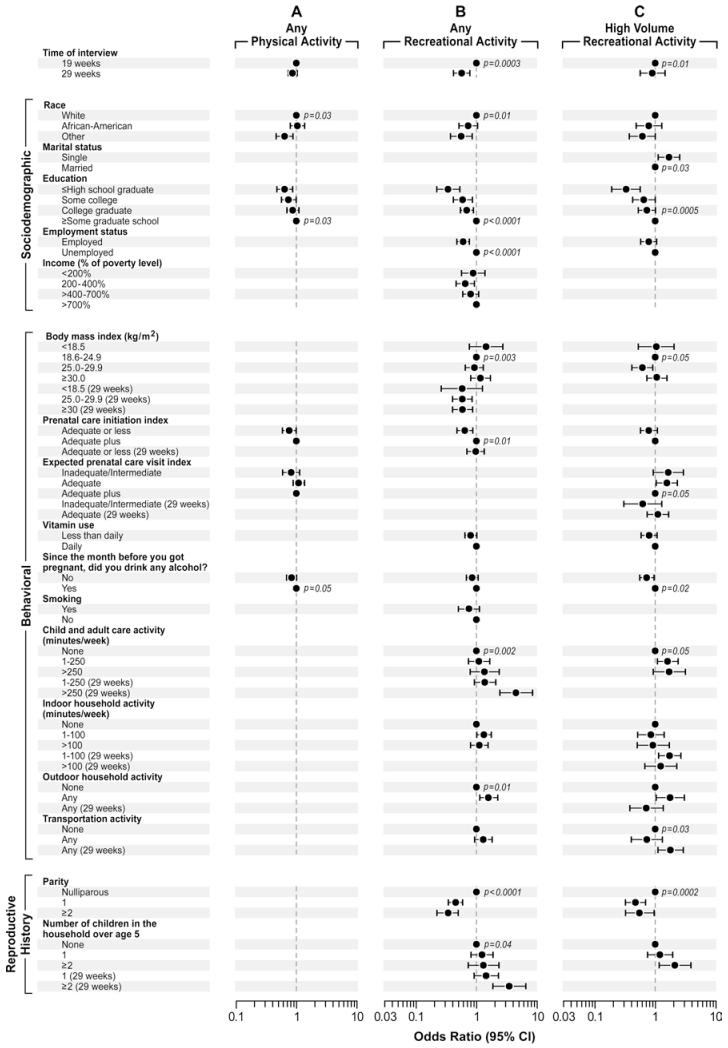
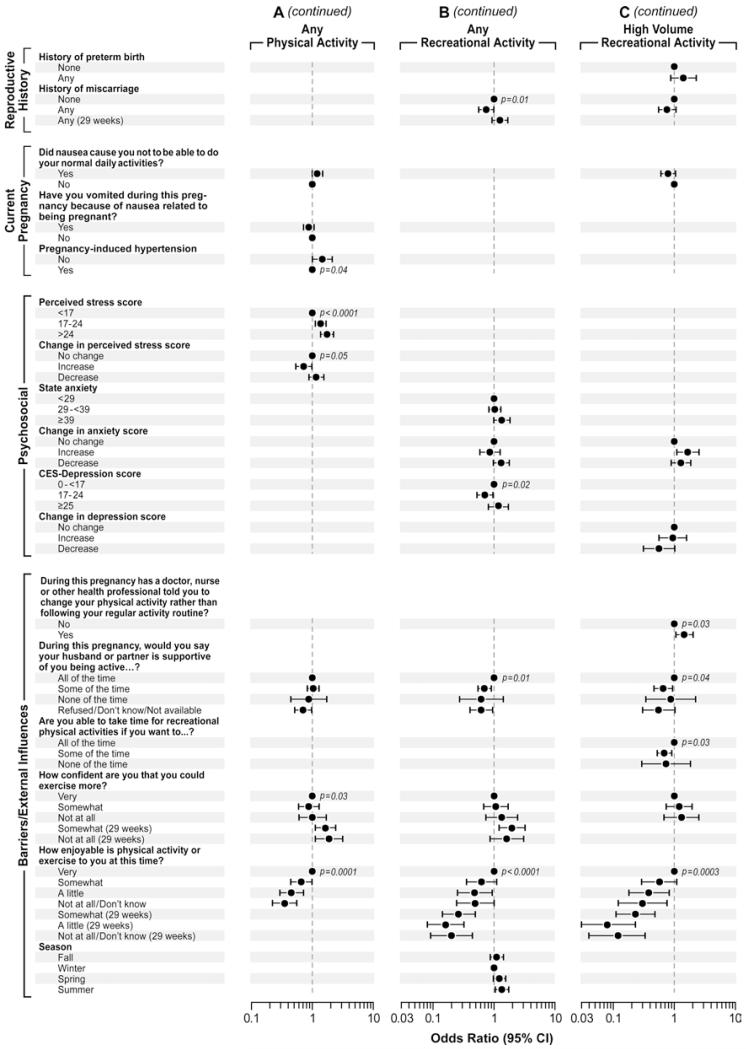
Figure 1 presents the correlates for each of the physical activity outcomes. Point estimates and confidence intervals are shown for variables that were retained in the final models. Variables with no odds ratio presented were not selected (P > .2) for that outcome. If an interaction with time was significant, odds ratios and point estimates are presented separately for each time point.
Figure 1.
Results of the multivariable analyses identifying correlates of 3 dichotomous physical activity outcomes, Pregnancy, Infection, and Nutrition 3 Study (2001–2005). “(29 weeks)” indicates a time-dependent association of the correlate with at least 1 of the activity outcomes. P-values are from a group test of all coefficients simultaneously and are drawn at the referent level for the variable (only P-values ≤ 0.03 are shown). Each variable is adjusted for the other nonmissing variables within each outcome. Variables with no odds ratio presented were not selected (P > .2) in that model.
Correlates of Any Physical Activity (Figure 1, Panel A)
Women of other races were less likely to perform any physical activity compared with white women [odds ratio (OR) 95% Confidence Interval (CI): 0.6 (0.5, 0.9)]. Lower education was associated with lower odds of engaging in any physical activity. Higher perceived stress score was associated with any physical activity [17–24 vs. <17 OR (CI): 1.4 (1.1, 1.7) and >24 vs. <17 OR (CI): 1.7 (1.4, 2.2)]. Women who were least confident that they could exercise more were more likely to engage in any physical activity. Lower reported enjoyment of physical activity was associated with lower odds of any physical activity [“not at all enjoyable/don’t know” vs. “very enjoyable” OR (CI): 0.3 (0.2, 0.6)].
One estimate changed by more than 10% from the presented model to the complete case analysis: partner support “none” from 0.87 to 0.97 in the complete case analysis (11%).
Correlates of Any Recreational Activity (Figure 1, Panel B)
Other race women were almost half as likely and African-American women were about three-fourths as likely as white women to perform any recreational activity. Women with a high school education or less were one-third as likely as women with some graduate school education to perform any recreational activity. Women who were employed had 0.6 times the odds of women who were not employed of performing any recreational activity (CI: 0.5, 0.8). Women who were lean prepregnancy were slightly more likely to perform any recreational activity at 19 weeks, while women who were overweight or obese prepregnancy were less likely to perform any recreational activity at 29 weeks. Compared with women who initiated prenatal care early, women who began prenatal care later were less likely to perform any recreational activity at 19 weeks, but were similar at 29 weeks. Women who reported > 250 min/wk of child/adult care activity were 4.5 times as likely as women who reported no child/adult care activity to perform any recreational activity (CI: 2.4, 8.5) at 29 weeks. Outdoor household activity was also positively associated with the performance of any recreational activity [OR (CI): 1.6 (1.1, 2.3)].
Parous women were much less likely than nulliparous women to perform any recreational activity [parity = 1, OR (CI): 0.4 (0.3, 0.6); parity ≥ 2, OR(CI): 0.3 (0.2, 0.5)]. However, women with 2 or more children over age 5 in the household were 3.5 times as likely as women with no children to perform any recreational activity at 29 weeks (CI: 1.8, 6.6). Women with a history of miscarriage were about three-quarters as likely as women without such a history to perform any recreational activity at 19 weeks, but groups were similar at 29 weeks. Partner support was positively associated with any recreational activity. Women who reported lower levels of enjoyment of physical activity were much less likely to perform any recreational activity.
One association changed by more than 10% from the presented model to the complete case analysis: the estimate for > 250 min/wk of child/adult care activity changed from 4.5 to 4.0 in the complete case analysis (12%).
Correlates of High Volume Recreational Activity (Figure 1, Panel C)
Single women were 1.7 times as likely as married women to perform high volume recreational activity (CI: 1.1, 2.5). Education was positively associated with the performance of high volume activity. Women who did not use alcohol were 0.7 times as likely as women who did report alcohol use to perform high volume recreational activity (CI: 0.5, 0.9). At 29 weeks, women who reported any transportation activity were 1.8 times as likely as women who did not report transportation activity to perform high volume recreational activity (CI: 1.1, 2.9).
Parity was negatively associated with high volume recreational activity. Women who reported that a health professional advised them to change their physical activity pattern were 1.5 times as likely as women who did not receive such advice to perform high volume activity (CI: 1.0, 2.0). Compared with women who reported being able to take time for recreational activity “all of the time,” women who reported less time were 0.7 times as likely to perform high volume recreational activity (“some of the time,” CI: 0.5, 0.9; “none of the time,” CI: 0.3, 1.8). Also similar to any recreational activity, enjoyment of physical activity was strongly associated with the performance of high volume recreational activity.
The estimates that changed from the presented model to the complete case analysis were, >100 min/wk of indoor activity at 29 weeks from 1.24 to 1.00 (19%) and change in depressive symptom score: “increase” from 0.94 to 0.82 (13%).
Discussion
We have identified characteristics related to total and recreational physical activity across pregnancy. These characteristics may be useful in defining population subgroups for intervention. Moreover, intervention tailoring may improve the effectiveness of physical activity interventions.35 Further research could determine if the correlates identified here are effective for tailoring physical activity interventions.
Some characteristics were strikingly consistent across outcomes and may inform interventions aimed at physical activity during pregnancy, regardless of mode. For example, women of higher education were more likely to be physically active no matter how activity was measured, which is supported by the literature.7,20,21,24,36-38 Women of white race were consistently more likely than other race women to perform any category of physical activity and more likely than African-American women to perform recreational activity. Previous studies of pregnant women have reported similar findings.15,21,22,24,39 Enjoyment of physical activity was a strong correlate of all 3 physical activity outcomes. While intuitive, to our knowledge this has not been reported previously among pregnant women. Focus groups conducted among pregnant women suggested that the most common barriers to physical activity during pregnancy were primarily intrapersonal, including time constraints and lack of energy or tiredness.25 Women may have to find physical activity very enjoyable to overcome these barriers. It is possible that by exposing pregnant women to different types of physical activities, they may be more likely to find something they enjoy and be physically active during pregnancy.
Some characteristics were associated with recreational activity specifically and may inform interventions that are targeted to that mode of physical activity. Employed women were less likely to perform recreational activity, while in previous studies employment was not associated9 or was positively associated.37 In agreement with one study,22 history of miscarriage was associated with any recreational activity (and in a similar direction for high volume recreational activity). The association was negative at 19 weeks, but positive at 29 weeks. We hypothesize that once the risk period for miscarriage has passed women are more comfortable with participating in recreational activity. Similarly, in 2 previous studies women who received fertility treatments were less likely to be active in early pregnancy.16,17
Similar to previous studies, parous women were less likely to perform recreational activity;10,16,22,24,37-39 however, women with children in the household older than age 5 were more likely to perform recreational activity. Adding maternal age or the number of children in the household who were younger than 5 back into the final model did not change the estimates for parity (data not shown). In addition, women who performed child/adult care activity were more likely to perform recreational activity. Thus it is not entirely clear what parity represents, as its association with recreational activity exists despite control for these related factors. In one focus group participants reported having children to look after as a barrier to being physically active,40 thus the availability of child care may be involved in these associations.
Differences in predictors between any and high volume recreational activity may be informative for interventions seeking to increase recreational activity levels. Single marital status and health professional advice were associated with high volume recreational activity. Both marital status16,21,37 and health professional advice9,12,37,40 have been inconsistently associated with physical activity. Women who reported having time for recreational activity were more likely to perform high volume recreational activity. Lack of time has been previously reported as a barrier to physical activity.12,40,41 It is possible that women are able to incorporate small amounts of recreational activity into their lives, but they feel they do not have time for higher levels of activity.
Interventions may need to be time dependent. As previously described history of miscarriage has a time-dependent association with recreational activity. Similarly, overweight and obese women were less likely to engage in any recreational activity, but only at 29 weeks. This suggests that interventions to increase recreational activity in overweight or obese women may be more important later in pregnancy. We did not observe the same associations for high volume recreational activity, however, our activity measures were based on perceived intensity and moderate or vigorous activity may not be difficult to achieve in an overweight or obese woman. Previous studies have found lower levels of physical activity during pregnancy among women who were overweight.22,36,38,42
Several factors were not associated with physical activity in the multivariable models although they have been associated in previous studies, these include age,20-22,24,36,39 higher income,21,37,39 and nonsmoking.21,24 One other study has reported no association with age in a multivariable analysis.37 It is possible that these associations are being explained by the other correlates included in our adjusted models.
Limitations
To improve interpretability and create parsimonious models we have performed model selection based on a P-value cut-off. Model selection may introduce bias since small associations are less likely to reach significance and variables that are significant may be overestimated.43 We have also measured physical activities by self-report. Women may tend to over-report their activities due to the perceived desirability of being active, or they may not accurately recall the activities they performed. However, the low proportion of active women in our data suggests that over-reporting may not be an issue. We examined over 35 potential correlates of activity and performed numerous hypothesis tests. To limit the number of spurious results we have not interpreted any variables with a P-value greater than 0.03. In addition, the women in our study, while recruited systematically, comprise a volunteer population which may limit generalizability. We lacked data to assess some characteristics previously associated with physical activity in the literature including, health insurance,15 multiple gestations,22,42 pelvic girdle pain,42 and prepregnancy activity.10,23,24,36,42,44
The definition of “high volume recreational activity” resembles recommendations for activity during pregnancy supported by several professional societies. However, definitions of these recommendations for research are difficult.1,2,45,46 The College recommends that “ … an accumulation of 30 minutes or more of moderate exercise a day should occur on most, if not all, days of the week.”1 Similarly, The Society of Obstetricians and Gynecologists of Canada recommends participation in 4 30-minute exercise sessions per week at a moderate intensity.46 Both of these recommendations specify exercise (not all physical activity) and only include moderate intensity activity, not vigorous. The current U.S. Health and Human Services recommendation is similar to The College’s recommendation, but is not limited to exercise.2 The position of the Royal College of Obstetricians and Gynecologists resembles the Canadian guideline but includes 4 to 7 sessions per week and acknowledges that “ … regular exercisers before pregnancy should be able to engage in high intensity exercise programmes …”45. However, they do not specify an amount of high intensity exercise.
Conclusions
This study had the advantage of a large population of women and detailed assessments of their physical activities. Several important and novel characteristics were measured including psychosocial variables and potential barriers to recreational activity. We found several previously unreported correlates of recreational physical activity in pregnancy. We also found that several associations changed between 2 time periods during pregnancy. This implies that physical activity interventions during pregnancy should change over gestation. This analysis identifies new avenues for investigation into encouraging women to be active during pregnancy.
Acknowledgments
This research was supported, in part, by the Intramural Research Program of the National Institutes of Health (NIH), National Institute of Environmental Health Sciences. Funding was provided by the NIH/National Institute of Child Health and Human Development (#HD37584), NIH/National Cancer Institute (#CA109804), and NIH General Clinical Research Center (#RR00046). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The Pregnancy, Infection, and Nutrition Study is a joint effort of many investigators and staff members whose work is gratefully acknowledged. We also thank Drs. Donna Baird and Lea Cupul-Uicab for their insightful comments on this manuscript.
Contributor Information
Anne Marie Z. Jukic, Epidemiology Branch, National Institute of Environmental Health Sciences, Durham, NC
Kelly R. Evenson, Dept of Epidemiology, University of North Carolina, Chapel Hill, NC
Amy H. Herring, Dept of Biostatistics, University of North Carolina, Chapel Hill, NC
Allen J. Wilcox, Epidemiology Branch, National Institute of Environmental Health Sciences, Durham, NC
Katherine E. Hartmann, Institute for Medicine and Public Health, Vanderbilt University, Nashville, TN
Julie L. Daniels, Dept of Epidemiology, University of North Carolina, Chapel Hill, NC
References
- 1.ACOG Committee Obstetric Practice ACOG Committee opinion. Number 267, January 2002: exercise during pregnancy and the postpartum period. Obstet Gynecol. 2002;99(1):171–173. doi: 10.1016/s0029-7844(01)01749-5. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services . Physical activity guidelines for Americans. 2008. p. 61. Available at: http://www.health.gov/PAGuidelines/guidelines/default.aspx. [Google Scholar]
- 3.Evenson K, Wen F. National prevalence and correlates of objectively measured physical activity and sedentary behaviors among pregnant women. Prev Med. 2011;53:39–43. doi: 10.1016/j.ypmed.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 4.Borodulin KM, Evenson KR, Wen F, Herring AH, Benson AM. Physical activity patterns during pregnancy. Med Sci Sports Exerc. 2008;40(11):1901–1908. doi: 10.1249/MSS.0b013e31817f1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clarke PE, Rousham EK, Gross H, Halligan AW, Bosio P. Activity patterns and time allocation during pregnancy: a longitudinal study of British women. Ann Hum Biol. 2005;32(3):247–258. doi: 10.1080/03014460500049915. [DOI] [PubMed] [Google Scholar]
- 6.DiNallo JM, Le Masurier GC, Williams NI, Downs DS. Walking for health in pregnancy: assessment by indirect calorimetry and accelerometry. Res Q Exerc Sport. 2008;79(1):28–35. doi: 10.1080/02701367.2008.10599457. [DOI] [PubMed] [Google Scholar]
- 7.Haakstad LA, Voldner N, Henriksen T, Bo K. Physical activity level and weight gain in a cohort of pregnant Norwegian women. Acta Obstet Gynecol Scand. 2007;86(5):559–564. doi: 10.1080/00016340601185301. [DOI] [PubMed] [Google Scholar]
- 8.Kinnunen TI, Pasanen M, Aittasalo M, et al. Preventing excessive weight gain during pregnancy—a controlled trial in primary health care. Eur J Clin Nutr. 2007;61(7):884–891. doi: 10.1038/sj.ejcn.1602602. [DOI] [PubMed] [Google Scholar]
- 9.Mottola MF, Campbell MK. Activity patterns during pregnancy. Can J Appl Physiol. 2003;28(4):642–653. doi: 10.1139/h03-049. [DOI] [PubMed] [Google Scholar]
- 10.Pereira MA, Rifas-Shiman SL, Kleinman KP, Rich-Edwards JW, Peterson KE, Gillman MW. Predictors of change in physical activity during and after pregnancy: Project Viva. Am J Prev Med. 2007;32(4):312–319. doi: 10.1016/j.amepre.2006.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rousham EK, Clarke PE, Gross H. Significant changes in physical activity among pregnant women in the UK as assessed by accelerometry and self-reported activity. Eur J Clin Nutr. 2006;60(3):393–400. doi: 10.1038/sj.ejcn.1602329. [DOI] [PubMed] [Google Scholar]
- 12.Symons Downs D, Hausenblas HA. Women’s exercise beliefs and behaviors during their pregnancy and postpartum. J Midwifery Womens Health. 2004;49(2):138–144. doi: 10.1016/j.jmwh.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 13.van Raaij JM, Schonk CM, Vermaat-Miedema SH, Peek ME, Hautvast JG. Energy cost of physical activity throughout pregnancy and the first year postpartum in Dutch women with sedentary lifestyles. Am J Clin Nutr. 1990;52(2):234–239. doi: 10.1093/ajcn/52.2.234. [DOI] [PubMed] [Google Scholar]
- 14.McParlin C, Robson SC, Tennant PW, et al. Objectively measured physical activity in pregnancy: a study in obese and overweight women. BMC Pregnancy Childbirth. 2010;10(1):76. doi: 10.1186/1471-2393-10-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evenson KR, Wen F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999-2006. Prev Med. 2010;50(3):123–128. doi: 10.1016/j.ypmed.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Juhl M, Madsen M, Andersen AM, Andersen PK, Olsen J. Distribution and predictors of exercise habits among pregnant women in the Danish National Birth Cohort. Scand J Med Sci Sports. 2010;22(1):128–138. doi: 10.1111/j.1600-0838.2010.01125.x. [DOI] [PubMed] [Google Scholar]
- 17.Hegaard HK, Damm P, Hedegaard M, et al. Sports and leisure time physical activity during pregnancy in nulliparous women. Matern Child Health J. 2010;14(1):1–8. doi: 10.1007/s10995-010-0647-y. [DOI] [PubMed] [Google Scholar]
- 18.IOM (Institute of Medicine) NRC (National Research Council) Weight gain during pregnancy: reexamining the guidelines. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- 19.Amorim AR, Rossner S, Neovius M, Lourenco PM, Linne Y. Does excess pregnancy weight gain constitute a major risk for increasing long-term BMI? Obesity (Silver Spring) 2007;15(5):1278–1286. doi: 10.1038/oby.2007.149. [DOI] [PubMed] [Google Scholar]
- 20.Evenson KR, Savitz DA, Huston SL. Leisure-time physical activity among pregnant women in the US. Paediatr Perinat Epidemiol. 2004;18(6):400–407. doi: 10.1111/j.1365-3016.2004.00595.x. [DOI] [PubMed] [Google Scholar]
- 21.Petersen AM, Leet TL, Brownson RC. Correlates of physical activity among pregnant women in the United States. Med Sci Sports Exerc. 2005;37(10):1748–1753. doi: 10.1249/01.mss.0000181302.97948.90. [DOI] [PubMed] [Google Scholar]
- 22.Zhang J, Savitz DA. Exercise during pregnancy among US women. Ann Epidemiol. 1996;6(1):53–59. doi: 10.1016/1047-2797(95)00093-3. [DOI] [PubMed] [Google Scholar]
- 23.Hinton PS, Olson CM. Predictors of pregnancy-associated change in physical activity in a rural white population. Matern Child Health J. 2001;5(1):7–14. doi: 10.1023/a:1011315616694. [DOI] [PubMed] [Google Scholar]
- 24.Ning Y, Williams MA, Dempsey JC, Sorensen TK, Frederick IO, Luthy DA. Correlates of recreational physical activity in early pregnancy. J Matern Fetal Neonatal Med. 2003;13(6):385–393. doi: 10.1080/jmf.13.6.385.393. [DOI] [PubMed] [Google Scholar]
- 25.Evenson KR, Moos MK, Carrier K, Siega-Riz AM. Perceived barriers to physical activity among pregnant women. Matern Child Health J. 2009;13(3):364–375. doi: 10.1007/s10995-008-0359-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evenson K, Wen F. Measuring physical activity among pregnant women using a structured one-week recall questionnaire: evidence for validity and reliability. Int J Behav Nutr Phys Act. 2010;7(1):21. doi: 10.1186/1479-5868-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health. 1994;84(9):1414–1420. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spielberger C. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto: 1983. [Google Scholar]
- 29.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 30.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 31.Evenson KR. Towards an understanding of change in physical activity from pregnancy through postpartum. Psychol Sport Exerc. 2011;12:36–45. doi: 10.1016/j.psychsport.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liang KY, Zeger SL. Regression analysis for correlated data. Annu Rev Public Health. 1993;14:43–68. doi: 10.1146/annurev.pu.14.050193.000355. [DOI] [PubMed] [Google Scholar]
- 33.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 34.Lipsitz SR, Laird NM, Harrington DP. Generalized estimating equations for correlated binary data—using the odds ratio as a measure of association. Biometrika. 1991;78(1):153–160. [Google Scholar]
- 35.Bull FC, Kreuter MW, Scharff DP. Effects of tailored, personalized and general health messages on physical activity. Patient Educ Couns. 1999;36(2):181–192. doi: 10.1016/s0738-3991(98)00134-7. [DOI] [PubMed] [Google Scholar]
- 36.Fell DB, Joseph KS, Armson BA, Dodds L. The impact of pregnancy on physical activity level. Matern Child Health. J Sport Exer Psychol. 2009;13(5):597–603. doi: 10.1007/s10995-008-0404-7. [DOI] [PubMed] [Google Scholar]
- 37.Domingues MR, Barros AJ. Leisure-time physical activity during pregnancy in the 2004 Pelotas Birth Cohort Study. Rev Saude Publica. 2007;41(2):173–180. doi: 10.1590/s0034-89102007000200002. [DOI] [PubMed] [Google Scholar]
- 38.Donahue SM, Zimmerman FJ, Starr JR, Holt VL. Correlates of pre-pregnancy physical inactivity: results from the pregnancy risk assessment monitoring system. Matern Child Health J. 2010;14(2):235–244. doi: 10.1007/s10995-009-0441-x. [DOI] [PubMed] [Google Scholar]
- 39.Schmidt MD, Pekow P, Freedson PS, Markenson G, Chasan-Taber L. Physical activity patterns during pregnancy in a diverse population of women. J Womens Health. 2006;15(8):909–918. doi: 10.1089/jwh.2006.15.909. [DOI] [PubMed] [Google Scholar]
- 40.Cioffi J, Schmied V, Dahlen H, et al. Physical activity in pregnancy: women’s perceptions, practices, and influencing factors. J Midwifery Womens Health. 2010;55(5):455–461. doi: 10.1016/j.jmwh.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 41.Cramp AG, Bray SR. A prospective examination of exercise and barrier self-efficacy to engage in leisure-time physical activity during pregnancy. Ann Behav Med. 2009;(Jun):5. doi: 10.1007/s12160-009-9102-y. [DOI] [PubMed] [Google Scholar]
- 42.Owe KM, Nystad W, Bo K. Correlates of regular exercise during pregnancy: the Norwegian Mother and Child Cohort Study. Scand J Med Sci Sports. 2009;19(5):637–45. doi: 10.1111/j.1600-0838.2008.00840.x. [DOI] [PubMed] [Google Scholar]
- 43.Miller AJ. Selection of subsets of regression variables. J R Stat Soc Ser A Stat Soc. 1984;147:389–425. [Google Scholar]
- 44.Taber L, Schmidt MD, Pekow P, Sternfeld B, Manson J, Markenson G. Correlates of physical activity in pregnancy among Latina women. Matern Child Health J. (4):353–363. doi: 10.1007/s10995-007-0201-8. [DOI] [PubMed] [Google Scholar]
- 45.Bell BB, Dooley P. Exercise in pregnancy: guidelines and audit committee of the Royal College of Obstetricians and Gynaecologists. 2006. RCOG Statement No. 4; p. 7. [Google Scholar]
- 46.Davies GA, Wolfe LA, Mottola MF, et al. Exercise in pregnancy and the postpartum period. J Obstet Gynaecol Can. 2003;25(6):516–529. doi: 10.1016/s1701-2163(16)30313-9. [DOI] [PubMed] [Google Scholar]